Abstract
OBJECTIVE: To determine whether interdisciplinary simulation team training can positively affect registered nurse and/or physician perceptions of collaboration in clinical decision making.
PARTICIPANTS AND METHODS: Between March 1 and April 21, 2009, a convenience sample of volunteer nurses and physicians was recruited to undergo simulation training consisting of a team response to 3 clinical scenarios. Participants completed the Collaboration and Satisfaction About Care Decisions (CSACD) survey before training and at 2 weeks and 2 months after training. Differences in CSACD summary scores between the time points were assessed with paired t tests.
RESULTS: Twenty-eight health care professionals (19 nurses, 9 physicians) underwent simulation training. Nurses were of similar age to physicians (27.3 vs 34.5 years; p=.82), were more likely to be women (95.0% vs 12.5%; p<.001), and were less likely to have undergone prior simulation training (0% vs 37.5%; p=.02). The pretest showed that physicians were more likely to perceive that open communication exists between nurses and physicians (p=.04) and that both medical and nursing concerns influence the decision-making process (p=.02). Pretest CSACD analysis revealed that most participants were dissatisfied with the decision-making process. The CSACD summary score showed significant improvement from baseline to 2 weeks (4.2 to 5.1; p<.002), a trend that persisted at 2 months (p<.002).
CONCLUSION: Team training using high-fidelity simulation scenarios promoted collaboration between nurses and physicians and enhanced the patient care decision-making process.
Team training using high-fidelity simulation scenarios promoted collaboration between nurses and physicians and thus enhanced the patient care decision-making process.
AHRQ = Agency for Healthcare Research and Quality; CSACD = Collaboration and Satisfaction About Care Decisions
Nearly a decade has passed since the Institute of Medicine released its seminal report To Err is Human: Building a Safer Health System.1 The report described the US health care system as a decade or more behind other high-risk industries in its attention to ensuring basic safety. One recommendation was that Congress should create a center for patient safety within the Agency for Healthcare Research and Quality (AHRQ). The AHRQ was asked to set standards, communicate with members about safety, and develop training programs that create a culture of safety across disciplines.1 The AHRQ supports simulation research through its patient safety program, recognizing that “simulation in health care creates a safe learning environment that allows researchers and practitioners to test new clinical processes and to enhance individual and team skills before encountering patients.”2
Effective collaboration between registered nurses and physicians has been shown to reduce morbidity and mortality rates, cost of care, and medical errors and to improve job satisfaction and retention of nursing staff.3-6 The nursing workforce is expected to decrease by 20% by 2020, putting the profession in a critical shortage.7 Collaboration between nurses and physicians improves professional job satisfaction and is considered a high priority for retention purposes. The literature has outlined the importance of nurse-physician collaboration but is lacking in strategies that enhance it. The team approach to health care requires that these different professions communicate and collaborate effectively in a rapidly changing and complex environment. Patients are at risk of adverse effects when exchanged information is misunderstood or misinterpreted.
The need for improvement in the ability of nurses and physicians to exchange information is well known. Team-training exercises for health care professionals are considered to be a highly effective tool to improve communication and team performance, particularly in crisis situations.8-10 TeamSTEPPS, developed by the Department of Defense and the AHRQ, is an evidence-based framework to optimize team performance across the health care delivery system.11,12 The framework comprises 4 teaching and learning skills: (1) leadership, (2) situation monitoring, (3) mutual support, and (4) communication. We have designed a team-training course that incorporates key concepts and principles from TeamSTEPPS and crisis resource management.11,12
High-fidelity simulation training, in a dedicated simulation center, offers a realistic and experiential environment in which learners practice response to clinical scenarios, debrief, and evaluate team performance in the absence of patient risk. Simulation exercises offer a venue for dialogue on and active listening to one another's perspectives, thoughts, and practices and may be beneficial in general medical-surgical settings as a vehicle to enhance nurse-physician collaboration. Therefore, our aim was to determine if interdisciplinary simulation team training can positively affect perceptions of nurses and/or physicians about collaboration in clinical decision making.
