Abstract
OBJECTIVE: To evaluate whether the addition of a physician assessment of patient fall risk at admission would reduce inpatient falls on a tertiary hospital neurology inpatient unit.
PATIENTS AND METHODS: A physician fall risk assessment was added to the existing risk assessment process (clinical nurse evaluation and Hendrich II Fall Risk Model score with specific fall prevention measures for patients at risk). An order to select either “Patient is” or “Patient is not at high risk of falls by physician assessment” was added to the physician electronic admission order set. Nurses and physicians were instructed to reach consensus when assessments differed. Full implementation occurred in second-quarter 2008. Preimplementation (January 1, 2006, to March 31, 2008) and postimplementation (April 1, 2008, to December 31, 2009) rates of falls were compared on the neurology inpatient unit and on 6 other medical units that did not receive intervention.
RESULTS: The rate of falls during the 7 quarters after full implementation was significantly lower than that during the 9 preceding quarters (4.12 vs 5.69 falls per 1000 patient-days; P=.04), whereas the rate of falls on other medical units did not significantly change (2.99 vs 3.33 falls per 1000 patient-days; P=.24, Poisson test). The consensus risk assessment at admission correctly identified patients at risk for falls (14/325 at-risk patients fell vs 0/147 low-risk patients; P=.01, χ2 test), but the Hendrich II Fall Risk Model score, nurse, and physician assessments individually did not.
CONCLUSION: A multidisciplinary approach to fall risk assessment is feasible, correctly identifies patients at risk, and was associated with a reduction in inpatient falls.
These authors found that a multidisciplinary approach to fall risk assessment is feasible, correctly identifies patients at risk, and is associated with a reduction in inpatient falls.
Falls are the most common adverse event reported in acute care settings.1,2 They prolong hospitalization, increase cost of care, and have the potential to cause serious injury.3 Multiple risk factors for falls have been identified: advanced age, muscle weakness, gait or balance problems, visual impairment, altered bowel or bladder elimination patterns, dizziness or vertigo, depression, cognitive deficits, impaired activities of daily living, use of psychotropic medications, and a history of falls.1,4-7 These risk factors are common among patients with neurologic disease. For this reason, several specific neurologic conditions, such as stroke, dementia, Parkinson disease, and peripheral neuropathy, confer an increased risk for falls,8 and neurology inpatient units have among the highest rates of falls.9
Among hospitalized patients, rates of falls range from 1.97 to 8.40 falls per 1000 patient-days.9-13 The rate of falls on our neurology inpatient unit was 5.69 falls per 1000 patient-days during 2006 and 2007. The objective of this study was to evaluate whether the addition of a physician fall risk assessment to the existing nurse fall risk assessment process was feasible and whether it would lead to a reduction in our inpatient rate of falls. Our hypothesis was that adding a physician assessment would increase the number of neurology inpatients identified as at risk for falls, leading to more patients receiving fall prevention measures and, ultimately, a reduction in rate of falls.
PATIENTS AND METHODS
This controlled pre-post quality improvement study was performed at a tertiary hospital (Saint Marys Hospital, Rochester, MN). The intervention group comprised adult patients with neurologic and cerebrovascular diseases hospitalized on the neurology inpatient unit. The control group comprised adult patients hospitalized on 6 other medical inpatient units (general internal medicine, gastroenterology, and pulmonary services) who did not receive our intervention and did not have continuous cardiac monitoring. The Mayo Clinic Institutional Review Board approved this study.
