Abstract
Objectives
Stroke mortality rates are reported to be lower for Hispanics than non-Hispanic Whites. We investigate the degree to which this lower reported mortality is explained by inaccuracies introduced through omission of nativity, imprecise measurement of cause of death, and under-ascertainment of Hispanic ethnicity on death certificates. We used national vital registration data for the years 1989–1991 and 1999–2002, including foreign- and US-born Hispanics and non-Hispanic Whites. Hispanic deaths were adjusted for misclassification of ethnicity on the death certificate. Denominators for the rates were derived from census estimates.
Results
Adjustment for nativity and death certificate misclassification removes the stroke mortality advantage for US-born Hispanic men, but not women. After adjustment, US-born Hispanic men and women have higher rates of mortality from subarachnoid hemorrhage than non-Hispanic Whites (RR: 1.23 and 1.23, respectively), but lower rates of mortality from Ischemic (RR: 0.76 and 0.73, respectively) and chronic effects of stroke (RR: 0.87 and 0.73, respectively).
Conclusions
When adjusted for misclassification the lower stroke mortality remains for Hispanic men and women at older ages. Part of the previously reported advantage is a combination of imprecise measurement and data quality.
Keywords: disparity, mortality, stroke
Despite declines in stroke mortality over the previous decades, it remained the third leading cause of death.1–4 Studies have shown significant differences in mortality among different racial/ethnic groups. Hispanics have lower rates of stroke mortality, particularly at older ages than non-Hispanic whites.1,5,6 Heterogeneity exists in the Hispanic population by country of origin, birthplace, education, and income. According to the US census, on average Hispanics possess lower levels of education, have lower paying jobs, and are more likely to live in poverty than non-Hispanic Whites.7 Thus, on average, Hispanics occupy a lower socioeconomic position than non-Hispanic whites. Lower socioeconomic position is associated with increased mortality from stroke.8–10 Given the lower socioeconomic position of Hispanics relative to non-Hispanic whites, it is surprising that Hispanics have lower rates of mortality from stroke compared with non-Hispanic whites. It has been suggested that the Hispanic mortality advantage is the result of confounding factors and thus not entirely accurate.11 The current study presents an examination of potential methodological explanations for the findings of lower stroke mortality in Hispanics.
One potential contributor to lower Hispanic stroke morality is nativity. It has been observed in all race/ethnic groups that the foreign born have markedly lower rates of all cause mortality than those born in this country.12 Foreign-born Hispanics have been shown to have significantly lower mortality rates due to circulatory causes (including stroke) than their US-born counter parts and non-Hispanic Whites.13,14 Nearly 40% of Hispanics in the United States are foreign born.15 Thus, the lower stroke mortality in Hispanics in the United States may be attributable to this “Healthy Migrant” effect.
Two additional methodological factors that may contribute to lower Hispanic stroke mortality involve data quality. The first of these is accuracy of cause of death coding on the death certificate. The International Classification of Diseases, version 9 (ICD-9) and version 10 (ICD-10), may be too vague, leading to variability in diagnostic assessment.16 The resulting diagnostic ambiguity may result in greater accuracy in diagnosis for death from an acute event (hemorrhagic or ischemic) relative to diagnosis of more chronic effects of stroke (unspecified, other cerebrovascular disease and sequelae of stroke). Such generalization of cause of death may understate mortality from specific subtypes of stroke by lumping deaths into the general category. Additionally, place of death may influence the reporting of underlying cause of death. It has been shown that out of hospital stroke deaths are primarily due to the chronic effects of stroke rather than a specific acute subtype.17,18 The association of these unobserved deaths with ambiguous diagnoses suggests that deaths that occur outside of a care facility may not be accurately classified.
Misreport of Hispanic ethnicity is the second data quality issue which can influence mortality rates. Ethnicity on death certificates is usually assigned by the funeral director, which can introduce error.19 Hispanics can be misidentified as non-Hispanics on death certificates leading to a biased mortality rate calculation.20–22 Mortality rates are calculated by dividing the number of deaths for a given race/ethnicity by the census estimate of the number of people alive at the middle of the year in question. If Hispanics are under-reported on the death certificate, the corresponding mortality rate would be artificially suppressed.
