Abstract
Study Objective
We evaluated the effectiveness of interventions for pediatric patients with suicide-related emergency department (ED) visits.
Methods
We searched of MEDLINE, EMBASE, the Cochrane Library, other electronic databases, references, and key journals/conference proceedings. We included experimental or quasi-experimental studies that evaluated psychosocial interventions for pediatric suicide-related ED visits. Inclusion screening, study selection, and methodological quality were assessed by two independent reviewers. One reviewer extracted the data and a second checked for completeness and accuracy. Consensus was reached by conference; disagreements were adjudicated by a third reviewer. We calculated odds ratios (OR), relative risks (RR), or mean differences (MD) for each study’s primary outcome with 95% confidence intervals (CI). Meta-analysis was deferred due to clinical heterogeneity in intervention, patient population, and outcome.
Results
We included 7 RCTs and 3 quasi-experimental studies grouping and reviewing them according to intervention delivery: ED-based delivery (n=1), post-discharge delivery (n=6), and ED transition interventions (n=3). An ED-based discharge planning intervention increased the number of attended post-ED treatment sessions (MD=2.6; 95%CI:0.05,5.15). Of the 6 studies of post-discharge delivery interventions, one found increased adherence with service referral in patients who received community nurse home visits compared to simple placement referral at discharge (RR=1.28; 95%CI:1.06,1.56). The 3 ED transition intervention studies reported: (1) reduced risk of subsequent suicide following brief ED intervention and post-discharge contact (RR=0.10; 95%CI:0.03,0.41), (2) reduced suicide-related hospitalizations when ED visits were followed up with interim, psychiatric care (RR=0.41; 95%CI:0.28,0.60), and (3) increased likelihood of treatment completion when psychiatric evaluation in the ED was followed by attendance of outpatient sessions with a parent (OR=2.78; 95%CI:1.20,6.67).
Conclusion
Transition interventions appear most promising for reducing suicide-related outcomes and improving post-ED treatment adherence. Use of similar interventions and outcome measures in future studies would enhance the ability to derive strong recommendations from the clinical evidence in this area.
Introduction
Suicide is the third leading cause of death for young people aged 15 to 24 years. Up to twelve percent of deaths among adolescents and young adults in the United States are attributed to suicide.1 Each year, approximately 2 million adolescents aged 13 to 19 years express suicide-related behavior and just under half of those youths seek medical attention for their behavior.1 While suicidal intent is considered low for adolescents2 and the long-term risk of death by suicide 10 years following a suicide-related event is similarly low (approximately 1%),2–3 visits to the Emergency Department (ED) for suicide-related events may be more strongly associated with the intent to die.3–5
Presentations to the ED for suicide-related behaviors have increased significantly over the past 10 years. A population-based review by Larkin et al. found that visits by patients of all ages for suicide-related events increased from 0.8 to 1.5 visits per 1,000 US population from 1992 to 2001 (p=.04).6 They concluded that despite this increase in ED presentations rates, there has been a significant reciprocal decrease in post-attempt hospitalization, making EDs an important environment for assessing and stabilizing the suicidal crisis and initiating follow-up care to reduce subsequent crises.6 The need for these roles has been reinforced by others as well.7–12 Guidelines in the emergency (ED-based) care of children and adolescents after suicide-related events are available,14–18 as is a body of literature reviews.7,19–21 Most guidelines and literature reviews have highlighted the limited high quality evidence available to inform ED clinical practices for suicide-related presentations, but these papers have not included several known ED-based trials or have not been updated with recently published data, thereby limiting the ability to make comprehensive clinical recommendations. The objective of this systematic review was to evaluate the quality of research evidence available to inform existing clinical and psychosocial recommendations for pediatric suicide-related emergency care, and to develop recommendations for future research in the field. Specifically, we evaluated the effectiveness of ED-initiated interventions aimed at improving mental health care and health outcomes for pediatric suicide-related ED presentations.
Methods
Search Strategies
A research librarian, with input from the clinical research team, developed and implemented systematic search strategies using language (English and French) and year (1985 to 2009) restrictions. The search was conducted in 15 electronic bibliographic databases: MEDLINE®, MEDLINE® In-Process & Other Non-Indexed Citations, EMBASE, Cochrane Central Register of Controlled Trials, HealthStar, Cochrane Database of Systematic Reviews, Health Technology Assessment Database, Database of Abstracts of Reviews of Effects, Academic Search Elite, PsycINFO®, Health Source: Nursing and Academic Edition, CINAHL®, SocIndex, ProQuest Theses and Dissertations, and Child Welfare Information Gateway. To identify unpublished studies and studies-in-progress, we searched ClinicalTrials.gov and contacted authors of relevant studies. An initial search was conducted in January 2008. In October 2009, we revised the search to incorporate newly identified self harm terms not included in the original search. We re-applied the revised strategy in all 15 databases using the same language and publication date restrictions. The revised search was also restricted to randomized controlled trials using a validated filter from Glanville et al.22 The final Medline strategy is provided (see Appendix 1); comprehensive strategies used in each database are available from the corresponding author on request. Reference lists, key journals, and conference proceedings (Canadian Association of Emergency Physicians, Society for Academic Emergency Medicine, American College of Emergency Physicians, Canadian Paediatric Society) were also reviewed. An a priori decision was made not to include studies published prior to 1985 that were identified in our hand-search of study reference lists and key journals given the substantial diagnostic changes that occurred in the Diagnostic and Statistical Manual (DSM) post 1980 (DSM-III) and 1987 (DSM-III-R).
Study Selection
The results of the search strategies were screened independently by two reviewers. The full manuscripts of potentially relevant studies were retrieved if identified as relevant by at least one of the reviewers and were confirmed for inclusion independently by two reviewers. Studies were included in the review if they met the following criteria: they were experimental and quasi-experimental studies in design; they evaluated a mental health-based, suicide prevention-focused intervention that was initiated in the ED and/or immediately following ED discharge through direct referral/enrolment; and, the intervention was evaluated with children and adolescents (≤18 years), or with parents or ED personnel with the intention of benefiting the pediatric patient with suicide-related behaviors. No restrictions were placed on comparison interventions (control groups). Finally, at least one clinically relevant primary outcome needed to be reported if the study was to be included in the review. Primary outcomes could be health related (rates of self-injurious behavior, death by suicide, suicidal ideation), parent related (reporting of means restriction), or care related (service delivery, consultation, documentation). A post-hoc decision was made to include studies that partially included our age range, but extended into adulthood given that the intervention in these potentially relevant studies was determined a priori to be appropriate for older adolescents. For these studies, particularly where adult and pediatric data were pooled together, the potential for variation in intervention dosing and response across the lifespan were considered. Reviewer agreement on study screening for inclusion was quantified with the Kappa statistic23 and discrepancies were resolved by consensus.