PARTICIPANTS AND METHODS
After approval by the Mayo Clinic Institutional Review Board, registered nurses and surgical faculty and surgical residents working together in a dedicated inpatient surgical ward at Mayo Clinic in Rochester, MN, were identified as potential participants. Volunteers were recruited between March 1 and April 21, 2009. Simulation training was conducted at the Mayo Clinic Multidisciplinary Simulation Center in Rochester, MN. The center provides classrooms for prebriefing and debriefing sessions and realistic mock-up examination rooms, ward units, and operating rooms, as well as high-fidelity interactive mannequins, 2-way mirrors, and audiovisual recording capability for review of key segments during debriefing. The Mayo Clinic Multidisciplinary Simulation Center has been accredited by the American College of Surgeons.13
Evaluation Tool, Clinical Scenarios, and Debriefing
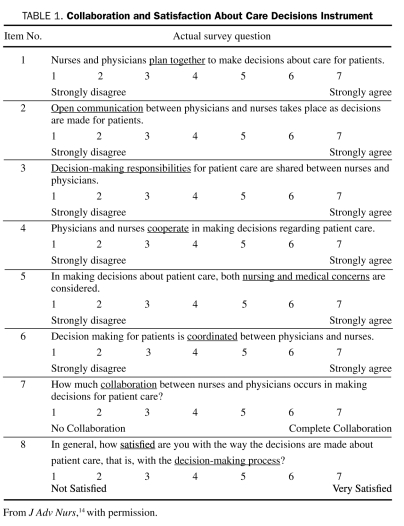
Study participants were given the Collaboration and Satisfaction About Care Decisions (CSACD)14 questionnaire at 3 time points: immediately before simulation training, 2 weeks after training, and 2 months after training.15 The CSACD is a validated Likert-scaled questionnaire that was designed to determine how well nurse-physician teams work together (Table 1). It is composed of 8 items and has an α reliability of 0.90, indicating that it is a highly reliable instrument. Six of the items have 7 response options ranging from “strongly disagree” to “strongly agree.” One of the items has 7 response options ranging from “no collaboration” to “complete collaboration,” and one of the items has 7 response options ranging from “not satisfied” to “very satisfied.” Additionally, demographic information was collected, including years of experience, sex, age, educational level, resident or faculty status, and previous interdisciplinary simulation training.
TABLE 1.
Collaboration and Satisfaction About Care Decisions Instrument
The team-training course used 3 clinical scenarios that would provide adequate opportunity for collaborative interaction between nurses and physicians. The clinical scenarios were developed in collaboration by content and simulation training experts and reflected potential postoperative complications in colon and rectal surgical patients. A prebriefing session before the first scenario described the overall process and role expectations. The first scenario involved a patient who showed clinical signs of sepsis after developing an anastomotic leak, the second scenario involved a patient experiencing postoperative bleeding, and the third involved a postoperative patient who developed respiratory distress and mental status changes. High-fidelity mannequins with simulated breath sounds, pulses, and the ability to respond verbally to questions from health care professionals were used. They were controlled through a 2-way mirror and placed in a realistic-appearing hospital room. Scenarios played out according to script design, with participants unaware of the patient's ultimate diagnosis. Scenarios lasted about 20 minutes, involved all team members (nurses and physicians), and were videotaped for debriefing recall purposes. After the first scenario, team principles were introduced in the debriefing session. After each scenario, a trained facilitator debriefed the participants and showed them instant replays of key interactions. The facilitator engaged the participants in dialogue around teamwork in the scenarios and actual practice setting to promote in-depth discussions regarding communication among team members.
