Introduction
The alarming increase in obesity among children in the United States (Jolliffe, 2004) has been accompanied by increases in the prevalence of hypertension (Muntner et al., 2004; Sorof et al., 2004), type 2 diabetes (Bloomgarden, 2004), and the metabolic syndrome (Cook et al., 2003; Duncan et al., 2004). Of particular concern is the disproportionate effect the obesity epidemic has had on minority children, who have greater prevalence of obesity than is seen in white children (Hedley et al., 2004) and are likely to shoulder much of the future burden of weight-related morbidity and mortality (Davis et al., 2000) unless effective treatments are found. While health care providers increasingly counsel patients about obesity (Rao, 2005), one of their foremost questions remains how best to manage this problem (Chien et al., 2006).
Identifying strategies to promote physical activity may be critical to stemming the tide of obesity. Physical inactivity, which is implicated in the development of obesity, is closely linked to cardiovascular risk factors independent of weight status among children (Andersen et al., 2006; Brage et al., 2004) and adults (Farrell et al., 2002; Blair and Brodney, 1999). However, despite the known benefits of physical activity, American youth are far from meeting recommended activity goals and minority children are less active than white children (YRBSS, 2004; NSCH, 2005). Most office-based interventions promoting physical activity have not demonstrated sustained increases in activity levels (Madsen et al., 2007; McCallum et al., 2006; Patrick et al., 2006; Saelens et al., 2002), in part because of child preferences for group activities (Madsen et al., 2007). School-based interventions to increase physical activity and reduce pediatric obesity have successfully reached children of diverse backgrounds in a group setting but, with a few exceptions (Gortmaker et al., 1999; Spiegel and Foulk, 2006), have had little effect on obesity (Caballero et al., 2003; Harrell et al., 1998; Resnicow et al., 1992; Webber et al., 1996; Sahota et al., 2001). In-school interventions have cited insufficient dose of physical activity, due in part to academic constraints during the school day, as a factor limiting their efficacy (Webber et al., 1996; Caballero et al., 2003). Physical Education (PE) instructors in the U.S. have also cited the low academic value of PE as a barrier to increasing activity during the school day (Barroso et al., 2005).
The frequently sedentary after-school hours (Hofferth and Jankuniene, 2001) are a promising venue in which to increase physical activity and reduce obesity among youth. Recent studies promoting physical activity in the after-school setting have reported mixed results regarding changes in weight status (Jago et al., 2006; Barbeau et al., 2007; Gutin et al., 2008). Several studies have had low program attendance (Robinson et al., 2003; Yin et al., 2005; Barbeau et al., 2007), a difficulty faced by many after-school programs (Dynarski et al., U.S. Dept of Ed, 2003; Weisman and Gottfredson, 2001).
Established after-school programs promoting activity that have track records of high attendance and retention could be community partners for primary care providers attempting to address obesity among minority children. One such program, America SCORES Bay Area (SCORES) is an after-school soccer and literacy program serving children who might otherwise have limited access to extracurricular activities, including physical activity. SCORES provides up to six hours a week of structured vigorous physical activity and includes four hours of a curriculum promoting self-esteem and literacy, which positively affect health behaviors and outcomes (Bandura, 1986; Schillinger et al., 2006). The investigators of this study hypothesized SCORES would positively impact both cardio respiratory endurance and reduce body mass index (BMI) and might have high enough levels of attendance and retention to warrant a large randomized trial.
Methods
Subjects
This pilot study employed a one-group pre-test post-test design, assessing changes in BMI and fitness over one school-year in 3rd to 5th grade children enrolled in SCORES in nine San Francisco primary schools. All parents/ guardians signed consent forms for their children to participate in SCORES, including anthropometric and fitness evaluations. Subjects gave verbal assent to participate. SCORES staff members were trained in data collection and collected all anthropometric and fitness data and provided investigators at the University of California, San Francisco (UCSF) with a de-identified data set. The Committee on Human Research at UCSF approved this study.