Quality Assessment
Experimental studies were scored using the Jadad 5-point scale to assess control of bias including: randomization (0–2 points), double blinding (0–2 points), and withdrawals/dropouts (0–1point).24 Concealment of allocation was assessed as adequate, inadequate, or unclear using Schulz et al.’s recommended guidelines.25 Quasi-experimental studies were assessed using methodological criteria developed by Downs and Black.26 Quality was measured by study reporting, external and internal validity, and power, with a maximal quality index (QI) of 29. QI scores of >20 were considered good, 11 to 20 moderate, and <11 poor. Two reviewers independently analysed each study’s methodological quality and agreement was quantified with the Kappa statistic.23 Discrepancies were resolved by consensus.
Data Abstraction
Data from the final set of studies were extracted using a standardized form that encompassed elements of study characteristics (e.g., language of publication, country), characteristics of the study population; study setting; description of the intervention and comparisons; primary outcome measures and measurements tools; and, results. Data were extracted by one reviewer and checked for accuracy and completeness by a second reviewer. Discrepancies were resolved by consensus. In the case of unclear or unreported information in the original studies, primary authors were contacted.
Data Analysis
Heterogeneity in the interventions, clinical population, suicide-related nomenclature, and outcomes precluded the use of meta-analysis to pool and interpret study results. To provide some commonality to primary outcome reporting, odds ratios (OR) or relative risks (RR) were calculated with 95% confidence intervals (95%CI) for dichotomous outcomes, and mean differences with 95%CI were calculated for continuous outcomes. Number Needed to Treat (NNT) was also calculated (StatsDirect Ltd., 2002). Given heterogeneity in study interventions, patient population, and outcomes, however, comparisons of these calculated values across studies should be made cautiously.
Results
Description of included studies
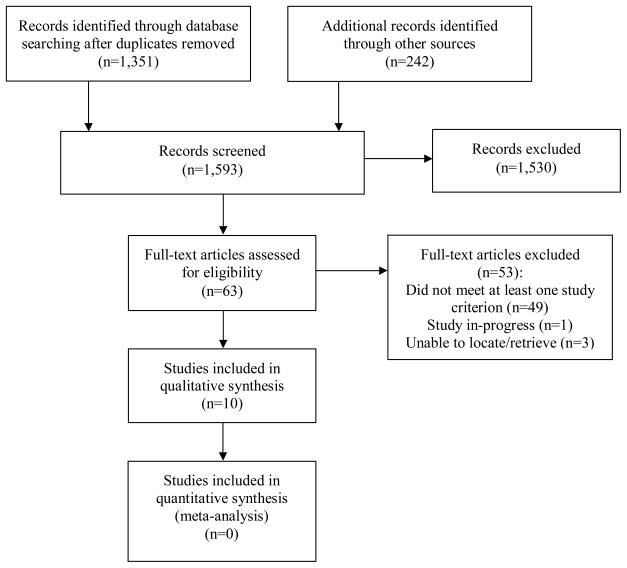
Figure 1 describes the flow of studies through the selection process. The search strategies identified 1,593 studies as potentially relevant to pediatric mental health care in the ED after removal of duplicates. Of these studies, 63 were identified as potentially relevant to interventions for suicide-related behaviors. Ten studies met the revised inclusion criteria: seven randomized controlled trials (RCTs)27–33 and three non-randomized (quasi-experimental) trials.34–36 One study34 had a duplicate publication.37 Five RCTs’ samples extended from adolescence to adulthood.29–33 One in-progress study was identified as relevant; but no data were available and the study was not included in this review.38 Two studies were excluded based on year of publication39–40 and we were unable to retrieve three studies through interlibrary loan.41–43 Forty-seven other studies were excluded based on patient population, intervention, or study setting after confirmation through full-text review or primary author contact. A list of excluded studies (n=53) is provided as a supplement to this paper. Reviewer agreement on study inclusion was substantial (99% observed agreement; κ=.63).
Figure 1.
Selection of studies investigating ED-initiated interventions for suicide-related behaviors.
Characteristics of the ten included studies are outlined in Table 1. These studies, published between 1986 and 2008, were conducted in: USA (n=4),27–28,34–35 UK (n=2),29,32 Belgium (n=1),30 Ireland (n=1),33 Canada (n=1),36 as well as Brazil, India, Iran, Sri Lanka and China (n=1).31 Patient populations included more females (sample average=72%; range=54–100%). Five studies included adolescents aged 12 and 18 years,27–28,34–36 four studies included participants ≥ 15 years of age,29–30,32–33 and one study reported a median age of 23 years for their study population.31 All studies were classified into three categories according to participant inclusion criteria using the Silverman et al.44–45 recommendations for defining and classifying patients’ suicide-related presentations and observed intent: (1) Studies that recruited subjects with ‘suicide attempts’ included patients whose behavior indicated a clear intent to die; (2) Studies that recruited subjects with ‘self-harm’ included patients whose behavior indicated no intent to die; (3) Studies that recruited subjects with ‘ideation/planning’ included patients who expressed ideation or planning without any clearly expressed suicide-related behaviors; and (4) Studies that recruited subjects with ‘undefined behaviors’ included patients where intent was undetermined or undefined. A conservative approach to categorization was employed. The lowest categorization level was identified if studies included multiple levels. A broad range of classification was evident in the studies: subjects with suicide attempts,27–28,30–31,34 subjects with self-harm behaviors,32 subjects with suicidal ideation,35–36 and subjects with undefined suicide-related behaviors.29,33 Variations in how suicide-related presentations were defined underscored definitional inconsistencies and patient heterogeneity across studies and limited comprehensive comparisons in this review.
Table 1.
Study characteristics
| First Author (Country, year) | Participants | ||
|---|---|---|---|
| Sample Size (n) (% female) | Age (y) (M) | Behavioral Intent | |
| Experimental Studies | |||
| Fleischmann31 (Brazil, India, Iran, Sri Lanka, China, 2008) | 1,867 (54%) | 10–85 (23†) | Suicide Attempt |
| Donaldson28 (USA, 2005) | 31 (82%) | 12–17 (15) | Suicide Attempt |
| Tyrer32 (UK, 2004) | 480 (68%) | 16–65 (31) | Self-Harm |
| Spirito27 (USA, 2002) | 63 (90%) | 12–18 (15) | Suicide Attempt |
| van Heeringen30 (Belgium, 1995) | 516 (57%) | ≥15 (34) | Suicide Attempt |
| McLeavey33 (Ireland, 1994) | 39 (74%) | 15–45 (24) | Undefined Intent |
| Waterhouse29 (UK, 1990) | 77 (62%) | ≥16 (30) | Undefined Intent |
| Quasi-Experimental Studies | |||
| Greenfield36 (Canada, 2002) | 286 (69%) | 12–17 (14) | Suicidal Ideation |
| Rotheram-Borus34 (USA, 2000) | 140 (100%) | 12–18 (15) | Suicide Attempt |
| Deykin35 (USA, 1986) | 319 (62%) | 13–17 (NR) | Suicidal Ideation |
Median value
Methodological quality of studies
Reviewer agreement on quality was excellent for both the quasi-experimental studies (κ=.83) and RCTs (κ=.96). While a randomized design was an overt strength in reducing risk of bias in the RCTs,27–33 because it is impossible to double-blind studies on psychiatric interventions, higher quality trials30–32 were limited to a maximum of three on the Jadad scale (out of five). Other trials were compromised with a lack of single-blinding (of outcome assessors) and unclear randomization resulting in Jadad scores of one29 or two.27–28,33 Allocation concealment was unclear in four studies27–28,30,33 and adequate in three studies.29,31–32 Two quasi-experimental studies were evaluated to be moderate to good in quality with scores of 20/29,34 21/29,35 and 24/29.36 These studies were rigorous in their use of comparison groups to reduce risk of bias, but were limited by their lack of randomization and therefore, potential confounding making causal attributions difficult.