Statistical Analyses
Differences in characteristics between nurses and physicians were assessed with nonparametric univariate analysis (Wilcoxon rank sum test for continuous data and Fisher exact test for categorical data). Responses to the CSACD survey items at the 3 time points were then collated, and a summary score was calculated for each time point; these summary scores represented our primary end point. In order to assess differences in the CSACD summary scores and responses to individual items between the time points, CSACD analysis was then performed using paired t tests.
The primary analysis was the CSACD posttest 1 summary score compared with the pretest summary score to determine if simulation training was associated with a change in perception. The secondary analysis was the CSACD posttest 2 summary score compared with the post-test 1 summary score to assess if any change in perception was sustained over time. In addition, univariate individual item analysis for both the primary and secondary analyses was performed. Finally, a univariate analysis of potential differences in perception between nurses and physicians was performed. The Bonferroni correction for multiple comparisons was applied to all p values. For all statistical comparisons, p<.05 was considered significant. All analyses were performed using JMP, version 8.0 for Mac (SAS Institute, Cary, NC).
RESULTS
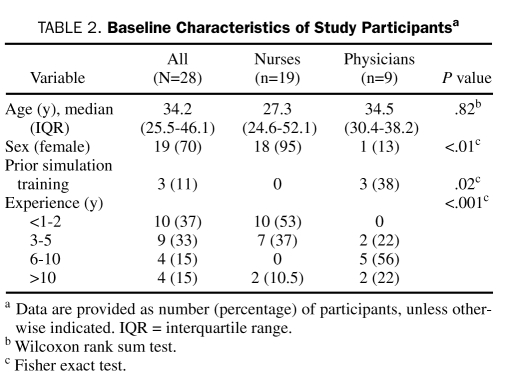
Twenty-eight health care professionals, including 19 RNs and 9 physicians (2 surgical faculty, 7 surgical residents), completed the pretest survey and underwent simulation training. Characteristics of participants are summarized in Table 2. Nurses were of similar age to physicians (27.3 vs 34.5 years; p=.82), were more likely to be women (95.0% vs 12.5%; p<.001), and were less likely to have undergone prior simulation training (0% vs 37.5%; p=.02).
TABLE 2.
Baseline Characteristics of Study Participantsa
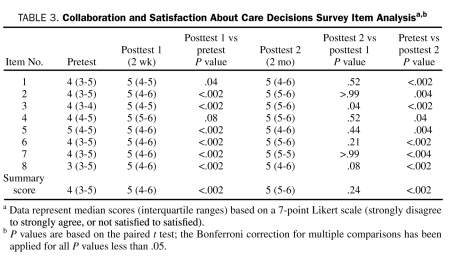
Responses to the CSACD surveys at all 3 time points are summarized in Table 3. Pretest CSACD item analysis revealed that up to 50% of respondents were dissatisfied with the current decision-making process (median score, 3). Two weeks after intervention, the CSACD median scores for each item improved significantly, as did the overall summary score (pretest vs posttest 1, 4.2 vs 5.1 points; p<.002). Improvement was sustained at 2 months (pretest vs posttest 2, p<.002) and also was evidenced by no statistical difference between the 2-week and 2-month scores (p=.24).
TABLE 3.
Collaboration and Satisfaction About Care Decisions Survey Item Analysisa,b
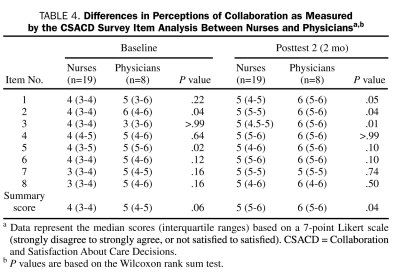
Differences in perceptions between nurses and physicians at baseline and at 2 months are outlined in Table 4. Pretest data showed that physicians were more likely to perceive that open communication exists between nurses and physicians (p=.04) and that both medical and nursing concerns influence the decision-making process (p=.02). The overall summary pretest score trended toward significance (p=.06); this difference in perceptions was statistically significant at 2 months (p=.04).