The 1980 Census was the first time that identification of Hispanic origin was used in the decennial census. Additionally, it was not until the late 1970s that a similar question appeared on death certificates. Initial analysis used the national longitudinal mortality study to assess accuracy of Hispanic ethnicity on death certificates.23 Examining a period from 1979 to 1985, Hispanic origin was found to be accurately coded on the death certificate in 89.7% of cases. Additionally, studies examining the report of country of origin on death certificates is highly concordant with that reported by self-report in the census.21,24,25 These studies have found 98.0% to 99.2% agreement between census and death certificate report of nativity.
Subsequent to this early research, Arias et al also assessed the impact of under reporting of Hispanic ethnicity on death certificates by linking the National Longitudinal Mortality Study (NLMS) to the Current Population Survey (CPS) which is linked to death certificates. In this way they were able to compare self-report of Hispanic ethnicity in the NLMS to death certificate classification. They found that foreign-born Hispanics were very rarely misclassified (~2%), but US-born Hispanics were estimated to be misclassified in 7% of cases.24,26
We examine national vital statistic data combined with census estimates to calculate age-adjusted stroke mortality rates for foreign- and US-born Hispanics, correcting for misreport of ethnicity on death certificate using the percentages reported by Arias et al. These rates are then compared with those for non-Hispanic whites. These rates are examined by subtype of stroke, focusing on deaths from acute stroke versus deaths from chronic effects of stroke. We hypothesized that, after correction for under-ascertainment of Hispanic ethnicity, US-born Hispanics would not have lower rates of stroke mortality than non-Hispanic whites from acute stroke. We also expected that dying outside of a care facility would alter the likelihood of acute cause of death classification for Hispanics.
METHODS
Multiple cause-of-death mortality data from the National Vital Statistics System of the National Center for Health Statistics were used for deaths occurring within the United States for the years 1989–1991 and 1999–2002. International Classification of Diseases versions 9 and 10 (ICD-9 and ICD-10) were used for 1989–1991 and 1999–2002, respectively, due to coding changes on death certificates. Our primary analyses examined only underlying cause of death. However, we performed a secondary analysis to examine the impact of reporting stroke mortality and death with stroke listed as the underlying cause or a contributing cause. All records were grouped into 2 general categories: acute and chronic. The acute category was further broken into subtypes: subarachnoid hemorrhage (ICD-9 codes 430, ICD-10 codes I60), intracerebral/intracranial hemorrhage (ICD-9 code 432, ICD-10 codes I61–I62), and acute ischemic stroke (ICD-9 codes 433–434, ICD-10 code I63). The chronic category consisted of stroke—other and ill-defined cerebrovascular disease (ICD-9 code 437, ICD-10 code I64), and late effects of cerebrovascular disease (ICD-9 code 438, ICD-10 code I69). Transient ischemic attack (ICD-9 code 435, ICD-10 code G45) was not included in these analyses. The data were pooled to generate numerators by 5-year age group, gender, race/ethnicity, and nativity for the time period around 1990 (n = 432,722) and 2000 (n = 662,121). Race/Ethnicity was defined as non-Hispanic white, foreign-born Hispanic, and US-born Hispanic. Hispanic race/ethnicity was defined as having Hispanic ethnicity regardless of race category. Missing data on death certificates for age (<0.01%), Hispanic origin (~1.9%), and place of birth (~0.6%) were imputed using the hot-deck procedure in STATA version 9. The numerators were aggregated into 4 groups: foreign-born Hispanics, US-born Hispanics, foreign-born non-Hispanic whites, and US-born non-Hispanic whites. Using the factors reported by Arias et al,26 the numerators for the foreign- and US-born Hispanics were then directly corrected for death certificate undercount by multiplying the number of deaths by 1.02 and 1.07 respectively. Additionally, we subtract 7% of the number of corrected Hispanic deaths (at each age group and sex) from the number of deaths reported for US-born non-Hispanic whites. Similarly, we subtract 2% of reported foreign-born Hispanic deaths from those reported for foreign-born non-Hispanic whites.