Description of interventions
Tables 2 to 4 illustrate the heterogeneity of study interventions in the place of delivery: one study examined an ED-based intervention,27 six studies examined interventions that were implemented immediately following ED discharge,28–30,32–33,35 and three studies examined interventions that were initiated in the ED and extended post-ED discharge in the community.31,34,36 The ED-based study evaluated an enhanced discharge plan to improve treatment adherence with outpatient therapy.27 A considerable range of post-ED interventions were evaluated to predominantly reduce suicide-related behaviors. Four studies evaluated one-on-one (patient + health care provider) interventions using specialized therapeutic components including cognitive behavior therapy,32 interpersonal skills training and problem-solving,33 and community-based outreach with referral planning.30,35 One study evaluated the role of one-on-one plus family sessions that taught problem-solving and affect management,28 and another evaluated the impact of patient hospitalization.29 Studies that examined interventions that were initiated in the ED and followed through to post-ED discharge contact focused on the role of ED-based evaluation and referral with immediate telephone/home-based support contacts for the patient,31 psychiatric support until longer-term care was in place,36 or outpatient treatment sessions for the patient and a parent.34 Primary outcomes were death by suicide,31 subsequent suicide-related hospitalizations,36 and treatment adherence post-ED discharge.34 One study was located that evaluated an intervention with parents;34 no studies were located that targeted ED personnel with the intention of benefiting the pediatric patient with suicide-related behaviors.
Table 2.
ED-based interventions
| First Author | Intervention (I) and Key Features | Comparison (C) | Primary Outcome and Measurement (time point) | Results (I vs. C) | Interpretation |
|---|---|---|---|---|---|
| Experimental Studies | |||||
| Spirito27 | Standard Disposition Planning (SDP) plus 1-hr Compliance Intervention (CI) SDP Features: - Evaluation by psychiatric clinician CI Features: - Review of treatment expectations and adherence - Verbal contract to attend sessions |
Standard Disposition Planning | Treatment (session) attendance at 3 months follow-up | MD†=2.6 sessions (95%CI: 0.05,5.15) | Enhanced disposition planning with youths can increase adherence to outpatient treatment only when service barriers are overcome. |
Using study data adjusted for the confound ‘service barriers’
Table 4.
ED + post-ED interventions
| First Author | Intervention (I) and Key Features | Comparison (C) | Primary Outcome and Measurement (time point) | Results (I vs. C) | Interpretation |
|---|---|---|---|---|---|
| Experimental Studies | |||||
| Fleischmann31 | Standard care plus Brief Intervention and Contact (BIC) BIC Features: - Information post-discharge on risk and protective factors, basic epidemiology, alternative behaviors and referral options - Nine follow-up contacts (telephone or in-person) |
Standard Care Features: - Treatment of somatic symptoms |
Death by suicide at 18 months follow-up | RR=0.10 (95%CI:0.03,0.41) NNT=52 (range:32, 98) |
Brief intervention with ongoing supportive contact can reduce the likelihood of mortality attributable to suicide across the lifespan. |
| Quasi-Experimental Studies | |||||
| Rotheram- Borus34 | Specialized ED care plus SNAP (Successful Negotiation Acting Positively) therapy Features: - Psychiatric evaluation - Referral to SNAP therapy - Crisis therapy session - Video viewing SNAP: 6 outpatient sessions that focused on role-playing, problem-solving, negotiation |
Standard ED care plus SNAP therapy Features: - Psychiatric evaluation - Referral to SNAP therapy |
Treatment completion and suicide re-attempts at 18 months | Treatment completion OR=2.78 (95%CI:1.20,6.67) NNT=5 (range:3,20) Suicide re-attempts RR=0.63 (95%CI:0.25,1.54) |
Specialized ED care for youths increases the likelihood of treatment completion, but does not significantly reduce the risk of suicide re- attempt. |
| Greenfield36 | Rapid response outpatient team Features: - Part-time psychiatrist and psychiatric nurse contacted patient immediately after assessment in ED to schedule follow-up appointment, and team provided care until long- term arrangements could be made in the community |
Standard Care Features: - Psychiatrist in the ED could hospitalize the patient, follow the patient as an outpatient, or refer the patient to community- based resources |
Suicide-related hospitalization at 6 months follow-up | RR=0.41 (95%CI:0.28,0.60) NNT=4 (range:3,7) |
A rapid response outpatient model can reduce subsequent suicide-related hospitalizations for youths. |
Impact of interventions on primary outcomes
Two primary outcomes were measured by the studies: suicide-related outcomes and treatment adherence. Similar outcomes were measured differently across studies. Effects are presented by intervention design and stratified by study design in Tables 2 to 4.
Effects of ED-based interventions
One ED-based intervention, evaluated in a high methodological quality study, was shown to be effective in increasing treatment adherence (see Table 2). In the Spirito trial,27 adolescents who received enhanced disposition planning (a review of treatment expectations and verbally contracting to attend post-ED care) attended more post-ED treatment sessions than those who received standard planning (MD=2.6 sessions; 95%CI:0.05,5.15) when barriers to service were addressed.
Effects of post-ED interventions
Five post-ED studies of mixed methodological quality examined the impact of specialized interventions on a range of suicide-related outcomes at various post-intervention time points (see Table 3). These outcomes included rates of subsequent suicidal ideation,28 self-harm or re-attempts,28,32–33 and re-presentation to the ED for suicide-related behaviors.29,35 One study examined intervention impact on adherence with treatment referral.30 No studies demonstrated significant impact on suicide-related outcomes between specialized treatment and standard care.28–29,32–33,35 In their higher quality study of both adolescents and young adults, van Heeringen et al.30 found that adherence to service referral was higher for those who received home visits by a community nurse post ED-discharge (RR=1.28; 95%CI:1.06–1.56) compared to individuals who received standard discharge. In this study, as few as 6 and as many as 38 patients needed to receive a home visit to result in one patient follow-up with referral (NNT=6–38).
