Abstract
Extrinsic oesophageal compression leading to dysphagia is a recognised but uncommon sole presentation of thoracic aortic aneurysms. This has been referred to as Dysphagia Aortica, and is a late presentation of large thoracic aneurysms, or a symptom of impending aorto-oesophageal fistula. We present the case of a 67 year old woman who presented repeatedly with dysphagia and weight loss over a 3 month period to specialists in three different disciplines. Eventually, a type II thoraco-abdominal aortic aneurysm causing extrinsic compression of the oesophagus was discovered. When dealing with patients who present with dysphagia, if no other cause is discovered, a thoracic aortic aneurysm should form part of the differential diagnosis, as this is potentially curable, and delays in diagnosis and treatment predispose to rupture and death.
Abstract
Dysphagie infolge äußerer Verengung des Ösophagus ist eine bekannte aber seltene Komplikation bei einem Aneurysma der thorakalen Aorta. Im weiteren Verlauf besteht die Gefahr einer drohenden Ruptur bzw. der aortoösophagealen Fistelbildung.
Wir präsentieren den Fall einer 67-jährigen Frau mit Gewichtsverlust und Dysphagie über drei Monate, die mehrere Spezialisten konsultierte und bei der schließlich eine Ösophagusstenose infolge eines thorakoabdominellen Aortenaneurymas Typ II diagnostiziert wurde.
Differenzialdiagnostisch sollte bei der Dysphagie, insbesondere wenn keine andere Ursache erhoben werden an, an ein thorakoabdominelles Aortenaneuryma gedacht werden, da diese Erkrankung potentiell korrigierbar ist und eine Verzögerung der Behandlung zur Ruptur führen kann.
Introduction
Thoracic aneurysms are usually asymptomatic. Typically they present with sudden onset of interscapular back pain, or central chest pain. Dysphagia as a result of oesophageal compression is an uncommon associated symptom. Other vascular causes of oesophageal compression are also rare, the commonest being dysphagia lusoria, where the oesophagus is compressed by an aberrant right subclavian artery [1].
We present the case of a 67 year old female patient, who presented repeatedly to various clinicians with increasingly severe dysphagia and weight loss as the only manifestation of a large thoracic aneurysm. She was dealt with by three different specialties, and despite multiple investigations, the aneurysm ruptured and the patient died.
Case presentation
A 67 year old woman presented to the emergency department complaining of worsening epigastric pain radiating to her back and dysphagia to solid foods over the previous two weeks. Her past medical history included hypertension, cerebro-vascular accident followed by a carotid endarterectomy, right femoro-popliteal bypass grafting and hysterectomy. Her vital signs were normal on admission. Clinical examination of her abdomen revealed tenderness on deep palpation of the epigastrium, with no other signs. An abdominal film and routine blood tests were all within normal results.
The signs and symptoms were felt to represent cholelithiasis. An ultrasound scan of her abdomen was requested, but this showed no abnormality. She was discharged following a brief admission, with colonoscopy and gastroscopy requested as an outpatient. These tests were both performed, and were both reported as normal. Her care was transferred from a surgical team to the gastroenterological team for further investigation of her dysphagia and weight loss.
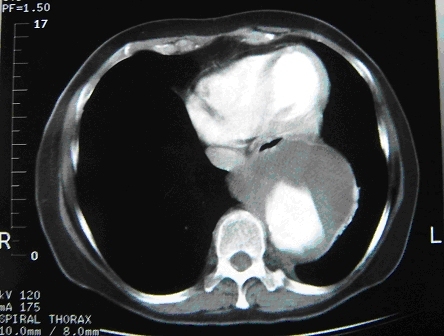
The patient’s symptoms persisted and worsened, with a weight loss of 20 kg in two months. She attended a medical outpatient clinic and was promptly admitted. She had a chest X-ray, an ultrasound scan, a barium enema, and two CT scans. The chest X-ray demonstrated a thoracic aneurysm, but the X-ray remained unreported. The second CT scan encompassed the thorax, and demonstrated a thoraco-abdominal aneurysm measuring 8.3 cm x 7.8 cm starting six centimetres above the diaphragm and ending at the origin of the coeliac axis (Figure 1 (Fig. 1)). There was no evidence of rupture. There was considerable compression and anterior displacement of the oesophagus. In the absence of other demonstrable pathology, this was clearly responsible for her symptoms.
