Abstract
Background
Significant pain from HIV-associated sensory neuropathy (HIV-SN) affects ∼40% of HIV infected individuals treated with antiretroviral therapy (ART). The prevalence of HIV-SN has increased despite the more widespread use of ART. With the global HIV prevalence estimated at 33 million, and with infected individuals gaining increased access to ART, painful HIV-SN represents a large and expanding world health problem. There is an urgent need to develop effective pain management strategies for this condition.
Method and Findings
Objective: To evaluate the clinical effectiveness of analgesics in treating painful HIV-SN. Design: Systematic review and meta-analysis. Data sources: Medline, Cochrane central register of controlled trials, www.clinicaltrials.gov, www.controlled-trials.com and the reference lists of retrieved articles. Selection criteria: Prospective, double-blinded, randomised controlled trials (RCTs) investigating the pharmacological treatment of painful HIV-SN with sufficient quality assessed using a modified Jadad scoring method. Review methods: Four authors assessed the eligibility of articles for inclusion. Agreement of inclusion was reached by consensus and arbitration. Two authors conducted data extraction and analysis. Dichotomous outcome measures (≥30% and ≥50% pain reduction) were sought from RCTs reporting interventions with statistically significant efficacies greater than placebo. These data were used to calculate RR and NNT values.
Results
Of 44 studies identified, 19 were RCTs. Of these, 14 fulfilled the inclusion criteria. Interventions demonstrating greater efficacy than placebo were smoked cannabis NNT 3.38 95%CI(1.38 to 4.10), topical capsaicin 8%, and recombinant human nerve growth factor (rhNGF). No superiority over placebo was reported in RCTs that examined amitriptyline (100mg/day), gabapentin (2.4g/day), pregabalin (1200mg/day), prosaptide (16mg/day), peptide-T (6mg/day), acetyl-L-carnitine (1g/day), mexilitine (600mg/day), lamotrigine (600mg/day) and topical capsaicin (0.075% q.d.s.).
Conclusions
Evidence of efficacy exists only for capsaicin 8%, smoked cannabis and rhNGF. However,rhNGF is clinically unavailable and smoked cannabis cannot be recommended as routine therapy. Evaluation of novel management strategies for painful HIV-SN is urgently needed.
Introduction
HIV-associated distal sensory neuropathy (HIV-SN) is a frequently occurring neurological complication of HIV infection. HIV-SN prevalence has increased despite (or because of) the introduction of otherwise successful antiretroviral therapy [1]. HIV-SN is one of the most prevalent problems experienced by people receiving antiretroviral therapy and the associated pain has a major impact on quality of life in otherwise largely healthy individuals. HIV-SN is a distal symmetrical axonal, predominantly sensory polyneuropathy that affects the feet and less frequently the hands. HIV-SN is comprised of at least two clinically indistinguishable, and often coexisting, neuropathies: A distal sensory polyneuropathy associated with HIV disease itself (HIV-DSP), and a distal sensory polyneuropathy associated with antiretroviral treatment, Antiretroviral toxic neuropathy (HIV-ATN). HIV-DSP was recognised early in the HIV pandemic [2] and is associated with advanced HIV disease [1] [3]. HIV-ATN was initially observed following the introduction of particular nucleoside reverse transcriptase inhibitors (NRTI) – stavudine, didanosine and zalcitabine - the ‘dNRTIs’ [4]–[5]. The presence of sensory neuropathic symptoms in an ARV naïve patient is highly suggestive of HIV -DSP. Often only a temporal association between the onset of symptoms and the starting of a particular ARV agent gives the only hint as to aetiology, as in most other clinical respects the two are almost identical.
The introduction of combination antiretroviral therapy (cART) in the mid 1990s dramatically reduced the morbidity and mortality associated with HIV among patients who have access to treatment [6]. Life expectancy with HIV in well-resourced countries is now estimated to be up to two-thirds that of the general population [7]–[8]. While the incidence of most neurological complications of HIV has fallen with the introduction of effective therapy, rates of HIV-SN have been rising since the first effective antiretroviral drugs were developed [9]. Recent estimates of HIV-SN prevalence among cohorts with access to cART range from 20% [10] to >50% [11]. Importantly, the available evidence suggests that HIV-SN prevalence remains high among cART-treated patients, even in countries where known neurotoxic antiretroviral drugs such as stavudine are no longer commonly used. Depending on the population surveyed, HIV-SN, regardless of previous ARV exposure, has a prevalence of between 13% [12] and >50% [13]–[14] of HIV infected individuals, of whom 40% experience severe pain, ≥5/10 Numeric Pain Rating Scale (NPRS), and 90% experiencing some pain, which can be severely debilitating [1]. In less well-resourced centres, use of stavudine, an inexpensive and effective antiretroviral, in first-line HIV treatment remains common despite the high risk of neurotoxicity [15].
Importantly two recent studies have emphasised the continued and growing global impact of HIV-SN. A large cross-sectional study of 598 HIV infected individuals in South Africa, reported that the frequency of symptomatic HIV-SN increases from 23% to 40% following exposure to ART therapy, with 60% being symptomatic if previously exposed to stavudine [16]. Another large cross-sectional study from the US studying 1539 HIV infected individuals has reported that 57%(881) demonstrated evidence of the presence of HIV-SN, with 38% of these individuals reporting pain [17].
Current estimates of global HIV prevalence stand at 33 million, with 2.7 new infections each year and more patients gaining access to cART [15]. With high rates of HIV-SN now reported globally, and up to 90% of affected patients experiencing potentially debilitating neuropathic pain, HIV-SN represents a large and potentially worsening source of global HIV-related morbidity. There is an urgent need to understand better the pathogenesis of HIV-SN, to identify risk factors, and identify and implement effective preventative and pain management strategies.
Evidence-based guidelines for the pharmacological management of neuropathic pain tend to focus on a “blanket” approach of recommending therapies across the spectrum of neuropathic pain, irrespective of the underlying condition [18]–[19]. Recent NICE guidance for the management of neuropathic pain in “non-specialist settings” have adopted this approach [20]. This may not be appropriate for HIV-SN for three main reasons. Firstly, neuropathic pain is a heterogeneous phenomenon, both within and across underlying conditions, and evidence obtained from the study of an analgesic in one condition cannot necessarily be applied to another [21]–[22]. Secondly, in high, middle and low income countries the pain associated with HIV-SN will usually be managed outside of specialist pain management clinics, so appropriate, disease specific guidance may be required. Finally, there are a number of randomised controlled trials (RCTs) conducted in HIV-SN, which were not identified in the NICE guidance. Therefore, we have conducted a systematic review and meta-analysis to elucidate the evidence base for pharmacological management of neuropathic pain in HIV-SN.
Methods
Eligibility, data sources and search strategy
In accordance with PRISMA [23], we sought to identify RCTs that included patients with painful HIV-SN and reported at least one clinically relevant pain outcome measure.
A systematic search, without language restrictions, was conducted on 20 June 2008, and a follow-up search on 22 February 2010, with the following databases: Medline (from 1966 to date searched), The Cochrane central register of controlled trials (Cochrane Library 2010, Issue 2), www.clinicaltrials.gov (a US registry of clinical trials) and www.controlled-trials.com (a meta-registry of controlled trials). Search terms used were: “HIV” “AIDS” “pain” “painful” “neuropathy” “neuropathic”, in combination with “random” “randomised” and “double-blinded”. Further trials were identified by hand searching the reference lists of identified trials and review articles, relevant NICE guidelines and Health Technology Assessment reports.
Study selection and risk of bias assessment
We excluded animal studies, reviews, letters, abstract-only trials, open-label trials, and trials that were not randomised. The identified RCTs then underwent independent quality assessment by four authors (TJCP, CLC, SC and ASCR) using a 7-point modified “Jadad” scoring system that assessed the presence and quality of double-blinding, randomisation, study size and reporting of withdrawal and drop outs [24]–[25]. RCTs with a score of less than five points and studies that enrolled fewer than five HIV-SN patients were excluded from the systematic review. Scoring discrepancies between authors were resolved through discussion and consensus; with final arbitration by ASCR.