Table 3.
Post-ED interventions (direct ED enrolment)
| First Author | Intervention (I) and Key Features | Comparison (C) | Primary Outcome and Measurement (time point) | Results (I vs. C) | Interpretation |
|---|---|---|---|---|---|
| Experimental Studies | |||||
| Donaldson28 | Skills-based Treatment (SBT) Features: - Problem-solving - Affect management skills - 9 individual sessions, 1–3 family sessions, plus 2 optional crisis sessions |
Supportive relationship treatment (Standard Care) Features: - Focus on mood, behaviors and factors that contribute to suicide- related behaviors - 9 individual sessions, 1- 3 family sessions, plus 2 optional crisis sessions |
Cumulative rates of suicide re-attempts and suicidal ideation± at 6 months follow-up | Rates of re-attempt RR=2.13 (95%CI:0.53,9.08) Suicidal ideation MD=-7.27 (95%CI:−35.13,20.59) |
Treatment designed to address skill deficits in youths does not reduce rates of suicide re- attempt or suicidal ideation. |
| Tyrer32 | Manual Assisted Cognitive Behavior Therapy (MACT) Features: - Up to seven treatment sessions with a therapist trained in MACT methods were offered and a manual illustrating management strategies was provided |
Treatment As Usual Features: - Patient seen by a therapist and was offered the standard treatment or the continuation of existing therapy |
Recurrent self-harm episodes at 1 year follow-up | RR=0.86 (95%CI:0.69,1.08) | Manual Assisted Cognitive Behavior Therapy does not reduce the likelihood of repeat episodes of self-harm across the lifespan. |
| van Heeringen30 | Home Visits Features: - Community nurse evaluated treatment needs and matches to available community services - 1–2 contacts in < 1month |
Standard Care Features: - Referral without home visits |
Adherence with referral at 7 days follow-up | RR=1.28 (95%CI:1.06,1.56) NNT=9 (range:6,38) |
Home visits by a community nurse increase the likelihood of adherence with referral in youths and adults. |
| McLeavey33 | Interpersonal problem-solving skills training Features: - Five weekly sessions were given with training in five general stages of problem solving, with a supplementary manual and homework assignments |
Brief problem-oriented treatment Features: - Patient seen by a therapist within 2 weeks of discharge from ED and received treatment focused on resolution or reduction of current problems |
Recurrent self-harm (self-poisoning) at 1 year follow-up† | RR=0.50 (95%CI:0.12,2.05) | Interpersonal problem- solving skills training does not significantly reduce the likelihood of self-poisoning in the year following the index event. |
| Waterhouse29 | Hospital admission Features: - Admission with recommendation to contact family physician if in need of further help |
Discharge home Features: - Recommendation to contact family physician if in need of further help |
Repeat ED presentations for self-harm at 16 weeks follow-up | RR=0.77 (95%CI:0.20,2.89) | Hospital admission of youth and adult patients with suicide-related behaviors does not decrease the likelihood of ED re-presentation following discharge. |
| Quasi-Experimental Studies | |||||
| Deykin35 | Specialized direct service Features: - Community-based outreach program providing support, a liaison with the hospital, and advocacy with relevant agencies - Unreported number of contacts |
Standard Care Features: - not described |
Repeat ED presentations for suicide attempt or self-harm at 24 months follow-up | RR=1.71 (95%CI:0.73,4.03) | Specialized direct service for youths does not reduce the likelihood of ED re-presentation for suicide attempt. |
Measured using the Suicidal Ideation Questionnaire (SIQ)
Analysis with treatment completers only
Effects of ED-based plus post-ED interventions
Studies examining the role of transition interventions (ED to post-ED care) were of good to high methodological quality. The Fleishmann trial reported a statistically significant reduction in death by suicide across several low- to middle-income countries using brief education and enhanced follow-up as an addition to standard care (i.e., treatment of somatic symptoms). The median age of treated patients was 23 years.31 The likelihood of death by suicide was reduced in the treatment group compared to standard care (RR=0.10; 95%CI:0.03,0.41); death by suicide occurred for 2.2% of patients in the standard care group versus 0.2% in the treatment group. As few as 32 and as many as 98 patients need to be treated with the enhanced intervention to prevent one death by suicide (NNT=32–98). In the Rotherham-Borus et al.34 study, adolescents who received psychiatric evaluation in the ED following by attendance of outpatient sessions with their mother were 2.78 times more likely to complete outpatient treatment compared to those who received standard care (95%CI:1.20,6.67). As few as 3 and as many as 20 youths needed to be treated with the enhanced intervention to result in one treatment completer (NNT=3–20). No intervention impact was demonstrated for suicide-related behaviors (see Table 4). Greenfield et al.36 found that an ED-based crisis response team designed to schedule follow-up care and provide support until care was in place reduced hospitalization for up to 6 months following the initial ED visit (RR=0.41; 95%CI:0.28,0.60). As few as 3 and as many as 7 youths required a rapid response team to prevent one hospitalization for suicide-related behaviors (NNT=3–7).
Limitations
The limitations of this systematic review stem primarily from the included studies themselves. While several of the study’s designs had the potential to offer results based on rigorous design implementation and sample size, they were limited by risk of bias due to lack of blinding or control group and inconsistent accounting of important confounding variables such as co-morbid mental illnesses, substance use, family functioning, and history of suicide-related behaviors. Further to this, parameters for participant inclusion criteria must be addressed. While limiting inclusion criteria can assist with study design, a more homogenous patient population can also reduce recruitment abilities as well as valuable data on patient sub-groups.46 Several studies’ inclusion of a broad age range (from 10 to 85 years) also limited this review’s ability to draw firm conclusions on whether the study’s treatment approach and patient response would be different if the studies only targeted youth. Evidence derived from these studies should be regarded as preliminary and used to inform pediatric-specific trials.
Another important study limitation was outcome heterogeneity across the studies, which precluded comprehensive between-study comparisons. Debate also exists in choice of outcome for this field of study—particularly for emergency medicine research a reduction in the rate of suicide-related behaviors seems a logical outcome given the acuity of the clinical setting and urgency of the patient’s presentation. As a primary outcome, however, it requires large sample sizes for adequate study powering as the reoccurrence of these behaviors can be low depending on their level of risk.8,46 Treatment adherence and improved problem-solving may be valuable as primary outcomes for future emergency medicine studies particularly for those studies examining transition interventions. On a final note, the few multi-site trials in this review limited geographical representation, and importantly, the level of behavioral risk and suicide-related terminology varied in meaning across studies thus reducing consistency with current recommendations.45,47
Discussion
Pediatric patients presenting to the ED with suicidal ideation, single or repeat suicide attempts fall along a continuum of increasing risk8 making appropriate care and disposition decisions essential. While most clinical practice guidelines and literature reviews for this field7,14–21 have emphasized limitations in the available evidence base, these papers have not accounted for several ED-based trials or been updated with recently published data. This systematic review identified several promising interventions that could significantly impact patient and system outcomes if additional research is conducted and more consistent approaches to this field of study are applied.