Existing Fall Risk Assessment Process
All inpatient units at our institution use a standard fall risk assessment process. This involves calculation of the Hendrich II Fall Risk Model score by nurses for each patient at admission and at least daily thereafter. Physicians were not expected to perform or document a fall risk assessment as part of their admissions process. The Hendrich II Fall Risk Model score is one of many fall risk assessment tools designed to identify patients at risk for falls.14,15 This tool was adopted for institution-wide use as a standard part of the nursing fall risk assessment in August 2005. It includes screening for 7 fall risk factors (confusion, disorientation, or impulsivity; symptomatic depression; altered bowel or bladder elimination; dizziness or vertigo; male sex; any administered antiepileptic; and any administered benzodiazepine) and a functional mobility assessment (Get Up and Go Test).1,16 Each fall risk factor is assigned a point value based on how much it contributed to increased fall risk in a multivariate model. Potential scores range from 0 to 16. A score of 5 or more indicates increased risk of falls, with such patients having a rate of falls that is 14 times that of patients with a score of 0.1
Patients designated at risk on the basis of either a clinical nurse assessment or a Hendrich II Fall Risk Model score of 5 or more receive specific fall prevention measures as part of an individualized patient care plan. These are selected by the nurse and could include assisting with ambulation, placing the call light within easy reach, instructions to call for assistance with movement, placing the hospital bed in its lowest position, selecting appropriate side rail use, providing an appropriate level of surveillance, or using bed and chair alarms. A sign indicating risk of falls is also placed at the patient's door. All patients, regardless of risk, receive fall prevention patient education materials. Screening for risk of injury from a fall was added to the standard institution-wide nurse fall risk assessment process in November 2009.
Intervention
Our intervention consisted of adding a physician fall risk assessment for all patients at admission to the neurology unit. Physicians were instructed to make this judgment on the basis of their usual admission history taking and physical examination and were blinded to the nursing fall risk assessment. An order requiring the admitting physician to then select either “Patient is” or “Patient is not at high risk of falls by physician assessment” was added to the neurology electronic admission order set. When a discrepancy between nurse and physician fall risk assessments occurred, the nurse and physician were instructed to reach a consensus risk designation. At our institution, patients are admitted to the inpatient neurology unit by residents who rotate every 4 to 5 weeks. Residents are from both neurology and nonneurology (internal medicine, neurosurgery, psychiatry, and physical medicine and rehabilitation) training programs. Nurse coordinators reviewed the physician fall risk assessment process with all residents at the beginning of every rotation, using a single-page handout that emphasized the importance of fall risk assessment, summarized the existing fall risk assessment process performed by nurses, and explained the nature of our intervention, including the expectation that they perform their own fall risk assessment.
The physician fall risk assessment order was added to the neurology electronic order set in January 2008. The resident education process began at the same time. The project was also introduced to nurses in January 2008. Given initial unfamiliarity with the new process, efforts were made during first-quarter 2008 to educate nurses about the need to review the physician fall risk assessment order and how to reconcile their risk assessment with that of the physician. The intervention was fully implemented during second-quarter 2008. Because of an institution-wide change to the nurse fall risk assessment process in the middle of fourth-quarter 2009, data collection ended on December 31, 2009.
Data Collection
Preimplementation (January 1, 2006, to March 31, 2008) and postimplementation (April 1, 2008, to December 31, 2009) rates of falls on the neurology inpatient unit were determined by using an established institutional process. Data from this system are reported quarterly as number of falls per 1000 patient-days. For the purposes of this system, a fall is defined as a fall to the floor, including instances when a member of the health care team helps guide or ease the patient to the floor. Patient-days are derived from hospital administrative data, which do not include patient demographics (eg, age and sex) or other patient-specific information (eg, reason for admission, comorbid conditions, medications, Hendrich II Fall Risk Model scores). The combined rates of falls from the 6 other medical units that did not receive our intervention were also determined during the same time frames.
A data collection card was developed to document nurse, physician, and consensus fall risk assessments for measurement purposes. Data recorded on the card included the following: (1) the admission Hendrich II Fall Risk Model score; (2) nurse fall risk assessment (not done, low risk, or at risk); (3) physician fall risk assessment (not done, low risk, or at risk); and (4) consensus fall risk designation. A card was to be completed by inpatient nurse coordinators for every admission to the neurology service within the first 24 hours.
