Abstract
Background
While in adults with sickle cell disease an elevation of tricuspid regurgitation velocity is associated with increased mortality, the importance of this finding in children has not been established. The role of intravascular hemolysis in the development of this complication is controversial.
Design and Methods
We conducted a prospective, longitudinal, multi-center study of 160 individuals aged 3–20 years with hemoglobin SS, performing baseline and follow-up determinations of clinical markers, six-minute walk distance less than tricuspid regurgitation velocity and E/Etdi ratio by echocardiography.
Results
At baseline, 14.1% had tricuspid regurgitation velocity of 2.60 m/sec or over, which suggests elevated systolic pulmonary artery pressure, and 7.7% had increased E/Etdi, which suggests elevated left ventricular filling pressure. Over a median of 22 months, baseline elevation in tricuspid regurgitation velocity was associated with an estimated 4.4-fold increase in the odds of a 10% or more decline in age-standardized six-minute-walk distance (P=0.015). During this interval, baseline values above the median for a hemolytic component derived from four markers of hemolysis were associated with a 9.0-fold increase in the odds of the new onset of elevated tricuspid regurgitation velocity (P=0.008) and baseline E/Etdi elevation was associated with an estimated 6.1-fold increase in the odds (P=0.039). In pathway analysis, higher baseline hemolytic component and E/Etdi predicted elevated tricuspid regurgitation velocity at both baseline and follow up, and these elevations in turn predicted decline in six-minute-walk distance.
Conclusions
Further studies should define the long-term risks of elevated tricuspid regurgitation velocity in childhood and identify potential interventions to prevent increased pulmonary artery pressure and preserve function.
Keywords: sickle cell anemia, tricuspid regurgitation velocity, E/Etdi, hemolysis, six minute walk
Introduction
The autosomal recessive substitution of valine for glutamic acid at position six of the β-globin chain of hemoglobin in sickle cell anemia results in mutant hemoglobin S that polymerizes upon deoxygenation. This is the central event that leads to hemolysis, vaso-occlusive episodes and numerous acute and chronic complications. Pulmonary hypertension may develop in most forms of hereditary and chronic hemolytic anemia,1–4 suggesting that there is a clinical syndrome of hemolysis-associated pulmonary hypertension. During intravascular hemolysis, hemoglobin and arginase-1 are released into the plasma from erythrocytes. Plasma cell-free hemoglobin scavenges nitric oxide and arginase-1 depletes the plasma of arginine, the obligate substrate for nitric oxide synthase, and these processes may produce a hemolysis-linked state of decreased nitric oxide bioavailability and vascular dysfunction.5–7 Cross-sectional studies have found associations between the degree of hemolysis and markers of pulmonary artery pressure in individuals with sickle cell disease.8,9 Elevated tricuspid regurgitation velocity measured by echocardiography occurs in up to one-third of adults with sickle cell disease, correlates with elevated systolic pulmonary artery pressure and is associated with increased morbidity and mortality.8,10,11 However, whether high degrees of hemolysis lead to pulmonary vascular complications in sickle cell anemia is controversial.12 Left ventricular diastolic dysfunction is a frequent finding in sickle cell disease adults with right heart catheterization-documented pulmonary hypertension13 and is also an independent predictor of death.14
Elevated tricuspid regurgitation velocity9,15–21 and left ventricular diastolic dysfunction22 develop in children with sickle cell disease but the clinical importance is not clear.16,22,23 In particular, whether screening and intervention for these complications should begin in childhood is not known. In the few longitudinal studies of cardiopulmonary complications in children with sickle cell disease that have been reported,18,21,24 an association with mortality during the short duration of follow up has not been observed. The Pulmonary Hypertension and the Hypoxic Response in SCD (PUSH) study is a prospective, ongoing, multicenter screening and longitudinal investigation of children and adolescents with sickle cell disease. Here we describe the consequences of increased hemolytic rate, elevated tricuspid regurgitation velocity, and left ventricular dysfunction among 160 children with sickle cell anemia followed for a median of 22 months, the largest such prospective screening and follow-up cohort study reported to date.
Design and Methods
Study participants and study design
The institutional review boards of all participating institutions approved the study and written consent was obtained for all participants. Of 269 participants aged 3–20 years with sickle cell anemia (hemoglobin SS) who had clinical evaluation, echocardiography and six-minute walk test performed at steady-state as previously described,9 follow-up information was available for 166 participants at the time of this report, giving a follow-up success rate of 62%. The other 103 children did not have follow-up studies because of a recent hospitalization, failure to keep an appointment, failure to agree to follow up or inability to make contact to schedule the follow up. The children having follow up did not differ significantly from those not having follow up in terms of baseline tricuspid regurgitation velocity, E/Etdi, hemolytic markers, hemoglobin concentration or six-minute walk distance. In addition 6 children were excluded from the present report because their follow up occurred less than 12 months from recruitment. The participants had hemoglobin SS as confirmed by molecular genetic testing, hemoglobin electrophoresis or HPLC. Participants were recruited at four centers: Howard University and Children’s National Medical Center in Washington DC, the University of Michigan in Ann Arbor, Michigan and the Pulmonary and Vascular Medicine Branch of the NHLBI, Bethesda, MD. Repeat echocardiogram was performed in 152 participants and repeat six-minute walk test was performed in 132 participants. Blood collections, echocardiograms and six-minute walk tests were performed at least three weeks after a blood transfusion.
