Abstract
The last three years have seen significant changes in the Defence Medical Services approach to trauma pain management. This article seeks to outline these changes that have occurred at every level of the casualty's journey along the chain of evacuation, from the point of injury to rehabilitation and either continued employment in the Services or to medical discharge. Particular attention is paid to the evidence for the interventions used for both acute pain and chronic pain management. Also highlighted are possible differences in pain management techniques between civilian and military casualties.
Keywords: military trauma pain, acute pain, chronic pain
1. Introduction
Until relatively recently, it could be said that the military medical Zeitgeist was still one of providing the greatest good to the greatest number. This was the approach not only in the hot wars of the twentieth century but also throughout the Cold War where the unwritten understanding was that military medical services would be overwhelmed by large numbers of casualties. Robust triage was the order of the day and pain issues were very much relegated to the back seat of medical thinking.
During the last decade this approach has been challenged and the provision of high quality pain management is now an explicit aspect of military medicine. In the summer of 2007, the Surgeon General of the British Defence Medical Services went as far as to make it one of his three ‘main efforts’ (personal communication (Lt General L. Lillywhite L/RAMC, March 2010)). This reflects the changes occurring within our broader society as shown by a similar declaration by the Chief Medical Officer [1].
There are many reasons for treating pain. Chief among them are simple ‘humanitarian’ issues. However, good analgesia is also thought to reduce many medical complications affecting cardiovascular, respiratory and endocrine systems [2]. A recent study has also suggested that analgesia protects casualties against post-traumatic stress disorder (PTSD) [3].
The aim of this article is to outline current concepts in pain management and to describe the present organization of the British military pain service that extends from point of wounding to the point at which the individual leaves the military; once discharged from military service an individual is currently cared for through the National Health Service. The evidence for current practice is also discussed.
2. Definitions
Whatever pain is, it certainly is not only nociception. One of the most common definitions of pain is that it is ‘an unpleasant sensory and emotional experience, associated with actual or potential tissue damage, or described in terms of such damage’ [4]. Thus, when considering pain, the emotional component must always be considered.
Two other definitions to consider relate to pain classification. Pain becomes ‘chronic’ after three months; until this time it is traditionally referred to as acute. Once it is chronic it is usually thought to no longer indicate ongoing damage and may instead become a disease in its own right; there are of course lively discussions about this [5]. Finally, neuropathic pain is pain generated from injury or dysfunction of the nervous system itself (painful diabetic neuropathy, post-trauma pains), while nociceptive pain is the pain that results from the direct action of a noxious stimulus on the nociceptors (burns, inflammation).
The last concept that needs to be outlined is that of echelons of medical care. Currently, the British Defence Medical Services use four echelons, although more have been suggested in the past [6] and other nations have their own variations [7]. Broadly speaking, Role 1 is that period immediately following the injury. Care at this point will be provided by the individual, their immediate colleagues or perhaps a paramedic or doctor. Role 2 sees a more formal medical facility offering medical interventions but no surgical ones; in most of the current conflicts, as a consequence of rapid evacuation, Role 2 facilities are not used. Role 3 is the field hospital where casualties undergo life and limb saving surgery and physiological stabilization before aeromedical evacuation back to the UK where they enter the Role 4 establishments. These are currently the Royal Center for Defence Medicine (RCDM) at the University Hospitals of Birmingham and the Defence Medical Rehabilitation Center (DMRC) at Headley Court.
3. Background
The number of deaths during the British military's involvement in Iraq (Operation TELIC) and Afghanistan (Operation HERRICK) have been, and continue to be, well publicized. In contrast, the scale of the numbers of non-fatal casualties is less often broadcast. However, this information is now publicly available from the Defense Analytical Services Agency and shows a significant increase even over the period the data are available [8,9]( see tables 1 and 2).
Table 1.
The published casualty numbers that are being treated at both the Royal Centre for Defence Medicine and the Defence Centre for Medical Rehabilitation.
| 2007 from 8 October 2007 | 2008 | 2009 | 2010 to 31 March 2010 | |
|---|---|---|---|---|
| Op TELIC | 121 | 281 | 180 | 45 |
| Op HERRICK | 163 | 573 | 909 | 505 |
Table 2.
