Abstract
We present a case that demonstrates the rare occurrence of type 1 second-degree atrioventricular block (Wenckebach or Mobitz type 1 block) as a result of block in the infranodal conduction system. This extremely rare occurrence often predicts progression to complete heart block and necessitates cardiac pacing. It also demonstrates the value of an electrophysiological study and exercise stress testing to identify the level of block, predict prognosis, and plan a management strategy.
Wenckebach phenomenon, or type 1 second-degree atrioventricular (AV) block, is a common type of AV block in which there is a delay in transmission of impulses from the atria to the ventricles. It was first described by Karel Frederik Wenckebach in 1893, before the invention of the electrocardiogram and the discovery of the sinoatrial and AV node. Wenckebach postulated that this block occurred due to decreased conduction at the AV border. The most common site of type 1 second-degree AV block, or Wenckebach phenomenon, is at the AV node. We describe a case in which the block occurred below the AV node, a location not originally described by Wenckebach.
CASE DESCRIPTION
An 83-year-old man with hypertension and diabetes mellitus presented with worsening chest pain, dyspnea, and bilateral lower-extremity edema. Bibasilar rales and a harsh late-peaking systolic murmur at the left upper sternal border were present.
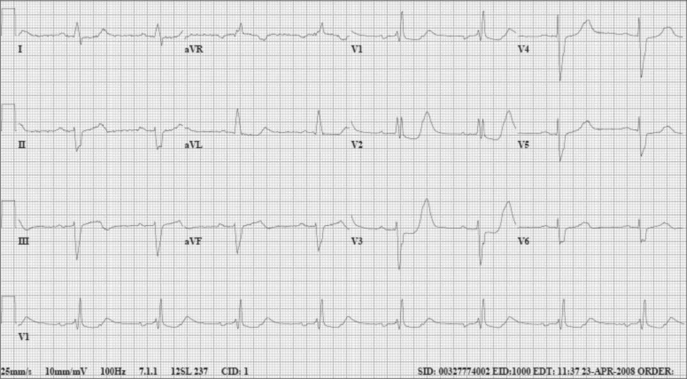
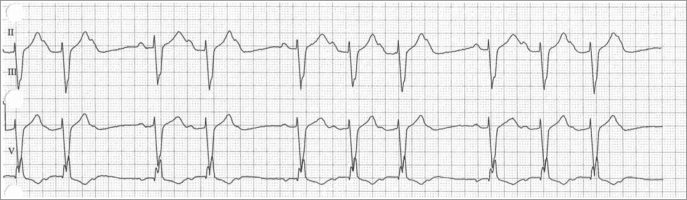
The initial 12-lead electrocardiogram showed sinus rhythm with 2:1 AV block, right bundle branch block, left anterior fascicular block, and ST-segment depression in precordial leads V1 to V3 (Figure 1). An echocardiogram showed inferior wall hypokinesis, moderate to severe aortic stenosis, and a left ventricular ejection fraction of approximately 45%. The patient's troponin levels were elevated. Cardiac catheterization showed localized narrowing of the left circumflex coronary artery, and a stent was inserted. After catheterization, telemetry revealed type 1 second-degree AV block (Wenckebach or Mobitz type 1 block) (Figure 2). The AV block appeared to worsen with increasing heart rate.
Figure 1.
The patient's 12-lead electrocardiogram.
Figure 2.
Telemetry strip showing Wenckebach or Mobitz type 1 block.