Echocardiography
Transthoracic echocardiography was performed and studies were interpreted centrally according to the guidelines of the American Society of Echocardiography.25 Systolic pulmonary artery pressure was estimated through measurement of the peak tricuspid regurgitation velocity.26,27 Left ventricular filling pressure was estimated by calculating the ratio of the mitral inflow E wave to the tissue Doppler E wave (E/Etdi).28,29 Based on the mean + 2 SDs in the controls of this study,9 peak tricuspid regurgitation velocity of 2.60 m/sec or higher and mitral valve E/Etdi ratio of 9.23 or higher were considered to be elevated.9
Six-minute walk
Non-encouraged six-minute walk testing was performed according to American Thoracic Society guidelines30 as previously described.9 The six-minute walk test is used in clinical practice and research to determine the level of functional exercise capacity31–33 and is an accepted method for evaluating response to pulmonary vasodilators for pulmonary artery hypertension.34
Molecular genetic testing
Hemoglobin S genotyping was conducted at ARUP Laboratories (Salt Lake City, UT, USA) using loci-spanning probe PCR as described.35
Follow-up information
Follow-up information included laboratory measurements, tricuspid regurgitation velocity, mitral valve E/Etdi ratio, left ventricular internal diastolic dimension (LVIDD) z-score, and six-minute walk distance at the time of follow up, as well as clinical events such as death, stroke, acute chest syndrome, and blood transfusions in the time interval since the baseline observations. We analyzed evolution of six-minute walk distance and of echocardiographically-determined tricuspid regurgitation velocity between the initial study and the follow-up evaluation.
Statistical analysis
Principal component analysis was used to derive a hemolytic component from absolute reticulocyte count and from age-adjusted values for lactate dehydrogenase, aspartate aminotransferase and bilirubin that was adjusted for site of enrollment. This component represents a normalized standard distribution with a mean value of 0 and reflects the maximal shared variance among the variables from which it is derived. Principal component analysis is useful for studying underlying mechanisms reflected in individual biological measurements.36,37 In the present study, additional advantage to the principle component was that it accounted for age-related changes in markers such as lactate dehydrogenase and for different reference ranges among the participating institutions.
For continuous variables that did not follow a normal distribution, the best transformation to a normal distribution was made for statistical analyses. Continuous variables were compared between screening and follow up with the paired t-test. Logistic regression or analysis of variance models as appropriate were used to assess baseline predictors of follow-up six-minute walk distance and tricuspid regurgitation velocity. As prospectively planned, the influence of hemolytic markers on these outcome variables was assessed in these models. For the analysis of decline in six-minute walk distance during follow up, the observed distances were age-standardized by regression.
Pathway analysis38 was also performed for exploring the predictors of high tricuspid regurgitation velocity and decline in six-minute walk distance during follow up. Pathway analysis is a multivariate statistical technique used to examine relationships among two or more variables. In this analysis, a hypothetical pathway from exogenous variables (predictors) to endogenous variables (responses) is tested against observed data. A standardized regression weight is computed for each relationship as adjusted for the other relationships. If the data supports the model, the overall P value is not significant. The fitness of final model to the observed data can be measured by several indicators, including the root mean square error of approximation (RMSEA), which measures the discrepancy function obtained by fitting the model to the population values. A RMSEA of about 0.05 or less indicates a close fit of the model.
Analyses were performed with STATA 10.1 (StataCorp, College Station, TX, USA) or AMOS 18.0 (SPSS Inc., Chicago, IL, USA).
Results
Baseline characteristics of the study cohort (Table 1)
Table 1.
Baseline characteristic of participants. Results are median (interquartile range) unless otherwise indicated.
At baseline, the median age of the 160 participants was 13 years and 51% of the participants were females. Forty-nine percent were receiving hydroxyurea therapy and 18% were on a chronic transfusion program, usually for elevated transcranial Doppler velocity values or history of stroke. Baseline tricuspid regurgitation velocity was not measurable in 11 participants and was 2.60 m/sec or higher in 21 (14.1%) of 149 participants. Baseline mitral valve E/Etdi was 9.23 or higher in 12 (7.7%) of 156 participants. The median duration of follow up was 22 months with a range of 13–35 months. Fifty-six (35%) of the subjects were receiving neither hydroxyurea nor chronic transfusion; among these the prevalence of tricuspid regurgitation velocity of 2.60 m/sec or higher was 14.0% and of E/Etdi of 9.23 or higher was 11.3%. The prevalence of elevated tricuspid regurgitation velocity or elevated E/Etdi according to hydroxyurea treatment or chronic transfusion therapy is shown in Table 2. The prevalence of elevated tricuspid regurgitation velocity was higher in children receiving chronic transfusion therapy and the prevalence of elevated E/Etdi was lower in children receiving hydroxyurea therapy.
Table 2.
Baseline elevations of tricuspid regurgitation velocity and mitral valve E/Etdi ratio by hydroxyurea therapy and chronic blood transfusion. Results in n. (%).