The denominators were compiled from the Integrated Public Use Microdata Series (IPUMS) 5% Census samples for 1990 and 2000 combined with bridged-race population estimates from the National Center for Health Statistics (NCHS) for the years 1989–1991 and 1999–2002. The IPUMS data were used to develop a ratio for the percent foreign/US born in a given gender, ethnicity, and age group. This ratio was then used as a multiplier with the census estimates to create denominators for both the foreign- and US-born Hispanics for each gender, ethnicity, and age group.
The numerators and denominators for the years 1989–1991 and 1999–2002 were pooled to yield more robust estimates for each stroke subtype. The resulting crude stroke mortality rates were age adjusted using the direct method with the year 2000 US standard million population, and 95% confidence intervals were calculated.27 To estimate the overall excess stroke mortality among foreign- and US-born Hispanics, rate ratios were calculated for foreign- and US-born Hispanics, using foreign- and US-born non-Hispanic whites as the referent group (respectively). A contingency table was constructed by multiplying the rate for non-Hispanic whites by the US-born Hispanic population resulting in an expected number of deaths for Hispanics. A log linear analysis of contingency tables was performed.28 The expected deaths and observed deaths were stratified by sex. Covariates in the model were age group and acute stroke compared with other underlying cause. Death outside of a care facility was then added and differences in coefficient for acute stroke were compared with determine the impact of dying outside of an institution on acute diagnosis.
RESULTS
Table 1 shows the effect of nativity and ethnicity misclassification on age-adjusted stroke mortality rates for Hispanics and non-Hispanic whites. Data for both 1990 and 2000 are presented. Adjustment for misreport of Hispanic ethnicity on death certificates resulted in a small increase in the mortality rate for foreign-born Hispanics. Adjustment for over-count among non-Hispanic whites also resulted in very small changes in mortality rates. For US-born Hispanics, adjusting for ethnicity misclassification resulted in an increase of greater magnitude than for the foreign born. Although the gap between Hispanics and non-Hispanic white rates narrowed, both foreign- and US-born Hispanic men and women still had substantially lower mortality rates. The rate for US-born Hispanic women was 25% lower than those for US-born non-Hispanic white women, while the rate for foreign-born Hispanic women was 35% lower than those for foreign-born non-Hispanic white women. The rates for US-born Hispanic men was 9% lower than those for US-born non-Hispanic white men. Foreign-born Hispanic men had a rate 24% lower than that for foreign-born non-Hispanic whites.
TABLE 1.
Age-Adjusted* and Corrected† Stroke Mortality Rates Comparing Hispanics to Non-Hispanic Whites by Sex and Nativity, United States, 1989–1991 and 1999–2002 (Stroke as Underlying Cause)
| Rate (95% CI) | Rate-Corrected (95% CI) | |
|---|---|---|
| Men | ||
| 1990 | ||
| Foreign born | ||
| Hispanic | 44.12 (42.60–45.63) | 45.00 (43.47–46.53) |
| Non-Hispanic white | 62.61 (61.44–63.77) | 62.16 (60.99–63.32) |
| US born | ||
| Hispanic | 49.74 (47.84–51.65) | 53.22 (51.25–55.19) |
| Non-Hispanic white | 60.92 (60.59–61.25) | 60.84 (60.51–61.18) |
| 2000 | ||
| Foreign born | ||
| Hispanic | 42.00 (41.00–43.01) | 42.84 (41.83–43.86) |
| Non-Hispanic white | 56.80 (55.79–57.81) | 56.14 (55.14–57.15) |
| US born | ||
| Hispanic | 47.06 (45.76–48.35) | 50.35 (49.01–51.69) |
| Non-Hispanic white | 55.21 (54.96–55.45) | 55.11 (54.86–55.36) |
| Women | ||
| 1990 | ||
| Foreign born | ||
| Hispanic | 40.68 (39.42–41.94) | 41.50 (40.22–42.77) |
| Non-Hispanic white | 61.62 (60.77–62.47) | 61.26 (60.42–62.11) |
| US born | ||
| Hispanic | 43.84 (42.21–45.46) | 46.90 (45.22–48.59) |
| Non-Hispanic white | 60.45 (60.18–60.71) | 60.38 (60.12–60.65) |
| 2000 | ||
| Foreign born | ||
| Hispanic | 37.89 (37.05–38.72) | 38.65 (37.80–39.49) |
| Non-Hispanic white | 58.51 (57.74–59.28) | 57.99 (57.23–58.76) |
| US born | ||
| Hispanic | 41.64 (40.54–42.74) | 44.56 (43.42–45.69) |
| Non-Hispanic white | 58.17 (57.97–58.37) | 58.09 (57.89–58.29) |
Age adjusted using the 2000 US standard million.