Cards were first implemented on a trial basis between January and April 2008. On the basis of feedback from nurses, adjustments were made to the cards to improve clarity and ease of use. Nurses also received instructions on how to correctly complete cards during this time. A revised card was introduced in April 2008, and completed cards were reviewed for accuracy. Once accuracy was ensured, data cards were collected from May 1, 2008, to February 28, 2009. No other changes were made to the fall risk assessment process or to the fall prevention measures used on the neurology inpatient unit for at-risk patients during this time.
Statistical Analyses
Our primary outcome was the rate of falls on the inpatient neurology unit during the postimplementation period that extended from April 1, 2008, to December 31, 2009. Given that falls are rare events compared with the number of admissions, the number of falls over time was assumed to follow a Poisson distribution. Ratios of 2 Poisson rates using preintervention and postintervention rates of falls on the neurology inpatient unit and of the combined rates of falls on the 6 control medical inpatient units during the same time frames were tested by using the uniformly most powerful and unbiased test approach as described by Lehmann and Romano.17
Other outcomes were as follows: (1) the number of admissions to the neurology unit identified as at risk for falls by the Hendrich II Fall Risk Model score, nurses, and physicians individually and after consensus; (2) the number of falls among patients designated as at risk by the Hendrich II Fall Risk Model score, nurses, and physicians individually and after consensus; (3) the number of times there was a discrepancy between the nurse and physician fall risk assessments; (4) whether the nurse or physician assessment was more likely to determine the consensus admission fall risk designation; and (5) whether the addition of a physician fall risk assessment significantly increased the number of patients admitted to the neurology unit who were identified as at risk. These outcomes were reported as proportions, and a 2-tailed χ2 test was used to compare proportions between 2 groups. Admissions were considered an independent unit of analysis. All tests were 2-sided, and P<.05 was considered statistically significant.
Finally, we reviewed the data collection cards of the neurology inpatients who fell during the study period and had provided authorization for use of their medical records in research so that we could determine whether they had been identified as at risk for falls at admission by the Hendrich II Fall Risk Model score, nurse, or physician.
RESULTS
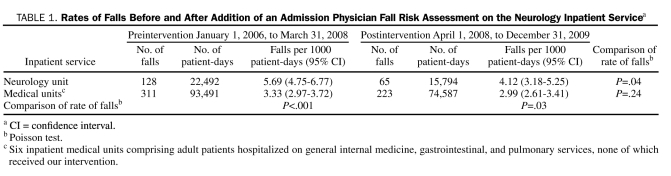
Falls, patient-days, and rates of falls for the neurology unit and 6 combined medical inpatient units before and after our intervention are shown in Table 1. The rate of falls during the 9 quarters before full implementation was 5.69 falls per 1000 patient-days. The rate of falls during the 7 quarters after full implementation was significantly lower at 4.12 falls per 1000 patient-days (P=.04). In contrast, the combined rate of falls on the 6 other medical units that did not receive our intervention showed no significant change during the same time frame (3.33 vs 2.99 falls per 1000 patient-days; P=.24). Before our intervention, the rate of falls on the neurology inpatient unit was significantly higher than that on the other 6 medical units (5.69 vs 3.33 falls per 1000 patient-days; P<.001). After our intervention, this difference, while still significant, had decreased (4.12 vs 2.99 falls per 1000 patient days; P=.03).
TABLE 1.
Rates of Falls Before and After Addition of an Admission Physician Fall Risk Assessment on the Neurology Inpatient Servicea
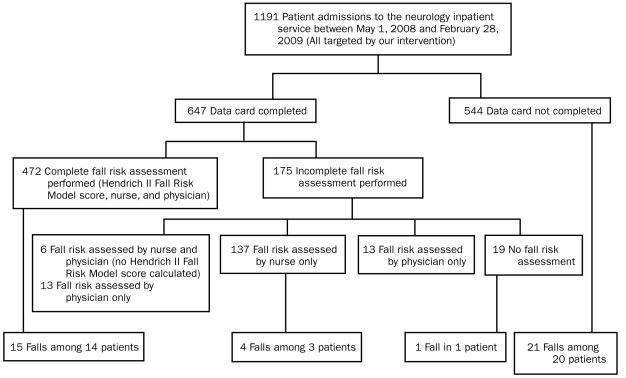
Data cards were collected from May 1, 2008, to February 28, 2009. During this period, there were 1191 admissions to the neurology inpatient service. Our aim was to collect a data card for every admission. However, because of logistic barriers (eg, delays in restocking the supply of blank cards, cards not being completed within the first 24 hours after admission), cards were completed for 647 admissions (54.3%; Figure).