Figure 1. Computerised tomogram showing anterior displacement and compression of the oesophagus by a large thoracic aortic aneurysm.
The patient remained haemodynamically stable, and was pain-free. She was discharged to attend a tertiary referral centre as an urgent outpatient, but unfortunately succumbed to rupture of the aneurysm soon after discharge.
Discussion
Oesophageal compression leading to dysphagia caused by a thoracic aortic aneurysm as a sole presentation is succinctly described in case reports and whose incidence is unknown to date. The presenting signs and symptoms can be very vague as the majority are asymtomatic. Expanding aneurysms can present with interscapular pain or central, ripping chest pain and dyspnoea. Atypical presentations of a thoracic aneurysm include hoarseness, dizziness and dysphagia. The association of thoracic aortic aneurysm and dysphagia was originally described by Pape in 1932, as reported by Wilkinson et al. [2], and is only infrequently reported in the medical literature.
Recent case reports suggest that patients who develop aorto-oesophageal fistula have a prodromal syndrome which includes dysphagia [2]. Symptomatic compression of the oesophagus by abnormal vasculature has been described as Dysphagia Lusoria [3]; this symptom is more commonly caused by aberrant or ectatic vessels in the region of the aortic arch [4], particularly an aberrant right subclavian artery giving rise to a so-called ‘vascular ring’ which encompasses the oesohagus. To date, there are only few reports linking thoracic aortic aneurysm to dysphagia [5]. Suggested diagnostic modalities include a thoracic CT scan, barium swallow studies and oesophageal manometry, the latter being of academic interest only. Clinical suspicion of the pathology remains a mainstay of diagnosis.
Unfortunately, our patient succumbed before she was seen at the tertiary centre. Dysphagia aortica is rarely considered in the differential diagnosis of dysphagia; the lack of awareness lead to a significant diagnostic delay in our case. We suggest that all patients presenting with atypical symptoms, especially dysphagia caused by a thoracic aneurysm, should be referred urgently to a tertiary centre for operative treatment, as this particular symptom is associated with imminent rupture and death.
Notes
Conflicts of interest
None declared.
References
- 1.Rivera P, Ferrer L, Tuset JA, Pamos S, Lopez Mut J, Lujan M, Tome A, Medina E. Non-Aneurysmatic Aortic Dysphagia. Gastroenterol Hepatol. 1999;22(7):345–348. [PubMed] [Google Scholar]
- 2.Wilkinson JM, Euinton HA, Smith LF, Bull MJ, Thorpe JA. Diagnostic Dilemmas in Dysphagia Aortica. Eur J Cardiothorac Surg. 1997;11:222–227. doi: 10.1016/s1010-7940(96)01053-6. [DOI] [PubMed] [Google Scholar]
- 3.Contini S, Corrente V, Nervi G, Franze A, Scarpignato C. Dysphagia aortica: a neglected symptom of aortoesophageal fistula. Dig Liver Dis. 2006;38(1):51–54. doi: 10.1016/j.dld.2005.03.015. [DOI] [PubMed] [Google Scholar]
- 4.Ponce J, Gaspar E, Del Val A, Garrigues V, Sancho-Tello MJ, Carrasquer J. Dysphagia of vascular origin. Rev Esp Enferm Dig. 1991;80(1):53–56. [PubMed] [Google Scholar]
- 5.Jovancevic L, Jovic R, Mitrovic SM. Dysphagia aortica--case report. Med Pregl. 2005;58(7-8):401–404. doi: 10.2298/mpns0508401j. [DOI] [PubMed] [Google Scholar]