The published numbers of amputees amongst British military casualties. Please see the original data for definitions of terms used.
| 2006 from 1 April 2006 | 2007 | 2008 | 2009 | 2010 to 31 March 2010 | |
|---|---|---|---|---|---|
| Op TELIC | |||||
| amputees | 6 | 10 | 5 | 0 | 0 |
| significant multiple amputees | 0 | 0 | 0 | 0 | 0 |
| Op HERRICK | |||||
| amputees | 7 | 12 | 30 | 55 | 16 |
| significant multiple amputees | <5 | <5 | 6 | 26 | |
4. Pain scores
There are probably three reasons for scoring pain. Firstly, it provides a clinician an idea of what type of analgesic to use initially; severe pain suggests a strong analgesic. Secondly, it provides an idea of how well any intervention has worked, and thus what may be required subsequently. Finally, it alters the patient's experience of the pain because the pain is recognized as being ‘real’ by another person. This last function of scoring pain is often overlooked but is probably of great significance. The American author Naomi Wolf is credited with saying ‘pain is real when you get other people to believe in it. If no one believes in it but you, your pain is madness or hysteria’ [10].
Until recently there was no formally agreed scale for the UK military to use when measuring pain although the 0–10 numerical rating scale (NRS) was the most commonly used scale. In 2009, it was decided to use a simpler four point scale, from 0 (no pain) to 3 (severe pain) [11], as had been used in acute pain studies for many decades [12]. The aim was to simplify decision making for inexperienced care providers. If a casualty describes their pain on the 0–10 NRS as 6/10 what sort of analgesic should be used? If it then moves to 5/10, is this clinically significant? This extended scale suggests a spurious precision and poses questions to which the answers are not clear. By choosing 0–3 the scores loosely parallel the three stages of the World Health Organization's pain ladder which has been broadly adopted as an appropriate basic approach to pain management. Changes of one point on the scale (from 3 to 2 or 2 to 1 downwards, or 1 to 2 or 3 upwards) are likely to be clinically significant. The final point to note is the expectation to try to keep scores below 2 [13]—no worse than mild pain—and there is evidence that this is what patients rate highly in acute and chronic pain [14], though pain reduction that may not achieve this level of stringency does improve quality of life in chronic pain [15]. It is clear that a score below 2 will not always be possible to achieve, but it is right to have it as the target.
5. Pre-hospital analgesia
A systematic review performed by the Department of Military Anaesthesia and Critical Care has shown that surprisingly little good quality evidence exists to guide the treatment of pain in the prehospital environment, and usually the best that can be done is to extrapolate from civilian hospital practice. Many people discussing the use of analgesics in areas of conflict still quote the tremendous work by Dr Henry K. Beecher in which he described his experiences and ‘lessons learnt’ while a doctor in the US Army in the European theatre of World War 2. He stated that up to 75 per cent of soldiers wounded in battle did not want any analgesia and he famously compares this to his experiences of civilian trauma where the requirement for analgesia was, he suggested, significantly higher [16]. He also described a series of over 200 casualties in which 32 per cent had no pain, 26 per cent slight pain, 19 per cent moderate pain and 24 per cent severe pain [17].
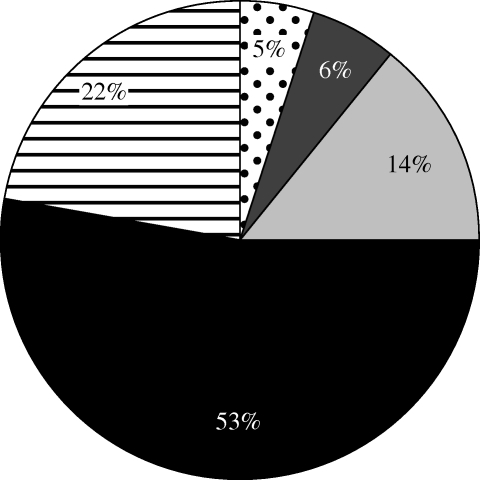
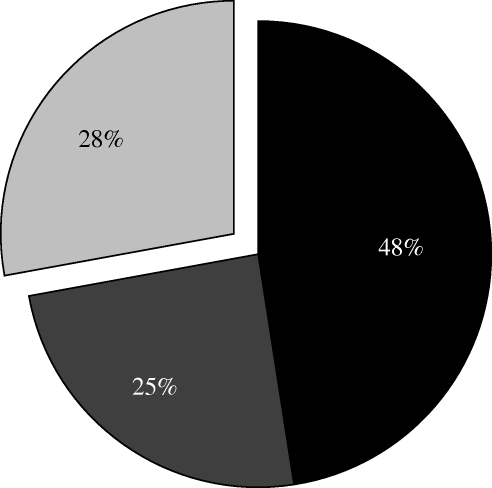
Against this background of 60 years ago, a study was conducted to establish current levels of pain. After gaining ethics committee approval a survey of casualties at Headley Court was conducted. Individuals were asked to estimate the severity of the pain they experienced from point of wounding back through the chain of evacuation to Headley Court (see figure 1). Two thirds, and the majority of those who could remember, remembered experiencing moderate or (more often) severe pain. They were also asked whether the initial analgesics helped. The results suggested that perhaps two thirds of those that could remember did think the pain was helped (figure 2).
