Abstract
Objectives
Recommendations by health care providers have been found to vary by patient race/ethnicity and socioeconomic status (SES) and may contribute to health disparities. This study investigated the effect of these factors on recommendations for contraception.
Study Design
One of 18 videos depicting patients of varying sociodemographic characteristics was shown to each of 524 health care providers. Providers indicated whether they would recommend levonorgestrel intrauterine contraception (IUC).
Results
Low SES Whites were less likely to have IUC recommended than high SES Whites (OR 0.20, 95% CI 0.06 to 0.69), while SES had no significant effect among Latinas and Blacks. By race/ethnicity, low SES Latinas and Blacks were more likely to have IUC recommended than low SES Whites (OR and 95% CI 3.4 (1.1 to 10.2) and 3.1 (1.0 to 9.6) respectively), with no effect for high SES patients.
Conclusion
Providers may have biases about IUC or make assumptions about its use based on patient race/ethnicity and SES.
Keywords: Contraceptive counseling, health disparities, intrauterine contraception, family planning
Introduction
Disparities in health outcomes by race/ethnicity and socioeconomic status (SES) are well documented in many areas.1 The role of health care providers in contributing to these disparities is an area of growing research,2 3 with multiple studies suggesting that providers treat patients differently depending on patients’ race/ethnicity4–6 and SES.7 8 These findings are consistent with social psychology research indicating that subconscious stereotyping by social categories is widespread even among those who self-identify as non-discriminatory.9
Previous research on the effect of patient race/ethnicity and SES on providers’ clinical behavior has focused on provider-patient interactions around discrete medical decisions for which there is general consensus about appropriate treatment.4 5 10 Contraceptive decision making, on the other hand, involves the consideration of multiple clinically appropriate options, with the best treatment being highly dependent on patients’ personal preferences. In addition, the discussion of sexual behavior and contraception use in a clinical encounter is a culturally and socially complex area of medicine in which providers’ subconscious biases or assumptions might play an important role.
The limited data analyzing potential disparities in providers’ decision making in this context suggest that providers may be susceptible to different influences on their recommendations. From one perspective, several studies have suggested that providers may be especially likely to encourage the use of highly effective contraceptive methods and discourage fertility in minority and low-income populations.11–13 On the other hand, minority and low-income women in the United States have higher rates of unintended pregnancy and lower use of contraceptive methods than do White and higher-income women.14 15 While system and patient related factors undoubtedly contribute to these statistics, the presence of these disparities also raises the possibility that clinicians may not, in fact, be promoting effective contraceptive methods among patients from these sociodemographic groups.
The effect of patient characteristics on provider recommendations for intrauterine contraception (IUC) is of particular interest due to this method’s high efficacy,16 as a any tendency towards discouraging the fertility of specific populations could be manifested in a greater likelihood of recommending this method. Alternatively, as many providers are concerned that the use of IUC could result in pelvic infections among women at increased risk for sexually transmitted infections,17 18 despite the fact that well-designed clinical studies have indicated that these concerns are misplaced,19 20 clinicians who make race-and class-based assumptions about sexual behaviors may be less likely to consider IUC as an appropriate contraceptive method for poor and minority women. As an expansion in the use of IUC is currently being advocated as a means to decrease unintended pregnancy,18 21 22 it is important to understand whether differences in provider recommendations by race/ethnicity and SES exist and, if so, consider how these differences may affect efforts to promote IUC in different demographic groups.
In order to determine whether patient race/ethnicity and SES affect provider recommendations for the levonorgestrel IUC, we conducted a study of providers’ recommendations using videos of standardized patients of different race/ethnicities and SES.
Materials and Methods
Standardized Patient Videos
We produced 18 videos portraying a standardized patient requesting advice about contraception, with the patient varying by race/ethnicity (White, Black, or Latina), SES (low- or upper-middle class), and gynecologic history (a woman with a history of a vaginal delivery and no history of sexually transmitted infections (STIs); a woman with a history of a vaginal delivery and history of pelvic inflammatory disease (PID); or a nulliparous women with no history of sexually transmitted infections). The low SES patient was portrayed as a housekeeper studying for her GED and the high SES patient as a recent business school graduate working as a bank manager. Both the high SES and the low SES patients were portrayed by the same actor within each racial/ethnic category. The providers were told that the patient was 27 years old, had normal blood pressure, and had recently had a negative test for Gonorrhea and Chlamydia and a normal Papanicolaou test. Each patient indicated that she was in a monogamous relationship and that she did not want to become pregnant for at least a few years. For the purpose of these analyses, the primary gynecologic profile of interest was the woman who had had a vaginal delivery and had no history of STIs, as women with this history have historically been perceived as ideal IUC candidates. The standardized patients who were nulliparous or had a history of PID were grouped together as having perceived risk factors for complications related to IUC". Photographs of the standardized patients are shown in Figure 1a through 1f.