Data extraction
Data were extracted from eligible RCTs by one author (TJCP). Data extracted included: year of publication; study design and duration; study sample population and characteristics; withdrawals; interventions; doses; pain and non-pain related primary and secondary outcome measures; and adverse events.
Where possible, dichotomous pain improvement outcome data were extracted from RCTs that reported efficacy superior to placebo. Intention to treat (ITT) responder rates for 30% and 50% pain relief were sought for the longest follow-up period reported in each study. If required, authors were contacted for missing or unreported data.
RCTs in which the primary pain outcome of a studied intervention did not show efficacy greater than placebo in the intention to treat population, were not included in subsequent analyses.
Statistical analysis
For each intervention the extracted dichotomous outcomes were used to calculate numbers needed to treat (NNT) by two authors (TJCP and ASCR), with 95% confidence intervals for 30% and 50% pain improvement responders. We originally planned to access heterogeneity according to the method of Armitage & Berry [26], and visually [27] however as only three studies were used in the meta-analysis, this was felt to be inappropriate. Similarly, a sensitivity analysis was not performed, as there were insufficient data. All calculations were undertaken using Microsoft Excel 2007.
Results
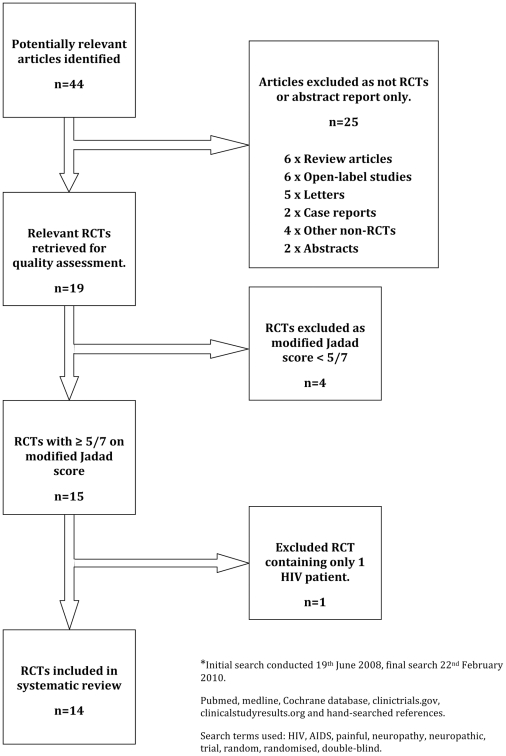
We identified 44 potentially relevant articles (Figure 1). Twenty-five articles were excluded after screening identified these as being a review article, letter, open-label study, case report or other non-RCT study. The remaining 19 RCTs were retrieved and independently reviewed by four authors (TJCP, CLC, SC and ASCR). Four articles were excluded at this stage by scoring <5 out of 7-points with the modified Jadad score. A further RCT was excluded as having <5 HIV-SN patients enrolled. Details of these excluded RCTs, and therefore of interventions that must be regarded as not having been adequately tested, are shown in Table 1.
Figure 1. PRISMA flow diagram of included randomized controlled trials.
Table 1. Studies excluded from the analysis.
| Reference | Treatment | Primary Reason for Exclusion |
| [37] | Acetyl-L-carnitine | Review |
| [61] | Acetyl-L-carnitine | Review |
| [43] | Cannabinoids | Review |
| [62] | Lamotrigine | Review |
| [63] | Antidepressants | Review |
| [64] | Herbal medicine | Review |
| [44] | 8% capsaicin patch | Open-label |
| [45] | 8% capsaicin patch | Abstract |
| [33] | Acetyl-L-carnitine | Open-label |
| [34] | Acetyl-L-carnitine | Open-label |
| [65] | Recombinant human NGF | Open-label |
| [66] | Flecainide | Open-label |
| [67] | 5% lidocaine patch | Open-label |
| [68] | Acupuncture | Letter |
| [69] | Acupuncture | Letter |
| [70] | Acupuncture | Letter |
| [46] | Gabapentin | Letter |
| [47] | Gabapentin | Letter |
| [49] | Gabapentin | Case report |
| [71] | Prednisolone | Case report |
| [48] | Gabapentin | Abstract |
| [42] | Smoked cannabis | Other non-RCT |
| [35] | Acetyl-L-carnitine | Other non-RCT |
| [72] | Acupuncture | Other non-RCT |
| [32] | Acetyl-L-carnitine | Other non-RCT |
| [73] | 5% lidocaine patch | Modified Jadad score <5 |
| [74] | Mexiletine | Modified Jadad score <5 |
| [75] | Memantine | Modified Jadad score <5 |
| [76] | Nimodipine | Modified Jadad score <5 |
| [52] | Lamotrigine | <5 patients enrolled |
The remaining 14 RCTs were retained for further analysis (Table 2). Of the 14 trials retained for further analysis, 13 were of a parallel group design and one a cross-over design. All were placebo controlled with one using “active” placebo [28]. Data extraction was for the longest follow-up period reported by the article. In most cases this was to the end of the treatment phase, except for a study of a topical 8% capsaicin [28] that reported data for 12 weeks after a single treatment application.
Table 2. Characteristics and results of included studies.
| Reference | Participants recruited (completed) | Design and duration | Intervention (n = patient episodes) | Maximum dose studied | Primary Outcome | Data (ITT) | Superior to placebo? |
| Youle M et al 2007 [36] | 90(76) | Parallel: 2 wks | Acetyl-L-carnitine 500 mg bd i.m. (n = 43); placebo (n = 47) | 1000mg/day | VAS (0–10cm) change: baseline to wk 2. | ITT: Acetyl-L-carnitine: −1.32 (SD 1.84); placebo −0.61 (SD 1.55)(p = 0.07) | No |
| Shlay JC et al 1998 [38] | 136 (105) | Parallel: 14 wks | Amitriptyline (n = 71); placebo (n = 65) | 75mg/day | GP score: change baseline to wk 14. | ITT with LOCF: Amitriptyline: −0.26; placebo: −0.30;difference 0.00 95%CI(−0.18 to 0.19)(p = 0.99) | No |
| Paice JA et al 2000 [29] | 26(14) | Parallel:4 wks. | Capsaicin 0.075% cream q.d.s. (n = 15); placebo (n = 11) | 0.075% q.d.s. | NRS (0–10): change from baseline to wk 4. | No numeric data given. Stated no statistically significant difference between capsaicin 0.075% and placebo (p>0.05) | No |
| Simpson DM et al 2008 [28] | 307(274) | Parallel: 12 wks follow-up. | Capsaicin 8% patch for 30min (n = 72); 60min (n = 78); 90min (n = 75); placebo (capsaicin 0.04%) (n = 82) | 8% for 90min. | NPRS: % change baseline to wk 12. | ITT with LOCF: Capsaicin: −22.8 (SD 30.6); placebo −10.7 (SD 30.8); (p = 0.0026) | Yes |
| Abrams DI et al 2007 [40] | 55(50) | Parallel: 5 days | Smoked cannabis (n = 27); placebo (n = 28) | 3.56% Δ-9- tetrahydrocannabinol t.d.s. | VAS: % change from baseline to day 5. | ITT: Cannabis: −34% (IQR −71 to −16); placebo −17% (IQR – 29 to 8) (p = 0.03) | Yes |
| Ellis RJ et al 2009 [41] | 34(27) | Crossover: 5 days, 2 wks washout, 5 days treatment. | Smoked cannabis (n = 28); placebo (n = 28) | Max tolerable: 1 to 8% Δ-9- tetrahydrocannabinol q.d.s. | DDS (0–20): median change from baseline to day 5. | Difference in DDS reduction cannabis vs placebo for PP: −3.3 p = 0.016, no data for ITT: said to be ‘similar’ with p = 0.020 | Yes |
| Hahn K et al 2004 [30] | 26(24) | Parallel: 4 wks treatment. | Gabapentin (n = 15); placebo (n = 11) | 2400mg/day | VAS: median change: baseline to wk 4. | Gabapentin: −44.1; placebo: −29.8. Stated as being not statistically significant. | No |
| Simpson DM et al 2010 [50] | 302(241) | Parallel: 14 wks treatment. | Pregabalin (n = 151); placebo (n = 151) | 1200mg/day | NPRS: mean change: baseline to wk 14. | ITT: Pregabalin: −2.88; placebo −2.63 (p = 0.39) | No |
| Simpson DM et al 2000 [51] | 42(29) | Parallel: 14 wks treatment | Lamotrigine (n = 20); placebo (n = 22) | 300mg/day | GP score: mean change: baseline to wk 14. | ITT with LOCF: Lamotrigine: −0.242 (SE 0.092); placebo: −0.183 (SE 0.087) (p = 0.65) | No |
| Simpson et al 2003 [31] | 227(172) | Parallel:12 wks treatment. | Lamotrigine (n = 150); placebo (n = 77) | 600mg/day | GP score: change: baseline to wk 12. | PP: Lamotrigine vs placebo. No data given, stated no statistically significant difference seen in all or ARV stratum. | No |