Correlation of baseline and follow-up results
In our previously published cross-sectional analysis of baseline data, we observed significant independent associations of higher hemolytic component and lower hemoglobin oxygen saturation with elevated tricuspid regurgitation velocity.9 In the present study, we evaluated how baseline screening observations correlate with repeat observations 13 to 35 months later and found the expected significant relationships for hemoglobin concentration (Figure 1A), hemolytic component (Figure 1B), hemoglobin O2 saturation (Figure 1C), tricuspid regurgitation velocity (Figure 1D), LVIDD z score (Figure 1E), and mitral valve E/Etdi ratio (Figure 1F). Hydroxyurea usage (58%) and participation in a chronic transfusion program (16%) did not differ significantly from the proportions at baseline.
Figure 1.
Correlation of baseline and follow-up measurements: (A) hemoglobin concentration, (B) hemolytic component, (C) hemoglobin oxygen saturation, (D) tricuspid regurgitation velocity, e) LVIDD z-score, (F) mitral valve E/Etdi, (G) six-minute walk distance.
One hundred and thirty-nine of the participants with a baseline tricuspid regurgitation velocity measurement also had a follow-up measurement. Eight of 20 (40.0%) participants with a baseline tricuspid regurgitation velocity of 2.60 m/sec or higher had a follow-up elevation compared to 18 (15.1%) of 119 participants with baseline tricuspid regurgitation velocity below 2.60 m/sec (P=0.008). The mean (SD) follow-up tricuspid regurgitation velocity was 2.51 (0.27) m/sec in participants with baseline tricuspid regurgitation velocity of 2.60 m/sec or higher compared to 2.34 (0.22) m/sec in participants with baseline tricuspid regurgitation velocity below 2.60 m/sec (P=0.003). In multivariate models, neither treatment with hydroxyurea nor participation in a chronic transfusion program was a significant predictor of follow-up tricuspid regurgitation velocity, and adjustment for these potential confounders did not affect the results.
Two (18.2%) of 11 participants with a baseline E/Etdi over 9.22 had an elevated E/Etdi at follow up compared to three (2.2%) of 134 without baseline elevation (P=0.005). The mean (SD) follow-up E/Etdi was 8.72 (2.29) in participants with elevated E/Etdi at baseline compared to 6.49 (1.33) in participants without elevated E/Etdi at baseline (P<0.0001). At follow up, 68.4% of participants with a baseline hemolytic component above the median had a hemolytic component above the median compared to 31.0% with baseline hemolytic component below the median (P=0.001). The mean (SD) follow-up hemolytic component was 0.57 (1.20) in participants with hemolytic component above the median at baseline compared to −0.83 (1.40) in participants with hemolytic component below the median at baseline (P<0.0001).
Evolution of six-minute walk distance during follow up
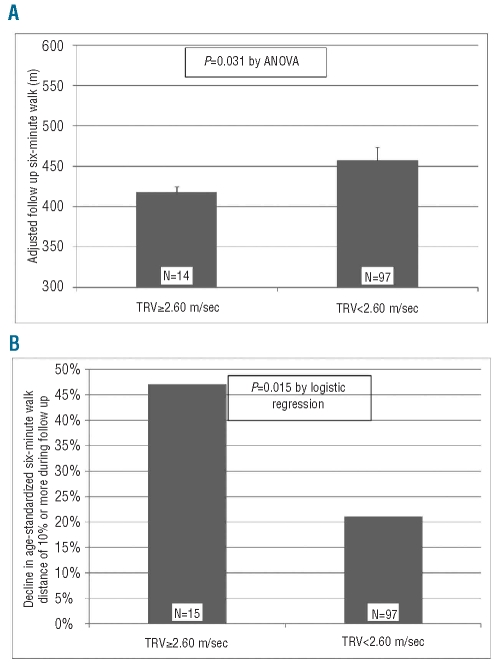
To evaluate functional capacity, the six-minute walk distance was measured at both baseline and follow up in 118 hemoglobin SS participants and there was significant correlation between the two measurements (Figure 1G). Among 111 hemoglobin SS patients, elevated baseline tricuspid regurgitation velocity was associated with a shorter follow-up six-minute walk distance (beta = −39.0, 95% CI = −3.6 to −74.5, P=0.031) after adjusting for baseline six-minute walk distance and duration of follow-up (Figure 2A). On the other hand, neither lower baseline hemoglobin concentration nor elevated E/Etdi ratio were associated with a shorter walk distance at follow up (P=0.8 in each case). After age-standardization, the frequency of a 10% or greater decline in the six-minute walk distance during follow up was 47% in participants with elevated tricuspid regurgitation velocity compared to 21% in those without elevated velocity (P=0.033). By logistic regression, elevated baseline tricuspid regurgitation velocity was associated with an estimated 4.4-fold increase in the odds of a 10% or greater decline in six-minute walk distance during follow up (95% CI = 1.3–14.5; P=0.015) after adjusting for duration of follow up (Figure 2B). Neither treatment with hydroxyurea nor participation in a chronic transfusion program was a significant predictor of follow-up six-minute walk distance, and adjustment for these potential confounders did not affect the results.
Figure 2.
Six-minute walk distance at follow up according to baseline tricuspid regurgitation velocity. (A) Mean (SE) distance. (B) Ten percent or more decline in age-standardized six-minute walk distance.