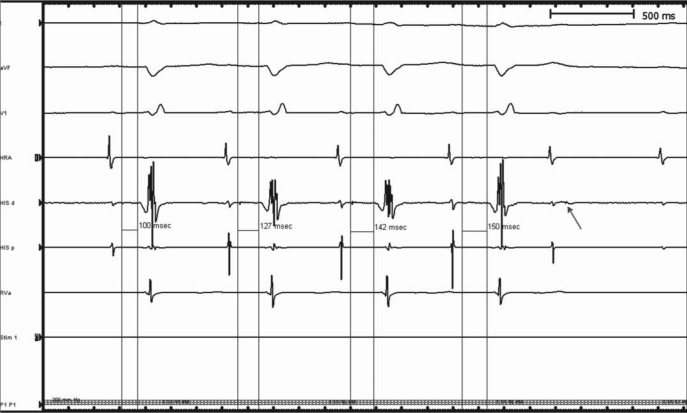
An electrophysiological study showed an atrial-His interval of 80 msec (normal, 55–125 msec) and His-ventricular interval of 100 msec (normal, 35–55 msec). The His-ventricular interval exhibited Wenckebach periodicity (Figure 3). A dual-chamber pacemaker was implanted.
Figure 3.
Prolonged HV interval exhibiting Wenckebach periodicity.
DISCUSSION
Wenckebach periodicity is almost always seen at the level of the AV node. The case described herein demonstrates that, although uncommon, Wenckebach block may occur at the infranodal level. The presence of bifascicular block and worsening AV block with increasing heart rates should raise the suspicion of infranodal Wenckebach with the attendant risk of progression to complete heart block.
Wenckebach
Wenckebach (1864–1940) (Figure 4) was born in The Hague, Netherlands (1). He entered medical school at the University of Utrecht in 1881. In 1888, after graduation, he initially taught zoology but quickly switched to physiology due to his color blindness. He worked with Theodur Engelmann, a prominent cardiac electrophysiologist, inducing arrhythmias in frogs. Wenckebach became familiar with the techniques of kymographic recordings and rhythm disturbances in frog experiments while working in Engelmann's laboratory (1, 2).
Figure 4.
Karel Frederik Wenckebach.
Wenckebach left Utrecht and started medical practice in Heerlen in 1891. He became a prominent physician with a keen interest in irregular pulses. He returned to Utrecht in 1896 to resume his research and continue investigating arrhythmias. He reported that ventricular extrasystoles with compensatory pauses that occurred in nonhumans were also seen in humans. He went on to show that atrial extrasystoles were not accompanied by compensatory pauses.
In 1898, he was consulted by a 40-year-old woman who was bothered by an irregular pulse. He studied her radial artery pulse tracings using a sphygmogram and a tuning fork. He noted that there were regular pauses every 3 to 4 beats, but the small extra pulse seen during pauses after extrasystoles was absent. The first interval after each pause was longer, and subsequent intervals were shorter. Wenckebach called this pattern of repeated changing pulse intervals that were grouped together “Luciani periods” after physiologist Luigi Luciani, who had described similar grouped beats in frogs in 1873 (3). Based on his observations of the radial artery tracing, Wenckebach made the following conclusions: there were groups of beats; the length of the pauses was less than twice the interval between the preceding pulses; the interval between the first two pulses after the pause was longer than the other pulse interval; and there was no evidence of extrasystole.
Engelmann provided Wenckebach with frog heart tracings from 1893, in which he was able to measure the time between atrial and ventricular contractions. On analyzing these data, Wenckebach noted that the time between the atrial and ventricular contractions increased gradually until a ventricular contraction was absent. After the pause, the AV conduction time was the shortest. Tracings from the frog heart also showed that the greatest increase in the AV pulse interval occurred in the second beat after the pause. He postulated that the group beating, along with changes in the AV conduction, was a result of decreased conduction at the AV border. The radial artery pulse tracing in his patient was very similar to the tracing that he noted in the data from Engelmann's laboratory. Wenckebach was able to construct “a model of heart action” based on his study of the radial artery and polygraph tracing from frogs hearts.
Finally, in 1906, Wenckebach used the electrocardiogram to prove the progressive prolongation of the PR interval before a dropped ventricular complex, which is now described as the Wenckebach phenomenon. In the same year, the AV node was first described by Tawara. The concept of “partial” vs “complete” block had been introduced by Gaskell in 1883 after he removed atrial tissue from a tortoise and noted that if the block was severe, then instead of every contraction passing the blocking point, every other contraction was able to pass (4). In 1906, Hay, in England, noted a different kind of Wenckebach block, where the AV interval did not prolong before the blocked beat.