Few ED interventions have been shown to reduce subsequent suicide-related behaviors and related hospitalizations. Interventions that initiate care in the ED and/or extended this care past ED discharge have shown impact on suicide-related outcomes compared to interventions initiated only after ED discharge. Findings should be interpreted with caution, however, given the studies’ noted limitations. Greenfield’s examination of a community outreach program was shown to decrease subsequent suicide-related hospitalizations for pediatric patients who presented to the ED with suicidal ideation, a group that is far less likely to be admitted to hospital than patients with behavioral intent.36 This study’s use of a quasi-experimental (non-randomized) design may have increased study feasibility (and possibly ethical conduct), but the role of confounding variables in hospitalization (e.g., comorbidity, behavioral intent, health care provider care) is still unclear. While the well-conducted Fleishmann trial31 suggested that brief intervention with ongoing supportive contact can reduce rates of death by suicide, conclusions were directed towards middle- to low-income countries and the intervention was evaluated with a predominantly young adult population. Both factors do limit the degree of study generalizability. Further, no perspective was offered on the intervention’s impact on rates of re-attempt and suicidal re-ideation, which are far more prevalent behaviors preceding death by suicide. Given that the Fleishmann trial demonstrated significant impact on a less frequently occurring outcome than other studies on a high risk clinical population (those with suicide attempt), the role of transition (ED + post-ED) care on suicide-related outcomes is important to thoroughly investigate. Although this approach to ED management would create a shift in how acute (and complex) conditions are treated, the care continuity in this approach is an important issue to evaluate. The failure of other studies to demonstrate a significant effect may be based on the nature of the intervention. For example, if interventions are disjointed from the critical clinical moment for the patient (such as post-ED interventions) they may fail to capitalize on motivation and opportunities to tailor treatment. However, it is impossible to address this, given current study designs. The introduction of ‘process evaluations’ to determine the effectiveness of individual intervention elements (rather than the collective intervention) would help address this gap. Of the studies that reported no significant effect of specialized interventions or standard care on suicide-related outcomes, current study limitations make firm conclusions difficult, and further evaluation using rigorous study design would allow for a more conclusive evaluation of the impact of ED, post-ED, and transition (ED + post-ED) care on suicide-related outcomes.
Strikingly absent from our review was the evaluation of the use of safety planning with patients. These plans are distinct from ‘no-harm contracts,’ which are not empirically supported.47–50 No studies with this intervention were screened during the initial stages of the review. The primary purpose of these safety planning contracts is to problem-solve with the patient and create a plan they will utilize during times of suicidal crisis. There may be utility in evaluating the impact of this form of planning on short-term and long-term patient outcomes given the lack of observed effect with both standard care and novel interventions.
Based on this review, it appears that re-attempts continue after an 18 to 24 month treatment period despite some reduction in suicidal ideation. As past suicide-related behaviors are strong indicators of later ones,4,19–20,51–52 it is critical that emergency and post-emergency based research improve the study and understanding of the role of clinical care in relation to these behaviors. Including known moderating and/or confounding relationships between ideation and attempts such as family environment, parental monitoring, co-morbidities, and risk-taking behaviors (i.e., substance use, smoking) is an important methodological step and one that was largely unaccounted for by the studies included in this review.
Increasing the inclusion of assessment, disposition planning, and adherence and problem-solving outcomes in ED-based research is also essential. These outcomes will better link research to the roles of clinicians in recognizing risk of suicide-related thoughts and behaviors, connecting young people and their families to necessary mental health services, and promoting continuity of care post-crisis.4,19–20 This review found rigorous evidence suggesting treatment adherence can be increased by addressing treatment barriers, discussing treatment expectations, and negotiating session attendance.27,30,34 Improved problem-solving, although measured as a secondary outcome, was reported by one study.33 Studies tailored to these foci are few, however, and more research is needed in both the ED setting and in referred community-based services with a link to other patient and system outcomes to determine long-term clinical and health utilization impact. Given the numbers needed to treat ranged greatly, linkage to other outcomes is essential.
One notable ED intervention absent from this review was parent means restriction. One observational study was excluded from our review based on design, but suggested that parental education in the ED may effectively improve means restriction in the home environment and may prove promising as a prevention effort.54 Future studies should extend these initial findings by evaluating enhanced parental education in RCTs and also including clinical outcomes to evaluate the effectiveness of means restriction on child/adolescent suicide-related behaviors and risk. Assessing family environment in the ED to gauge parental abilities may also limit means access and encourage monitoring.55–56
Behavioral lethality has received much attention in general treatment literature,4,9,19–20 disposition literature,57–58 and by the American Psychiatric Association (APA).59 Lethality assessment during ED history taking has been recommended,59 and scales have been suggested as adjunctive rather than as a rigid replacement to standard history taking,20 given the uniqueness to each child and adolescent’s risk factors and experiences.4 Using scales (e.g., the Beck Scale for Suicide Ideation, or the Beck Suicide Intent Scale60–61) to augment clinician understanding of risk may help address the concern that ED clinicians can underestimate the seriousness of suicidal intent.20,62 However, our review identified only one study that has used an ED-based population of suicidal patients to evaluate its tool’s psychometric properties.63 As this study did not focus on clinical outcomes, it was excluded in the review. An evaluation of such tools and/or actuarial instruments (which may reveal, more accurately, suicidality because of their self-report nature47) in the ED setting is needed with a focus on impact on clinical assessment and disposition decision-making.