Description of Program
America SCORES began in Washington D.C. in 1994 with a concerned public-school teacher who saw after-school time as an opportunity to improve student literacy and decided to use soccer as a “hook” to draw children in. Over the last 16 years, the non-profit program has developed a national curriculum and has expanded to 14 cities, including the San Francisco Bay Area. Bay Area SCORES is conducted in 24 public primary schools selected for having students with low academic performance and a high percentage of low-income families. For eight weeks in the fall and ten weeks in the spring, children in the program play soccer three days a week (two practice days with up to 2 hours of moderate-to-vigorous physical activity and one inter-school game day with a warm-up period followed by a 1-hour game) and performing community service or creative writing the remaining two days a week. The program uses separate coaches for the soccer and literacy curricula, most of whom are teachers during the day at the same schools where they coach for SCORES. In the spring, each team picks a community service project, which they execute under the guidance of their writing coach. Such projects have included community food, clothing, and toy drives, and neighborhood beautification activities. The program’s curriculum, focused on literacy, leadership and teamwork skills, is identical for both genders, but all activities are conducted separately for girls and boys to best match sports skills. Bay Area SCORES, in existence for eight years, receives part of its funding from the Cities of San Francisco and Oakland, with the balance coming from corporate and individual donors. SCORES coaches recruit up to 17 girls and 17 boys in the fourth and fifth grades at each school, focusing on children in need of literacy development and on those who might not have other opportunities to participate in extra-curricular activities.
Procedure
Trained SCORES staff members collected BMI and fitness data from participants during the 2004-2005 school year at nine San Francisco schools at baseline (in the fall) and at follow-up (after the spring session). Fitness was assessed using the 20-meter shuttle test, which has been validated as a measure of aerobic capacity in children (Liu et al., 1992; Leger et al., 1988). Anthropometric measures were taken with children in indoor clothes and shoes off: weight was assessed to the nearest tenth of a kilogram using a portable electronic scale, and height to the nearest tenth of a centimeter using a portable stadiometer (Seca model 214, Seca, Hamburg, Germany).
Data Analysis
All analyses were performed in STATA version 8 (Statacorp LP, College Station, TX), taking clustering by school into account. BMI was calculated as weight(kg)/height(m)2. BMI z-scores were calculated using the 2000 CDC Growth reference data (Kuczmarski et al., 2000; National Center for Health Statistics, 2002). BMI categories are: overweight (BMI 85th to 95thpercentile) and obese (BMI ≥ 95th percentile). Each subject’s predicted follow-up BMI was calculated using each child’s baseline BMI z-score, assuming no change in z-score (i.e. they stayed on their CDC growth curve).
Analysis included: a paired t-test to assess the significance of change in BMI z-score and fitness from baseline to follow-up; two-group t-tests to compare change in BMI z-score and fitness (total number of laps run) between different groups of children; multivariate regression including attendance, race and baseline fitness and BMI z-score to assess the effect of multiple variables on change in BMI z-score and change in fitness; and the Wilcoxon signed-rank test to compare the proportion of children who were obese (based on a BMI at or above the 95th percentile for age and sex) at baseline and at follow-up, after participating in SCORES. Logistic regression was used to look for difference in baseline variables between children with and without follow-up data and to look for predictors of dropping out of SCORES.
RESULTS
Average daily attendance in the program was 90% during the fall session and 84% in the spring. While there were no differences in attendance in the fall, in the spring session, African-American children attended 75% of the time compared to 86% attendance among other participants (p=0.018). Cumulative retention in the SCORES program is shown in Figure 1. Over 95% of enrolled children completed the fall session; 91% of children who started the spring session completed it. Compared to other participants, Latino children were 3.4 times less likely to drop out (95% CI 1.4, 8.4), adjusting for baseline fitness and BMI z-score.
Figure 1.
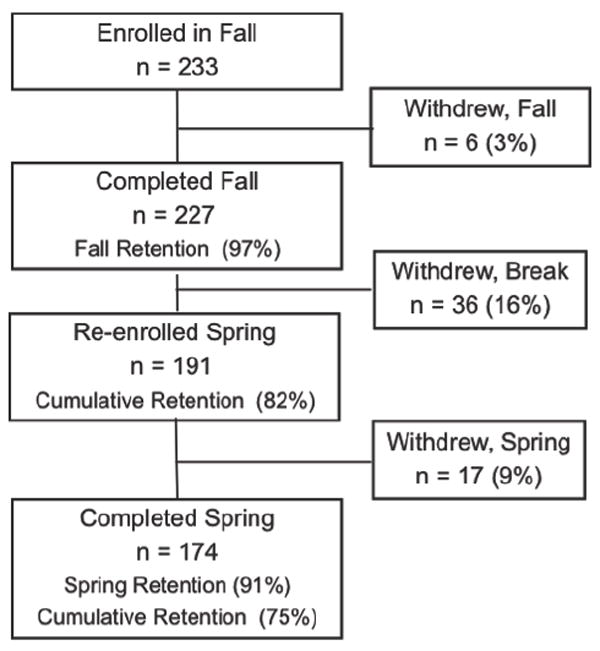
SCORES Program Retention
Baseline measures were collected on 178 children (76% of the 233 children enrolled in the fall). Baseline characteristics are presented in Table 1. Of note, at baseline 18% of children were overweight and 34% were obese. Asian boys had the highest prevalence of obesity (44%) followed by African-American boys (42%) and Latino boys (33%).