FIGURE.
Study profile.
Of the 647 admissions for which a data card was available, a nurse fall risk assessment was performed in 615 (95.1%), a Hendrich II Fall Risk Model score was calculated in 607 (93.8%), and a physician fall risk assessment was performed in 491 (75.9%). A complete fall risk assessment (Hendrich II Fall Risk Model score, nurse and physician assessments) was performed in 472 (72.9%). The median Hendrich II Fall Risk Model score of this group was 5 (range, 0-15; interquartile range, 2-8), with 261 (55.3%) having a score of 5 or more. Nurses identified more patients as at risk for falls (312/472; 66.1%) than a Hendrich II Fall Risk Model score of 5 or more would have alone (261/472; 55.3%; P=.001). Physicians identified a higher proportion of patients as at risk for falls (332/472; 70.3%) than did nurses (312/472; 66.1%), but this difference was not significant (P=.16).
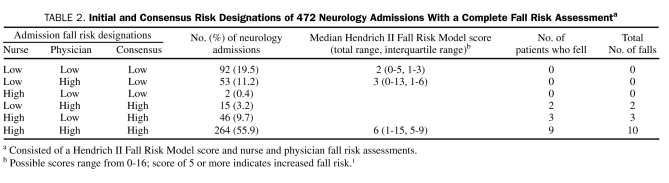
Nurse, physician, and consensus risk designations for the 472 admissions with a complete fall risk assessment are shown in Table 2. Initial nurse and physician fall risk assessments were both low-risk in 92 (19.5%), were both at-risk in 264 (55.9%), and differed in 116 (24.6%). When discrepancies occurred, the physician usually changed his or her initial fall risk assessment to match that of the nurse (99/116; 85.3%). After consensus was reached, 325 patients (68.9%) were considered at risk for falls. Of these, 46 (14.2%) were originally identified as at risk by only the nurse, 15 (4.6%) by only the physician, and 264 (81.2%) by both the nurse and the physician. The number of additional patients ultimately identified as at risk for falls because of the addition of a physician fall risk assessment was not statistically significant (325/472 vs 310/472; P=.30).
TABLE 2.
Initial and Consensus Risk Designations of 472 Neurology Admissions With a complete Fall Risk Assessmenta
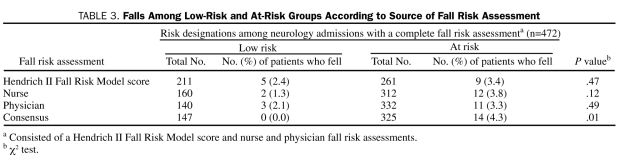
Of the 472 admissions with a complete fall risk assessment, 14 patients experienced a total of 15 falls: 13 patients fell once, and 1 patient fell twice during a single admission. The median Hendrich II Fall Risk Model score among these patients was 6 (range, 2-10; interquartile range, 4-9), and all had been identified as at risk for falls by the nurse, physician, or both (Table 2). The occurrence of falls according to Hendrich II Fall Risk Model score, nurse, physician, and consensus fall risk designations is shown in Table 3. The proportion of patients who fell was not significantly different in low-risk vs at-risk groups according to any individual assessment. However, when the consensus risk designation was used, the proportion of patients who fell was significantly higher in the at-risk group (P=.01).
TABLE 3.
Falls Among Low-Risk and At-Risk Groups According to Source of Fall Risk Assessment
Falls among the 175 neurology patients with an incomplete fall risk assessment at admission and the 544 for whom a data card was not completed are shown in the Figure. There was no significant difference in the number of patients who fell between those who did (18/647 [2.8%]) and those who did not (20/544 [3.7%]) have a completed data card (P=.41).