Increase in tricuspid regurgitation velocity during follow up
The mean (SD) tricuspid regurgitation velocity at baseline in 149 participants with this measurement available was 2.33 (0.26) m/sec. Among 139 participants with tricuspid regurgitation velocity measurable at both baseline and follow up, 24 (17.3%) had an increase in the velocity of one SD or more: 13.6% of participants with baseline hemolytic component below the median had such an increase compared to 20.6% of participants with baseline hemolytic component above the median. After adjustment for the duration of follow up and baseline velocity, a hemolytic component above the median was associated with an estimated 9.0-fold increase in the odds of an increase in the tricuspid regurgitation velocity of one SD or more (95% CI= 1.9 – 43.1; P=0.006). Similar findings applied to the measurements from which the hemolytic component was derived. An LDH above the median was associated with an estimated 12.4-fold increase in the odds of an increase in the tricuspid regurgitation velocity of one SD or more (P=0.004), an AST above the median with an estimated 6.6-fold increase in the odds (P=0.011), a bilirubin above the median with an estimated 12.9-fold increase in the odds (P=0.001), and a reticulocyte percent above the median with an estimated 10.4-fold increase in the odds (P=0.007).
Forty-two patients on neither hydroxyurea nor chronic transfusion at baseline had tricuspid regurgitation velocity measured at both baseline and follow up, and 10 (23.8%) had an increase of one SD or more. In this subgroup of participants on neither hydroxyurea nor chronic transfusion, a hemolytic component above the median was associated with an estimated 4.3-fold increase in the odds of an increase in the tricuspid regurgitation velocity of one SD or more after adjustment for the duration of follow up and baseline velocity (95% CI = 0.3 – 54.0; P=0.3).
Increase in mitral valve E/Etdi during follow up
The mean (SD) E/Etdi at baseline in 156 participants with this measurement available was 6.82 (1.56). Among 145 participants with E/Etdi measurable at both baseline and follow up, 17 (11.7%) had an increase in E/Etdi of one SD or more: 10.1% of participants with baseline hemolytic component below the median had such an increase compared to 14.3% of participants with baseline hemolytic component above the median. After adjustment for the duration of follow up and baseline E/Etdi, a hemolytic component above the median was associated with an estimated 1.6-fold increase in the odds of an increase in the E/Etdi of one SD or more (95% CI = 0.5–4.5; P=0.4).
Forty-seven patients on neither hydroxyurea nor chronic transfusion at baseline had E/Etdi measured at both baseline and follow up, and 6 (12.8%) had an increase of one SD or more. In this subgroup of participants on neither hydroxyurea nor chronic transfusion, a hemolytic component above the median was associated with an estimated 4.4-fold increase in the odds of an increase in E/Etdi of one SD or more after adjustment for the duration of follow up and baseline E/Etdi (95% CI = 0.4–43.1; P=0.2).
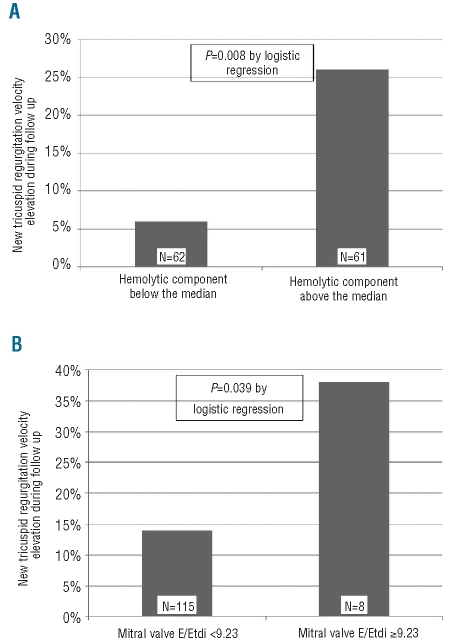
New development of elevated tricuspid regurgitation velocity elevation during follow up
To assess the new development of elevated tricuspid regurgitation velocity during the study, we evaluated 119 participants without elevated tricuspid regurgitation velocity at baseline. Eighteen (15.1%) of these participants developed an elevation of tricuspid regurgitation velocity by the time of the follow-up evaluation. After adjustment for the follow-up interval, higher baseline hemolytic component (P=0.002), lower baseline hemoglobin concentration (P=0.033) and higher mitral valve E/Etdi ratio (P=0.030) were individually associated with increased odds of newly developing velocity of 2.60 m/sec or higher during follow up. Further analysis indicated that only the hemolytic component and mitral valve E/Etdi ratio were independent predictors of newly developing elevated velocity. Four of 62 hemoglobin SS participants (6.5%) with lower hemolytic component at baseline developed elevated velocity during follow up compared to 14 of 61 (26.2%) with higher hemolytic component. Sixteen of 115 children (13.9%) with E/Etdi ratio below 9.23 developed elevated velocity during follow up compared to 3 of 8 (28.6%) with E/Etdi ratio over this limit. In a logistic regression analysis, each 12-month interval of follow up was associated with a 6.3-fold increase in the odds of newly developing elevated velocity during follow up (95% CI 1.4–27.6; P=0.015), elevated hemolytic component at baseline with an estimated 9.0-fold increase in the odds (95% CI 1.8–44.8; P=0.008) (Figure 3A), and elevated mitral valve E/Etdi ratio with an estimated 6.1-fold increase in the odds (95% CI 1.1–41.8; P=0.039) (Figure 3B).