Table 1.
Baseline Demographics
| N = 178 | # or mean (% or SD) [range] |
|---|---|
| Female | 86 (48%) |
| Age (years) | 9.8 (0.9) [7.9 to 12.2] |
| BMI (kg/m2) | 20.9 (4.9) [13.4 to 36.8] |
| BMI z-score* | 1.01 (1.05) [-2.8 to 2.8] |
| Normal Wt | 86 (48%) |
| Overweight | 32 (18%) |
| Obese | 60 (34%) |
| Race | |
| Latino | 86 (48%) |
| Asian | 46 (26%) |
| African-American | 32 (18%) |
| White | 1 (1%) |
| Other/Unknown | 13 (7%) |
BMI z-scores of 0, 1.036 and 1.645 are equivalent to the 50th, 85th and 95th percentiles, respectively. A BMI z-score of 2.31 or greater is above the 99th percentile.
Of the 174 children completing the full year, follow-up measures were obtained on 128 children (74% of enrolled children), 91 of whom had baseline measures. There were no differences in attendance, race, baseline BMI z-score, or fitness between children with and without follow-up measures, but schools had significantly different rates of follow-up, ranging from 43% to 100%.
Children significantly increased the maximum number of laps they could run from a mean of 22 at baseline to 35 at follow-up (p<0.001), which correlates with a 2.6 ml/kg/min increase in VO2 max (Leger et al., 1988). This improvement in fitness was significant for children in each weight category (Figure 2). In a multivariate model including attendance, race and baseline fitness and BMI z-score, lower fitness levels at baseline predicted greater improvement in fitness over the school year (p=0.002), while higher baseline BMI z-scores predicted lesser improvements in fitness (p<0.001). Race did not significantly predict change in fitness although there was a trend for African-American children to show smaller gains (on average eight shuttles less than other participants, p =0.099).
Figure 2.
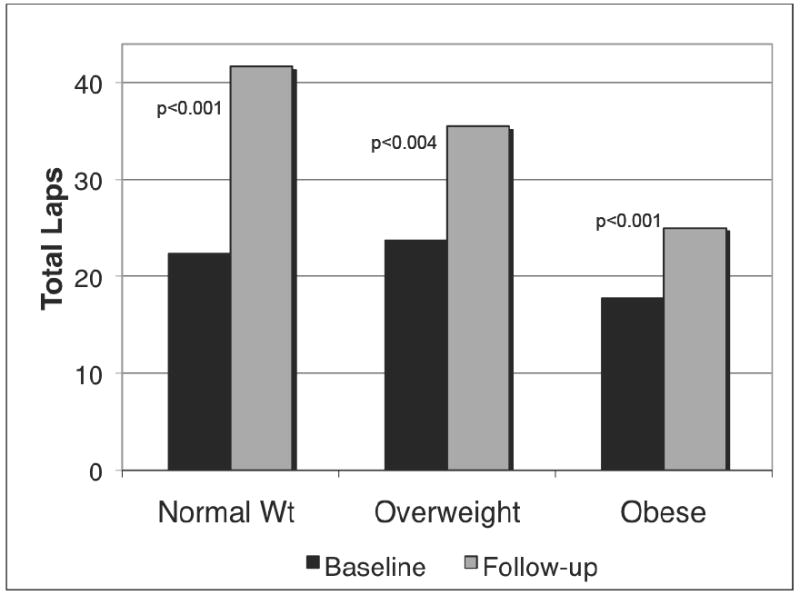
Mean laps run at baseline and follow-up, by BMI category
From baseline to the end of spring, BMI z-score decreased by 0.04 among all subjects (p=0.103) and by 0.05 among obese children (p=0.079). Response to the intervention differed significantly by race (p<0.05 for pair-wise comparisons), with Asian children demonstrating the greatest decrease in BMI z-score (−0.23, p<0.001) and African-American children demonstrating an increase in BMI z-score (+0.13, p=0.003) (Table 2). To put these numbers in perspective, for a 10-year old boy with a BMI at the 85th percentile whose height is increasing at the 50th percentile, a decrease in BMI z-score of 0.2 over 8 months translates to a weight increase that is 1.4 kg less than would be expected based on the 2000 CDC growth charts. For a similar boy with a 0.1 increase in BMI z-score over 8 months, it would mean gaining 0.8 kg more than expected. Figure 3 shows actual change in BMI versus the change that would be predicted had children remained on their growth curve (i.e. no change in BMI z-score). Baseline BMI z-score, fitness and average daily attendance did not significantly predict change in BMI z-score (modeled separately for African-American children because of interaction). The percent of children who were obese declined from 33% at baseline to 27% at follow-up (p=0.103).