Numerators adjusted for under-report of Hispanic ethnicity on death certificates and over-report of non-Hispanic white ethnicity.
Table 2 presents age adjusted stroke mortality rate ratios (non-Hispanic whites as reference group) by sex and stroke subtype adjusting for nativity and misreport of ethnicity on death certificates. For intracranial hemorrhage, ischemic stroke, and chronic effects of stroke, foreign-born Hispanics had lower rates than foreign-born non-Hispanic whites. However, foreign-born Hispanic men and women had higher rates of subarachnoid hemorrhage than non-Hispanic whites and US-born Hispanics. A similar pattern emerges in the case of US-born Hispanics compared with non-Hispanic whites. Rates for ischemic stroke and chronic effects of stroke are lower for US-born Hispanic men and women than US-born non-Hispanic whites. In US-born Hispanic men the rates are lower only for ischemic stroke and ill-defined stroke. Rates for subarachnoid hemorrhage are much higher for US-born Hispanic men and women than for non-Hispanic whites.
TABLE 2.
Age-Adjusted Stroke Mortality Rate Ratios Corrected for Misidentification of Ethnicity on Death Certificates Comparing Hispanics to non-Hispanic Whites by Sex, Nativity, and Stroke Subtype, United States, 1999–2002
| Men |
Women |
|||
|---|---|---|---|---|
| Foreign Born | US Born | Foreign Born | US Born | |
| All strokes | 0.76 | 0.91 | 0.67 | 0.77 |
| Acute stroke | 0.83 | 1.01 | 0.78 | 0.94 |
| Subarachnoid hemorrhage | 1.03 | 1.23 | 1.11 | 1.23 |
| Intracranial hemorrhage | 0.87 | 1.11 | 0.82 | 0.97 |
| Ischemic | 0.65 | 0.76 | 0.54 | 0.73 |
| Chronic effects | 0.73 | 0.87 | 0.62 | 0.70 |
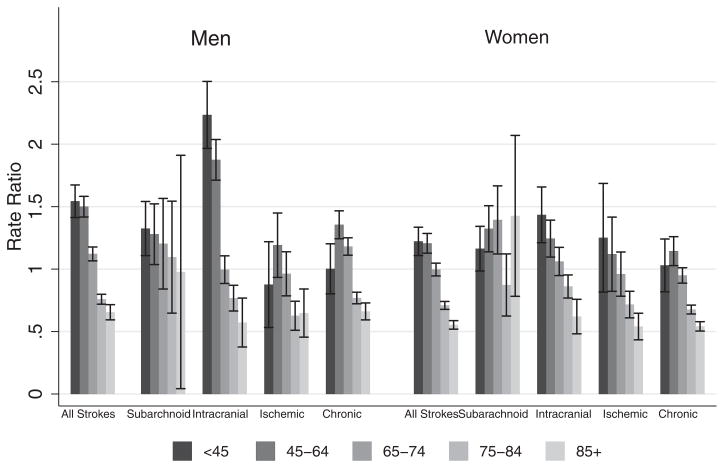
Figure 1 shows US-born stroke mortality by sex, age group, and stroke subtype adjusting for ethnicity misreport on death certificates. This figure compares US-born non-Hispanic white and US-born Hispanic rates for 5 age groupings: those 45 and younger, 45 to 64, 65–74, 75–84, and 85 and older. This comparison reveals higher rates of stroke mortality in US-born Hispanic men and women at younger ages for most subtypes of stroke. These comparisons also show a mortality cross over which occurs around the age of 75 for US-born Hispanics for most subtypes of stroke. The exception to this cross over is in the rate of subarachnoid hemorrhage for US-born Hispanic men and women. Since most strokes occur in individuals 75 years old and older, the overall ratio is lower.