Figure 3.
New development of tricuspid regurgitation velocity 2.60 m/sec or over during follow up according to (A) baseline hemolytic component and (B) mitral valve E/Etdi ratio.
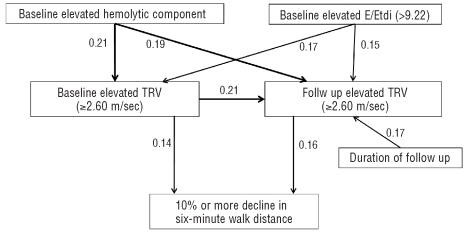
Pathway analysis of the relationships of hemolytic component, tricuspid regurgitation velocity and E/Etdi ratio with decline in six-minute walk distance (Figure 4)
Figure 4.
Pathway analysis of elevated tricuspid regurgitation velocity (TRV) and decline of age-standardized six-minute walk distance. Standardized betas are indicated in the model. χ2= 8.6 (P=0.6). Root Mean Square Error of Approximation of model = 0.0 (90% CI = 0.0–0.08). Each beta represents a positive association with a significance level of less than 0.021. According to this analysis baseline elevations of hemolytic component and E/Etdi were directly related to both baseline and follow up elevations of tricuspid regurgitation velocity. In tandem, baseline elevation of tricuspid regurgitation velocity and duration of follow up were both associated with follow-up elevation in the velocity. In turn, both baseline and follow-up tricuspid regurgitation velocity were directly associated with decline in six-minute walk distance of 10% or more.
In pathway analysis, both baseline higher hemolytic component and increased E/Etdi ratio were significant predictors of elevated tricuspid regurgitation velocity at baseline and follow up, and baseline elevated tricuspid regurgitation velocity was also a predictor of elevated velocity at follow up. Both baseline and follow-up elevations of tricuspid regurgitation velocity were associated with higher risk of a 10% or more decline in the age-standardized six-minute walk distance. This model fits the data well (χ2 = 8.6; degrees of freedom = 10; P=0.6 and Root Mean Square Error of Approximation = 0.0; 90% confidence interval 0.0 – 0.08).
Adverse outcomes at follow up according to baseline hemolytic component and tricuspid regurgitation velocity
Prospectively chosen 2-year outcomes in this study included death, stroke, acute chest syndrome and blood transfusion requirement during the follow-up interval. New events, i.e. events that occurred during the follow-up interval in subjects not reporting the complication at baseline, are summarized in Table 3. None of 133 participants without a past history of stroke developed a stroke during the follow-up period. Two (1.3%) of 160 participants died during the follow-up period. One of these children had elevated hemolytic component and history of stroke at baseline but neither of them was observed to have elevated baseline tricuspid regurgitation velocity or mitral valve E/Etdi ratio. Elevated mitral valve E/Etdi ratio, but not increased hemolytic component or elevated tricuspid regurgitation velocity, was associated with higher proportion of new acute chest syndrome episodes (P<0.001) and new transfusion (P=0.043).
Table 3.
New adverse outcomes during follow up, results are in n. (%).
Discussion
In our previously reported prospective cross sectional study of 310 children and adolescents with sickle cell disease at steady state,9 we found an 11.0% prevalence of elevated tricuspid regurgitation velocity (≥2.60 m/sec). The prevalence was 14.0% among children with sickle cell anemia (homozygous hemoglobin SS genotype) and 3.6% among children with other genotypes. We now report that, in the follow up of the children with sickle cell anemia, baseline elevation of tricuspid regurgitation velocity was predictive of a decline in the age-standardized six-minute walk distance during a follow-up interval that ranged from 13 to 35 months. Further research should determine whether an elevation of tricuspid regurgitation velocity may also identify a subset of children and adolescents at heightened risk for becoming adults with high pulmonary arterial pressures, low six-minute walk distance,39 and high rate of early mortality.8,10,11
Also, among hemoglobin SS participants without initial elevation of tricuspid regurgitation velocity, we observed that a high hemolytic component and elevated mitral valve E/Etdi ratio at baseline and the duration of follow up were independent predictors of the new development of elevated tricuspid regurgitation velocity at follow up. Thus, our results are consistent with age-related increases in the prevalence of high pulmonary artery pressure that are linked to a high intensity of hemolysis and to left ventricular diastolic dysfunction. The derivation of a hemolytic component and logistic regression analysis allowed us to find a statistically stronger contribution of hemolysis than that of anemia to a high tricuspid regurgitation velocity. This is consistent with our previous model based on biochemical evidence of nitric oxide scavenging by plasma hemoglobin and arginine depletion by plasma arginase, plasma hemoglobin and arginase being products of intravascular red blood cell breakdown.5,6 The additional finding that elevated E/Etdi ratio was an independent predictor of the new development of elevated tricuspid regurgitation velocity in this cohort parallels findings in adults with sickle cell disease that elevated pulmonary capillary wedge pressure is a frequent accompaniment of right heart catheterization-documented pulmonary hypertension.13 Because of the low prevalence of elevated mitral valve E/Etdi ratio in the present cohort, hemolytic component was a more important risk factor than elevated mitral valve E/Etdi ratio for new onset of elevated tricuspid regurgitation velocity, the population attributable risks being 73% versus 26%.