| Keiburtz K et al 1998 [39] | 145(104) | Parallel: 8 wks | Mexilitine (n = 48); amitriptyline (n = 47); placebo (n = 50) | Mexilitine: 300mg/day Amitriptyline: 100mg/day | GP score: mean change: baseline to wk 8. | ITT: Amitriptyline: −0.31 (SD 0.31); mexilitine: −0.23 (SD 0.41); placebo −0.20 (SD 0.30) No p value given, stated no statistical significance | No |
| McArthur JC et al 2000 [53] | 270(235) | Parallel:18 wks | Recombinant human NGF (n = 180); placebo (n = 90) | 0.3µg/kg s.c. twice weekly | GP score: median change: baseline to wk 18. | ITT with LOCF: NGF 0.1µg/kg: −0.18 (−0.10 to −0.25)(p = 0.05); NGF 0.3µg/kg: −0.21 (−0.14 to −0.29)(p = 0.04); placebo: 0.06 (+0.01 to −0.14) | Yes |
| Simpson DM et al 1996 [54] | 104(81) | Parallel: 12 wks | Peptide-T (n = 40); placebo (n = 41)* PP data | 6mg/day intranasal | Modified GP score: mean change: baseline to wk 12. | PP: Peptide-T: −0.24 (±0.45); placebo −0.39 (±0.19) (p = 0.32). ITT results not presented but stated showed the ‘same pattern’. | No |
GP - Gracely Pain Score, VAS – Visual Analogue Scale, ITT – Intention To Treat population, PP -Per Protocol population, NRS – Numerical Rating Scale, NPRS- Numerical Pain Rating Scale, DDS – Descriptor Differential Scale, LOCF - Last Observation Carried Forward.
In two studies [29] and [30] no reference to ITT analysis was made. In one of these RCTs studying topical capsaicin 0.075% efficacy [29] no primary outcome data were published, as it was reported that no superiority to placebo was seen. In a study of lamotrigine efficacy [31] only a per protocol (PP) population data analysis was undertaken. This was reported to show no superiority over placebo; however no primary outcome data were reported.
Of the four trials that reported superiority of an intervention over placebo, three reported dichotomous pain outcome measures. Where possible we used responder rate data for ≥30% and ≥50% improvement in pain as measured using Visual Analogue Scale (VAS) or Numerical Pain Rating Scale (NPRS). These data were requested from the authors if they had not been reported.
Acetyl –L-carnitine
Whilst acetyl-L-carnitine has been the subject of six articles [32]–[37] in the treatment of painful HIV-SN, only one was an RCT [36] and eligible for inclusion. This was a parallel group trial of acetyl-L-carnitine (1000mg/day) and placebo intramuscular injections. In this RCT acetyl-L-carnitine, in an analysis of the PP population, showed a modest superiority to placebo. However an analysis of the ITT population did not show superiority to placebo: mean change in VAS (0–10cm)(SD) from baseline to the end of week 2: acetyl-L-carnitine −1.32 (1.84); placebo −0.61 (1.55) p = 0.07. Consequently we undertook no further analysis of this trial.
Amitriptyline and Mexilitine
Two trials [38] and [39] that were included studied the efficacy of amitriptyline. Both trials compared amitriptyline to placebo and another intervention. One RCT [38] examined efficacy of amitriptyline as part of a trial also assessing acupuncture treatment. However despite being described as a parallel group, placebo controlled RCT, its design was complex. Consequently the results of this trial are difficult to evaluate. In particular bias may have been introduced because of unconventional randomisation procedures and because true placebo controls were not used. Specifically, patients were allowed to ‘opt-out’ of being randomised to the amitriptyline arms of the trial based on personal preference. In addition, many participants included in the analysis of amitriptyline efficacy, had also received acupuncture or sham acupuncture, further complicating analysis. Ignoring the methodological concerns, amitriptyline demonstrated no superiority to placebo in the primary outcome measure. The mean change in Gracely pain scores from baseline to week 14 was −0.26 with amitriptyline (maximum dose 75mg/day) and −0.30 with placebo. The difference between amitriptyline and placebo was: 0.00 95%CI(−0.18 to 0.19) p = 0.99.
The second trial [39] compared amitriptyline, mexilitine and placebo. This trial was terminated early following an interim review of results. It was deemed by the trial monitoring board that further enrolment into the study was unlikely to detect significant differences in either amitriptyline or mexilitine arms compared to placebo. No superiority was reported in reducing mean Gracely pain scores (SD) from baseline to the end of treatment week 8 for: amitriptyline (maximum dose 100mg/day) −0.31 (0.31); mexilitine −0.23 (0.41); compared to placebo −0.20 (0.30).
Smoked Cannabis
The original literature search found four articles related to cannabinoid use and painful HIV-SN. Only two were RCTs [40]–[41]. The excluded articles included one clinical survey [42] and one review article [43].
One of these included articles [41] was a cross-over study that compared the efficacy of smoked cannabis (maximum tolerated dose 1 to 8% Δ-9-tetrahydrocannabinol q.d.s.) to placebo cigarettes in reducing subjects pain measured using the Descriptor Differential Scale (DDS). The DDS is a ratio scale (0 to 20) containing 24 words describing pain intensity and unpleasantness. Smoked cannabis was reported to be superior to placebo in reducing DDS from baseline to end of treatment day five in the PP population. The median difference between cannabis and placebo was −3.3 out of 20; p = 0.016. No data were reported for the ITT analysis, however the authors stated that the PP analysis was similar to the ITT analysis with p = 0.02. VAS data not reported by the authors, but was supplied on request, relating to cannabis and placebo subjects who reported a ≥30% (18/34 and 7/34 respectively) and ≥50% (13/34 and 4/34 respectively) improvement in pain intensity.
This trial reported a high proportion of inadvertent unblinding amongst subjects following dose titration with smoked cannabis cigarettes in the treatment arms, but not with placebo cigarettes.
A second study [40] compared smoked cannabis (3.56% Δ-9-tetrahydrocannabinol t.d.s.) to placebo cigarettes in a parallel group RCT. Smoked cannabis was shown to be superior to placebo in reducing pain from baseline to end of treatment day 5 in the ITT analysis: cannabis −34% (IQR −71 to −16), placebo −17% (IQR −29 to 8) p = 0.03. More subjects reported ≥30% VAS improvement with smoked cannabis compared to the placebo: 13/27 and 6/27 respectively.
Inclusion into the study required subjects to have had previous exposure to cannabis, with current users asked to discontinue prior to the study. Of note no attempt was made to assess unintentional unblinding during the course of the study, which may have been high due to subjects' previous experience with smoked cannabis.