Figure 1.
Figure 1a: Low SES White Patient
Figure 1b: High SES White Patient
Figure 1c: Low SES Black Patient
Figure 1d: High SES Black Patient
Figure 1e: Low SES Latina Patient
Figure 1f: High SES Latina Patient
In each video, the patient presented her history as a monologue, with the only variation being the study factors. The scripts used in the videos were pre-tested with a sample of 15 providers to ensure the maximal level of realism. Standardization of verbal factors, such as inflection and tone, were practiced with the three actors. Five health care providers watched all 18 videos in order to verify overall consistency of non-verbal and verbal content.
Study Design
We recruited a convenience sample of health care providers (MDs, DOs, Nurse Practitioners and Physician Assistants) at meetings of professional societies of family medicine and obstetrics and gynecology. Eligibility criteria consisted of being a practicing health care provider in the United States who had completed training. After observing one video, selected using randomly permuted blocks of 18, the providers completed a survey about their contraceptive recommendations for the patient shown, ranking each of 6 methods on a scale of −3 to +3, with −3 indicating “Strongly Recommend Against”, 0 indicating “Neither Recommend for nor Against” and +3 indicating “Strongly Recommend For”. The computerized survey randomized the order in which the contraceptive methods were displayed to avoid any sequence effect. The subjects were informed during the survey that the patient’s health care insurance covered all contraceptive methods. Our outcome of interest was the recommendation regarding the levonorgestrel IUC, as this is the more effective of the two IUCs offered in the United States.23 Providers also answered questions about their perceptions of the patient in the video, indicating whether they felt the patient was more or less likely to experience specific outcomes and whether she was more or less intelligent and knowledgeable than an average woman her age. The providers were not aware of the primary study hypothesis regarding the effect of patient race/ethnicity and SES on provider recommendations for IUC.
Our primary research question was whether the recommendations of providers for IUC differ for African American, Latina and White patients. We based our sample size on a binary outcome of willingness to recommend an IUC. We hypothesized that a difference of 15 percentage points in prevalence of this outcome would be clinically significant in populations where overall prevalence of the outcome is 30%. Our sample of 524 provided 84% power to detect a difference of this magnitude in separate comparisons of African American and Latina women to White women.
Statistical Analysis
We performed bivariate analysis of the outcome variable of recommendation for the levonorgestrel IUC using chi-squared tests, Fisher’s exact tests and t-tests as appropriate. Multivariate logistic regression was performed using a dichotomized response variable of >=+1 or <=0. Due to the complicated interplay between social factors in other studies,23 prespecified analyses included analysis of interactions between the patient characteristics of race/ethnicity, SES, and gynecologic history. For the multivariate model, we prespecified the following provider-level variables to be included in the model: age, sex, race/ethnicity, specialty and provision of IUC. For all other variables, we utilized backwards selection and included any variables that changed any of the coefficients of interest by >10%. The subjects’ perceptions of the patients were analyzed in the same manner. All analyses were performed using Stata Version 9.2 (Stata Corp, College Station Tx).
The Committee of Human Research at the University of California, San Francisco approved this study, and all subjects provided informed consent prior to participation.
Results
The videos were shown at four meetings between September 2007 and May 2008; two regional and one national meeting of the American College of Obstetricians and Gynecologists, and the national meeting of the American Academy of Family Physicians. Five hundred and twenty four health care providers completed the study, and the race/ethnicity, SES, and gynecologic profile of the standardized patients were balanced between all provider characteristics except provider race/ethnicity in the overall sample (Table 1). Within each strata defined by the standardized patients gynecologic characteristics, the provider characteristics were balanced, with the exception that male providers assigned to standardized patients with perceived risk factors were more likely to be assigned the Black patient and less likely to be assigned the Latina patient than were female providers (p=0.02).
Table 1.