At present, there is also no high quality research evidence to suggest that the quality of clinical care can be improved by using a specialized ED team. We think further evaluation is necessary. Within this research agenda, the impact of pediatric emergency- trained physicians versus general emergency practitioners in the ED on clinical care and patient outcomes should be examined. Future studies should also examine systemic factors influencing ED personnel attitudes and readiness to modify practice, and consider how to improve documentation of drug and alcohol use, family history, and co-morbidities given the lack of impact noted in this review, and the demonstrated association between these factors and suicide-related behaviors.64–65
To summarize, robust research evidence to inform current clinical and psychosocial management of pediatric suicide-related ED presentations is emerging but limited. The lack of consistency in methods and outcomes tracked along with the overall limited quality of the studies available suggests that this is an area of research requiring maturation and refinement. A systematic and comprehensive program of research across multiple settings could help to identify the relevant research questions that need to be answered to move this field forward. Multi-setting research efforts with consistent indicators of success in ED management of both children and adolescents will provide more definitive knowledge to guide practice. The dimensions of this research would include: risk assessment, discharge planning, ED capacity and skill set requirements, personnel attitudes and beliefs, crisis interventions, and outcomes tracking. Future studies must address methodological limitations of the reviewed literature and further evaluate already established clinical interventions to establish utility and benefit to patient and family outcomes. This will involve: (1) justifying the level of care to be provided in the ED and appropriate outcomes that should result,65 (2) including ‘process evaluations’ to determine the effectiveness the individual intervention elements of care that are deemed essential to the ED, (3) including well-defined treatment-as-usual control groups which are now considered the standard for conducting suicide-related treatment research,67 (4) distinguishing between short-term and long-term outcome variables that are appropriate for this field,46,68 (5) strict operationalization of the various subtypes of suicidality,44–45 and (6) using multi-site studies to recruit pediatric-only populations to avoid over-generalizing study effects on a broad patient age range. Finally, studies must sample subsets of suicide-related behaviors to increase the likelihood that studies are feasible, ethical and clinically meaningful.46,69 Highly suicidal individuals, for example, have been excluded from clinical trials and measures of certain suicide-related behaviors (i.e., ideation) not included as outcomes. The need to address these shortcomings, particularly in children and youths at risk, is now well recognized.70
Supplementary Material
Acknowledgments
Funding for this project was provided by a Knowledge Synthesis grant awarded to the principal author from the Canadian Institutes of Health Research (200805KRS). Dr. Newton is a CIHR Training Fellow (Career Development Award) in the Canadian Child Health Clinician Scientist Program, in partnership with the SickKids Foundation, Child & Family Research Institute (British Columbia), Women & Children’s Health Research Institute (Alberta), Manitoba Institute of Child Health.
The authors would like to acknowledge the important contributions from Mr. Ben Vandermeer (Alberta Research Centre for Health Evidence, University of Alberta) for consulting on statistical analysis and Ms. Belle Zou (Department of Pediatrics, University of Alberta) for assisting with initial screening, quality assessment, and data extraction.
References
- 1.Centers for Disease Control and Prevention. Youth risk behavior surveillance – United States, 2007. MMWR. 2008;57(SS-4) [PubMed] [Google Scholar]
- 2.Hawton K, Harriss L. Deliberate self-harm in young people: Characteristics and subsequent mortality in a 20-year cohort of patients presenting to hospital. J Clin Psychiatry. 2007;68:1574–83. [PubMed] [Google Scholar]
- 3.Hawton K, Zahl D, Weatherall R. Suicide following deliberate self-harm: Long-term follow-up of patients who presented to general hospital. Br J Psychiatry. 2003;182:537–42. doi: 10.1192/bjp.182.6.537. [DOI] [PubMed] [Google Scholar]
- 4.Rodham K, Hawton K, Evans E. Reasons for deliberate self-harm: Comparison of self-poisoners and self-cutters in a community sample of adolescents. J Am Acad Child Adolesc Psychiatry. 2004;43:80–7. doi: 10.1097/00004583-200401000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Owens D, Horrocks J, House A. Fatal and non-fatal repetition in self-harm: Systematic review. Br J Psychiatry. 2002;181:193–9. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 6.Larkin GL, Smith RP, Beautrais AL. Trends in US emergency department visits for suicide attempts, 1992–2001. Crisis. 2008;29:73–80. doi: 10.1027/0227-5910.29.2.73. [DOI] [PubMed] [Google Scholar]
- 7.Stewart SE, Manion IG, Davidson S. Emergency management of the adolescent suicide attempter: A review of the literature. J Adolesc Health. 2002;30:312–25. doi: 10.1016/s1054-139x(01)00321-4. [DOI] [PubMed] [Google Scholar]
- 8.Asarnow JR, Baraff LJ, Berk M, et al. Pediatric emergency department suicidal patients: Two-site evaluation of suicide ideators, single attempters, and repeat attempters. J Am Acad Child Adolesc Psychiatry. 2008;47:958–66. doi: 10.1097/CHI.0b013e3181799ee8. [DOI] [PubMed] [Google Scholar]
- 9.Wintersteen MB, Diamond GS, Fein JA. Screening for suicide risk in the pediatric emergency and acute care setting. Curr Opin Pediatr. 2007;19:398–404. doi: 10.1097/MOP.0b013e328220e997. [DOI] [PubMed] [Google Scholar]
- 10.Crandall C, Fullerton-Gleason L, Aguero R, LaValley J. Subsequent suicide mortality among emergency department patients seen for suicidal behavior. Acad Emerg Med. 2006;13:435–42. doi: 10.1197/j.aem.2005.11.072. [DOI] [PubMed] [Google Scholar]
- 11.Aschkenasy JR, Clark DC, Zinn LD, Richtsmeier AJ. The non-psychiatric physician’s responsibilities for the suicidal adolescent. NY State J Med. 1992;92:97–104. [PubMed] [Google Scholar]