Using the ITT analysis dichotomous VAS data from both trials, an NNT for smoked cannabis was calculated as 3.38 95%CI (2.19 to 7.50) (Table 3)
Table 3. Summary of RCTs which demonstrated treatment superior to placebo, for which Relative Risk and Number Needed to Treat values could be calculated.
| Active Treatment (maximum tested dose) | Number of patient Episodes | Benefit Efficacy on Treatment (≥30% improvement VAS | Efficacy on Placebo (≥30% improvement VAS) | RR (95% CI) | NNT (95% CI) | |
| Smoked cannabis | ||||||
| Abrams et al 2007 [40] | Smoked cannabis: 3.56% Δ-9-tetrahydrocannabinol | 55 (50) | 13/27 | 6/28 | 2.17 (0.97 to 4.86) | 3.86 (1.98 to 71.11) |
| Ellis et al 2009 [41] | Smoked cannabis: 8% Δ-9-tetrahydrocannabinol | 68 (56) | 18/34 | 7/34 | 2.57 (1.24 to 5.35) | 3.09 (1.98 to 9.30) |
| Abrams et al [40]+Ellis et al [41] | Combined smoked cannabis studies | 122 (106) | 31/61 | 15/61 | 2.38 (1.38 to 4.10) | 3.38 (2.19 to 7.50) |
Topical Capsaicin
Four trials [44] [29] [28] and [45] were found that assessed topical capsaicin efficacy in painful HIV-SN. Two reports were excluded from further analysis; one was an open-label study [28] and the other has been reported in abstract form only [45]. Of the included trials, one [29] examined the efficacy of topical capsaicin 0.075% cream in a parallel group RCT. The authors stated that no superiority of capsaicin 0.075% over placebo in mean improvement in a numeric rating score (NRS) (0–10) was seen, however only graphical data were presented.
A second study [28] examined topical capsaicin 8%. Patients received either the 8% patch or an active placebo (capsaicin 0.04%) in a single application lasting either 30, 60 or 90 minutes. Following this single application patients were followed-up for 12 weeks. Capsaicin 8% was found to be superior to placebo in the percentage reduction of the NPRS (SD) from baseline to week 2 to 12: 8% capsaicin: −22.8 (30.6); compared to placebo: −10.7 (30.8), (p = 0.0026). The study also reported responder rates as percentage of patients measured on the NPRS who experienced ≥30% mean reduction in pain: capsaicin 8%: 76/225; placebo (capsaicin 0.04%): 15/82; p = 0.0092. It is not possible to calculate an NNT that is strictly comparable to those calculated for other studies included in this review since the placebo control used here was not pharmacologically inactive. However, as an informative exercise using these data, and presuming that the control capsaicin 0.04% is a true placebo, an NNT of 6.46 95%CI(3.86–19.69) was calculated for treatment with capsaicin 8% patch.
Gabapentin
Only one retrieved report related to treatment of painful HIV-SN with gabapentin was an RCT. Four additional articles were excluded. Two were letters [46]–[47] one an abstract [48], and one a case series [49]. The included study [30] compared gabapentin (titrated to a maximum of 2400mg/day) to placebo in a parallel group RCT. At the longest treatment period assessed, no difference in efficacy was reported between gabapentin and placebo groups for the primary outcome measure, median change in VAS (0–100mm) baseline to end of week 4: gabapentin: −44.1, placebo: −29.8. No indication of variance or p value was documented.
It is noteworthy that this trial demonstrated an unusual placebo response. The placebo subjects' pain VAS baseline remained unchanged for the first two weeks, after which a stronger placebo response followed to week 4. This unusual placebo response may have contributed to the apparent superiority of gabapentin over placebo at week 2, which was not evident at week 4.
Pregabalin
One large multi-centre RCT [50] examined the efficacy of pregabalin, titrated over 2 weeks to a maximum tolerated dose up to 1200mg/day, in a multicentre, 14 week parallel group, placebo controlled RCT. No superiority of pregabalin over placebo in the primary pain outcome measure was reported: mean change in NPRS baseline to end of week 14: pregabalin −2.88; placebo −2.63, p = 0.39.
Lamotrigine
Three trials assessing the efficacy of lamotrigine in painful HIV-SN were identified [51], [52] and [29], [31]). One trial [52], enrolled only one painful HIV-SN patient (to the placebo control group) and was therefore excluded from further analysis. The included lamotrigine trials [51] and [31] were both conducted by the same group; with [51] being smaller and preceding [31]. The smaller study [51] did demonstrate some efficacy superior to placebo when the primary outcome for the PP population was analysed. However in the ITT analysis with ‘last value carried forward’ (LVCF), lamotrigine was not superior to placebo: improvement in mean Gracely pain score (SE): lamotrigine: −0.242 (0.009); placebo: −0.183 (0.087); (p = 0.65). The large number of drop-outs in the lamotrigine group (n = 11 of 20) compared to placebo (n = 3 of 22) suggest a narrow therapeutic index and make interpretation of the trial results difficult.
Similarly the larger trial [31], where participants were stratified according to previous exposure to neurotoxic ARVs, did not demonstrate a superiority of lamotrigine over placebo for the primary outcome measure (mean improvement in Gracely pain score) in the total cohort or in either stratum. However lamotrigine did show superiority to placebo in the neurotoxic ARV-exposed stratum in a secondary outcome measure, mean improvement in VAS (0–100mm) baseline to end of treatment: lamotrigine: −27.1; compared to placebo: −9.0; p = 0.003.
For each stratum the number of responders (≥30% improvement in VAS) were calculated from the published data. For the neurotoxic ARV stratum: lamotrigine 36/62, placebo 7/30 (p = 0.02) and for no exposure to neurotoxic ART: lamotrigine 46/88, placebo 21/47. As an informative exercise using these data the NNT for lamotrigine was calculated for each stratum, and for the overall trial. Subjects with exposure to neurotoxic ARVs: 2.88 95%CI(1.84 to 6.57); no exposure to neurotoxic ARVs: 13.17 95%CI(3.96 to −9.95) and for the unstratified population: 6.09 95%CI(3.51 to 23.08)(Not included in Table 3 as no superiority of lamotrigine over placebo was demonstrated for any primary endpoint).
NGF
One RCT [53] examined the efficacy of subcutaneous recombinant human Nerve Growth Factor (rhNGF) in the treatment of painful HIV-SN. This study assessed two doses (0.1 and 0.3µg/kg) given twice weekly compared with placebo for 18 weeks. rhNGF was superior to placebo for the primary outcome measure in the ITT analysis; median change of the Gracely pain score from baseline to end of week 18: rhNGF 0.1µg/kg: −0.18 (−0.10 to −0.25) p = 0.05, 0.3µg/kg: −0.21 (−0.14 to −0.29) p = 0.04, and placebo: 0.06 (+0.01 to −0.14).
No significant dose effect was reported and no differential effect was seen based on baseline stratification of subjects according to neurotoxic ARV drug exposure. As rhNGF was reported to be associated with myalgia, there may have been inadvertent breaking of the blinding.
Dichotomous data were requested from the authors however we were unable to calculate RR and NNT values for rhNGF from the data provided.
Prosaptide and Peptide –T
Two trials [54], [55] examined the efficacy of the novel agents in placebo controlled parallel group RCTs. One [55] reported the use of subcutaneous prosaptide (maximum dose of 16mg/day) over 6 treatment weeks and did not report efficacy superior to placebo in the primary outcome measure; mean change in Gracely pain score baseline to week 6. The study was terminated after a planned interim futility analysis. Another trial [54] studied efficacy of intranasal peptide T (maximum dose 6mg/day), over 12 treatment weeks, but reported no superiority over placebo in the primary outcome measure; mean change in a modified Gracely pain score baseline to end of week 12.