FIGURE 1.
US-born Hispanic stroke mortality rate ratios and 95% confidence intervals (US-born non-Hispanic whites as referent) by sex, stroke subtype, and age group, United States, 1999–2002.
Examination of place of death revealed that 87% of both US-born Hispanics and non-Hispanic whites died in an institution. About 71% of US-born Hispanic men died in a hospital compared 17% who died in a nursing facility. For non-Hispanic white men, 60% died in a hospital versus 28% in a nursing facility. About 66% of US-born Hispanic women died in a hospital compared with 21% who died in a nursing facility. For non-Hispanic white women, 48% died in a hospital while 40% died in a nursing facility. Log linear analysis of contingency tables comparing US-born non-Hispanic whites to US-born Hispanics showed little change in the coefficient for acute stroke as underlying cause of death (β = −4.16, 95% CI: −4.19, −3.79) after accounting for place of death outside of an institution (β = −3.99, 95% CI: −4.23, −3.75).
The main analyses examined mortality based on report of underlying cause of death. We also performed similar analyses where stroke mortality was identified as any case where stroke was listed as an underlying or contributing cause. This resulted in an approximate 75% and 80% increase in stroke mortality rates for US-born Hispanic women and men, respectively. The rates for US-born non-Hispanic white women and men increased 62% and 75%, respectively. However, the ratio of Hispanic to non-Hispanic whites changed little. For example, in 2000 the ratio for US-born Hispanic men compared with US-born non-Hispanic men was 0.91, using underlying cause of death. The same ratio calculated using underlying and any contributing cause was 0.94. For US-born Hispanic women the ratio for underlying cause was 0.77, whereas the ratio for underlying and contributing causes combined was 0.83.
DISCUSSION
This study explored the degree to which the relatively lower stroke mortality of Hispanics compared with non-Hispanic Whites is explained by inaccuracies introduced through omission of nativity, imprecise measurement of cause of death and under-ascertainment of Hispanic ethnicity. These factors were examined by adjusting mortality rates for both misclassification of Hispanic ethnicity on death certificates (and consequent over-count of non-Hispanic whites) and foreign versus US place of birth. Imprecision was examined through the calculation of rates for subtypes of stroke and comparison of place of death.
The over-all rate of stroke mortality for Hispanic women remained lower than that for non-Hispanic White women after adjustment for nativity and misreport of Hispanic ethnicity. The lower stroke mortality for US-born Hispanic men narrows after adjustment for nativity and misreport. Examination of death from subtype of stroke reveals a different pattern. Hispanic men and women have a higher rate of mortality from subarachnoid hemorrhage than do non-Hispanic Whites. In contrast, Hispanic men and women have lower mortality rates from ischemic and chronic effects of stroke than do non-Hispanic whites. Hispanics have greater odds of dying outside of an institution than non-Hispanic whites. Additionally, when the place of death is not an institution, the odds are more than 3 times higher for an underlying cause of death diagnosis to be chronic effects of stroke as opposed to acute stroke.
The clear mortality advantage for the foreign-born Hispanics supports the notion of a Healthy Immigrant effect within the Hispanic population. This relative health advantage of the foreign born suggests that immigrants are selected to be healthier than the native born.
The majority of stroke deaths occurred in the chronic effects of stroke category. This has been noted previously by the CDC.17,18 Such a lack of specificity draws into question the accuracy of rates for subtypes. Almost all of the stroke mortality advantage for Hispanics lay in the chronic category: other and ill-defined stroke and late effects of stroke. These chronic effects leave a great deal of room for interpretation and correspondingly misinterpretation, and thus more prone to erroneous report. In contrast, diagnosis of more acute events is likely more accurate.