- 12.Cooper JB, Lawlor MP, Hiroeh U, et al. Factors that influence emergency department doctors’ assessment of suicide risk in deliberate self-harm patients. Eur J Emerg Med. 2003;10:283–7. doi: 10.1097/00063110-200312000-00008. [DOI] [PubMed] [Google Scholar]
- 13.Shain BN. Committee on Adolescence. Suicide and suicide attempts in adolescents. Pediatrics. 2007;120:669–76. doi: 10.1542/peds.2007-1908. [DOI] [PubMed] [Google Scholar]
- 14.National Collaborating Centre for Mental Health. National Clinical Practice Guideline Number 16. Rushden, Northamptonshire, UK: Stanley L. Hunt (Printers) Ltd; 2004. Self-harm: The Short-Term Physical and Psychological Management and Secondary Prevention of Self-Harm in Primary and Secondary Care. See: http://www.nice.org.uk/nicemedia/pdf/CG16FullGuideline.pdf for complete guideline. [Google Scholar]
- 15.American Academy of Child and Adolescent Psychiatry. Practice Parameters for the Assessment and Treatment of Children and Adolescents with Suicidal Behavior. Washington, DC: Author; 2000. [Google Scholar]
- 16.Royal College of Psychiatrists. Council Report CR64. London, UK: Author; 1998. Managing Deliberate Self-Harm in Young People. [Google Scholar]
- 17.Australasian College for Emergency Medicine and the Royal Australian and New Zealand College of Psychiatrists. Guidelines for the Management of Deliberate Self Harm in Young People. Melbourne, AUS: Authors; 2000. [Google Scholar]
- 18.New Zealand Guidelines Group and Ministry of Health (Manatu Hauora) The Assessment and Management of People at Risk of Suicide. Wellington, NZ: Authors; 2003. [Google Scholar]
- 19.Tishler CL, Staats Reiss N, Rhodes AR. Suicidal behavior in children younger than twelve: A diagnostic challenge for emergency department personnel. Acad Emerg Med. 2007;14:810–18. doi: 10.1197/j.aem.2007.05.014. [DOI] [PubMed] [Google Scholar]
- 20.Kennedy SP, Baraff LJ, Suddath RL, Asarnow JR. Emergency management of suicidal adolescents. Ann Emerg Med. 2004;43:452–60. doi: 10.1016/j.annemergmed.2003.09.009. [DOI] [PubMed] [Google Scholar]
- 21.Gould MS, Greenberg T, Velting DM, Shaffer D. Youth suicide risk and preventive interventions: A review of the past 10 years. J Am Acad Child Adolesc Psychiatry. 2003;42:386–405. doi: 10.1097/01.CHI.0000046821.95464.CF. [DOI] [PubMed] [Google Scholar]
- 22.Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: Ten years on. J Med Libr Assoc. 2006;94(2):130–6. Erratum: J Med Libr Assoc 2006;94(3):354. [PMC free article] [PubMed] [Google Scholar]
- 23.Altman DG. Practical Statistics for Medical Research. London, UK: Chapman and Hall; 1991. [Google Scholar]
- 24.Jadad AR, Moore RA, Carrol D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 25.Shulz KF, Chalmers I, Hayes RJ, Altman DG. Empirical evidence of bias. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273:408–12. doi: 10.1001/jama.273.5.408. [DOI] [PubMed] [Google Scholar]
- 26.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality of both randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998;52:377–84. doi: 10.1136/jech.52.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spirito A, Boergers J, Donaldson D, et al. An intervention trial to improve adherence to community treatment by adolescents after a suicide attempt. J Am Acad Child Adolesc Psychiatry. 2002;41:435–42. doi: 10.1097/00004583-200204000-00016. [DOI] [PubMed] [Google Scholar]
- 28.Donaldson D, Spirito A, Esposito-Smythers C. Treatment for adolescents following a suicide attempt: Results of a pilot trial. J Am Acad Child Adolesc Psychiatry. 2005;44:113–20. doi: 10.1097/00004583-200502000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Waterhouse J, Platt S. General hospital admission in the management of parasuicide: A randomised controlled trial. Br J Psychiatry. 1990;156:236–42. doi: 10.1192/bjp.156.2.236. [DOI] [PubMed] [Google Scholar]
- 30.van Heeringen C, Jannes S, Buylaert W, et al. The management of non-compliance with referral to out-patient after-care among attempted suicide patients: A controlled intervention study. Psychol Med. 1995;25:963–70. doi: 10.1017/s0033291700037454. [DOI] [PubMed] [Google Scholar]
- 31.Fleischmann A, Bertolote JM, Wasserman D, et al. Effectiveness of brief intervention and contact for suicide attempters: A randomized controlled trial in five countries. Bull World Health Organ. 2008;86:703–09. doi: 10.2471/BLT.07.046995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tyrer P, Tom B, Byford S, et al. Differential effects of manual assisted cognitive behavior therapy in the treatment of recurrent deliberate self-harm and personality disturbance: The POPMACT study. J Pers Disord. 2004;18:102–16. doi: 10.1521/pedi.18.1.102.32770. [DOI] [PubMed] [Google Scholar]
- 33.McLeavey BC, Ludgate RJ, Murray CM. Interpersonal problem-solving skills in the treatment of self-poisoning patients. Suicide Life Threat Behav. 1994;24:382. [PubMed] [Google Scholar]
- 34.Rotheram-Borus MJ, Piacentini J, Cantwell C, et al. The 18-month impact of an emergency room intervention for adolescent female suicide attempters. J Consult Clin Psychol. 2000;68:1081–93. doi: 10.1037//0022-006x.68.6.1081. [DOI] [PubMed] [Google Scholar]
- 35.Deykin EY, Hsieh C, Joshi N, McNamarra JJ. Adolescent suicidal and self-destructive behavior: Results of an intervention study. J Adolesc Health Care. 1986;7:88–95. doi: 10.1016/s0197-0070(86)80002-x. [DOI] [PubMed] [Google Scholar]
- 36.Greenfield B, Larson C, Hechtman L, Rousseau C, Platt R. A rapid-response outpatient model for reducing hospitalization rates among suicidal adolescents. Psychiatr Serv. 2002;53:1574–79. doi: 10.1176/appi.ps.53.12.1574. [DOI] [PubMed] [Google Scholar]
- 37.Rotheram-Borus MJ, Piacentini J, Van Rossem R, Graae F, Cantwell C, Castro-Blanco D, Miller S, Feldman J. Enhancing treatment adherence with a specialized emergency room program for adolescent suicide attempters. J Am Acad Child Adolesc Psychiatry. 1996;35:654–63. doi: 10.1097/00004583-199605000-00021. [DOI] [PubMed] [Google Scholar]
- 38.Asarnow JRPI. Family intervention for suicidal youth: Emergency care. ClinicalTrials.gov. [Accessed January 21, 2009]. Web site. Available at: www.clinicaltrials.gov.