Discussion
This systematic review found that RCT evidence of analgesic efficacy superior to placebo in the context of HIV-SN pain exists only for smoked cannabis, rhNGF and high dose (8%) topical capsaicin. Several other agents have been examined in high quality RCTs and found to be no more effective than placebo for managing HIV-SN pain in the doses examined, specifically acetyl-L carnitine (1g/day), amitriptyline (100mg/day), topical capsaicin 0.075%, gabapentin (2.4g/day), mexilitine (600mg/day), peptide –T (6mg/day), pregabalin(1200mg/day), lamotrigine (600mg/day) and prosaptide (16mg/day). Therefore, there is evidence that both of the first line therapies (pregabalin and amitriptyline) recommended in the NICE guidance for non-specialist management of neuropathic pain show no superiority to placebo in the management of pain in HIV-SN [20].
Of the pharmacological interventions shown to be effective for HIV-SN in RCTs, only topical capsaicin 8% is currently approved for marketing for neuropathic pain indications. In Europe 8% capsaicin has been approved for the treatment of peripheral neuropathic pain in non-diabetic adults, whilst the U.S. Food and Drug Administration (FDA) has approved its use only for the indication of post herpetic neuralgia. However, it should also be borne in mind that we located a preliminary report (conference abstract only and therefore excluded from the systematic review) of another parallel group RCT which included 494 patients with HIV-SN in which topical 8% capsaicin was compared to 0.04% topical capsaicin [45]. No analgesic superiority of 8% capsaicin over 0.04% was demonstrated. rhNGF therapy is not currently clinically available and both legal and mental health issues preclude routine recommendation of long term smoked cannabis for pain management [56].
This systematic review represents a comprehensive review of the literature relating to the pharmacological management of painful HIV-SN. It used a predefined protocol for the initial literature search, data extraction and analysis. There was also strict adherence to inclusion quality criteria as assessed by four independent authors using the modified Jadad score, a tool that assesses each study for potential bias as well as evaluating study power.
This systematic review was limited by the paucity of high quality RCTs examining pharmacological treatment of painful HIV-SN. Additionally the heterogeneity of the included studies design and size made evaluation and comparison of trials difficult. In particular, use of the Gracely pain scale (GPS) in five of the 15 included RCTs made evaluation and inter-study comparison complicated. The GPS is a log unit pain outcome measure that is not a frequently used measure outside trials of HIV-SN. In a recent consensus statement regarding core chronic pain outcome measures [57] it was not one of the recommended pain scales. Several of the studies utilising the Gracely pain score also included more validated secondary pain outcome measures such as either a VAS score or a NPRS. These were used here in preference to the Gracely pain score in the calculation of NNT and RR.
The Jadad tool has been validated and used widely to identify common and major sources of experimental bias in RCTs identified in systematic reviews. Nevertheless, whilst the use of the modified Jadad score improves the probability that only high quality RCTs were included in the systematic review, its use may conceivably have biased our systematic review in favour of more recently tested agents. The RCTs associated with these agents now routinely report the information required by the modified Jadad tool, because of the nature of the evolution of RCT methodology over the past few years.
Both of the RCTs that examined the efficacy of smoked cannabis, were of high quality, however the apparent marked superiority of smoked cannabis to placebo cigarettes should be tempered by the high proportion of potential unblinding measured in [41] (92% correctly guessing treatment allocation after treatment crossover), and its lack of measurement in [40] despite participants having all had previous experience of smoked cannabis. In a similar manner, the RCT investigating recombinant human NGF demonstrated a high degree of unblinding related to injection site myalgia, which when accounted for in a separate analysis reported a more attenuated treatment-related difference which consequently lost statistical significance.
Lamotrigine was the subject of two high quality RCTs. Both failed to show superiority over placebo in the primary pain outcome measure, improvement in the GPS in the ITT population. However, in the larger of the two RCTs, analysis of a secondary pain outcome measure, mean improvement in VAS, did demonstrate efficacy superior to placebo in the subpopulation of subjects who had been previously exposed to neurotoxic ARTs. If this stratum alone is examined an NNT of 2.88 is calculated.
Most of the included RCTs did not stratify subjects with painful HIV-SN according to their exposure to neurotoxic ARTs. This stratification was instrumental in demonstrating an efficacy of lamotrigine in neurotoxic ART exposed painful HIV-SN subjects. It is possible to speculate that a similar strategy of stratifying other RCTs might have elucidated other agents with sub-group efficacy, despite lack of observed analgesic efficacy in an unstratified painful HIV-SN subject population. Additionally, the included RCTs were not uniform in their approach to the use of concomitant analgesics; whilst most allowed continued use of drugs at stable doses, two elected to stop them [30] [58]. The use of such concomitant analgesics, and also the inclusion of participants with previously failed therapies, may conceivably have influenced the outcomes of these RCTs.
Gabapentin and pregabalin were the subject of two high quality RCTs in which neither agent was shown to be superior to placebo. This contrasts with the efficacy of these agents demonstrated in other peripheral neuropathic pain conditions [20] [59] [18], [19]. However the gabapentin study was small, with only 30 patients randomised [30]. This finding may therefore represent a ‘failed trial’ rather than a true lack of efficacy.
Amitriptyline efficacy was examined in two large RCTs. The evaluation of one study [38] was made difficult by a complicated study design that may have not been truly randomised or placebo controlled. However the finding that amitriptyline did not display superior analgesic efficacy than placebo in the context of HIV-SN is supported by a similar finding a second, higher quality RCT [39]. Again, this finding directly contrasts with evidence of efficacy for tricyclic antidepressants in a range of other peripheral neuropathic pain conditions [20] [59] [19] [18].
Capsaicin 0.075% cream was the subject of a small RCT enrolling only 26 subjects. The authors stated that capsaicin 0.075% did not demonstrate statistically significant superiority to placebo in the primary pain outcome measure. However, outcome data were published only in a graphical representation of mean current pain scores from baseline to the end of treatment. From this graph there does appear to be a trend for capsaicin to be superior to placebo at this final time point measured at week 4. However a high drop-out rate in both arms resulted in only 6/11 patients remaining in the capsaicin group, and only 8/15 in the placebo group. It is therefore difficult to determine from this study if capsaicin 0.075% was indeed without efficacy. This has two implications: the first being that capsaicin 0.075% might have some degree of clinically relevant efficacy in painful HIV-SN; and secondly, if capsaicin 0.075% is indeed efficacious, then the use of a similar concentration (capsaicin 0.04%) as an active placebo in the large capsaicin 8% patch RCT would change the design of this study from a placebo controlled to a superiority approach.
In the treatment of painful HIV-SN, the lack of efficacy compared with placebo of many agents with proven efficacy in other forms of neuropathic pain has implications in the understanding of neuropathic pain in general. These findings further support the hypothesis that neuropathic pain cannot be considered as a single symptom with a single pathogenesis [21], [22]. A more mechanistic approach to the treatment of specific types of neuropathic pain is therefore warranted as has been established in trigeminal neuralgia and post herpetic neuralgia. Equally, caution should be exercised in the use of neuropathic pain treatment algorithms that do not consider these potential mechanistic differences, as their rationale may be fundamentally flawed.
The absence of studies examining the efficacy of opioid use in painful HIV-SN is notable and mandates additional research. Opioids have shown efficacy in other neuropathic pain conditions [18] [59] [19]. Furthermore, the efficacy of duloxetine in diabetic neuropathy, a condition that has similarities to HIV-SN, may suggest that it is worth investigating [20]. In addition, the efficacy of cannabis in HIV-SN would suggest that cannabinoids with an appropriate therapeutic index when delivered by a mechanism other than smoking might be worthy of investigation [56].
Conclusions
On the basis of current published evidence, topical capsaicin 8%, smoked cannabis and Nerve Growth Factor have evidence of efficacy in pain associated with HIV-SN. However this is potentially contentious, as a recent larger RCT, currently reported in abstract form only, has suggested this treatment is not superior to placebo [45]. Some commonly recommended analgesics, including opioids, have not been formally studied for the management of painful HIV-SN.
The current evidence base available for the treatment of painful HIV-SN is at odds with the recommendations made by NICE for neuropathic pain management in the non-specialist situation. This indicates the potential dangers of extrapolating efficacy from one neuropathic pain condition to another where efficacy has not been directly assessed. In particular amitriptyline, pregabalin, and gabapentin have been demonstrated to have no superiority to placebo in the treatment of painful HIV-SN.