Figure 1.
A pie chart indicating the distribution of pain scores at the point of wounding as remembered by casualties (pain scores: dotted region, none; dark grey region, mild; light grey region, moderate; black region, severe; hatched region, do not remember).
Figure 2.
A pie chart representing the distribution of responses given when casualties were asked to remember whether their initial analgesia helped to relieve their pain (responses: black region, yes; dark grey region, no; light grey region, do not remember).
These results seem to disagree with Beecher's findings, although clearly there are important differences in the study designs. For example Beecher asked casualties who could respond on arrival at the field hospitals, often several hours after injury. In our study casualties were weeks after injury and were asked their recollection of pain experienced at the point of injury. It is also fair to say that our population had probably experienced a greater degree of injury severity [18].
Currently, UK policy is for all service personnel to carry individual 10 mg morphine doses in intramuscular autojects. Although these have been issued for many years, the UK is the only country to entrust conventional forces with an individual issue. However, 10 mg intramuscular morphine has a similar analgesic efficacy to 1 g paracetamol or 400 mg ibuprofen [19] and thus complete analgesia cannot be expected from a few doses of morphine especially in the most severe injury. Following the systematic review and other anecdotal reports it has been decided to trial the use of oral transmucosal fentanyl citrate as an agent to augment the morphine. This trial is currently underway in Afghanistan. Although fentanyl and morphine act on the same receptors, it is likely that the fentanyl will have the added advantage of a built-in method of distraction: the applicator is rubbed against the oral mucosa to allow absorption. Thus, as pain increases casualties rub more vigorously so allowing a sense of control.
6. Role 3 field hospital analgesia
The choice of analgesia available in the field hospital mirrors that in a civilian hospital, with the usual mix of analgesic medication together with patient controlled analgesic (PCA) devices. The current device used is the Baxter Infusor PCA which has the advantage of being entirely mechanical, with no electronic components. This is important because a power supply is now not an issue, and more importantly there is no chance of it interfering with the navigation aids and other equipment used on Royal Air Force transport aircraft.
One significant development has been in the use of regional anaesthetic techniques. Regional anaesthesia is the process whereby local anaesthetic solutions are injected in such a way as to render a region of the body anaesthetized. This may be the result of epidural or spinal injections or alternatively peripheral nerve blocks. Although such techniques have been described in the military medical literature for many years [20], and often in very trying circumstances such as the jungles of Malaya when amputations had to be performed under spinal anaesthetic as that was all there was available [21], there have been concerns about their usefulness in the military setting.
Traditionally both techniques have involved the single bolus dose of local anaesthetic which gives excellent analgesia, albeit briefly. This may be sufficient within the civilian setting, but within the military it is more useful to be able to maintain analgesia for as long as possible. This concern has been allayed with the use of continuous infusions. The principal potential harm with epidural techniques has been that of infection, subsequent epidural abscess formation and the possible devastating sequelae of this [22,23]. However deployed military hospitals are moved from initial tented facilities into buildings more recognizable as hospitals as soon as possible, and with this comes significantly improved levels of cleanliness and operating theatre sterility.
There have been concerns around the use of peripheral nerve blockade, where the fear has been of delaying the diagnosis of acute compartment syndrome when the cardinal symptom of pain is removed. A systematic review conducted outlined the current understanding of the syndrome [24]. This was then combined with a discussion between the senior military surgeons and representatives of the Military Pain Special Interest Group. The result was the phrase in an editorial stating ‘clinicians should be encouraged to use regional analgesic techniques’ [25]. One significant difference between civilian and military casualties is that the latter will undergo repatriation, usually within hours of injury, and in a process that may itself take tens of hours. During this period the development of a compartment syndrome would be catastrophic as there is unlikely to be any facility to undertake the necessary treatment, fasciotomy, with the lack of a surgical team. Consequently, as part of the initial management of the military casualty, prophylactic fasciotomies may have to be performed [26].
There is also the problem of siting the block. Traditionally, one would use an electrical current transmitted through the tip of the needle; as the needle approaches the nerve to be blocked it stimulates the nerve, which results in motor stimulation of the limb, seen as movement distal to the nerve. This relies on an intact limb and in military casualties the limb may be absent or too injured to move. Recent development of portable ultrasound devices are revolutionising the procedure as they provide realtime views of anatomical structures allowing placing of catheters next to nerves. Through these catheters local anaesthetics can be infused allowing prolonged periods of analgesia [27].