Pathway analysis was consistent with the possibility that the degree of hemolysis and elevated left ventricular filling pressure at baseline together contributed to elevation of tricuspid regurgitation velocity at both baseline and follow up. In turn, these elevations in estimated pulmonary artery pressure were more directly associated with decline in functional capacity during follow up.
There are several limitations to our study. First, the median follow-up interval of 22 months, which was dictated by the limited period of funding, was short and may have prevented identifying clinically important associations of elevations of hemolysis and tricuspid regurgitation velocity with other adverse events. Second, the numbers of participants having elevations of tricuspid regurgitation velocity or mitral valve E/Etdi at baseline were relatively small. To fully characterize the clinical associations of elevations of hemolysis and tricuspid regurgitation velocity in children with sickle cell anemia will require the longitudinal study of a larger cohort than was included in this report. Third, the tricuspid regurgitation velocity is an indirect reflection of systolic pulmonary artery pressure that can vary from day to day. A preliminary report in adult sickle cell disease individuals suggested that the specificity of a tricuspid regurgitation velocity of 2.8 m/sec for predicting high mean pulmonary artery pressure was 50%.40 Our results showed a strong correlation between two measurements taken about two years apart, but a single screening elevated measurement was confirmed on repeat testing in less than half of the cases. Fourth, the degree of hemolysis may be affected considerably by a recent blood transfusion. Therefore, in this study, blood collection, echocardiogram and six-minute walk testing were performed at least three weeks after a blood transfusion.
In summary, our results indicate that elevated tricuspid regurgitation velocity may be a biomarker in children with sickle cell anemia that is associated with a decline in exercise capacity and that increases in prevalence with age, especially in the presence of high hemolytic rate or increased left ventricular filling pressure. Further research should determine whether elevated tricuspid regurgitation velocity and mitral valve E/Etdi ratio identify children with sickle cell anemia who will become adults with high hemolytic rate and elevated tricuspid regurgitation velocity, a group known to be at high risk for early mortality. The clinical importance of pulmonary hypertension in sickle cell disease and the usefulness of elevated tricuspid regurgitation velocity to predict pulmonary hypertension in sickle cell disease are controversial.12 Nevertheless, we propose that accumulated evidence may justify consideration of clinical trials directed at risk reduction in an early pre-symptomatic stage in childhood to prevent the development of clinically significant elevation of tricuspid regurgitation velocity in adulthood. Potential modalities to be tested would include hydroxyurea or a blood transfusion program. This proposed approach is conceptually similar in the general population to identifying and treating systemic hypertension in children in order to reduce cardiovascular risks in adulthood.41
Footnotes
Funding: Supported in part by grant ns. 2 R25 HL003679-08 and 1 R01 HL079912-02 from NHLBI, by Howard University GCRC grant n. 2MOI RR10284-10 from NCRR, NIH, Bethesda, MD, and by the intramural research program of the National Institutes of Health.
Authorship and Disclosures
The information provided by the authors about contributions from persons listed as authors and in acknowledgments is available with the full text of this paper at www.haematologica.org.
Financial and other disclosures provided by the authors using the ICMJE (www.icmje.org) Uniform Format for Disclosure of Competing Interests are also available at www.haematologica.org.
References
- 1.Hayag-Barin JE, Smith RE, Tucker FC., Jr Hereditary spherocytosis, thrombocytosis, and chronic pulmonary emboli: a case report and review of the literature. Am J Hematol. 1998;57(1):82–4. doi: 10.1002/(sici)1096-8652(199801)57:1<82::aid-ajh15>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 2.Collins FS, Orringer EP. Pulmonary hypertension and cor pulmonale in the sickle hemoglobinopathies. Am J Med. 1982;73 (6):814–21. doi: 10.1016/0002-9343(82)90763-x. [DOI] [PubMed] [Google Scholar]
- 3.Aessopos A, Farmakis D, Karagiorga M, Voskaridou E, Loutradi A, Hatziliami A, Joussef J, Rombos J, Loukopoulos D. Cardiac involvement in thalassemia intermedia: a multicenter study. Blood. 2001;97(11):3411–6. doi: 10.1182/blood.v97.11.3411. [DOI] [PubMed] [Google Scholar]