Table 2.
Unadjusted change in BMI z-score over school-year
| All Subjects | African-Americans | Asian | Latino | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Category | n | Chg | p | n | Chg | p | n | Chg | p | n | Chg | p |
| All Children | 91 | -.04 | 0.103 | 15 | +.13 | 0.003 | 17 | -.23 | <0.001 | 54 | -.03 | 0.317 |
| Normal Weight | 46 | -.03 | 0.473 | 8 | +.16 | 0.023 | 7 | -.30 | 0.004 | 29 | -.01 | 0.791 |
| Overweight | 16 | -.06 | 0.398 | 4 | +.07 | 0.404 | 6 | -.19 | 0.212 | 6 | -.01 | 0.913 |
| Obese | 29 | -.05 | 0.079 | 3 | +.12 | 0.172 | 4 | -.17 | 0.122 | 19 | -.06 | 0.034 |
| Girls | 47 | -.03 | 0.386 | 11 | +.14 | 0.004 | 10 | -.24 | 0.027 | 25 | -.02 | 0.602 |
| Boys | 44 | -.05 | 0.156 | 4 | +.09 | 0.403 | 7 | -.22 | 0.006 | 29 | -.04 | 0.402 |
Figure 3.
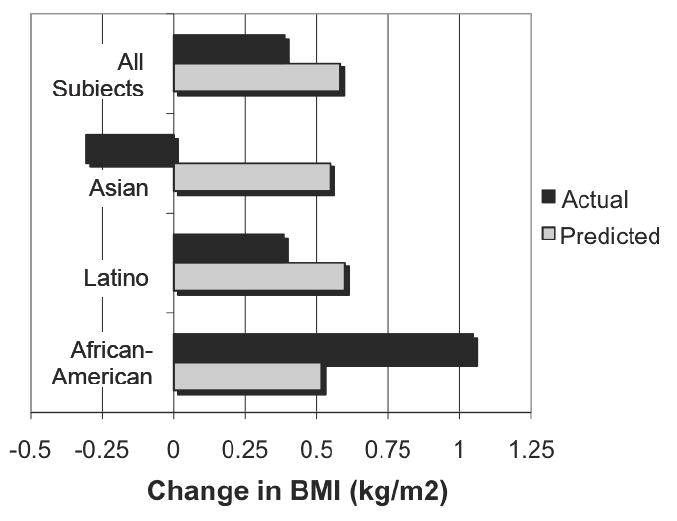
Actual vs predicted change in BMI over 8 months by race
DISCUSSION
While physicians can provide important information and encouragement about physical activity and nutrition, when children leave the physician’s office they are exposed to environments that do not encourage healthy choices. It is imperative to identify community partners that provide programs that are consistent with a healthy lifestyle. The promising results of this pilot study suggest that SCORES improves fitness among participants and may reduce obesity amongst Latino and Asian children. While a few interventions to prevent or address obesity have had success (Robinson, 1999; Barbeau et al., 2007), fewer have shown any significant improvement in anthropometric measures. It is clear that much work remains in addressing the obesity epidemic.
Compared to other interventions promoting physical activity in the after-school setting (Barbeau et al., 2007; Melnyk et al., 2007; Robinson et al., 2003; Yin et al., 2005), SCORES experienced high program attendance and retention within sessions. A major strength of this pilot study is that it evaluates a pre-existing, community-based program that appears to be sustainable and appealing to children. These results warrant further research on larger, diverse student populations to see if community-based programs of this type improve fitness and slow progression to obesity.