DISCUSSION
This controlled pre-post quality improvement study shows that including physicians as a standard part of the process of fall risk assessment at admission is feasible and is associated with a durable reduction in the rate of falls in our inpatient neurology unit. The rates of falls on 6 other medical units showed no significant change during the same preimplementation and postimplementation time frames, suggesting that the reduced rate of falls on the neurology unit was not simply due to increased institutional awareness of fall risk and prevention. The feasibility of our process was established despite the heterogeneous nature of resident physicians rotating on our services; this was likely due to use of a standard electronic admission order tool to trigger the physician assessment process.
Most patients who fell during the postimplementation time frame had been identified as at risk for falls at admission. This supports previous studies that showed the predictive value of fall risk assessment processes.14 Furthermore, significantly more patients fell in the at-risk group compared with those in the low-risk group when the consensus risk designation was used, but not when the Hendrich II Fall Risk Model score, nurse, or physician risk designations were used alone. This provides evidence for the value of multidisciplinary fall risk assessment.
The observed reduction in the rate of falls could be due to a number of factors. First, physician history taking and physical examination may identify fall risk factors that are not readily apparent on a nursing assessment. However, addition of a physician fall risk assessment did not significantly increase the number of patients identified as at risk, and few falls occurred in patients identified as at risk for falls only by a physician. Second, physicians may identify fall risk factors that are not included in the Hendrich II Fall Risk Model score. For example, a history of falls has been identified as a significant fall risk factor supported by Level A evidence,8 but it is not included in the Hendrich II Fall Risk Model score. Third, the presence of a physician fall risk assessment may serve as a “safety net” in the event that a nursing fall risk assessment is not performed or as a prompt that reminds nurses to complete their fall risk assessment. Fourth, asking physicians to consider fall risk at admission may alter their subsequent medical decision making and prescribing patterns in ways that reduce fall risk. This was not specifically measured in our study but is worthy of further investigation. Finally, adding a physician fall risk assessment might heighten the overall awareness of fall risk and prevention among the entire health care team, although this effect would be difficult to measure.
Our study has a number of limitations. First, it is possible that the reduced rate of falls was not due to our intervention but instead reflected a change in compliance with the event reporting process. However, other event types that are routinely tracked on the neurology inpatient unit did not decrease during the same time interval, making this unlikely. Likewise, no changes were made to the fall prevention measures used for patients at risk. Second, the administrative data used to determine rates of falls do not include demographic or other clinical information. Thus, we cannot exclude the possibility that clinical differences between patients admitted before and after our intervention could have influenced rates of falls. However, the clear temporal relationship between the introduction of our intervention and the downward trend in patient falls argues against this, and no changes have been made in the neurology admission processes that would favor admission of patients with lower fall risk. Likewise, although we specifically chose those medical services that were most similar to our neurology service as our control group, it is possible that clinical differences between neurology and other medical inpatients could have also influenced rates of falls. Finally, it is possible that the process of completing data collection cards affected the postintervention rate of falls. However, we think this is unlikely because the reduced rate of falls persisted after discontinuation of data card collection. Furthermore, our intervention targeted all patients on the neurology unit, and there was no significant difference in the number of patients who fell between those who did and those who did not have a completed data card.
Physician participation in the fall risk assessment process at admission was lower than expected, given placement of a required order on the neurology electronic order set. On further investigation, we determined that this likely resulted from the lack of a force-functioning feature in the electronic ordering system to prevent the use of nonneurology admission order sets for neurology inpatients. Some resident physicians rotating on the neurology service were from nonneurology training programs and were accustomed to using other institutional general admission order sets. This could be addressed in the future by electronically enforcing the use of department-specific order sets or by making the physician fall risk assessment order a standard part of all electronic admission order sets.