7. Repatriation
The next phase of the casualty's care is repatriation. The fundamental tenet of this phase is to ensure analgesia is achieved before the journey begins since trying to do so during the journey is always very difficult. It should also be remembered that in an aircraft there are no drugs or equipment available that you have not already put on board and getting expert help is also impossible unless it too is onboard at take-off [28]. The Royal Air Force's aeromedical teams are now able to manage PCAs, epidurals and continuous peripheral nerve blocks in flight. They are also able to manage the casualties who do not have these advanced techniques but who may still develop pain.
8. Role 4: the royal center for defence medicine
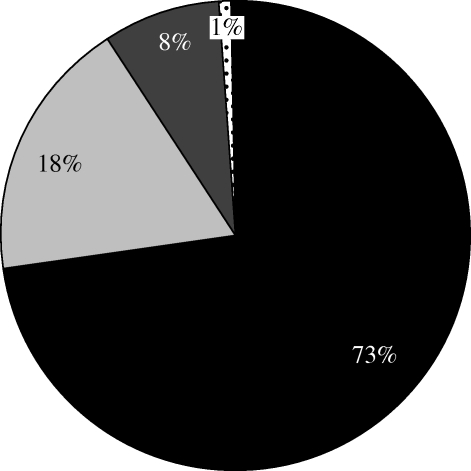
RCDM is located within the University Hospitals Birmingham NHS Foundation Trust, and has been the primary receiving unit for British military casualties since 2001. Most civilian hospitals in the UK have acute pain teams although it may be proper to suggest that they are ‘analgesic risk management services’; their primary role appears to be ensuring the use of techniques such as epidurals and local anaesthetic infusions is safe. Thus only patients with these ‘advanced’ devices will be seen rather than all of the other patients who are likely to have pain [29]. Rates of moderate and severe pain in patients on civilian surgical wards typically range from 30 to 80 per cent [29–31]. The results of a prospective survey of pain scores collected over five weeks and including 922 data points on the military ward at RCDM showed our combined moderate and severe pain scores were less than 10 per cent (figure 3) with 90 per cent of casualties having pain scores of no more than 0 or 1.
Figure 3.
A pie chart demonstrating the distribution of pain scores recorded among the military patients at RCDM over five weeks. There were 922 data points (pain score: black region, 0; light grey region, 1; dark grey region, 2; dotted region, 3).
The techniques used in RCDM mirror those that would be expected in any hospital dealing with acute trauma although there is a particular focus on regional anaesthetic techniques. There are probably two reasons for this. First, it has been suggested that continuous peripheral nerve blocks lead to lower pain scores [32]. Secondly, for patients who undergo multiple operations over a short period of time, as the military do, having an analgesic that does not have systemic side effects is intuitively of more use than the alternative (opiate based) analgesia. There are of course exceptions such as the soldier who refused such a technique, instead taking relatively significant doses of opioid for his pain. When asked why he refused his answer was to be able to see his thumb move was of great importance to him as it reassured him that the nerves were getting better and thus his future serving with his infantry regiment was still possible.
Unlike normal civilian practice it is routine for us to send all catheters, both epidural and peripheral nerve block, to the pathology department for culture and identification of any microorganisms. The reason for this is the fear surrounding increased risks of contamination. This fear is not related to the conditions in which the catheters were introduced, as was the original worry mentioned above, but more because of the conditions the patients themselves are in. Very often, unlike civilian practice, casualties will have come into the field hospital after weeks of living in very basic conditions with limited washing facilities. Happily, after more than 130 catheters on the database, although a few have grown microorganisms, none have been clinically significant. This then tends to support the continued use of this relatively new technique in deployed military analgesia.
Morphine PCAs are also used regularly. In contrast to many civilian pain services the simultaneous use of oral opiates, PCAs and continuous peripheral nerve blocks on the same patient is not a rare event.
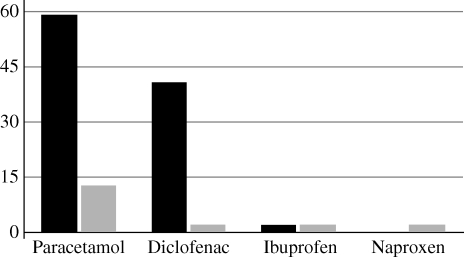
Although most of the medication used is the same as would be found in any hospital, treatment against neuropathic pain is started at a relatively early stage. Indeed, the question asked is not so often ‘should we start it?’, But more often ‘why should we not start it?’. If significant nerve injury is suspected amitriptyline will have been started in Role 3. At RCDM this will be continued but pregabalin will often be introduced. In a recent survey of patients on the military ward at RCDM, 66 per cent were on a combination of amitripyline and pregabalin (see figure 4).