The decreases in BMI z-score suggest that on average, obese Latino and Asian children in SCORES gained almost 1 kilogram less than would be expected had they stayed on their projected growth curve over the school year. On average, Asian children decreased their BMI (though no child was considered underweight [BMI <5th percentile] at follow-up) and Latino children demonstrated an increase in BMI half of that typically expected in this age group (Figure 3). Furthermore, our results compare favorably to those seen in other interventions: the mean change in BMI over the school year for SCORES participants was 0.39 kg/m2 (95% CI 0.19, 0.59) and in a large trial among mostly white children of the same ages, the mean change in BMI over a school year was 0.29 kg/m2 in intervention subjects and 0.71 kg/m2 in controls (Robinson, 1999).
As in the large CATCH study (Webber et al., 1996), African-American children in SCORES experienced greater increases in BMI than did children of other ethnicities. The difference by race may represent lower levels of engagement among African-American children, who did have lower attendance rates and were more likely to drop out. Alternatively, the differential results may reflect a higher growth rate and more advanced pubertal stage (which was not assessed in this pilot study) among African-American children (Morrison et al., 1994).
The prevalence of obesity decreased from 33% to 27% among children in this study. While this decrease was not statistically significant, even small favorable changes in BMI with lifestyle interventions have been correlated with significant improvements in metabolic health (Kirk et al., 2005). Additionally, between 2001 and 2004, the prevalence of obesity among California children in grades five, seven, and nine increased by six percent (CCPHA, 2005). Given this secular trend, improvements among SCORES participants might be relatively greater when compared to their peers’ changes in prevalence of overweight. To interpret these results with any certainty, a control group will be necessary. Planning is underway for a controlled trial of SCORES to further evaluate its efficacy to prevent and address obesity in minority children. A controlled trial would also address whether the differences seen by race are due to different rates of growth at this age or to differential effects of the program.
Incomplete data are a limitation to the validity of these results. While SCORES was committed to undertaking an evaluation of their program, they were balancing the competing priorities of program delivery with data collection. They reported that coaches found it difficult to incorporate measures into busy and exciting game days (when most measures were scheduled in order to centralize the evaluation process). They also reported that a lack of coordination with schools (who scheduled field trips and special events on data collection days) hindered the evaluation. Finally, discipline issues leading to short-term suspension from SCORES for some children contributed to incomplete follow-up. However, there did not appear to be differential loss to follow-up as there were no differences in baseline measures (race, sex, BMI z-score and fitness) between children with and without follow-up data. Similarly, among children who remained in the program, attendance did not predict who would have complete data, suggesting that follow-up data were not systematically biased to include more frequent attendees. Thus, the greatest impact of lack of follow-up in this study is likely a decrease in power to see changes in BMI z-score.
A second limitation of this study is that participants in SCORES were recruited by coaches and elected to enroll. Children who wouldn’t volunteer for SCORES might not benefit equally from the program. Nonetheless, overweight children – a crucial group to reach – were both willing to enroll and showed the greatest decrease in BMI z-score. Additionally, because SCORES provides free after-school care and has a focus on building literacy, some children were likely to enroll due to parental interest in these aspects of the program, not solely because of the child’s interest in soccer.
Recent evidence-based guidelines for physical activity in school-age youth recommend a minimum of 60 minutes of daily moderate-to-vigorous physical activity that is both developmentally appropriate and enjoyable (Strong et al., 2005). Community-based after-school programs may provide realistic venues in which to achieve these goals in children of all ethnicities, and thus help to narrow health disparities. Programs such as America SCORES that have developed a national curriculum and expanded to multiple sites, have proven their portability – a barrier new interventions will face once they’re proven effective. SCORES has the potential to serve as a model for after-school programs focused on improving fitness and reducing BMI, but further evaluation will be required to confirm and further interpret these initial results.
Contributor Information
KRISTINE A. MADSEN, UCSF, Department of Pediatrics, San Francisco, CA.
HANNAH R. THOMPSON, UCSF, Department of Pediatrics, San Francisco, CA.
LIDYA WLASIUK, UCSF, Department of Pediatrics, San Francisco, CA.
EMILY QUELIZA, America SCORES Bay Area, San Francisco, CA.
COLIN SCHMIDT, America SCORES Bay Area, San Francisco, CA.
THOMAS B. NEWMAN, UCSF, Departments of Pediatrics and Epidemiology and Biostatistics, San Francisco, CA.