- 39.Welu T. A follow-up programme for suicide attempters: Evaluation of effectiveness. Suicide Life Threat Behav. 1977;7:17–30. [PubMed] [Google Scholar]
- 40.Termansen PE, Bywater C. S.A.F.E.R: A follow-up service for attempted suicide in Vancouver. Can Psychiatr Assoc J. 1975;20:29–34. doi: 10.1177/070674377502000106. [DOI] [PubMed] [Google Scholar]
- 41.Suicide prevention. Postgrad Med. 2000;108:155–6. doi: 10.3810/pgm.2000.11.1306. No authors. [DOI] [PubMed] [Google Scholar]
- 42.Morgan HG. Intervention to reduce rates of deliberate self harm in attenders at accident and emergency clinics. National Research Register; 1997. [Google Scholar]
- 43.Torhorst A, Moller HJ, Buerk F, Kurz A, Waechtler C, Lauter H. Outpatient aftercare treatment following attempted suicide. Initial results of an experimental study. Suizidprophylaxe. 1984;4(254):73. [Google Scholar]
- 44.Silverman MM, Berman AL, Sanddal ND, et al. Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 1: Background, rationale, and methodology. Suicide Life Threat Behav. 2007;37:248–63. doi: 10.1521/suli.2007.37.3.248. [DOI] [PubMed] [Google Scholar]
- 45.Silverman MM, Berman AL, Sanddal ND, O’Carroll PW, Joiner TE. Rebuilding the tower of Babel: A revised nomenclature for the study of suicide and suicidal behaviors. Part 2: Suicide-related ideations, communications, and behaviors. Suicide Life Threat Behav. 2007;37:264–77. doi: 10.1521/suli.2007.37.3.264. [DOI] [PubMed] [Google Scholar]
- 46.Hatcher S, Sharon C, Coggan C. Beyond randomized controlled trials in attempted suicide research. Suicide Life Threat Behav. 2009;39:396–407. doi: 10.1521/suli.2009.39.4.396. [DOI] [PubMed] [Google Scholar]
- 47.Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol. 2006;62:185–200. doi: 10.1002/jclp.20222. [DOI] [PubMed] [Google Scholar]
- 48.McMyler C, Pryjmachuk S. Do ‘no-suicide’ contracts work? J Psychiatr Ment Health Nurs. 2008;15:512–22. doi: 10.1111/j.1365-2850.2008.01286.x. [DOI] [PubMed] [Google Scholar]
- 49.Lewis LM. No-harm contracts: A review of what we know. Suicide Life Threat Behav. 2007;37:50–7. doi: 10.1521/suli.2007.37.1.50. [DOI] [PubMed] [Google Scholar]
- 50.Rudd MD, Mandrusiak M, Joiner TE. The case against no-suicide contracts: The commitment to treatment statement as a practice alternative. J Clin Psychol. 2006;62:243–51. doi: 10.1002/jclp.20227. [DOI] [PubMed] [Google Scholar]
- 51.Goldston DB, Daniel SS, Reboussin DM, et al. Suicide attempts among formerly hospitalized adolescents: A prospective naturalistic study of risk during the first 5 years after discharge. J Am Acad Child Adolesc Psychiat. 1999;38:660–71. doi: 10.1097/00004583-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 52.Joiner TE, Conwell Y, Fitzpatrick KK, et al. Four studies on how past and current suicidality relate even when “everything but the kitchen sink” is covaried. J Abnorm Psychol. 2005;114:291–303. doi: 10.1037/0021-843X.114.2.291. [DOI] [PubMed] [Google Scholar]
- 53.LaRicka R, Wingate MS, Joiner TE, et al. Empirically informed approaches to topics in suicide risk assessment. Behav Sci Law. 2004;22:651–65. doi: 10.1002/bsl.612. [DOI] [PubMed] [Google Scholar]
- 54.Kruesi MJP, Grossman J, Pennington JM, et al. Suicide and violence prevention: parent education in the emergency department. J Am Acad Child Adolesc Psychiatry. 1999;38:250–55. doi: 10.1097/00004583-199903000-00010. [DOI] [PubMed] [Google Scholar]
- 55.Li G, Ling J, DiScala C, et al. Characteristics and outcomes of self inflicted pediatric injuries: The role of method of suicide attempt. Inj Prev. 1997;3:115–9. doi: 10.1136/ip.3.2.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.McManus BL, Kruesi MJ, Dontes AE, et al. Child and adolescent suicide attempts: An opportunity for emergency departments to provide injury prevention education. Am J Emerg Med. 1997;15:357–60. doi: 10.1016/s0735-6757(97)90124-8. [DOI] [PubMed] [Google Scholar]
- 57.Baca-Garcia E, Diaz-Sastre C, Resa EG, et al. Variables associated with hospitalization decisions by emergency physicians after a patient’s suicide attempt. Psychiatr Serv. 2004;55:792–7. doi: 10.1176/appi.ps.55.7.792. [DOI] [PubMed] [Google Scholar]
- 58.Goldberg JF, Ernst CL, Bird S. Predicting hospitalization versus discharge of suicidal patients presenting to a psychiatric emergency service. Psychiatr Serv. 2007;58:561–5. doi: 10.1176/ps.2007.58.4.561. [DOI] [PubMed] [Google Scholar]
- 59.American Psychiatric Association. Practice Guidelines for the Treatment of Psychiatric Disorders Compendium. 2. Arlington, VA: Author; 2004. Practice guidelines for the assessment and treatment of patients with suicidal behaviors; pp. 1315–1456. [Google Scholar]
- 60.Beck AT, Brown GK, Steer RA. Psychometric characteristics of the Scale for Suicide Ideation with psychiatric outpatients. Behav Res Ther. 1997;35:1039–46. doi: 10.1016/s0005-7967(97)00073-9. [DOI] [PubMed] [Google Scholar]
- 61.Beck AT, Schuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnik HLP, Lettieri DJ, editors. The Prediction of Suicide. Bowie, MD: Charles Press; 1974. pp. 45–56. [Google Scholar]
- 62.Bethell J, Rhodes AE. Identifying deliberate self-harm in emergency department data. Health Rep. 2009;20(2):35–42. [PubMed] [Google Scholar]
- 63.Potter LB, Kresnow M, Powell KE, et al. Identification of nearly fatal suicide attempts: Self-Inflicted Injury Severity Form. Suicide Life Threat Behav. 1998;28:174–86. [PubMed] [Google Scholar]
- 64.King RA, Schwab-Stone M, Flisher AJ, et al. Psychosocial and risk behavior correlates of youth suicide attempts and suicidal ideation. J Am Acad Child Adolesc Psychiat. 2001;40:837–46. doi: 10.1097/00004583-200107000-00019. [DOI] [PubMed] [Google Scholar]
- 65.Gould MS, King R, Greenwald S, et al. Psychopathology associated with suicidal ideation and attempts among children and adolescents. J Am Acad Child Adolesc Psychiat. 1998;37:915–23. doi: 10.1097/00004583-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 66.Burns J, Dudley M, Hazell P, Patton G. Clinical management of deliberate self-harm in young people: The need for evidence-based approaches to reduce repetition. Aust N Z J Psychiatry. 2005;39:121–8. doi: 10.1080/j.1440-1614.2005.01532.x. [DOI] [PubMed] [Google Scholar]
- 67.Spirito A, Stanton C, Donaldson D, Boergers J. Treatment-as-usual for adolescent suicide attempters: Implications for the choice of comparison groups in psychotherapy research. J Clin Child Adolesc Psychol. 2002;31:41–7. doi: 10.1207/S15374424JCCP3101_06. [DOI] [PubMed] [Google Scholar]
- 68.Arensman E, Townsend E, Hawton K, et al. Psychosocial and pharmacological treatment of patients following deliberate self-harm: The methodological issues involved in evaluating effectiveness. Suicide Life Threat Behav. 2001;31:169–80. doi: 10.1521/suli.31.2.169.21516. [DOI] [PubMed] [Google Scholar]
- 69.Cwik MF, Walkup JT. Can randomized controlled trials be done with suicidal youths? Int Rev Psychiatry. 2008;20:177–82. doi: 10.1080/09540260801889104. [DOI] [PubMed] [Google Scholar]
- 70.Campo JV. Youth suicide prevention: Does access to care matter? Curr Opin Pediatr. 2009;21:628–34. doi: 10.1097/MOP.0b013e32833069bd. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.