Characteristics of Study Subjects, by Standardized Patient Characteristics
| Characteristics of Study Subjects |
Standardized Patient Characteristics | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| All Subjects |
White n=179 |
Black n=172 |
Latina n=173 |
P value | High SES n=262 |
Low SES n=262 |
P value | No Risk Factors n=173 |
Perceived Risk Factors n=351 |
P value | |
| Male Sex (%) | 53.6 | 52.5 | 59.3 | 49.1 | 0.16 | 50.8 | 56.5 | 0.19 | 52.0 | 54.4 | 0.61 |
|
Race/Ethnicity (%) |
0.96 | 0.38 | 0.008 | ||||||||
| White | 76.9 | 79.9 | 75.0 | 75.7 | 78.2 | 75.6 | 84.4 | 73.2 | |||
| Black | 7.8 | 7.3 | 7.6 | 8.7 | 6.1 | 9.5 | 2.3 | 10.5 | |||
| Latina | 3.8 | 2.8 | 4.1 | 4.6 | 5.0 | 2.7 | 3.5 | 4.0 | |||
| Asian | 9.2 | 7.8 | 11.1 | 8.7 | 8.4 | 9.9 | 6.9 | 10.3 | |||
| Other | 2.3 | 2.2 | 2.3 | 2.3 | 2.3 | 2.3 | 2.9 | 2.0 | |||
| Age (Mean/SD) | 45.9 (10.5) |
44.9 (9.7) |
46.9 (11.3) |
45.8 (10.4) |
0.22 | 44.6 (10.0) |
47.2 (10.8) |
0.10 | 45.5 (10.9) |
46.0 (10.3) |
0.47 |
| Specialty (%) | 0.94 | 0.80 | 0.57 | ||||||||
| Ob/Gyn | 59.0 | 59.8 | 59.9 | 57.2 | 58.0 | 59.9 | 59.5 | 58.7 | |||
| Family Medicine |
38.7 | 38.6 | 37.8 | 39.9 | 39.3 | 38.2 | 39.3 | 38.5 | |||
| Other | 2.3 | 1.7 | 2.3 | 2.9 | 2.7 | 1.9 | 1.2 | 2.9 | |||
|
Performs IUC Insertions (%) |
74.1 | 76.0 | 75.0 | 71.1 | 0.55 | 72.1 | 76.0 | 0.32 | 76.9 | 72.7 | 0.30 |
|
Professional Degree (%) |
0.07 | 0.82 | 0.48 | ||||||||
| MD/DO | 96.0 | 97.8 | 97.1 | 93.1 | 95.8 | 96.2 | 97.1 | 95.4 | |||
| NP or PA | 4.0 | 2.2 | 2.9 | 6.9 | 4.2 | 3.8 | 2.9 | 4.6 | |||
|
Frequency of Prescribing Contraception (%) |
0.99 | 0.86 | 0.25 | ||||||||
| Never or Rarely |
5.9 | 6.2 | 5.8 | 5.8 | 6.5 | 5.3 | 5.2 | 6.3 | |||
| Occasionally | 16.2 | 16.2 | 16.9 | 15.6 | 16.0 | 16.4 | 12.7 | 18.0 | |||
| Frequently | 77.9 | 77.7 | 77.3 | 78.6 | 77.5 | 78.2 | 82.1 | 75.8 | |||
|
Board Certified (%) |
92.0 | 92.2 | 89.0 | 94.8 | 0.14 | 90.5 | 93.5 | 0.20 | 93.1 | 91.5 | 0.52 |
|
Percentage of Patients of Reproductive Age (%) |
0.44 | 0.51 | 0.79 | ||||||||
| 0–25% | 16.0 | 14.5 | 14.0 | 19.7 | 15.6 | 16.4 | 14.5 | 16.8 | |||
| 26–75% | 62.0 | 64.8 | 64.5 | 56.7 | 60.3 | 63.7 | 63.0 | 61.5 | |||
| >75% | 22.0 | 20.7 | 21.5 | 23.7 | 24.1 | 19.9 | 22.5 | 21.7 | |||
|
Accepts Medicaid (%) |
81.3 | 77.7 | 82.6 | 83.8 | 0.29 | 81.7 | 80.9 | 0.82 | 82.7 | 80.6 | 0.58 |
|
Hours/Wk of Clinical Care (%) |
0.76 | 0.32 | 0.62 | ||||||||
| <10 | 5.0 | 3.4 | 5.8 | 5.8 | 4.2 | 5.7 | 3.5 | 5.7 | |||
| 10–20 | 7.4 | 7.8 | 5.8 | 8.7 | 5.7 | 9.2 | 6.4 | 8.0 | |||
| 21–30 | 14.7 | 16.8 | 13.4 | 13.9 | 14.1 | 15.3 | 15.0 | 14.5 | |||
| >30 | 72.9 | 72.1 | 75.0 | 71.7 | 76.0 | 69.9 | 75.1 | 71.8 | |||
|
Practice Type (%) |
0.95 | 0.58 | 0.88 | ||||||||
| Academic | 24.6 | 23.5 | 26.2 | 24.3 | 25.2 | 24.1 | 25.4 | 24.2 | |||
| Private | 54.4 | 57.5 | 52.3 | 53.2 | 54.6 | 54.2 | 52.0 | 55.6 | |||
| HMO | 7.3 | 6.2 | 8.1 | 7.5 | 5.7 | 8.8 | 8.1 | 6.8 | |||
| Family Planning/ Community Health Clinic |
13.7 | 12.9 | 13.4 | 15.0 | 14.5 | 13.0 | 14.5 | 13.4 | |||
| Region (%) | 0.80 | 0.43 | 0.19 | ||||||||
| Midwest | 31.7 | 27.9 | 32.6 | 34.7 | 34.4 | 29.0 | 37.6 | 28.8 | |||
| South | 30.2 | 29.6 | 31.4 | 29.5 | 29.4 | 30.9 | 29.5 | 30.5 | |||
| West | 19.5 | 21.8 | 17.4 | 19.1 | 17.2 | 21.8 | 16.2 | 21.1 | |||
| Northeast | 18.7 | 20.7 | 18.6 | 16.8 | 19.1 | 18.3 | 16.8 | 19.7 | |||
Recommendations for Levonorgestrel IUC
Significant interactions between patient race/ethnicity and gynecologic history (p=0.05) and patient SES and gynecologic history (p=0.04) were identified with respect to recommendations for the levonorgestrel IUC. As the woman with no perceived risk factors was of primary interest, we focused our analysis on this stratum (n=173). Analyzing race/ethnicity separately, low SES women were significantly less likely to have IUC recommended than were high SES women (57% vs. 75%, p=0.01). Black women were significantly more likely to have IUC recommended compared with White women (75% and 66% vs. 57%, p=0.04).