References
- Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, Anderssen SA. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study) Lancet. 2006;368:299–304. doi: 10.1016/S0140-6736(06)69075-2. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice Hall; 1986. [Google Scholar]
- Barbeau P, Johnson MH, Howe CA, Allison J, Davis CL, Gutin B, Lemmon CR. Ten months of exercise improves general and visceral adiposity, bone, and fitness in black girls. Obesity. 2007;15:2077–85. doi: 10.1038/oby.2007.247. [DOI] [PubMed] [Google Scholar]
- Barroso CS, Mccullum-Gomez C, Hoelscher DM, Kelder SH, Murray NG. Self-reported barriers to quality physical education by physical education specialists in Texas. J Sch Health. 2005;75:313–9. doi: 10.1111/j.1746-1561.2005.00042.x. [DOI] [PubMed] [Google Scholar]
- Blair SN, Brodney S. Effects of physical inactivity and obesity on morbidity and mortality: current evidence and research issues. Med Sci Sports Exerc. 1999;31:S646–62. doi: 10.1097/00005768-199911001-00025. [DOI] [PubMed] [Google Scholar]
- Bloomgarden ZT. Type 2 diabetes in the young: the evolving epidemic. Diabetes Care. 2004;27:998–1010. doi: 10.2337/diacare.27.4.998. [DOI] [PubMed] [Google Scholar]
- Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, Froberg K. Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: the European Youth Heart Study (EYHS) Diabetes Care. 2004;27:2141–8. doi: 10.2337/diacare.27.9.2141. [DOI] [PubMed] [Google Scholar]
- Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, Norman J, Story M, Stone EJ, Stephenson L, Stevens J. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. 2003;78:1030–8. doi: 10.1093/ajcn/78.5.1030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CCPHA. California Center for Public Health Advocacy (CCPHA). The Growing Epidemic: Child Overweight Rates On The Rise In California Assembly Districts 2005 [Google Scholar]
- Chien A, Coker T, Choi L, Slora E, Bodnar P, Weiley V, Wasserman R, Johnson J. What do pediatric primary care providers think are important research questions? A perspective from PROS providers. Ambul Pediatr. 2006;6:352–5. doi: 10.1016/j.ambp.2006.07.002. [DOI] [PubMed] [Google Scholar]
- Cook S, Weitzman M, Auinger P, Nguyen M, Dietz WH. Prevalence of a metabolic syndrome phenotype in adolescents: findings from the third National Health and Nutrition Examination Survey, 1988-1994. Arch Pediatr Adolesc Med. 2003;157:821–7. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- Davis SP, Northington L, Kolar K. Cultural considerations for treatment of childhood obesity. J Cult Divers. 2000;7:128–32. [PubMed] [Google Scholar]
- Duncan GE, Li SM, Zhou XH. Prevalence and trends of a metabolic syndrome phenotype among u.s. Adolescents, 1999-2000. Diabetes Care. 2004;27:2438–43. doi: 10.2337/diacare.27.10.2438. [DOI] [PubMed] [Google Scholar]
- Dynarski M, Moore M, Mullens J, Gleason P, James-Burdumy S, Rosenberg L, Masnfield W, Heaviside S, Levy D, Pistorino C, Silva T, Deke J. When Schools Stay Open Late: The National Evaluation of the 21st-Century Community Learning Centers Program. First Year Findings. U.S. Dept of Ed; 2003. [Google Scholar]
- Farrell SW, Braun L, Barlow CE, Cheng YJ, Blair SN. The relation of body mass index, cardiorespiratory fitness, and all-cause mortality in women. Obes Res. 2002;10:417–23. doi: 10.1038/oby.2002.58. [DOI] [PubMed] [Google Scholar]
- Gortmaker SL, Peterson K, Wiecha J, Sobol AM, Dixit S, Fox MK, Laird N. Reducing obesity via a school-based interdisciplinary intervention among youth: Planet Health. Arch Pediatr Adolesc Med. 1999;153:409–18. doi: 10.1001/archpedi.153.4.409. [DOI] [PubMed] [Google Scholar]