TABLE 4.
Differences in Perceptions of Collaboration as Measured by the CSACD Survey Item Analysis Between Nurses and Physiciansa,b
DISCUSSION
This study demonstrated that team training using high-fidelity simulation and debriefing for nurses and physicians promoted collaborative teamwork in a working environment in which dissatisfaction with the existing teamwork approach to patient care was high according to results from Professional Research Consultants (Omaha, NE) surveys and unit-based teamwork surveys. Moreover, after the training experience, participants perceived that significant improvements in the patient care decision-making process were sustained over time in the practice setting. A secondary effect of the team training was a better understanding by physicians of the challenges faced by nurses (and vice versa) and an overwhelming motivation to improve professional relationships through more effective communication in the future.
One of the major concerns in our work unit was that patients might be at increased risk of adverse effects when exchanged information was misunderstood or misinterpreted (ie, miscommunicated). For good outcomes in health care, collaborative practice whereby nurses and physicians make a concerted effort to combine their unique professional skills and knowledge base is crucial.16 Collaboration between team members has been clearly shown to increase awareness of each other's type of knowledge and skill, leading to continued improvement in decision making.2 Effective nurse-physician collaboration has been shown to reduce morbidity and mortality rates, cost of care, and errors and to improve job satisfaction and retention of nursing staff.3-6 According to McConaughey17 and Marshall and Manus,18 the Joint Commission identified communication problems as the root cause of 65% of sentinel events, with 74% resulting in death. Health care organizations can no longer ignore the role of failures in teamwork and communication if the goal is to create sustainable, safe environments.
Rarely do health care professionals train as teams, yet evidence shows that team training improves team performance and safety outcomes.19 Our study showed a statistically significant improvement in the perception by nurses and physicians of collaboration and decision making at 2 weeks after high-fidelity simulation team training. These improvements were sustained and continued to increase at 2 months, especially in the nursing staff. However, at 2 months, the physicians showed a slight decline in the areas of communication and cooperation. These results indicate that simulating or practicing team collaboration in this manner has the potential to improve patient care, but whether initial improvements can be sustained over longer periods of time is unknown.
Our study also demonstrated that nurses and physicians have significantly different perceptions of clinical decision making. These findings emphasize the importance of developing strategies to overcome these differences and optimize the nurse-physician relationship. In a multisite, evidence-based management practice initiative to identify structures that foster critical care nurse-physician relations, Schmalenberg et al5 described different levels of collaboration and stated that collaboration is best viewed as a relationship. According to their study, “The lowest level is characterized by the sequential reporting by each discipline without interaction or dialogue,” and was called multidisciplinary by interviewees. The highest level of collaboration, interdisciplinary, is described by “interaction and spirited dialogue” occurring between members of differing disciplines.5
Factors that enhance and impede the perceived level of interdisciplinary collaboration are examined by Fewster-Thuente and Velsor-Friedrich20 in the context of the King theory of goal attainment. Factors that impede collaborative relationships between those with differing professional roles are patriarchal relationships, time, lack of role clarification, sex, and culture. Time for interaction, a building block for trust, is an essential ingredient in collaborative relationships. Interventions that support these relationships include collaborative practice order sets and care plans. As a result of these interventions, health care professionals in differing roles converge on a common path to influence the best outcome for patients.
Interdisciplinary training has been shown to foster respect for the contributions of each discipline.21 Health care team members interact with each other in the clinical setting, but learning to problem-solve as a team in a collaborative manner can be done in a simulated environment. According to Rodehorst et al,22 simulation provides an alternative teaching strategy that allows individual team members to problem-solve and identify ways to work together given a particular clinical scenario.