The association of place of death and acute versus chronic stratum was anticipated, as patients who die in an institution are more likely to receive a more accurate underlying cause of death diagnosis than those who die elsewhere. As such, rates derived from death in hospital are assumed to be more accurate. Out of hospital deaths, in contrast, receive more vague diagnoses which in turn lead to more questionable mortality rates. This study found higher rates of out of health care facility mortality for Hispanics compared with non-Hispanic whites which is consistent with other research.29 However, adjusting for death outside of a health care facility resulted in no changes in the coefficients for acute stroke as underlying cause of death.
When acute subtypes of stroke are examined, Hispanics are more likely to die of subarachnoid hemorrhage than non-Hispanic Whites. Additionally, Hispanics are less likely to die of ischemic stroke. These findings are consistent with other studies.2,3 This difference in mortality is indicative of differences in the etiology of the underlying disease process for Hispanics and non-Hispanics whites. Although the prevalence of hypertension appear to be slightly lower in Hispanics compared with non-Hispanic whites (25% and 27%, respectively), Hispanics are less likely than whites to be aware of their condition and significantly less likely to be under treatment or to have their condition under control.30. It may be the lack of treatment and control of hypertension that contributes to their higher risk for this type of stroke.
Although the overall stroke mortality rate for US-born Hispanic men after adjustment moves closer to the rate for non-Hispanic white men, this rate is still lower than might be expected given their socioeconomic status. This advantage has been previously observed and called the Hispanic Paradox.31 Several studies have suggested that this paradox is due either to ethnicity misclassification (and thus miscounting) of Hispanics or the contribution of healthy immigrants.11,32,33 The current study supports the supposition that these factors explain part, but not all, of the stroke mortality advantage for Hispanics in the United States.
These analyses also highlight the excess burden of stroke mortality among Hispanics at younger ages. The alarmingly high rates of Intracranial stroke mortality among US-born Hispanic men under the age of 65, more than twice those of US-born non-Hispanic men, suggests the need for interventions in this younger age group.
There are several limitations to this study. One limitation is the misreporting of age on death certificates, especially at older ages. Misstatement of age biases mortality estimates downward. Studies have found this to be true for non-Hispanic Blacks and non-Hispanic Whites.34–37 The extent to which this is an issue with Hispanics is not as well established. In this study, however, we pooled data for ages greater than 85 years which should minimize any biases.
Another potential limitation of this study could be the misreport of underlying cause of death. As previously discussed, the internal vagaries introduced are problematic at the level of stroke subtype mortality estimation. However, these data cannot tell us the extent to which stroke attributable deaths are completely misclassified as another underlying cause. We did find that those who die in institutions as opposed to outside of institutions have more accurate underlying cause of death diagnoses.
Due to the limitations imposed by the misreport of race/ethnicity in vital registration data, researchers have examined data from large, nationally representative survey samples, such as the National Health Interview Survey (NHIS) and the National Mortality Follow-up Survey (NLMS), and then link them to the National Death Index (NDI).5,11,14,38–40 The chief advantage of this approach is that race/ethnicity is self-reported, and thus not susceptible to the biases of a third party. However, these studies are limited in several ways. The nature of these samples results in small numbers when examining cause-specific mortality along with sex, race/ethnicity, and nativity, resulting in broad confidence intervals for rate estimates. Additionally, these studies rely on linkage to the NDI, a linkage that has been questioned in regards to Hispanic immigrants.32 The NDI has no facility to track return migrants whose death outside the United States would lead to understated mortality rates. In contrast to these studies, we examined death certificate data and correct for misreport of Hispanic ethnicity.
Misreport of Hispanic ethnicity on death certificates contributes to the perceived Hispanic stroke mortality advantage, more so for US-born Hispanics than for the foreign born. When adjusted for misclassification the lower stroke mortality for Hispanic men and women persists only at older ages. Additionally, Hispanic men and women have higher rates of mortality attributed to subarachnoid and intracranial hemorrhage than do non-Hispanic whites under the age of 65. Part of the previously reported advantage is a combination of imprecise measurement and data quality. However, after accounting for these factors, an advantage still remains for Hispanic men and women at older ages.
Acknowledgments
This work was funded by T32 AG00270, Health of Older Minorities, University of Texas Medical Branch.