Figure 4.
The typical doses of amitriptyline taken at night and pregabalin taken twice a day used by the military casualties at RCDM. The size of the data point is proportional to the number of patients on that combination, so most are on 75 mg amitriptyline (at night) and 300 mg pregabalin (twice a day).
Studies have suggested that anti-neuropathic pain agents reduce peri-operative opiate requirements [33], although this effect has not been studied.
Effort is also taken to educate the patients in what they are taking, how often they should take them, what the side effects are likely to be, and finally when and how they should reduce the doses. This is an important aspect to their acute pain management since once they are discharged from RCDM they will immediately become responsible for their own medication. Although the use of dedicated telephone support is provided they may have difficulty getting other advice so the better the preparation for their discharge the fewer the problems they should encounter once out of the regimented schedule of a hospital.
9. Role 4: the defence medical rehabilitation center
The primary center for the rehabilitation of British military casualties is the DMRC at Headley Court. This was originally developed for the rehabilitation of Officers of the Royal Air Force following World War 2 but now serves casualties of all ranks and all services.
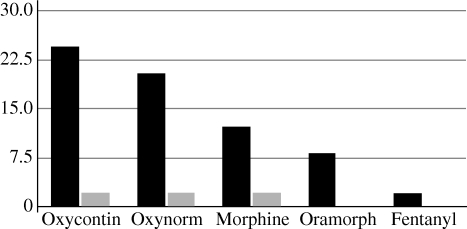
One of the greatest fears with the use of morphine is that of addiction. Indeed much is made of the rates of addiction encountered by the soldiers of America's Civil War, leading to the development of the term ‘soldier's disease’; there is of course much discussion around whether or not this is just a twentieth century construct but that is beyond the scope of this essay. Suffice to say it was against this background a survey was conducted at DMRC to compare rates of opiate use on arrival and final entry in patient's notes. The expectation was that most patients, who were all amputees in this study, would be on opiates of varying type and dose on arrival and during the course of their rehabilitation they would come off their medication. The results showed that there is no indication of inappropriate medication use in the British military population (figures 5 and 6).
Figure 5.
The differences between the percentage of amputees taking simple analgesics when they initially presented at DMRC and the last entry in their notes (black bars, % initially; grey bars, % finally).
Figure 6.
The differences between the percentage of amputees taking strong opioids when they initially presented at DMRC and the last entry in their notes (black bars, % initially; grey bars, % finally).
Some of the less seriously injured personnel will receive most of their rehabilitation in one of the regional rehabilitation units that have been established around the country. Efforts are underway to ensure that these receive regular visits from military pain specialists and that they have appropriate routes of communication for support at all other times.
10. Primary healthcare: completing the circle
The final step in the process is the management of pain issues in primary care. This will be for those casualties that have managed to return to work or who are still undergoing their rehabilitation. One of the problems is that many of the agents and processes being used in the British military will be outside the normal experience of a primary care doctor, either military or civilian. In an attempt to help both the casualties and their medical officers, steps are being taken to provide pain clinics in the larger garrisons. These are clinics at which senior consultants in pain medicine and their colleagues in rehabilitation or sports and exercise medicine see patients together. An integral aspect of these clinics is the education of junior primary care physicians.
11. Other agencies and issues
The importance of involving many disciplines in the management of pain is well recognized; the management of pain extends throughout the continuum of patient care. The explicit involvement of anaesthetists, surgeons, physicians, psychiatrists and primary care doctors, together with nurses, physiotherapists, occupational therapists and psychologists is encouraged at every level. The current structure of British military healthcare also involves the integration of military and civilian healthcare providers, adding another dimension to the organizational mix.
As well as the clinical changes outlined above there have been a number of other aspects to the management of pain within the British military that have changed recently. The first of these is a clear understanding of the importance of good surveys and audit processes. These are now encouraged at every level and every site of intervention. These are not performed ‘just for fun’ but have all provided useful information to allow the further development of the service, and as an essential component of quality management and to drive home that ‘no worse than mild pain’ is the target.
Research is also recognized as being an important aspect of the service. However, because of the relatively small numbers of casualties, the huge number of confounding elements that exist when considering pain and finally the austere environments that may be faced, it is difficult to design studies of sufficient power to allow any conclusive findings. To date systematic reviews of the medical literature, notably of acute compartment syndrome and prehospital analgesia, have been used in an attempt to overcome some of these problems. These have been written in collaboration with colleagues from the University of Oxford.