CONCLUSION
The results of this study indicate that a multidisciplinary approach to fall risk assessment can lead to a reduction in inpatient falls. Advantages of this approach include its simplicity, low cost, and easy applicability to other inpatient settings. However, to be successful, any assessment of fall risk must be combined with effective fall prevention measures. Although among the most commonly used, interventions such as fall risk identification bracelets,18 lowered beds,19 bed alarm systems,20 bed rails and restraints (or their removal),21 and medication reviews22 do not prove effective when studied in isolation. Rather, existing evidence suggests that multifaceted (eg, using a variety of fall prevention measures in combination)23 and multidisciplinary24 interventions that specifically target individual fall risk factors25,26 are required to reduce inpatient falls. Direct supervision27 and making nursing rounds hourly or every 2 hours28 also show promise as effective fall prevention strategies.
Given the high percentage of neurologic inpatients identified as at risk for falls by all our screening methods, an argument could be made for the use of universal fall precautions on neurology inpatient units. Consideration could also be given to using an “opt-out” approach that assumes neurology inpatients are at risk for falls and uses screening tools to instead identify those not at risk. Nevertheless, it would remain important to identify patients at highest risk so the time and resources required for more intensive fall prevention measures could be optimally allocated.
Acknowledgments
We acknowledge Loreene K. Caswell, RN, Connie L. Krueger, RN, Tammy R. Mathias, RN, Terri L. McKenzie, RN, Denise A. Pyfferoen, RN, and Kathleen M. Spoo, RN, for completing data collection cards; Mark S. Fratzke, RN, for help in project conceptualization; Anna M. Halvorson, RN, for compiling falls data; and Julie M. Yost for adding the physician fall risk assessment order to the neurology electronic admission order set.
REFERENCES
- 1. Hendrich AL, Bender PS, Nyhuis A. Validation of the Hendrich II fall risk model: a large concurrent case/control study of hospitalized patients. Appl Nurs Res. 2003;16(1):9-21 [DOI] [PubMed] [Google Scholar]
- 2. Gaebler S. Predicting which patient will fall again… and again. J Adv Nurs. 1993;18(12):1895-1902 [DOI] [PubMed] [Google Scholar]
- 3. Bates DW, Pruess K, Souney P, Platt R. Serious falls in hospitalized patients: correlates and resource utilization. Am J Med. 1995;99(2):137-143 [DOI] [PubMed] [Google Scholar]
- 4. Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18(2):141-158 [DOI] [PubMed] [Google Scholar]
- 5. Oliver D, Britton M, Seed P, Martin FC, Hopper AH. Development and evaluation of evidence based risk assessment tool (STRATIFY) to predict which elderly inpatients will fall: case-control and cohort studies. BMJ. 1997;315(7115):1049-1053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Leipzig RM, Cumming RG, Tinetti ME. Drugs and falls in older people: a systematic review and meta-analysis: I. Psychotropic drugs. J Am Geriatr Soc. 1999;47(1):30-39 [DOI] [PubMed] [Google Scholar]
- 7. Tinetti ME, Kumar C. The patient who falls: “it's always a trade-off”. JAMA. 2010;303(3):258-266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Thurman DJ, Stevens JA, Rao JK. Practice parameter: assessing patients in a neurology practice for risk of falls (an evidence-based review): report of the quality standards subcommittee of the American Academy of Neurology. Neurology. 2008;70(6):473-479 [DOI] [PubMed] [Google Scholar]
- 9. Hitcho EB, Krauss MJ, Birge S, et al. Characteristics and circumstances of falls in a hospital setting: a prospective analysis. J Gen Intern Med. 2004;19(7):732-739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Halfon P, Eggli Y, Van Melle G, Vagnair A. Risk of falls for hospitalized patients: a predictive model based on routinely available data. J Clin Epidemiol. 2001;54(12):1258-1266 [DOI] [PubMed] [Google Scholar]