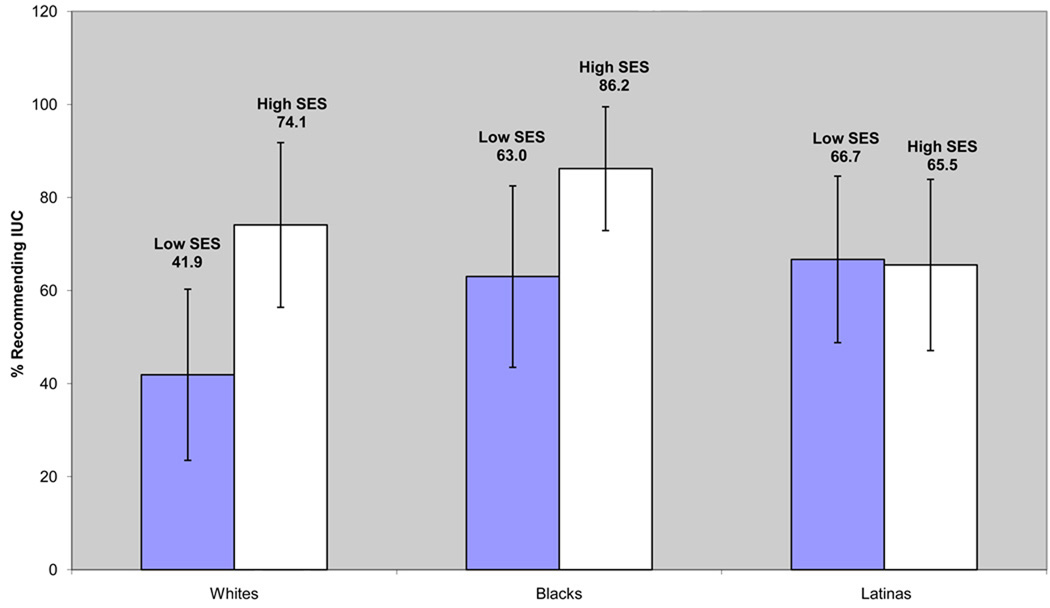
As an additional interaction between patient race/ethnicity and SES (p=0.02) was identified, Figure 2 presents the percent of providers recommending IUC stratified by both race/ethnicity and SES. A significant difference between low and high SES White women (p=0.01) and low and high SES Black women (p=0.04) was identified, with the low SES women being less likely to have IUC recommended. There was no difference by SES among Latinas (p=0.93). Within the low and high SES groups, respectively, there were no significant differences by race/ethnicity.
Figure 2.
Percent of Providers Recommending IUC to Women with No Perceived Risk Factors, Stratified by Patient SES and Race/Ethnicity (n=173)
The adjusted results are presented in Table 2. In multivariate analyses, the effect of SES on recommendations for IUC among White patients remained significant (p=0.009), while the difference between low SES and high SES Black women was no longer significant (p=0.12). The effect of race/ethnicity among low SES patients was more prominent in the multivariate model, with low SES Blacks and Latinas significantly more likely to have IUC recommended than low SES Whites (p=0.046 and p=0.03).Among high SES women there were no significant differences in recommendations by patient race/ethnicity.
Table 2.