After clinical issues, audit and research, the other principle on which the military pain service is built is education. The Battlefield Advanced Life Support (BATLS) course has had its section on pain issues updated. This is the course that many UK and other nation's [34] healthcare providers will undergo to provide them with the necessary military medical skills prior to operational deployments. Tailored lectures on pain are provided to the staff deploying to the field hospitals as part of their pre-deployment training phase (HOSPEX—hospital exercise [35]) and the Standard Operating Procedures and Clinical Governance on Operations documents are annually reviewed to ensure they are up to date. All doctors joining the Royal Army Medical Corps undergo a period of training in military medicine, the Post-Graduate Medical Officers (PGMO) course, and there is now a full day devoted to discussing military pain management issues; this itself is a coup given that most UK medical graduates receive less education in pain management than a veterinarian [36].
12. Discussion
At the outset of this section, it must be stated that although this essay has focused on the management of pain following trauma on an operational deployment, a significant number of casualties repatriated will not be from this group; 24 per cent of US operational repatriations, the largest single group in one study, were classified as musculoskeletal and connective tissue disorders [37] and not direct battle-related injuries. Because the UK has deployed forward rehabilitation units [38] this is significantly lower for the UK. However, to any military force it is significant, as one would expect from an organization where physical performance is so important [39].
Over the last three years since the Surgeon General made his ‘main effort’ statement, military pain management has come a very long way. The reasons for this are multiple. Most important was the main effort statement itself; if the top of an organization thinks a cause is important it facilitates all actions aimed at addressing it. The fact that as a nation we have been involved in two large-scale military operations that have produced significant casualty numbers is also important; the public support for the Help for Heroes organization is a clear manifestation of this.
Another change is the dawning recognition that military casualties are different to civilian ones. The largest cause of significant acute pain in our civilian population is probably post-operative pain. In this case patients have had a condition for some time before voluntarily travelling to a hospital and undergoing an operative procedure, having received information on what to expect post-operatively. In a survey of a civilian hospital most patients experienced significantly less pain than they thought they would [40]. This is clearly different to the young military trauma casualty who may wake up thousands of miles away and after life-changing injuries. The military patient with persistent pain is again different to their civilian counterpart; they are usually younger and possibly on the brink of losing their jobs. The consequence of this is that military pain management specialists, arguably unlike their civilian colleagues, have the clear aim of keeping their patients employed within the service and if this is not possible to prepare them as well as possible for life after service.
The Defence Medical Services also have the advantage of being an organization that has relatively good communication and is able to promote new ideas and guidelines rapidly across its membership. Thus, many changes can be swiftly promulgated and can be expected to be implemented. It is against this background a service that is integrated and sustainable is being created: integrated at each stage with what has gone before and afterwards, and sustainable so that each provider can fulfil the basic requirement and it does not rely upon a few high performers alone.
One of the great problems associated with the treatment of pain is a lack of the fundamental understanding of the mechanisms that cause pain. The call for a mechanism-based treatment for pain was made some time ago [41,42] and as can be seen the split between neuropathic and nociceptive management is made in our system. However, most pain treatment is still fundamentally empirical in nature and thus the importance of good audit and surveys of pain experiences, particularly in our relatively small populations cannot be underestimated.
Of course, the holy grail of pain management is the prevention of chronic pain conditions [43]. As already stated, because of the large number of variables involved and the relative rarity of the outcome, it would not be possible to prove that the current military approach does achieve this. However the data collected, presented here, and used as a guide appears to support the system being developed.
Acknowledgements
The authors would like to thank all of the members of the Defence Medical Services, together with their civilian colleagues, who have helped to provide the data used while maintaining their significant clinical outputs. In particular, thanks go to Col S. Jagdish L/RAMC, Lt Col J. Ralph RAMC, Sqn Ldr C. Flutter RAF, Dr P. Wood, Mrs D. Edwards, Sgt Devonport QARANC.
Footnotes
One contribution of 20 to a Theme Issue ‘Military medicine in the 21st century: pushing the boundaries of combat casualty care’.