Using simulation as a venue for interdisciplinary learning has been shown to enhance nurse-physician collaboration.19,23,24 Miller et al19 found that simulation training with pediatric residents and nurses during life-threatening scenarios enhanced relationships between the nurses and physicians. Similarly, Ker et al23 found that interdisciplinary learning between medical and nursing students allowed the students to recognize professional roles and contributions. The students came to understand the importance of collaboration and teamwork.
The current study has several limitations. Using only 1 specialty practice group from a single surgical nursing unit has inherent bias and does not address the ability of training to be widely applicable to other surgical nursing units. The residents who participated rotate to different units every 6 weeks, so some of the resident participants had rotated to different surgical services by the time the last survey was administered. Moreover, the length of resident experience was limited to 1 to 3 years, whereas the years of nursing experience ranged from less than 1 year to more than 10 years. Finally, our study may have been underpowered to detect differences in the secondary analysis or differences between nurses and physicians. Another limitation was that the study design did not include a control group. Without a control group, the findings may be attributed to learning or testing effects (participants do better on follow-up tests because they learned from the baseline test).25 The outcome could also have been affected by the Hawthorne effect (participants modify their behavior in response to being studied)26 and the Pygmalion effect (people perform better because of expectations placed on them).27 Nevertheless, the desired effect was achieved. Because our study used a convenience sample, the participants may not have represented all personality types. The study results are preliminary, and further research using a stronger design is needed to clarify if the positive results are reproducible.
Does one need to use a simulation center to achieve these results, or would the same results have occurred by another intervention? The simulation center offers staff the opportunity to perform patient care activities in a non-threatening environment. Future research should include randomizing staff for simulation team training or another type of problem-based learning.
As the complexity of patient care increases and more standardization of postoperative pathways occurs, good communication and collaboration between multidisciplinary teams of caregivers will be essential. Without a highly collaborative approach, outcomes cannot be optimized and our patients will be at increased risk of postoperative complications.
CONCLUSION
High-fidelity simulation team training can be an effective method to increase awareness of the barriers to good communication among caregivers and improve collaboration in patient care decision-making processes.
REFERENCES
- 1. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Building A Safer Health System. Washington, DC: National Academy Press; 2000:1–67 [PubMed] [Google Scholar]
- 2. AHRQ Agency for Healthcare Research and Quality Improving Patient Safety Through Simulation Research. Rockville, MD: US Department of Health and Human Services; 2008. http://www.ahrq.gov/qual/simulproj.htm Accessed October 13, 2010 [Google Scholar]
- 3. Kramer M, Schmalenberg C. Securing “good” nurse/physician relationships. Nurs Manage. 2003;34(7):34-38 [DOI] [PubMed] [Google Scholar]
- 4. Manojlovich M. Linking the practice environment to nurses' job satisfaction through nurse-physician communication. J Nurs Scholarsh. 2005;37(4):367-373 [DOI] [PubMed] [Google Scholar]
- 5. Schmalenberg C, Kramer M, King CR, et al. Excellence through evidence: securing collegial/collaborative nurse-physician relationships, part 1. J Nurs Adm. 2005;35(10):450-458 [DOI] [PubMed] [Google Scholar]