Effect of Patient SES and Race/Ethnicity on Recommendations for IUC (OR, 95% CI)
| Unadjusted | Adjusted* | |
|---|---|---|
| SES Comparisons Within Race/Ethnicity | ||
| Low SES Whites (ref. high SES Whites) | 0.25 (0.08 to 0.77) | 0.20 (0.06 to 0.69) |
| Low SES Blacks (ref. high SES Blacks) | 0.27 (0.07 to 1.0) | 0.33 (0.08 to 1.3) |
| Low SES Latinas (ref. high SES Latinas) | 1.1 (0.36 to 3.1) | 1.1 (0.36 to 3.6) |
| Race/Ethnicity Comparisons Within SES | ||
| Low SES (ref. Low SES Whites) | ||
| Blacks | 2.4 (0.82 to 6.8) | 3.1 (1.0 to 9.6) |
| Latinas | 2.8 (0.98 to 7.8) | 3.4 (1.1 to 10.2) |
| High SES (ref. High SES Whites) | ||
| Blacks | 2.2 (0.56 to 8.5) | 1.9 (0.44 to 8.5) |
| Latinas | 0.67 (0.21 to 2.1) | 0.60 (0.17 to 2.1) |
Adjusted for provider sex, specialty, age, race/ethnicity, whether inserts IUC in his or her practice, and frequency of prescribing contraception.
Recommendations for Intrauterine Contraception in Women with Perceived Risk Factors
Differences by SES in recommendations for IUC were attenuated in comparisons of women with perceived risk factors for IUC in both bivariate and multivariate analysis. In contrast to the findings for the low-risk patients, for patients with perceived risk factors providers were as likely to recommend IUC to low SES White (adjusted OR 0.69, 95% CI 0.31 to 1.6) and low SES Black women (adjusted OR 0.99, 95% CI 0.45 to 2.2) as to their high SES counterparts. Similarly, the presence of a history of PID or nulliparity eliminated the effect of Black and Latina race/ethnicity among low SES women (adjusted OR 0.85, 95% CI 0.39 to 1.5 for low SES Blacks compared to low SES Whites and adjusted OR 1.5, 95% CI 0.64 to 3.4 for low SES Latinas compared to low SES Whites).
Providers’ Perceptions of Patients
The providers’ perceptions of the patients shown in the video, compared to “an average women her age” are shown in Table 3. Interactions between patient race/ethnicity and SES were identified in responses to two questions; for these questions stratified results are presented. Low SES patients were judged to be significantly more likely than high SES patients to have a sexually transmitted infection (STI) and an unintended pregnancy, and were also judged to be less knowledgeable. In contrast, providers’ perceptions did not differ by patient race/ethnicity for most items and only among high SES patients when differences were found. All significant differences identified in bivariate analysis were also significant in multivariate logistic regression.
Table 3.
Perceptions of Standardized Patients, by Patient Characteristics
| Provider Perceptions | White (%) |
Black (%) |
Latina (%) |
P value | High SES (%) |
Low SES (%) |
P value |
|---|---|---|---|---|---|---|---|
| Likely to have STI | 17.3 | 20.4 | 20.2 | 0.72 | 14.9 | 23.7 | 0.01 |
|
Likely to have unintended pregnancy |
16.2 | 14.5 | 16.8 | 0.84 | 11.1 | 20.6 | 0.003 |
|
Likely to forget > 2 pills/month |
17.3 | 12.2 | 15.0 | 0.40 | 14.1 | 15.6 | 0.62 |
| Knowledgeable | 55.3 | 64.0 | 66.5 | 0.08 | 69.1 | 54.6 | 0.001 |
| Intelligent* | |||||||
| High SES | 83.0 | 92.9 | 76.4 | 0.01 | -- | -- | -- |
| Low SES | 60.4 | 66.7 | 71.4 | 0.31 | -- | -- | -- |
| White | -- | -- | -- | -- | 83.0 | 60.4 | 0.001 |
| Black | -- | -- | -- | -- | 92.9 | 66.7 | <0.001 |
| Latina | -- | -- | -- | -- | 76.4 | 71.4 | 0.46 |
|
Likely to follow up with medical care+ |
|||||||
| High SES | 71.6 | 88.2 | 70.8 | 0.009 | -- | -- | -- |
| Low SES | 53.9 | 58.6 | 61.9 | 0.55 | -- | -- | -- |
| White | -- | -- | -- | -- | 71.6 | 53.9 | 0.01 |
| Black | -- | -- | -- | -- | 88.2 | 58.6 | <0.001 |
| Latina | -- | -- | -- | -- | 70.8 | 61.9 | 0.22 |
Significant interaction between race/ethnicity and SES (p=0.02)
Significant interaction between race/ethnicity and SES (p=0.05)
Comment
The study of health care disparities is complicated by the difficulty of controlling for all factors which are related both to the predictors of race/ethnicity and SES and to the relevant outcomes. The use of videos of standardized patients provides one of the best methods for minimizing confounding and varying only the sociodemographic factors of interest. Although this method has been used in several published studies,4 5 25–27 none of these prior studies applied this method to reproductive health decision making or investigated the interaction between patient race/ethnicity and SES.