References
- 1.Ayala C, Greenlund KJ, Croft JB, et al. Racial/ethnic disparities in mortality by stroke subtype in the United States, 1995–1998. Am J Epidemiol. 2001;154:1057–1063. doi: 10.1093/aje/154.11.1057. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control Prevention. Age-specific excess deaths associated with stroke among racial/ethnic minority populations—-United States, 1997. MMWR Morb Mortal Wkly Rep. 2000;49:94–97. [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. Disparities in deaths from stroke among persons aged <75 years—-United States, 2002. MMWR Morb Mortal Wkly Rep. 2005;54:477–481. [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. The atlas of stroke mortality: racial, ethnic and geographic disparities in the United States. Atlanta, GA: Centers for Disease Control and Prevention; 2006. [Google Scholar]
- 5.Howard G, Anderson R, Sorlie P, et al. Ethnic differences in stroke mortality between non-Hispanic whites, Hispanic whites, and blacks. The National Longitudinal Mortality Study. Stroke. 1994;25:2120–2125. doi: 10.1161/01.str.25.11.2120. [DOI] [PubMed] [Google Scholar]
- 6.Karter AJ, Gazzaniga JM, Cohen RD, et al. Ischemic heart disease and stroke mortality in African-American, Hispanic, and non-Hispanic white men and women, 1985 to 1991. West J Med. 1998;169:139–145. [PMC free article] [PubMed] [Google Scholar]
- 7.Ramirez RR, Cruz GPdl. Current population reports. Washington DC: US Census Bureau; 2002. The Hispanic Population in the United States: March 2002. [Google Scholar]
- 8.Banks J, Marmot M, Oldfield Z, et al. Disease and disadvantage in the United States and in England. JAMA. 2006;295:2037–2045. doi: 10.1001/jama.295.17.2037. [DOI] [PubMed] [Google Scholar]
- 9.Cooper R, Cutler J, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: findings of the national conference on cardiovascular disease prevention. Circulation. 2000;102:3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 10.Kapral MK, Wang H, Mamdani M, et al. Effect of socioeconomic status on treatment and mortality after stroke. Stroke. 2002;33:268–273. doi: 10.1161/hs0102.101169. [DOI] [PubMed] [Google Scholar]
- 11.Palloni A, Arias E. Paradox lost: explaining the Hispanic adult mortality advantage. Demography. 2004;41:385–415. doi: 10.1353/dem.2004.0024. [DOI] [PubMed] [Google Scholar]
- 12.Kestenbaum B. Mortality by nativity. Demography. 1986;23:87–90. [PubMed] [Google Scholar]
- 13.Eschbach KS, Stimpson JP, Kuo YF, et al. Mortality of Hispanic immigrants and US born Hispanics at younger ages: a reexamination of recent patterns. Am J Public Health. 2007;97:1297–1304. doi: 10.2105/AJPH.2006.094193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hummer RA. Adult mortality differentials among Hispanic subgroups and non-Hispanic whites. Soc Sci Q. 2000;81:459–476. [PubMed] [Google Scholar]
- 15.Bureau UC. Current Population Survey, Annual Social and Economic Supplement Survey. Washington, DC: US Census Bureau, Population Division, Ethnicity & Ancestry Branch; 2006. [Google Scholar]
- 16.Brown DL, Al-Senani F, Lisabeth LD, et al. Defining cause of death in stroke patients: the brain attack surveillance in Corpus Christi Project. Am J Epidemiol. 2007;165:591–596. doi: 10.1093/aje/kwk042. [DOI] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention. State-specific mortality from stroke and distribution of place of death–United States, 1999. MMWR Morb Mortal Wkly Rep. 2002;51:429–433. [PubMed] [Google Scholar]
- 18.Centers for Disease Control and Prevention. Place of death after stroke—-United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2006;55:529–532. [PubMed] [Google Scholar]
- 19.Hahn RA, Wetterhall SF, Gay GA, et al. The recording of demographic information on death certificates: a national survey of funeral directors. Public Health Rep. 2002;117:37–43. doi: 10.1016/S0033-3549(04)50106-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenberg HM, Maurer JD, Sorlie PD, et al. Quality of death rates by race and Hispanic origin: a summary of current research, 1999. Vital Health Stat. 1999;2:1–13. [PubMed] [Google Scholar]