- Gutin B, Yin Z, Johnson M, Barbeau P. Preliminary findings of the effect of a 3-year after-school physical activity intervention on fitness and body fat: the Medical College of Georgia Fitkid Project. Int J Pediatr Obes. 2008;3(Suppl 1):3–9. doi: 10.1080/17477160801896457. [DOI] [PubMed] [Google Scholar]
- Harrell JS, Gansky SA, Mcmurray RG, Bangdiwala SI, Frauman AC, Bradley CB. School-based interventions improve heart health in children with multiple cardiovascular disease risk factors. Pediatrics. 1998;102:371–80. doi: 10.1542/peds.102.2.371. [DOI] [PubMed] [Google Scholar]
- Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999-2002. JAMA. 2004;291:2847–50. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- Hofferth SL, Jankuniene Z. Life after school: data from the 1997 Child Development Supplement. Educational Leadership. 2001;58:19–23. [Google Scholar]
- Jago R, Jonker ML, Missaghian M, Baranowski T. Effect of 4 weeks of Pilates on the body composition of young girls. Prev Med. 2006;42:177–80. doi: 10.1016/j.ypmed.2005.11.010. [DOI] [PubMed] [Google Scholar]
- Jolliffe D. Extent of overweight among US children and adolescents from 1971 to 2000. Int J Obes Relat Metab Disord. 2004;28:4–9. doi: 10.1038/sj.ijo.0802421. [DOI] [PubMed] [Google Scholar]
- Kirk S, Zeller M, Claytor R, Santangelo M, Khoury PR, Daniels SR. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res. 2005;13:876–82. doi: 10.1038/oby.2005.101. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, Mei Z, Curtin LR, Roche AF, Johnson CL. CDC growth charts: United States. Adv Data. 2000:1–27. [PubMed] [Google Scholar]
- Leger LA, Mercier D, Gadoury C, Lambert J. The multistage 20 metre shuttle run test for aerobic fitness. J Sports Sci. 1988;6:93–101. doi: 10.1080/02640418808729800. [DOI] [PubMed] [Google Scholar]
- Liu NY, Plowman SA, Looney MA. The reliability and validity of the 20-meter shuttle test in American students 12 to 15 years old. Res Q Exerc Sport. 1992;63:360–5. doi: 10.1080/02701367.1992.10608757. [DOI] [PubMed] [Google Scholar]
- Madsen KA, Yen S, Wlasiuk L, Newman TB, Lustig R. Feasibility of a dance videogame to promote weight loss among overweight children and adolescents. Arch Pediatr Adolesc Med. 2007;161:105–7. doi: 10.1001/archpedi.161.1.105-c. [DOI] [PubMed] [Google Scholar]
- Mccallum Z, Wake M, Gerner B, Baur LA, Gibbons K, Gold L, Gunn J, Harris C, Naughton G, Riess C, Sanci L, Sheehan J, Ukoumunne OC, Waters E. Outcome data from the LEAP (Live, Eat and Play) trial: a randomized controlled trial of a primary care intervention for childhood overweight/mild obesity. Int J Obes (Lond) 2006 doi: 10.1038/sj.ijo.0803509. [DOI] [PubMed] [Google Scholar]
- Melnyk BM, Small L, Morrison-Beedy D, Strasser A, Spath L, Kreipe R, Crean H, Jacobson D, Kelly S, O’haver J. The COPE Healthy Lifestyles TEEN program: feasibility, preliminary efficacy, & lessons learned from an after school group intervention with overweight adolescents. J Pediatr Health Care. 2007;21:315–22. doi: 10.1016/j.pedhc.2007.02.009. [DOI] [PubMed] [Google Scholar]
- Morrison JA, Barton B, Biro FM, Sprecher DL, Falkner F, Obarzanek E. Sexual maturation and obesity in 9- and 10-year-old black and white girls: the National Heart, Lung, and Blood Institute Growth and Health Study. J Pediatr. 1994;124:889–95. doi: 10.1016/s0022-3476(05)83176-2. [DOI] [PubMed] [Google Scholar]
- Muntner P, He J, Cutler JA, Wildman RP, Whelton PK. Trends in blood pressure among children and adolescents. JAMA. 2004;291:2107–13. doi: 10.1001/jama.291.17.2107. [DOI] [PubMed] [Google Scholar]
- National Center for Health Statistics. CDC growth charts for the United States: Methods and Development. [August 16 2004];2002 http://www.cdc.gov/growthcharts/ [PubMed]
- NSCH. National Survey of Children’s Health, Data Resource Center on Child and Adolescent Health; 2005. [August 5 2005]. Child and Adolescent Health Measurement Initiative. www.nschdata.org. [Google Scholar]