References
- 1.Sir Liam Donaldson C.M.O. 2009. 150 years of the annual report of the Chief Medical Officer: on the state of public health 2008. pp. 73 London, UK: Department of Health [Google Scholar]
- 2.Cousins M., Power I. 1994. Acute and postoperative pain. In Textbook of pain (eds Melzack R., Wall P. D.), pp. 357–385 London, UK: Churchill Livingstone [Google Scholar]
- 3.Holbrook T. L., Galarneau M. R., Dye J. L., Quinn K., Dougherty A. L. 2010. Morphine use after combat injury in Iraq and post-traumatic stress disorder. N. Engl. J. Med. 362, 110–117 (doi:10.1056/NEJMoa0903326) [DOI] [PubMed] [Google Scholar]
- 4.Merskey H., Bogduk N. 1994. Classification of chronic pain (eds Merskey H., Bogduk N.). Seattle: International Association for the Study of Pain [Google Scholar]
- 5.Tracey I., Bushnell M. C. 2009. How neuroimaging studies have challenged us to rethink: is chronic pain a disease? J. Pain 10, 1113–1120 (doi:10.1016/j.jpain.2009.09.001) [DOI] [PubMed] [Google Scholar]
- 6.Ryan J. M., Sibson J., Howell G. 1990. Assessing injury severity during general war. Will the Military Triage system meet future needs? J. R. Army Med. Corps 136, 27–35 [DOI] [PubMed] [Google Scholar]
- 7.Saric V., Atias-Nikolov V., Frankovic E., Mrsic V., Lucak J. 1994. NATO war medicine doctrine revisited in Bosnia and Herzegovina. J. R. Army Med. Corps 140, 132–134 [DOI] [PubMed] [Google Scholar]
- 8.DASA 2010. British casualties—Afghanistan. www.dasa.mod.uk
- 9.DASA 2010. Monthly Iraq and Afghanistan UK Patient Treatment Statistics—RCDM and DMRC Headley Court. www.dasa.mod.uk
- 10.Wolf N. 1998. The beauty myth: how images of beauty are used against women, 1st edn. London, UK: Vintage [Google Scholar]
- 11.Looker J., Aldington D. 2009. Pain scores—as easy as counting to three. J. R. Army Med. Corps 155, 42–43 [DOI] [PubMed] [Google Scholar]
- 12.Moore R. A., Jayne E., Jodie B., Henry M. 2003. Bandolier's little book of pain. Oxford, UK: Oxford University Press [Google Scholar]
- 13.McQuay H. J. 2009. Measuring acute pain. Foreword. J. R. Army Med. Corps 155, 42. [DOI] [PubMed] [Google Scholar]
- 14.Mhuircheartaigh R. J., Moore R. A., McQuay H. J. 2009. Analysis of individual patient data from clinical trials: epidural morphine for postoperative pain. Br. J. Anaesth. 103, 874–881 (doi:10.1093/bja/aep300) [DOI] [PubMed] [Google Scholar]
- 15.Moore R. A., Straube S., Paine J., Phillips C. J., McQuay H. J. 2010. Fibromyalgia: moderate and substantial pain intensity reduction predicts improvement in other outcomes and substantial quality of life gain. Pain 149, 360–364 (doi:10.1016/j.pain.2010.02.039) [DOI] [PubMed] [Google Scholar]
- 16.Beecher H. K. 1960. Control of suffering in severe trauma. Usefulness of a quantitative approach. J. Am. Med. Assoc. 173, 534–536 [DOI] [PubMed] [Google Scholar]
- 17.Beecher H. K. 1946. Pain in men wounded in battle. Ann. Surg. 123, 96–105 (doi:10.1097/00000658-194601000-00008) [PMC free article] [PubMed] [Google Scholar]
- 18.Rayment S. 2010. Thousands of British troops wounded in Afghanistan. The Telegraph, 20 Feb. (online). Available at: <http://www.telegraph.co.uk/news/worldnews/asia/afghanistan/7278645/Thousands-of-British-troops-wounded-in-Afghanistan.html> (accessed 30 October 2010). [Google Scholar]
- 19.McQuay H., Moore R. A. 1998. Acute pain: conclusion. In An evidence based resource for pain relief, pp. 187–193 Oxford: Oxford University Press. [Google Scholar]
- 20.Robbe 1946. A reliable method of performing the peridural analgesia (P.D.A.). J. R. Army Med. Corps 87, 169–172 [PubMed] [Google Scholar]
- 21.Markowitz J. 1946. A series of over 100 amputations of the thigh for tropical ulcer. J. R. Army Med. Corps 86, 159–170 [PubMed] [Google Scholar]
- 22.Horlocker T. T., Wedel D. J. 2008. Infectious complications of regional anesthesia. Best Pract. Res. Clin. Anaesthesiol. 22, 451–475 (doi:10.1016/j.bpa.2008.06.003) [DOI] [PubMed] [Google Scholar]
- 23.Reynolds F. 2008. Neurological infections after neuraxial anesthesia. Anesthesiol. Clin. 26, 23–52 [DOI] [PubMed] [Google Scholar]