- 4.Heller PG, Grinberg AR, Lencioni M, Molina MM, Roncoroni AJ. Pulmonary hypertension in paroxysmal nocturnal hemoglobinuria. Chest. 1992;102(2):642–3. doi: 10.1378/chest.102.2.642. [DOI] [PubMed] [Google Scholar]
- 5.Reiter CD, Wang X, Tanus-Santos JE, Hogg N, Cannon RO, 3rd, Schechter AN, Gladwin MT. Cell-free hemoglobin limits nitric oxide bioavailability in sickle-cell disease. Nat Med. 2002;8(12):1383–9. doi: 10.1038/nm1202-799. [DOI] [PubMed] [Google Scholar]
- 6.Morris CR, Kato GJ, Poljakovic M, Wang X, Blackwelder WC, Sachdev V, et al. Dysregulated arginine metabolism, hemolysis-associated pulmonary hypertension, and mortality in sickle cell disease. JAMA. 2005;294(1):81–90. doi: 10.1001/jama.294.1.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Machado RF, Gladwin MT. Chronic sickle cell lung disease: new insights into the diagnosis, pathogenesis and treatment of pulmonary hypertension. Br J Haematol. 2005;129(4):449–64. doi: 10.1111/j.1365-2141.2005.05432.x. [DOI] [PubMed] [Google Scholar]
- 8.Gladwin MT, Sachdev V, Jison ML, Shizukuda Y, Plehn JF, Minter K, et al. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med. 2004;350(9):886–95. doi: 10.1056/NEJMoa035477. [DOI] [PubMed] [Google Scholar]
- 9.Minniti CP, Sable C, Campbell A, Rana S, Ensing G, Dham N, et al. Elevated tricuspid regurgitant jet velocity in children and adolescents with sickle cell disease: association with hemolysis and hemoglobin oxygen desaturation. Haematologica. 2009;94(3):340–7. doi: 10.3324/haematol.13812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ataga KI, Moore CG, Jones S, Olajide O, Strayhorn D, Hinderliter A, Orringer EP. Pulmonary hypertension in patients with sickle cell disease: a longitudinal study. Br J Haematol. 2006;134(1):109–15. doi: 10.1111/j.1365-2141.2006.06110.x. [DOI] [PubMed] [Google Scholar]
- 11.De Castro LM, Jonassaint JC, Graham FL, Ashley-Koch A, Telen MJ. Pulmonary hypertension associated with sickle cell disease: clinical and laboratory endpoints and disease outcomes. Am J Hematol. 2008;83 (1):19–25. doi: 10.1002/ajh.21058. [DOI] [PubMed] [Google Scholar]
- 12.Bunn HF, Nathan DG, Dover GJ, Hebbel RP, Platt OS, Rosse WF, Ware RE. Pulmonary hypertension and nitric oxide depletion in sickle cell disease. Blood. 2010;116(5):687–92. doi: 10.1182/blood-2010-02-268193. [DOI] [PubMed] [Google Scholar]
- 13.Castro O, Hoque M, Brown BD. Pulmonary hypertension in sickle cell disease: cardiac catheterization results and survival. Blood. 2003;101(4):1257–61. doi: 10.1182/blood-2002-03-0948. [DOI] [PubMed] [Google Scholar]
- 14.Sachdev V, Machado RF, Shizukuda Y, Rao YN, Sidenko S, Ernst I, et al. Diastolic dysfunction is an independent risk factor for death in patients with sickle cell disease. J Am Coll Cardiol. 2007;49(4):472–9. doi: 10.1016/j.jacc.2006.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sedrak A, Rao SP, Miller ST, Hekmat V, Rao M. A prospective appraisal of pulmonary hypertension in children with sickle cell disease. J Pediatr Hematol Oncol. 2009;31 (2):97–100. doi: 10.1097/MPH.0b013e31818e5343. [DOI] [PubMed] [Google Scholar]
- 16.Kato GJ, Onyekwere OC, Gladwin MT. Pulmonary hypertension in sickle cell disease: relevance to children. Pediatr Hematol Oncol. 2007;24(3):159–70. doi: 10.1080/08880010601185892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pashankar FD, Carbonella J, Bazzy-Asaad A, Friedman A. Prevalence and risk factors of elevated pulmonary artery pressures in children with sickle cell disease. Pediatrics. 2008;121(4):777–82. doi: 10.1542/peds.2007-0730. [DOI] [PubMed] [Google Scholar]
- 18.Lee MT, Small T, Khan MA, Rosenzweig EB, Barst RJ, Brittenham GM. Doppler-defined pulmonary hypertension and the risk of death in children with sickle cell disease followed for a mean of three years. Br J Haematol. 2009;146(4):437–41. doi: 10.1111/j.1365-2141.2009.07779.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liem RI, Young LT, Thompson AA. Prolonged QTc interval in children and young adults with sickle cell disease at steady state. Pediatr Blood Cancer. 2009;52 (7):842–6. doi: 10.1002/pbc.21973. [DOI] [PubMed] [Google Scholar]
- 20.Campbell A, Minniti CP, Nouraie M, Arteta M, Rana S, Onyekwere O, et al. Prospective evaluation of haemoglobin oxygen saturation at rest and after exercise in paediatric sickle cell disease patients. Br J Haematol. 2009;147(3):352–9. doi: 10.1111/j.1365-2141.2009.07854.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dahoui HA, Hayek MN, Nietert PJ, Arabi MT, Muwakkit SA, Saab RH, et al. Pulmonary hypertension in children and young adults with sickle cell disease: Evidence for familial clustering. Pediatr Blood Cancer. 2009;54(3):398–402. doi: 10.1002/pbc.22306. [DOI] [PubMed] [Google Scholar]