Our stratified multivariate results indicate that providers are more likely to recommend IUC to Black and Latina women than to White women, but only when these women are of low SES. They are less likely to recommend IUC to a low SES woman than to a high SES woman, but only when the woman is White. Moreover, these patterns only seem to hold among women with no perceived risk factors for IUC.
The results of this study do not lend themselves to easy interpretation. While the contrary and interacting ways in which race/ethnicity and SES influence provider recommendations is one source of complexity, this pattern is itself of interest, as it underscores the importance of considering race/ethnicity and SES, both alone and in combination, in the study of health care disparities. In addition, the preference-sensitive nature of contraceptive decision-making does not allow for conclusions about whether one group is receiving better care. Regardless of the etiology or the interpretation of these differences, however, the finding of variation in recommendations to individuals who differ on no clinically relevant variables, but only on their race/ethnicity and SES, deserves attention. While contraceptive recommendations will and should vary by patient, and IUC may be the most appropriate method for many patients, it is important to consider whether patient’s race/ethnicity and SES should be a factor in these recommendations.
Possible explanations for the variation in recommendations for IUC by sociodemographic group include the presence of conscious or subconscious biases regarding the use of this method in certain groups. Alternatively, these results could indicate that providers are making assumptions about the appropriateness of IUC based on the patient’s SES or race not due to bias, but rather as a result of an overly broad application of probabilistic reasoning.28 This phenomenon - termed “statistical discrimination” – occurs when epidemiologic evidence or clinical experience is used to guide treatment decisions for patients within specific sociodemographic groups without the appropriate use of individualizing information.28
With respect to SES, one possible explanation for our findings is that providers perceived low SES patients to be at higher risk of an STI than high SES patients. As prior studies have documented that providers believe that providing IUCs to women at risk of STIs can lead to complications such as infertility,17 18 the lower likelihood of recommending this method to low SES Whites compared to high SES Whites could be related to this perception. As there is evidence that in fact there is an epidemiologic association between SES and risk for STIs,29 this can be interpreted as an example of statistical discrimination, in that knowledge of this association appears to be influencing providers’ decision-making despite the lack of any differences in the histories of the low SES and high SES White patient. The finding that there was no significant differences in recommendations between low and high SES Latina and Black patients could indicate that providers consider the perceived risk of infertility differently in White than in minority patients.
The findings that low SES Black and Latina women were more likely to have IUC recommended could be interpreted as indicating that providers have a bias towards use of this method in minority populations. Alternatively, this could result from the use of race-and ethnicity-based assumptions about the acceptability or appropriateness of IUC which are unrelated to bias. Regardless of the underlying causes of these differences, the increased odds of recommending IUC to Black and Latina women is of concern given the historical relationship of efforts to promote contraception with attempts to limit the fertility of minority and poor women in the United States.30 31 Providers recommending highly effective pregnancy prevention methods in a differential manner by race/ethnicity could be perceived negatively by communities and individuals aware of these issues.32 These findings are consistent with one previous study of physician behaviors, in which physicians provided with clinical vignettes were more willing to sterilize Black women than White women.13 In addition, several studies of patient experiences of contraceptive counseling have found that Black and Latina women more frequently report being encouraged to limit their family size and use contraceptive methods than Whites.11 12 33
The finding that being of higher SES eliminated the effect of race/ethnicity on recommendations for the levonorgestrel IUC may indicate that being of high SES equalizes perceptions across racial/ethnic categories. Similarly, the attenuation of differences in recommendations by both race/ethnicity and SES by the presence of gynecologic characteristics historically considered to be risk factors related to use of IUC may indicate that these risk factors are of greater importance to providers than their differing perceptions of patients by sociodemographic characteristics.
Limitations of our study include the difficulty of ensuring blinding of study participants to our interest in measuring disparities, given the previous publication of reports of studies with similar methodologies. While we had no indication from participants that this awareness existed, we anticipate that, if present, it would result in a conservative bias. The use of a convenience sample obtained at meetings of professional medical societies could affect the generalizability of our results. There is also the possibility that providers would be less likely to recommend IUC to low SES women because of concern about insurance coverage. We consider this unlikely due to the information provided to the participants that the patient had insurance which would pay for all the methods. An additional limitation is our inability to explore the effect of racial/ethnic concordance between providers and patients on recommendations for IUC due to the limited number of non-White health care providers in our sample. Finally, the use of an experimental design with videos of standardized patients may not accurately capture the recommendations of providers in their actual clinical practice.