- 21.Sorlie PD, Rogot E, Johnson NJ. Validity of demographic characteristics on the death certificate. Epidemiology. 1992;3:181–184. doi: 10.1097/00001648-199203000-00018. [DOI] [PubMed] [Google Scholar]
- 22.Swallen K, Guend A. Data quality and adjusted Hispanic mortality in the United States, 1989–1991. Ethn Dis. 2003;13:126–133. [PubMed] [Google Scholar]
- 23.Sorlie PD, Backlund E, Johnson NJ, et al. Mortality by Hispanic status in the United States. JAMA. 1993;270:2464–2468. [PubMed] [Google Scholar]
- 24.Eschbach K, Kuo YF, Goodwin JS. Ascertainment of Hispanic ethnicity on California death certificates: implications for the explanation of the Hispanic mortality advantage. Am J Public Health. 2006;96:2209–2215. doi: 10.2105/AJPH.2005.080721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hambright Z. Marital status, nativity, and country of origin on the death certificate and matching census record. National Center for Health Statistics. Vital Health Stat. 1969;2:1–47. [PubMed] [Google Scholar]
- 26.Arias E, Schauman WS, Eschbach KE, et al. The Validity of Race and Hispanic Origin Reporting on Death Certificates in the United States. Vital and Health Statistics. 2008;2:1–24. [PubMed] [Google Scholar]
- 27.Gordis L. Epidemiology. Philadelphia, PA: Saunders Elsevier; 2009. [Google Scholar]
- 28.Selvin S. Epidemiologic Analysis. New York, NY: Oxford University Press; 2001. [Google Scholar]
- 29.Wein TH, Smith MA, Morgenstern LB. Race/ethnicity and location of stroke mortality: implications for population-based studies. Stroke. 1999;30:1501–1505. doi: 10.1161/01.str.30.8.1501. [DOI] [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention. Racial/ethnic disparities in prevalence, treatment, and control of hypertension–United States, 1999–2002. MMWR Morb Mortal Wkly Rep. 2005;54:7–9. [PubMed] [Google Scholar]
- 31.Markides KS, Coreil J. The health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep. 1986;101:253–265. [PMC free article] [PubMed] [Google Scholar]
- 32.Franzini L, Ribble JC, Keddie AM. Understanding the Hispanic paradox. Ethn Dis. 2001;11:496–518. [PubMed] [Google Scholar]
- 33.Smith DP, Bradshaw BS. Rethinking the Hispanic paradox: death rates and life expectancy for US non-Hispanic White and Hispanic populations. Am J Public Health. 2006;96:1686–1692. doi: 10.2105/AJPH.2003.035378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Elo IT, Preston SH. Estimating African-American mortality from inaccurate data. Demography. 1994;31:427–458. [PubMed] [Google Scholar]
- 35.Hill ME, Preston SH, Rosenwaike I. Age reporting among white Americans aged 85+: results of a record linkage study. Demography. 2000;37:175–186. [PubMed] [Google Scholar]
- 36.Hussey JM, Elo IT. Cause-specific mortality among older African-Americans: correlates and consequences of age misreporting. Soc Biol. 1997;44:227–246. [PubMed] [Google Scholar]
- 37.Preston S, Elo IT, Stewart Q. Effects of Age misrepoting on mortality estimates at older ages. Popul Stud. 1999;53:165–177. [Google Scholar]
- 38.Singh GK, Hiatt RA. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979–2003. Int J Epidemiol. 2006;35:903–919. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- 39.Singh GK, Siahpush M. All-cause and cause-specific mortality of immigrants and native born in the United States. Am J Public Health. 2001;91:392–399. doi: 10.2105/ajph.91.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Singh GK, Siahpush M. Ethnic-immigrant differentials in health behaviors, morbidity, and cause-specific mortality in the United States: an analysis of two National data bases. Hum Biol. 2002;74:83–109. doi: 10.1353/hub.2002.0011. [DOI] [PubMed] [Google Scholar]