- 11. Healey F, Scobie S, Oliver D, Pryce A, Thomson R, Glampson B. Falls in English and Welsh hospitals: a national observational study based on retrospective analysis of 12 months of patient safety incident reports. Qual Saf Health Care. 2008;17(6):424-430 [DOI] [PubMed] [Google Scholar]
- 12. Shorr RI, Mion LC, Rosenblatt LC, Lynch D, Kessler LA. Improving the capture of fall events in hospitals: combining a service for evaluating inpatient falls with an incident report system. J Am Geriatr Soc. 2008;56(4):701-704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Bradley SM, Karani R, McGinn T, Wisnivesky J. Predictors of serious injury among hospitalized patients evaluated for falls. J Hosp Med. 2010;5(2):63-68 [DOI] [PubMed] [Google Scholar]
- 14. Perell KL, Nelson A, Goldman RL, Luther SL, Prieto-Lewis N, Rubenstein LZ. Fall risk assessment measures: an analytic review. J Gerontol A Biol Sci Med Sci. 2001;56(12):M761-M766 [DOI] [PubMed] [Google Scholar]
- 15. Scott V, Votova K, Scanlan A, Close J. Multifactorial and functional mobility assessment tools for fall risk among older adults in community, home-support, long-term, and acute care settings. Age Ageing. 2007;36(2):130-139 [DOI] [PubMed] [Google Scholar]
- 16. Vassallo M, Vignaraja R, Sharma JC, Briggs R, Allen SC. Predictors for falls among hospital inpatients with impaired mobility. J R Soc Med. 2004;97(6):266-269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lehmann EL, Romano JP. Testing Statistical Hypotheses. 3rd ed. New York, NY: Springer; 2005:125 [Google Scholar]
- 18. Mayo NE, Gloutney L, Levy AR. A randomized trial of identification bracelets to prevent falls among patients in a rehabilitation hospital. Arch Phys Med Rehabil. 1994;75(12):1302-1308 [PubMed] [Google Scholar]
- 19. Haines TP, Bell RA, Varghese PN. Pragmatic, cluster randomized trial of a policy to introduce low-low beds to hospital wards for the prevention of falls and fall injuries. J Am Geriatr Soc. 2010;58(3):435-441 [DOI] [PubMed] [Google Scholar]
- 20. Tideiksaar R, Feiner CF, Maby J. Falls prevention: the efficacy of a bed alarm system in an acute-care setting. Mt Sinai J Med. 1993;60(6):522-527 [PubMed] [Google Scholar]
- 21. Hanger HC, Ball MC, Wood LA. An analysis of falls in hospital: can we do without bedrails? J Am Geriatr Soc. 1999;47(5):529-531 [DOI] [PubMed] [Google Scholar]
- 22. Haumschild MJ, Karfonta TL, Haumschild MS, Phillips SE. Clinical and economic outcomes of a fall-focused pharmaceutical intervention program. Am J Health Syst Pharm. 2003;60(10):1029-1032 [DOI] [PubMed] [Google Scholar]
- 23. Oliver D, Connelly JB, Victor CR, et al. Strategies to prevent falls and fractures in hospitals and care homes and effect of cognitive impairment: systematic review and meta-analyses. BMJ. 2006;334(82):1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Haines TP, Bennell KL, Osborne RH, Hill KD. Effectiveness of targeted falls prevention programme in subacute hospital setting: randomised controlled trial. BMJ. 2004;328(7441):676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Coussement J, De Paepe L, Schwendimann R, Denhaerynck K, Dejaeger E, Milisen K. Interventions for preventing falls in acute- and chronic-care hospitals: a systematic review and meta-analysis. J Am Geriatr Soc. 2008;56(1):29-36 [DOI] [PubMed] [Google Scholar]
- 26. Dykes PC, Carroll DL, Hurley A, et al. Fall prevention in acute care hospitals: a randomized trial. JAMA, 2010;304(17):1912-1918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Giles LC, Bolch D, Rouvray R, et al. Can volunteer companions prevent falls among inpatients? A feasibility study using a pre-post comparative design. BMC Geriatr. 2006;6:11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Meade CM, Bursell AL, Ketelson L. Effects of nursing rounds: on patients' call light use, satisfaction, and safety. Am J Nurs. 2006;106(9):58-70 [DOI] [PubMed] [Google Scholar]