With an estimated 33 million people living with HIV and more gaining access to ARV every day, the management of HIV-SN associated neuropathic pain is a problem of major global significance. There is an urgent need for the development of effective, evidence based analgesic strategies for this common condition. Gene microarrays have been used to identify novel drug targets [60]. Ongoing evaluation of both novel analgesics and existing untested strategies for HIV-SN is a clear research priority.
Footnotes
Competing Interests: ASCR has received fees and associated expenses for research-related consultancy services contracted via Imperial College Consultants from Pfizer, Eisai, Solvay, Spinifex, Organon, Lectus Astellas, Allergan, GSK, NeuroGsx, Esteve and Daiichi Sankyo. ASCR is a member of the EU funded Innovative Medicines Initiative grant “Europain” in which a number of pharmaceutical companies are also participating: Astra-Zeneca, Esteve, Boehinger-Ingelheim, Pfizer, Eli Lilly, GlaxoSmithKline, Wyeth, UCB and Sanofi Aventis. ASCR has also received a research grant from Pfizer; CLC has had investigator initiated research grants from GlaxoSmithKline, Roche Australia and Zymes LLC; CLC is also on the advisory boards of Gilead Science and BMS Australia Virology, honoraria for both have been donated to charity. CLC undertakes consultancy work and is a principle investigator on two clinical studies for CNS Bio; TJCP, SM and SC have no financial interests that may be relevant to the submitted work. This does not alter the authors' adherence to all the PLoS ONE policies on sharing data and materials.
Funding: The investigator TJCP was funded by a grant from The Derek Butler Trust (UK Reg Charity 1081995). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Smyth K, Affandi JS, McArthur JC, Bowtell-Harris C, Mijch AM, et al. Prevalence of and risk factors for HIV-associated neuropathy in Melbourne, Australia 1993–2006. HIV Med. 2007;8:367–373. doi: 10.1111/j.1468-1293.2007.00478.x. [DOI] [PubMed] [Google Scholar]
- 2.Lipkin WI, Parry G, Kiprov D, Abrams D. Inflammatory neuropathy in homosexual men with lymphadenopathy. Neurology. 1985;35:1479–1483. doi: 10.1212/wnl.35.10.1479. [DOI] [PubMed] [Google Scholar]
- 3.Barohn R, Gronseth G, Leforce B, McVey A, McGuire A, et al. Peripheral nerve involvement in a large cohort of human immunodeficiency virus-infected individuals. Arch Neurol. 1993;50:167–171. doi: 10.1001/archneur.1993.00540020045016. [DOI] [PubMed] [Google Scholar]
- 4.Blum AS, Dal Pan GJ, Feinberg J, Raines C, Mayjo K, et al. Low-dose zalcitabine-related toxic neuropathy: frequency, natural history, and risk factors. Neurology. 1996;46:999–1003. doi: 10.1212/wnl.46.4.999. [DOI] [PubMed] [Google Scholar]
- 5.Yarchoan R, Perno CF, Thomas RV, Klecker RW, Allain JP, et al. Phase I studies of 2′,3′-dideoxycytidine in severe human immunodeficiency virus infection as a single agent and alternating with zidovudine (AZT). Lancet. 1988;1:76–81. doi: 10.1016/s0140-6736(88)90283-8. [DOI] [PubMed] [Google Scholar]
- 6.Mocroft A, Ledergerber B, Katlama C, Kirk O, Reiss P, et al. Decline in the AIDS and death rates in the EuroSIDA study: an observational study. Lancet. 2003;362:22–29. doi: 10.1016/s0140-6736(03)13802-0. [DOI] [PubMed] [Google Scholar]
- 8.Lohse N, Hansen AB, Pedersen G, Kronborg G, Gerstoft J, et al. Survival of persons with and without HIV infection in Denmark, 1995–2005. Ann Intern Med. 2007;146:87–95. doi: 10.7326/0003-4819-146-2-200701160-00003. [DOI] [PubMed] [Google Scholar]
- 9.Bacellar H, Muñoz A, Miller EN, Cohen BA, Besley D, et al. Temporal trends in the incidence of HIV-1-related neurologic diseases: Multicenter AIDS Cohort Study, 1985–1992. Neurology. 1994;44:1892–1900. doi: 10.1212/wnl.44.10.1892. [DOI] [PubMed] [Google Scholar]
- 10.Wright E, Brew B, Arayawichanont A, Robertson K, Samintharapanya K, et al. Neurologic disorders are prevalent in HIV-positive outpatients in the Asia-Pacific region. Neurology. 2008;71:50–56. doi: 10.1212/01.wnl.0000316390.17248.65. [DOI] [PubMed] [Google Scholar]
- 11.Konchalard K, Wangphonpattanasiri K. Clinical and electrophysiologic evaluation of peripheral neuropathy in a group of HIV-infected patients in Thailand. J Med Assoc Thai. 2007;90:774–781. [PubMed] [Google Scholar]
- 12.Lichtenstein KA, Armon C, Baron A, Moorman AC, Wood KC, et al. Modification of the incidence of drug-associated symmetrical peripheral neuropathy by host and disease factors in the HIV outpatient study cohort. Clin Infect Dis. 2005;40:148–157. doi: 10.1086/426076. [DOI] [PubMed] [Google Scholar]
- 13.Morgello S, Estanislao L, Simpson D, Geraci A, DiRocco A, et al. HIV-associated distal sensory polyneuropathy in the era of highly active antiretroviral therapy: the Manhattan HIV Brain Bank. Arch Neurol. 2004;61:546–551. doi: 10.1001/archneur.61.4.546. [DOI] [PubMed] [Google Scholar]
- 14.Simpson DM, Kitch D, Evans SR, McArthur JC, Asmuth DM, et al. HIV neuropathy natural history cohort study: assessment measures and risk factors. Neurology. 2006;66:1679–1687. doi: 10.1212/01.wnl.0000218303.48113.5d. [DOI] [PubMed] [Google Scholar]
- 15.UNAIDS JUNPOH. AIDS epidemic update, December 2009. 2009. AIDS epidemic update, December 2009. www.unaids.org.