Woldemar Mobitz from Germany, in 1924, finally classified partial AV block into type 1, or Wenckebach periodicity, and type 2 AV block noted earlier by Hay (5). Mobitz noted that type 1 block was reversible, and the autopsy studies did not show significant AV node or His bundle disease. He believed that type 2 block was associated with significant structural damage to the bundle. In 1969, Scherlag introduced the His bundle recording, which helped in localizing the exact site of disease in AV blocks as either proximal or distal to the His bundle. The Wenckebach type of AV block was found to be proximal to the His bundle, as predicted by Mobitz in 1924.
Wenckebach phenomenon and other blocks
The Wenckebach phenomenon, or Mobitz type 1 AV block, is one of the most common eponyms used in medicine. The diagnostic criteria, which have not changed since Wenckebach described them, are progressive prolongation of the PR interval and shortening of the RR interval until a P wave is blocked; an RR interval containing the nonconducted P wave that is less than the sum of two PP intervals; and group beating due to the presence of the nonconducted P wave.
During a typical type 1 block, the increment in conduction time is greatest in the second beat of the Wenckebach group, and the absolute increase in conduction time decreases progressively over subsequent beats. Variations from the classic description of type 1 block are seen with higher ratio blocks, such as 7:6 or 11:10, and with variations in the sinus rate, as seen with sinus arrhythmias. Type 1 block is commonly seen in people who have a high vagal tone, such as young people or athletes at rest. It is also seen in patients with inferior wall acute myocardial infarction, Chagas disease, and AV nodal disease and in those who have had mitral valve surgery. Type 1 second-degree block is generally benign. When type 1 AV block occurs with bifascicular block, however, the risk of progression to complete heart block is significantly increased because of probable infranodal disease. Mobitz type 1 block, or Wenckebach phenomenon, usually occurs at the AV node and is also considered benign. On the other hand, type 2 second-degree AV block is more likely infranodal, and the site of block is in the His-Purkinje system in 30% and in the bundle branches in the remainder.
Electrophysiological testing allows analysis of conduction abnormalities, the His bundle, and the ventricular electrogram. As such, it is valuable in identifying the level of block, determining prognosis, and planning a management strategy. Evidence of worsening conduction with increasing heart rates, as with exercise testing or exertion or with atropine, predicts intra- or infrahisian block and often requires cardiac pacing. The infrahisian system, which comprises the main bundle branches, fascicles, and the Purkinje network, is the source of most clinically important heart block in adults and is measured by the His-ventricular interval on an electrophysiological study.
Normally the His-ventricular interval, which represents conduction time from the proximal His bundle to the ventricular myocardium, should not exceed 55 to 60 msec. A prolonged His-ventricular interval is almost always associated with an abnormal QRS. A markedly prolonged His-ventricular interval over 100 msec is associated with a high incidence (up to 12%) of progression to complete heart block (6). This almost universally manifests as second-degree type 2 AV block on the surface 12-lead electrocardiogram and only rarely as second-degree type 1 AV block. In the presence of second-degree type 1 AV block, a gradual prolongation of the HV interval occurs until an AH group is not followed by a ventricular depolarization. The HV interval shortens following a blocked impulse. This is, however, much less common than second-degree type 2 AV block or 2:1 block. In the presence of a type 2 block, infrahisian block occurs in the absence of progressive HV prolongation and is typically sudden and unexpected.