- Patrick K, Calfas KJ, Norman GJ, Zabinski MF, Sallis JF, Rupp J, Covin J, Cella J. Randomized controlled trial of a primary care and home-based intervention for physical activity and nutrition behaviors: PACE+ for adolescents. Arch Pediatr Adolesc Med. 2006;160:128–36. doi: 10.1001/archpedi.160.2.128. [DOI] [PubMed] [Google Scholar]
- Rao G. Pediatric obesity-related counseling in the outpatient setting. Ambul Pediatr. 2005;5:377–9. doi: 10.1367/A05-040R.1. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Cohn L, Reinhardt J, Cross D, Futterman R, Kirschner E, Wynder EL, Allegrante JP. A three-year evaluation of the know your body program in inner-city schoolchildren. Health Educ Q. 1992;19:463–80. doi: 10.1177/109019819201900410. [DOI] [PubMed] [Google Scholar]
- Robinson TN. Reducing children’s television viewing to prevent obesity: a randomized controlled trial. JAMA. 1999;282:1561–7. doi: 10.1001/jama.282.16.1561. [DOI] [PubMed] [Google Scholar]
- Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, Pruitt LA, Powell TM, Owens AS, Thompson NS, Flint-Moore NM, Davis GJ, Emig KA, Brown RT, Rochon J, Green S, Varady A. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis. 2003;13:S65–77. [PubMed] [Google Scholar]
- Saelens BE, Sallis JF, Wilfley DE, Patrick K, Cella JA, Buchta R. Behavioral weight control for overweight adolescents initiated in primary care. Obes Res. 2002;10:22–32. doi: 10.1038/oby.2002.4. [DOI] [PubMed] [Google Scholar]
- Sahota P, Rudolf MC, Dixey R, Hill AJ, Barth JH, Cade J. Randomised controlled trial of primary school based intervention to reduce risk factors for obesity. BMJ. 2001;323:1029–32. doi: 10.1136/bmj.323.7320.1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger D, Barton LR, Karter AJ, Wang F, Adler N. Does literacy mediate the relationship between education and health outcomes? A study of a low-income population with diabetes. Public Health Rep. 2006;121:245–54. doi: 10.1177/003335490612100305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorof JM, Lai D, Turner J, Poffenbarger T, Portman RJ. Overweight, ethnicity, and the prevalence of hypertension in school-aged children. Pediatrics. 2004;113:475–82. doi: 10.1542/peds.113.3.475. [DOI] [PubMed] [Google Scholar]
- Spiegel SA, Foulk D. Reducing overweight through a multidisciplinary school-based intervention. Obesity. 2006;14:88–96. doi: 10.1038/oby.2006.11. [DOI] [PubMed] [Google Scholar]
- Strong WB, Malina RM, Blimkie CJ, Daniels SR, Dishman RK, Gutin B, Hergenroeder AC, Must A, Nixon PA, Pivarnik JM, Rowland T, Trost S, Trudeau F. Evidence based physical activity for school-age youth. J Pediatr. 2005;146:732–7. doi: 10.1016/j.jpeds.2005.01.055. [DOI] [PubMed] [Google Scholar]
- Webber LS, Osganian SK, Feldman HA, Wu M, Mckenzie TL, Nichaman M, Lytle LA, Edmundson E, Cutler J, Nader PR, Luepker RV. Cardiovascular risk factors among children after a 2 1/2-year intervention-The CATCH Study. Prev Med. 1996;25:432–41. doi: 10.1006/pmed.1996.0075. [DOI] [PubMed] [Google Scholar]
- Weisman SA, Gottfredson DC. Attrition from after school programs: Characteristics of students who drop out. Prevention Science. 2001;2:201–205. doi: 10.1023/a:1011515024809. [DOI] [PubMed] [Google Scholar]
- Yin Z, Moore JB, Johnson MH, Barbeau P, Cavnar M, Thornburg J, Gutin B. The Medical College of Georgia Fitkid project: the relations between program attendance and changes in outcomes in year 1. Int J Obes (Lond) 2005;29(Suppl 2):S40–5. doi: 10.1038/sj.ijo.0803061. [DOI] [PubMed] [Google Scholar]
- YRBSS. National Center for Chronic Disease Prevention and Health Promotion; 2004. [November 1 2005]. YRBSS Youth Online: Comprehensive Results. http://apps.nccd.cdc.gov/yrbss/CategoryQuestions.asp?Cat=6&desc=Physical%20Activity. [Google Scholar]