- 16.Maritz J, Benatar M, Dave JA, Harrison TB, Badri M, et al. HIV neuropathy in South Africans: frequency, characteristics, and risk factors. Muscle Nerve. 2010;41:599–606. doi: 10.1002/mus.21535. [DOI] [PubMed] [Google Scholar]
- 17.Ellis RJ, Rosario D, Clifford DB, McArthur JC, Simpson D, et al. Continued high prevalence and adverse clinical impact of human immunodeficiency virus-associated sensory neuropathy in the era of combination antiretroviral therapy: the CHARTER Study. Arch Neurol. 2010;67:552–558. doi: 10.1001/archneurol.2010.76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finnerup NB, Sindrup SH, Jensen TS. The evidence for pharmacological treatment of neuropathic pain. Pain. 2010;150:573–581. doi: 10.1016/j.pain.2010.06.019. [DOI] [PubMed] [Google Scholar]
- 19.Dworkin RH, O'Connor AB, Backonja M, Farrar JT, Finnerup NB, et al. Pharmacologic management of neuropathic pain: evidence-based recommendations. Pain. 2007;132:237–251. doi: 10.1016/j.pain.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 20.Tan T, Barry P, Reken S, Baker M Guideline Development Group. Pharmacological management of neuropathic pain in non-specialist settings: summary of NICE guidance. BMJ. 2010;340:c1079. doi: 10.1136/bmj.c1079. [DOI] [PubMed] [Google Scholar]
- 21.Baron R, Tölle TR, Gockel U, Brosz M, Freynhagen R. A cross-sectional cohort survey in 2100 patients with painful diabetic neuropathy and postherpetic neuralgia: Differences in demographic data and sensory symptoms. Pain. 2009;146:34–40. doi: 10.1016/j.pain.2009.06.001. [DOI] [PubMed] [Google Scholar]
- 22.Scholz J, Mannion RJ, Hord DE, Griffin RS, Rawal B, et al. A novel tool for the assessment of pain: validation in low back pain. PLoS Med. 2009;6:e1000047. doi: 10.1371/journal.pmed.1000047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009;6:e1000100. doi: 10.1371/journal.pmed.1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rice ASC, Lever IJ, Zarnegar R. Cannabinoids and analgesia, with special reference to neuropathic pain. In: McQuay HJ, Kalso E, Moore RA, editors. Reviews and Meta-Analyses in Pain. Seattle: IASP Press; 2008. 233 [Google Scholar]
- 25.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 26.Armitage P, Berry G. Statistical methods in medical research. Oxford: Blackwell Scientific Publications; 1990. [Google Scholar]
- 27.L'Abbé KA, Detsky AS, O'Rourke K. Meta-analysis in clinical research. Ann Intern Med. 1987;107:224–233. doi: 10.7326/0003-4819-107-2-224. [DOI] [PubMed] [Google Scholar]
- 28.Simpson DM, Brown S, Tobias J NGX-4010 C107 Study Group. Controlled trial of high-concentration capsaicin patch for treatment of painful HIV neuropathy. Neurology. 2008;70:2305–2313. doi: 10.1212/01.wnl.0000314647.35825.9c. [DOI] [PubMed] [Google Scholar]
- 29.Paice JA, Ferrans CE, Lashley FR, Shott S, Vizgirda V, et al. Topical capsaicin in the management of HIV-associated peripheral neuropathy. J Pain Symptom Manage. 2000;19:45–52. doi: 10.1016/s0885-3924(99)00139-6. [DOI] [PubMed] [Google Scholar]
- 30.Hahn K, Arendt G, Braun JS, von Giesen HJ, Husstedt IW, et al. A placebo-controlled trial of gabapentin for painful HIV-associated sensory neuropathies. J Neurol. 2004;251:1260–1266. doi: 10.1007/s00415-004-0529-6. [DOI] [PubMed] [Google Scholar]
- 31.Simpson DM, McArthur JC, Olney R, Clifford D, So Y, et al. Lamotrigine for HIV-associated painful sensory neuropathies: a placebo-controlled trial. Neurology. 2003;60:1508–1514. doi: 10.1212/01.wnl.0000063304.88470.d9. [DOI] [PubMed] [Google Scholar]
- 32.Hart AM, Wilson AD, Montovani C, Smith C, Johnson M, et al. Acetyl-l-carnitine: a pathogenesis based treatment for HIV-associated antiretroviral toxic neuropathy. AIDS. 2004;18:1549–1560. doi: 10.1097/01.aids.0000131354.14408.fb. [DOI] [PubMed] [Google Scholar]
- 33.Osio M, Muscia F, Zampini L, Nascimbene C, Mailland E, et al. Acetyl-l-carnitine in the treatment of painful antiretroviral toxic neuropathy in human immunodeficiency virus patients: an open label study. J Peripher Nerv Syst. 2006;11:72–76. doi: 10.1111/j.1085-9489.2006.00066.x. [DOI] [PubMed] [Google Scholar]
- 34.Scarpini E, Sacilotto G, Baron P, Cusini M, Scarlato G. Effect of acetyl-L-carnitine in the treatment of painful peripheral neuropathies in HIV+ patients. J Peripher Nerv Syst. 1997;2:250–252. [PubMed] [Google Scholar]
- 35.Herzmann C, Johnson MA, Youle M. Long-term effect of acetyl-L-carnitine for antiretroviral toxic neuropathy. HIV Clin Trials. 2005;6:344–350. doi: 10.1310/CH1N-YBNU-G3CU-JBXR. [DOI] [PubMed] [Google Scholar]
- 36.Youle M, Osio M ALCAR Study Group. A double-blind, parallel-group, placebo-controlled, multicentre study of acetyl L-carnitine in the symptomatic treatment of antiretroviral toxic neuropathy in patients with HIV-1 infection. HIV Med. 2007;8:241–250. doi: 10.1111/j.1468-1293.2007.00467.x. [DOI] [PubMed] [Google Scholar]
- 37.Chiechio S, Copani A, Gereau RW, Nicoletti F. Acetyl-L-carnitine in neuropathic pain: experimental data. CNS Drugs. 2007;21(Suppl 1):31–8; discussion 45–6. doi: 10.2165/00023210-200721001-00005. [DOI] [PubMed] [Google Scholar]
- 38.Shlay JC, Chaloner K, Max MB, Flaws B, Reichelderfer P, et al. Acupuncture and amitriptyline for pain due to HIV-related peripheral neuropathy: a randomized controlled trial. Terry Beirn Community Programs for Clinical Research on AIDS. JAMA. 1998;280:1590–1595. doi: 10.1001/jama.280.18.1590. [DOI] [PubMed] [Google Scholar]
- 39.Kieburtz K, Simpson D, Yiannoutsos C, Max MB, Hall CD, et al. A randomized trial of amitriptyline and mexiletine for painful neuropathy in HIV infection. AIDS Clinical Trial Group 242 Protocol Team. Neurology. 1998;51:1682–1688. doi: 10.1212/wnl.51.6.1682. [DOI] [PubMed] [Google Scholar]
- 40.Abrams DI, Jay CA, Shade SB, Vizoso H, Reda H, et al. Cannabis in painful HIV-associated sensory neuropathy: a randomized placebo-controlled trial. Neurology. 2007;68:515–521. doi: 10.1212/01.wnl.0000253187.66183.9c. [DOI] [PubMed] [Google Scholar]
- 41.Ellis RJ, Toperoff W, Vaida F, van den Brande G, Gonzales J, et al. Smoked medicinal cannabis for neuropathic pain in HIV: a randomized, crossover clinical trial. Neuropsychopharmacology. 2009;34:672–680. doi: 10.1038/npp.2008.120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Woolridge E, Barton S, Samuel J, Osorio J, Dougherty A, et al. Cannabis use in HIV for pain and other medical symptoms. J Pain Symptom Manage. 2005;29:358–367. doi: 10.1016/j.jpainsymman.2004.07.011. [DOI] [PubMed] [Google Scholar]
- 43.Beaulieu P, Ware M. Reassessment of the role of cannabinoids in the management of pain. Curr Opin Anaesthesiol. 2007;20:473–477. doi: 10.1097/ACO.0b013e3282efd175. [DOI] [PubMed] [Google Scholar]
- 44.Simpson DM, Estanislao L, Brown SJ, Sampson J. An open-label pilot study of high-concentration capsaicin patch in painful HIV neuropathy. J Pain Symptom Manage. 2008;35:299–306. doi: 10.1016/j.jpainsymman.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 45.Clifford D, Simpson D, Brown S, Moyle G, Brew B, et al. A multicenter, randomized, double-blind, controlled study of NGX-4010 (Qutenza®), a high concentration capsaicin patch for the treatment of HIV-associated distal sensory polyneuropathy. 2010. 17th Conference on Retroviruses and Opportunistic Infections Feb 16–19th 2010 Abstract #411 – accessible at www.retroconference.org/2010/Abstracts/37371.htm.