Our results suggest that providers of contraception, policy makers and advocates should be vigilant and aware of the potential effect of patient sociodemographic characteristics on contraceptive recommendations. On one hand, our study suggests that there may be barriers to providing IUC to low SES White women which should be specifically addressed by these efforts. From another perspective, our results draw attention to the need for historical and cultural sensitivity in the promotion of this highly effective contraceptive method among minorities. Future research could address whether and how much provider recommendations contribute to disparities in contraception use, as well as determine what types of interventions may alleviate differences in recommendations. These studies should build on research in other fields which suggest that enhancing provider awareness of the presence and effect of stereotyping and promoting an emphasis on patient-centered care may be of use in decreasing health care disparities.9 34
Acknowledgements
The authors would like to thank Alison Perencevich, BA for her assistance with data collection.
Funding: This project was supported by the Fellowship in Family Planning. This project was also supported by NIH/NCRR/OD UCSF-CTSI Grant Number KL2 RR024130. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Presentation Information: Data presented in this manuscript have been presented in preliminary form at the annual meeting of the Association of Reproductive Health Professionals in October, 2009 in Los Angeles, CA.
References
- 1.Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, D.C.: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.van Ryn M, Fu SS. Paved with good intentions: do public health and human service providers contribute to racial/ethnic disparities in health? Am J Public Health. 2003;93(2):248–255. doi: 10.2105/ajph.93.2.248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sabin JA, Rivara FP, Greenwald AG. Physician implicit attitudes and stereotypes about race and quality of medical care. Med Care. 2008;46(7):678–685. doi: 10.1097/MLR.0b013e3181653d58. [DOI] [PubMed] [Google Scholar]
- 4.McKinlay J, Link C, Marceau L, O'Donnell A, Arber S, Adams A, et al. How do doctors in different countries manage the same patient? Results of a factorial experiment. Health Serv Res. 2006;41(6):2182–2220. doi: 10.1111/j.1475-6773.2006.00595.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schulman KA, Berlin JA, Harless W, Kerner JF, Sistrunk S, Gersh BJ, et al. The effect of race and sex on physicians' recommendations for cardiac catheterization. N Engl J Med. 1999;340(8):618–626. doi: 10.1056/NEJM199902253400806. [DOI] [PubMed] [Google Scholar]
- 6.van Ryn M, Burgess D, Malat J, Griffin J. Physicians' perceptions of patients' social and behavioral characteristics and race disparities in treatment recommendations for men with coronary artery disease. Am J Public Health. 2006;96(2):351–357. doi: 10.2105/AJPH.2004.041806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bao Y, Fox SA, Escarce JJ. Socioeconomic and racial/ethnic differences in the discussion of cancer screening: "between-" versus "within-" physician differences. Health Serv Res. 2007;4(3 Pt 1):950–970. doi: 10.1111/j.1475-6773.2006.00638.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Griggs JJ, Culakova E, Sorbero ME, Poniewierski MS, Wolff DA, Crawford J, et al. Social and racial differences in selection of breast cancer adjuvant chemotherapy regimens. J Clin Oncol. 2007;25(18):2522–2527. doi: 10.1200/JCO.2006.10.2749. [DOI] [PubMed] [Google Scholar]
- 9.Burgess D, van Ryn M, Dovidio J, Saha S. Reducing racial bias among health care providers: lessons from social-cognitive psychology. J Gen Intern Med. 2007;22(6):882–887. doi: 10.1007/s11606-007-0160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krupat E, Irish JT, Kasten LE, Freund KM, Burns RB, Moskowitz MA, et al. Patient assertiveness and physician decision-making among older breast cancer patients. Soc Sci Med. 1999;49(4):449–457. doi: 10.1016/s0277-9536(99)00106-9. [DOI] [PubMed] [Google Scholar]
- 11.Borrero S, Schwarz EB, Creinin M, Ibrahim S. The impact of race and ethnicity on receipt of family planning services in the United States. J Womens Health (Larchmt) 2009;18(1):91–96. doi: 10.1089/jwh.2008.0976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Downing RA, LaVeist TA, Bullock HE. Intersections of ethnicity and social class in provider advice regarding reproductive health. Am J Public Health. 2007;97(10):1803–1807. doi: 10.2105/AJPH.2006.092585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harrison DD, Cooke CW. An elucidation of factors influencing physicians' willingness to perform elective female sterilization. Obstet Gynecol. 1988;72(4):565–570. [PubMed] [Google Scholar]