Our patient had evidence of a diseased conduction system on his baseline electrocardiogram, with sinus rhythm with 2:1 AV block and bifascicular block (right bundle branch block and left anterior hemiblock). His electrophysiology study also revealed a baseline His-ventricular interval of 100 msec. The finding of type 1 second-degree AV block in the infrahisian system is extremely rare. Bifascicular block (especially right bundle branch block and left anterior hemiblock) is the most common pattern on electrocardiogram that precedes complete heart block in adults. The incidence of progression to complete heart block ranges from 2% in asymptomatic patients with an intraventricular conduction delay to approximately 6% in patients with an intraventricular conduction delay and neurological symptoms like syncope (7, 8). Clinically, second-degree block in the intrahisian or infrahisian system is indicative of impending high-grade or complete heart block, which may occur paroxysmally, and hemodynamic survival depends on the emergence of a low junctional (distal His), fascicular, or idioventricular rhythm. If the escape rhythm is slow, the patient might present with syncope. The American College of Cardiology/American Heart Association guidelines for permanent pacing in chronic bifascicular block classify an incidental finding at electrophysiological study of a markedly prolonged HV interval (≥100 msec) in asymptomatic patients as a class IIa indication for permanent pacing (9).
References
- 1.Silverman ME, Upshaw CB., Jr Karel Frederik Wenckebach and partial atrioventricular block. ACC Current J Rev. 2000;9(3):13–17. [Google Scholar]
- 2.Upshaw CB, Jr, Silverman ME. The Wenckebach phenomenon: a salute and comment on the centennial of its original description. Ann Intern Med. 1999;130(1):58–63. doi: 10.7326/0003-4819-130-1-199901050-00011. [DOI] [PubMed] [Google Scholar]
- 3.Upshaw CB, Jr, Silverman ME. Luigi Luciani and the earliest graphic demonstration of Wenckebach periodicity. Circulation. 2000;101(22):2662–2668. doi: 10.1161/01.cir.101.22.2662. [DOI] [PubMed] [Google Scholar]
- 4.Silverman ME, Upshaw CB., Jr Walter Gaskell and the understanding of atrioventricular conduction and block. J Am Coll Cardiol. 2002;39(10):1574–1580. doi: 10.1016/s0735-1097(02)01839-9. [DOI] [PubMed] [Google Scholar]
- 5.Silverman ME, Upshaw CB, Jr, Lange HW. Woldemar Mobitz and his 1924 classification of second-degree atrioventricular block. Circulation. 2004;110(9):1162–1167. doi: 10.1161/01.CIR.0000140669.35049.34. [DOI] [PubMed] [Google Scholar]
- 6.Scheinman MM, Peters RW, Suavé MJ, Desai J, Abbott JA, Cogan J, Wohl B, Williams K. Value of the H-Q interval in patients with bundle branch block and the role of prophylactic permanent pacing. Am J Cardiol. 1982;50(6):1316–1322. doi: 10.1016/0002-9149(82)90469-6. [DOI] [PubMed] [Google Scholar]
- 7.Imanishi R, Seto S, Ichimaru S, Nakashima E, Yano K, Akahoshi M. Prognostic significance of incident complete left bundle branch block observed over a 40-year period. Am J Cardiol. 2006;98(5):644–648. doi: 10.1016/j.amjcard.2006.03.044. [DOI] [PubMed] [Google Scholar]
- 8.McCullough PA, Hassan SA, Pallekonda V, Sandberg KR, Nori DB, Soman SS, Bhatt S, Hudson MP, Weaver WD. Bundle branch block patterns, age, renal dysfunction, and heart failure mortality. Int J Cardiol. 2005;102(2):303–308. doi: 10.1016/j.ijcard.2004.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, 3rd, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Faxon DP, Halperin JL, Hiratzka LF, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura RA, Ornato JP, Page RL, Riegel B, Tarkington LG, Yancy CW, American College of Cardiology/American Heart Association Task Force on Practice Guidelines. American Association for Thoracic Surgery. Society of Thoracic Surgeons ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities. J Am Coll Cardiol. 2008;51(21):e1–e62. doi: 10.1016/j.jacc.2008.02.032. [DOI] [PubMed] [Google Scholar]