- 46.Valdivelu N. Neuropathic pain after anti-HIV gene therapy successfully treated with gabapentin. J Pain Symptom Manage. 1999;1999 Mar;17(3):155–6. 1999 Mar: 155–156. doi: 10.1016/s0885-3924(98)00154-7. [DOI] [PubMed] [Google Scholar]
- 47.Newshan G. HIV neuropathy treated with gabapentin. (letter). AIDS. 1998;12:219–221. [PubMed] [Google Scholar]
- 48.Gatti, Antonella; Jann, Stefano; Sandro, et al. Gabapentin in the Treatment of Distal Symmetric Axonopathy in HIV Infected Patients.[Abstract]. Neurology. 1998;50:A216. [Google Scholar]
- 49.La Spina I, Porazzi D, Maggiolo F, Bottura P, Suter F. Gabapentin in painful HIV-related neuropathy: a report of 19 patients, preliminary observations. Eur J Neurol. 2001;8:71–75. doi: 10.1046/j.1468-1331.2001.00157.x. [DOI] [PubMed] [Google Scholar]
- 50.Simpson DM, Schifitto G, Clifford DB, Murphy TK, Durso-De Cruz E, et al. Pregabalin for painful HIV neuropathy: a randomized, double-blind, placebo-controlled trial. Neurology. 2010;74:413–420. doi: 10.1212/WNL.0b013e3181ccc6ef. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Simpson DM, Olney R, McArthur JC, Khan A, Godbold J, et al. A placebo-controlled trial of lamotrigine for painful HIV-associated neuropathy. Neurology. 2000;54:2115–2119. doi: 10.1212/wnl.54.11.2115. [DOI] [PubMed] [Google Scholar]
- 52.Silver M, Blum D, Grainger J, Hammer AE, Quessy S. Double-blind, placebo-controlled trial of lamotrigine in combination with other medications for neuropathic pain. J Pain Symptom Manage. 2007;34:446–454. doi: 10.1016/j.jpainsymman.2006.12.015. [DOI] [PubMed] [Google Scholar]
- 53.McArthur JC, Yiannoutsos C, Simpson DM, Adornato BT, Singer EJ, et al. A phase II trial of nerve growth factor for sensory neuropathy associated with HIV infection. AIDS Clinical Trials Group Team 291. Neurology. 2000;54:1080–1088. doi: 10.1212/wnl.54.5.1080. [DOI] [PubMed] [Google Scholar]
- 54.Simpson DM, Dorfman D, Olney RK, McKinley G, Dobkin J, et al. Peptide T in the treatment of painful distal neuropathy associated with AIDS: results of a placebo-controlled trial. The Peptide T Neuropathy Study Group. Neurology. 1996;47:1254–1259. doi: 10.1212/wnl.47.5.1254. [DOI] [PubMed] [Google Scholar]
- 55.Evans SR, Simpson DM, Kitch DW, King A, Clifford DB, et al. A randomized trial evaluating Prosaptide for HIV-associated sensory neuropathies: use of an electronic diary to record neuropathic pain. PLoS ONE. 2007;2:e551. doi: 10.1371/journal.pone.0000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rice AS. Should cannabinoids be used as analgesics for neuropathic pain? Nat Clin Pract Neurol. 2008;4:654–655. doi: 10.1038/ncpneuro0949. [DOI] [PubMed] [Google Scholar]
- 57.Dworkin RH, Katz J, Gitlin MJ. Placebo response in clinical trials of depression and its implications for research on chronic neuropathic pain. Neurology. 2005;65:S7–19. doi: 10.1212/wnl.65.12_suppl_4.s7. [DOI] [PubMed] [Google Scholar]
- 58.Evans SR, Simpson DM, Kitch DW, King A, Clifford DB, et al. A randomized trial evaluating Prosaptide for HIV-associated sensory neuropathies: use of an electronic diary to record neuropathic pain. PLoS ONE. 2007;2:e551. doi: 10.1371/journal.pone.0000551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hempenstall K, Nurmikko TJ, Johnson RW, A'Hern RP, Rice AS. Analgesic therapy in postherpetic neuralgia: a quantitative systematic review. PLoS Med. 2005;2:e164. doi: 10.1371/journal.pmed.0020164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maratou K, Wallace VC, Hasnie FS, Okuse K, Hosseini R, et al. Comparison of dorsal root ganglion gene expression in rat models of traumatic and HIV-associated neuropathic pain. Eur J Pain. 2009;13:387–398. doi: 10.1016/j.ejpain.2008.05.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Youle M. Acetyl-L-carnitine in HIV-associated antiretroviral toxic neuropathy. CNS Drugs. 2007;21(Suppl 1):25–30; discussion 45–6. doi: 10.2165/00023210-200721001-00004. [DOI] [PubMed] [Google Scholar]
- 62.Wiffen PJ, Rees J. Lamotrigine for acute and chronic pain. Cochrane Database Syst Rev. 2007:CD006044. doi: 10.1002/14651858.CD006044.pub2. [DOI] [PubMed] [Google Scholar]
- 63.Saarto T, Wiffen PJ. Antidepressants for neuropathic pain. Cochrane Database Syst Rev. 2007:CD005454. doi: 10.1002/14651858.CD005454.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Liu JP, Manheimer E, Yang M. Herbal medicines for treating HIV infection and AIDS. Cochrane Database Syst Rev. 2005:CD003937. doi: 10.1002/14651858.CD003937.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schifitto G, Yiannoutsos C, Simpson DM, Adornato BT, Singer EJ, et al. Long-term treatment with recombinant nerve growth factor for HIV-associated sensory neuropathy. Neurology. 2001;57:1313–1316. doi: 10.1212/wnl.57.7.1313. [DOI] [PubMed] [Google Scholar]
- 66.von Gunten CF, Eappen S, Cleary JF, Taylor SG, Moots P, et al. Flecainide for the treatment of chronic neuropathic pain: a Phase II trial. Palliat Med. 2007;21:667–672. doi: 10.1177/0269216307083031. [DOI] [PubMed] [Google Scholar]
- 67.Dorfman D, Dalton A, Khan A, Markarian Y, Scarano A, et al. Treatment of painful distal sensory polyneuropathy in HIV-infected patients with a topical agent: results of an open-label trial of 5% lidocaine gel. AIDS. 1999;13:1589–1590. doi: 10.1097/00002030-199908200-00025. [DOI] [PubMed] [Google Scholar]
- 68.King SA. Acupuncture and amitriptyline for HIV-related peripheral neuropathic pain. JAMA. 1999;281:1271–1272. [PubMed] [Google Scholar]
- 69.Ulett GA. Acupuncture and amitriptyline for HIV-related peripheral neuropathic pain. JAMA. 1999;281:1270–1; author reply 1271–2. [PubMed] [Google Scholar]
- 70.Kaptchuk TJ. Acupuncture and amitriptyline for HIV-related peripheral neuropathic pain. JAMA. 1999;281:1270; author reply 1271–1270; author reply 1272. [PubMed] [Google Scholar]
- 71.Bradley WG, Verma A. Painful vasculitic neuropathy in HIV-1 infection: relief of pain with prednisone therapy. Neurology. 1996;47:1446–1451. doi: 10.1212/wnl.47.6.1446. [DOI] [PubMed] [Google Scholar]
- 72.Phillips KD, Skelton WD, Hand GA. Effect of acupuncture administered in a group setting on pain and subjective peripheral neuropathy in persons with human immunodeficiency virus disease. J Altern Complement Med. 2004;10:449–455. doi: 10.1089/1075553041323678. [DOI] [PubMed] [Google Scholar]
- 73.Estanislao L, Carter K, McArthur J, Olney R, Simpson D Lidoderm-HIV Neuropathy Group. A randomized controlled trial of 5% lidocaine gel for HIV-associated distal symmetric polyneuropathy. J Acquir Immune Defic Syndr. 2004;37:1584–1586. doi: 10.1097/00126334-200412150-00010. [DOI] [PubMed] [Google Scholar]
- 74.Kemper CA, Kent G, Burton S, Deresinski SC. Mexiletine for HIV-infected patients with painful peripheral neuropathy: a double-blind, placebo-controlled, crossover treatment trial. J Acquir Immune Defic Syndr Hum Retrovirol. 1998;19:367–372. doi: 10.1097/00042560-199812010-00007. [DOI] [PubMed] [Google Scholar]
- 75.Schifitto G, Yiannoutsos CT, Simpson DM, Marra CM, Singer EJ, et al. A placebo-controlled study of memantine for the treatment of human immunodeficiency virus-associated sensory neuropathy. J Neurovirol. 2006;12:328–331. doi: 10.1080/13550280600873835. [DOI] [PubMed] [Google Scholar]