- 6. Thomas EJ, Sexton JB, Helmreich RL. Discrepant attitudes about teamwork among critical care nurses and physicians. Crit Care Med. 2003;31(3):956-959 [DOI] [PubMed] [Google Scholar]
- 7. Buerhaus PI, Donelan K, Ulrich BT, Norman L, Williams M, Dittus R. Hospital RNs' and CNOs' perceptions of the impact of the nursing shortage on the quality of care. Nurs Econ. 2005;23(5):214-221 [PubMed] [Google Scholar]
- 8. Rall M, Manser T, Guggenberger H, Gaba DM, Unertl K. Patient safety and errors in medicine: development, prevention and analyses of incidents [in German]. Anasthesiol Intensivmed Notfallmed Schmerzther. 2001;36(6):321-330 [DOI] [PubMed] [Google Scholar]
- 9. Subash F, Dunn F, McNicholl B, Marlow J. Team triage improves emergency department efficiency. Emerg Med J. 2004;21(5):542-544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wiener EL, Kanki BG, Helmreich RL, eds. Cockpit Resource Management. Oxford, UK: Elsevier; 1993. [Google Scholar]
- 11. King HB, Battles J, Baker DP, et al. TeamSTEPPS™: Team Strategies and Tools to Enhance Performance and Patient Safety. Rockville, MD: Agency for Healthcare Research and Quality; 2006. [PubMed] [Google Scholar]
- 12. Clancy CM, Tornberg DN. TeamSTEPPS: assuring optimal teamwork in clinical settings. Am J Med Qual. 2007;22(3):214-217 [DOI] [PubMed] [Google Scholar]
- 13. Mayo Clinic multidisciplinary simulation center receives distinction as an ACS-accredited education institute. Mayo Clinic News. Published September 13, 2007. http://www.mayoclinic.org/news2007-rst/4245.html Accessed October 13. 2010
- 14. Baggs JG. Development of an instrument to measure collaboration and satisfaction about care decisions. J Adv Nurs. 1994;20(1):176-182 [DOI] [PubMed] [Google Scholar]
- 15. Bratt MM, Broome M, Kelber S, Lostocco L. Influence of stress and nursing leadership on job satisfaction of pediatric intensive care unit nurses. Am J Crit Care. 2000;9(5):307-317 [PubMed] [Google Scholar]
- 16. Weiss SJ, Davis HP. Validity and reliability of the Collaborative Practice Scales. Nurs Res. 1985;34(5):299-305 [PubMed] [Google Scholar]
- 17. McConaughey E. Crew resource management in healthcare: the evolution of teamwork training and MedTeams. J Perinat Neonatal Nurs. 2008;22(2):96-104 [DOI] [PubMed] [Google Scholar]
- 18. Marshall DA, Manus DA. A team training program using human factors to enhance patient safety. AORN J. 2007;86(6):994-1011 [DOI] [PubMed] [Google Scholar]
- 19. Miller KK, Riley W, Davis S, Hansen HE. In situ simulation: a method of experiential learning to promote safety and team behavior. J Perinat Neonatal Nurs. 2008;22(2):105-113 [DOI] [PubMed] [Google Scholar]
- 20. Fewster-Thuente L, Velsor-Friedrich B. Interdisciplinary collaboration for healthcare professionals. Nurs Adm Q. 2008;32(1):40-48 [DOI] [PubMed] [Google Scholar]
- 21. Lowry LW, Burns CM, Smith AA, Jacobson H. Compete or complement? An interdisciplinary approach to training health professionals. Nurs Health Care Perspect. 2000;21(2):76-80 [PubMed] [Google Scholar]
- 22. Rodehorst TK, Wilhelm SL, Jensen L. Use of interdisciplinary simulation to understand perceptions of team members' roles. J Prof Nurs. 2005;21(3):159-166 [DOI] [PubMed] [Google Scholar]
- 23. Ker J, Mole L, Bradley P. Early introduction to interprofessional learning: a simulated ward environment. Med Educ. 2003;37(3):248-255 [DOI] [PubMed] [Google Scholar]
- 24. Messmer PR. Enhancing nurse-physician collaboration using pediatric simulation. J Contin Educ Nurs. 2008;39(7):319-327 [DOI] [PubMed] [Google Scholar]
- 25. Burns N, Grove SK. The Practice of Nursing Research: Conduct, Critique, & Utilization. 4th ed. Philadelphia, PA: WB Saunders Co; 2001:41 [Google Scholar]
- 26. Hulley SB, Cummings SR, Browner WS, Grady D, Hearst N, Newman TB. Designing Clinical Research: An Epidemiologic Approach. 2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:168-169 [Google Scholar]
- 27. Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton Mifflin Co; 2002:78-79 [Google Scholar]