- 22.Zilberman MV, Du W, Das S, Sarnaik SA. Evaluation of left ventricular diastolic function in pediatric sickle cell disease patients. Am J Hematol. 2007;82(6):433–8. doi: 10.1002/ajh.20866. [DOI] [PubMed] [Google Scholar]
- 23.Hagar RW, Michlitsch JG, Gardner J, Vichinsky EP, Morris CR. Clinical differences between children and adults with pulmonary hypertension and sickle cell disease. Br J Haematol. 2008;140(1):104–12. doi: 10.1111/j.1365-2141.2007.06822.x. [DOI] [PubMed] [Google Scholar]
- 24.Pashankar FD, Carbonella J, Bazzy-Asaad A, Friedman A. Longitudinal follow up of elevated pulmonary artery pressures in children with sickle cell disease. Br J Haematol. 2009;144(5):736–41. doi: 10.1111/j.1365-2141.2008.07501.x. [DOI] [PubMed] [Google Scholar]
- 25.Lai WW, Geva T, Shirali GS, Frommelt PC, Humes RA, Brook MM, et al. Guidelines and standards for performance of a pediatric echocardiogram: a report from the Task Force of the Pediatric Council of the American Society of Echocardiography. J Am Soc Echocardiogr. 2006;19(12):1413–30. doi: 10.1016/j.echo.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 26.Ensing G, Seward J, Darragh R, Caldwell R. Feasibility of generating hemodynamic pressure curves from noninvasive Doppler echocardiographic signals. J Am Coll Cardiol. 1994;23(2):434–42. doi: 10.1016/0735-1097(94)90431-6. [DOI] [PubMed] [Google Scholar]
- 27.Pettersen MD, Du W, Skeens ME, Humes RA. Regression Equations for Calculation of Z Scores of Cardiac Structures in a Large Cohort of Healthy Infants, Children, and Adolescents: An Echocardiographic Study. J Am Soc Echocardiogr. 2008;21(8):922–34. doi: 10.1016/j.echo.2008.02.006. [DOI] [PubMed] [Google Scholar]
- 28.Quinones MA, Otto CM, Stoddard M, Waggoner A, Zoghbi WA. Recommendations for quantification of Doppler echocardiography: a report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. J Am Soc Echocardiogr. 2002;15(2):167–84. doi: 10.1067/mje.2002.120202. [DOI] [PubMed] [Google Scholar]
- 29.Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quinones MA. Doppler tissue imaging: a noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol. 1997;30(6):1527–33. doi: 10.1016/s0735-1097(97)00344-6. [DOI] [PubMed] [Google Scholar]
- 30.ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 31.Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783–5. [PubMed] [Google Scholar]
- 32.Nixon PA, Joswiak ML, Fricker FJ. A six-minute walk test for assessing exercise tolerance in severely ill children. J Pediatr. 1996;129(3):362–6. doi: 10.1016/s0022-3476(96)70067-7. [DOI] [PubMed] [Google Scholar]
- 33.Gulmans VA, van Veldhoven NH, de Meer K, Helders PJ. The six-minute walking test in children with cystic fibrosis: reliability and validity. Pediatr Pulmonol. 1996;22(2):85–9. doi: 10.1002/(SICI)1099-0496(199608)22:2<85::AID-PPUL1>3.0.CO;2-I. [DOI] [PubMed] [Google Scholar]
- 34.Galie N, Olschewski H, Oudiz RJ, Torres F, Frost A, Ghofrani HA, et al. Ambrisentan for the treatment of pulmonary arterial hypertension: results of the ambrisentan in pulmonary arterial hypertension, randomized, double-blind, placebo-controlled, multicenter, efficacy (ARIES) study 1 and 2. Circulation. 2008;117(23):3010–9. doi: 10.1161/CIRCULATIONAHA.107.742510. [DOI] [PubMed] [Google Scholar]
- 35.Pont-Kingdon G, Chou LS, Damjanovich K, Sumner K, Herrmann M, Erali M, Lyon E. Multiplex genotyping by melting analysis of loci-spanning probes: beta-globin as an example. Biotechniques. 2007;42(2):193–7. doi: 10.2144/000112330. [DOI] [PubMed] [Google Scholar]
- 36.Van Belle G, Fisher LD, Heageny PJ, Lumley T. Biostatistics: A Methodology for the Health Sciences. Second ed. Hoboken: John Wiley & Sons; 2004. [Google Scholar]
- 37.Genser B, Cooper PJ, Yazdanbakhsh M, Barreto ML, Rodrigues LC. A guide to modern statistical analysis of immunological data. BMC Immunol. 2007;8:27. doi: 10.1186/1471-2172-8-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Raykov T, Marcoulides GA. Path analysis A First Course in Structural Equation Modeling. Mahwah, NJ: Lawrence Erlbaum Associates, Publishers; 2006. pp. 77–116. [Google Scholar]
- 39.Anthi A, Machado RF, Jison ML, Taveira-Dasilva AM, Rubin LJ, Hunter L, et al. Hemodynamic and functional assessment of patients with sickle cell disease and pulmonary hypertension. Am J Respir Crit Care Med. 2007;175(12):1272–9. doi: 10.1164/rccm.200610-1498OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bachir D, Parent F, Hajji L, Inamo J, Loko G, Lionnet F, Driss F, et al. Prospective multi-centric survey on pulmonary hypertension (PH) in adults with sickle cell disease. Abstract 572. American Society of Hematology Annual Meeting; New Orelans Louisianna. 2009. [Google Scholar]
- 41.NHLBI. The Fourth Report on the Diagnosis, Evaluation, and Treatment of High Blood Pressure in Children and Adolescents. Bethesda, MD: National Institutes of Health; 2005. [Google Scholar]