- 14.Chandra A, Martinez GM, Mosher WD, Abma JC, Jones J. Fertility, family planning, and reproductive health of U.S. women: data from the 2002 National Survey of Family Growth. Vital Health Stat 23. 2005;25:1–160. [PubMed] [Google Scholar]
- 15.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38(2):90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 16.Hatcher RA. Contraceptive technology. 19th rev. ed. New York, N.Y.: Ardent Media; 2007. [Google Scholar]
- 17.Stanwood NL, Garrett JM, Konrad TR. Obstetrician-gynecologists and the intrauterine device: a survey of attitudes and practice. Obstet Gynecol. 2002;99(2):275–280. doi: 10.1016/s0029-7844(01)01726-4. [DOI] [PubMed] [Google Scholar]
- 18.Harper CC, Blum M, de Bocanegra HT, Darney PD, Speidel JJ, Policar M, et al. Challenges in translating evidence to practice: the provision of intrauterine contraception. Obstet Gynecol. 2008;111(6):1359–1369. doi: 10.1097/AOG.0b013e318173fd83. [DOI] [PubMed] [Google Scholar]
- 19.Hubacher D, Lara-Ricalde R, Taylor DJ, Guerra-Infante F, Guzman-Rodriguez R. Use of copper intrauterine devices and the risk of tubal infertility among nulligravid women. N Engl J Med. 2001;345(8):561–567. doi: 10.1056/NEJMoa010438. [DOI] [PubMed] [Google Scholar]
- 20.Farley TM, Rosenberg MJ, Rowe PJ, Chen JH, Meirik O. Intrauterine devices and pelvic inflammatory disease: an international perspective. Lancet. 1992;339(8796):785–788. doi: 10.1016/0140-6736(92)91904-m. [DOI] [PubMed] [Google Scholar]
- 21.MacIsaac L, Espey E. Intrauterine contraception: the pendulum swings back. Obstet Gynecol Clin North Am. 2007;34(1):91–111. doi: 10.1016/j.ogc.2007.02.004. ix. [DOI] [PubMed] [Google Scholar]
- 22.Hubacher D, Vilchez R, Gmach R, Jarquin C, Medrano J, Gadea A, et al. The impact of clinician education on IUD uptake, knowledge and attitudes: results of a randomized trial. Contraception. 2006;73(6):628–633. doi: 10.1016/j.contraception.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 23.Trussell J. Contraceptive efficacy. In: Hatcher R, Trussell J, Nelson A, Cates W, Stewart F, Kowal D, editors. Contraceptive Technology. 19th ed. New York, NY: Ardent Media; 2007. [Google Scholar]
- 24.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 25.McKinlay JB, Burns RB, Durante R, Feldman HA, Freund KM, Harrow BS, et al. Patient, physician and presentational influences on clinical decision making for breast cancer: results from a factorial experiment. J Eval Clin Pract. 1997;3(1):23–57. doi: 10.1111/j.1365-2753.1997.tb00067.x. [DOI] [PubMed] [Google Scholar]
- 26.Woo JK, Ghorayeb SH, Lee CK, Sangha H, Richter S. Effect of patient socioeconomic status on perceptions of first- and second-year medical students. CMAJ. 2004;170(13):1915–1919. doi: 10.1503/cmaj.1031474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.McKinlay JB, Link CL, Freund KM, Marceau LD, O'Donnell AB, Lutfey KL. Sources of variation in physician adherence with clinical guidelines: results from a factorial experiment. J Gen Intern Med. 2007;22(3):289–296. doi: 10.1007/s11606-006-0075-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balsa AI, McGuire TG, Meredith LS. Testing for statistical discrimination in health care. Health Serv Res. 2005;40(1):227–252. doi: 10.1111/j.1475-6773.2005.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Krieger N, Waterman PD, Chen JT, Soobader MJ, Subramanian SV. Monitoring socioeconomic inequalities in sexually transmitted infections, tuberculosis, and violence: geocoding and choice of area-based socioeconomic measures--the public health disparities geocoding project (US) Public Health Rep. 2003;118(3):240–260. doi: 10.1093/phr/118.3.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stern AM. Sterilized in the name of public health: race, immigration, and reproductive control in modern California. Am J Public Health. 2005;95(7):1128–1138. doi: 10.2105/AJPH.2004.041608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Critchlow DT. Birth control, population control, and family planning: an overview. J Policy Hist. 1995;7(1):1–21. doi: 10.1017/s0898030600004127. [DOI] [PubMed] [Google Scholar]
- 32.Thorburn S, Bogart LM. Conspiracy beliefs about birth control: barriers to pregnancy prevention among African Americans of reproductive age. Health Educ Behav. 2005;32(4):474–487. doi: 10.1177/1090198105276220. [DOI] [PubMed] [Google Scholar]
- 33.Becker D, Tsui AO. Reproductive health service preferences and perceptions of quality among low-income women: racial, ethnic and language group differences. Perspect Sex Reprod Health. 2008;40(4):202–211. doi: 10.1363/4020208. [DOI] [PubMed] [Google Scholar]
- 34.Beach MC, Rosner M, Cooper LA, Duggan PS, Shatzer J. Can patient-centered attitudes reduce racial and ethnic disparities in care? Acad Med. 2007;82(2):193–198. doi: 10.1097/ACM.0b013e31802d94b2. [DOI] [PMC free article] [PubMed] [Google Scholar]