- 24.Hayakawa H., Aldington D. J., Moore R. A. 2009. Acute traumatic compartment syndrome: a systematic review of results of fasciotomy. Trauma 11, 5–35 (doi:10.1177/1460408608099028) [Google Scholar]
- 25.Clasper J. C., Aldington D. J. 2010. Regional anaesthesia, ballistic limb trauma and acute compartment syndrome. J. R. Army Med. Corps 156, 77–78 [DOI] [PubMed] [Google Scholar]
- 26.Clasper J. C., Standley D., Heppell S., Jeffrey S., Parker P. J. 2009. Limb compartment syndrome and fasciotomy. J. R. Army Med. Corps 155, 298–301 [DOI] [PubMed] [Google Scholar]
- 27.Hughes S., Birt D. 2009. Continuous peripheral nerve blockade on OP HERRICK 9. J. R. Army Med. Corps 155, 57–58 [DOI] [PubMed] [Google Scholar]
- 28.Flutter C., Ruth M., Aldington D. 2009. Pain management during Royal Air Force strategic aeromedical evacuations. J. R. Army Med. Corps 155, 61–63 [DOI] [PubMed] [Google Scholar]
- 29.Dolin S. J., Cashman J. N., Bland J. M. 2002. Effectiveness of acute postoperative pain management: I. Evidence from published data. Br. J. Anaesth. 89, 409–423 (doi:10.1093/bja/aef207) [PubMed] [Google Scholar]
- 30.Drew J., Aldington D. 2005. A hospital audit of pain. In Abstracts of IASP (International Association for the Study of Pain), 11th World Congress on Pain, Sydney, Australia, 21–26 August 2005. Seattle: IASP Press. [Google Scholar]
- 31.Popping D. M., Zahn P. K., Van Aken H. K., Dasch B., Boche R., Pogatzki-Zahn E. M. 2008. Effectiveness and safety of postoperative pain management: a survey of 18925 consecutive patients between 1998 and 2006 (2nd revision): a database analysis of prospectively raised data. Br. J. Anaesth. 101, 832–840 (doi:10.1093/bja/aen300) [DOI] [PubMed] [Google Scholar]
- 32.Buckenmaier C. C., Rupprecht C., McKnight G., McMillan B., White R. L., Gallagher R. M., Polomano R. 2009. Pain following battlefield injury and evacuation: a survey of 110 casualties from the wars in Iraq and Afghanistan. Pain Med. 10, 1487–1496 (doi:10.1111/j.1526-4637.2009.00731.x) [DOI] [PubMed] [Google Scholar]
- 33.Tiippana E. M., Hamunen K., Kontinen V. K., Kalso E. 2007. Do surgical patients benefit from perioperative gabapentin/pregabalin? A systematic review of efficacy and safety. Anesth. Analg. 104, 1545–1556 (doi:10.1213/01.ane.0000261517.27532.80) [DOI] [PubMed] [Google Scholar]
- 34.Molde A., Milasius S., Lundberg L. 2006. BATLS/BARTS training in Lithuania. J. R. Army Med. Corps 152, 217–220 [DOI] [PubMed] [Google Scholar]
- 35.Davies T., Nadin M. N., McArthur D. J., Cox C. W., Roberts P. 2008. Hospex 2008. J. R. Army Med. Corps 154, 195–201 [DOI] [PubMed] [Google Scholar]
- 36.Briggs E., Whittaker M., Carr E. 2009. Survey of undergraduate pain curricula for healthcare professionals in the United Kingdom. A short report. London: The British Pain Society; Available at <http://www.britishpainsociety.org/members_sig_edu_short_report_survey.pdf> (accessed 30 October 2010). [DOI] [PubMed] [Google Scholar]
- 37.Cohen S. P., Brown C., Kurihara C., Plunkett A., Nguyen C., Strassels S. A. 2010. Diagnoses and factors associated with medical evacuation and return to duty for service members participating in Operation Iraqi Freedom or Operation Enduring Freedom: a prospective cohort study. Lancet 375, 301–309 (doi:10.1016/S0140-6736(09)61797-9) [DOI] [PubMed] [Google Scholar]
- 38.Bennett A., Phillip R., Scott P., Minden D., Jones T., Mistlin A. 2006. Rheumatology, rehabilitation medicine and sports and exercise medicine. J. R. Army Med. Corps 152, 163–174 [DOI] [PubMed] [Google Scholar]
- 39.Aldington D. 2009. Back pain: the silent military threat. Arch. Intern. Med. 169, 1923–1924 (doi:10.1001/archinternmed.2009.385) [DOI] [PubMed] [Google Scholar]
- 40.Aldington D., Hatton K. 2007. A comparison of peri-operative pain expectation and experience. A poster abstract at: Annual Scientific Meeting of the British Pain Society, Glasgow, UK, 24–27 April 2007. [Google Scholar]
- 41.Woolf C. J. 2004. Pain: moving from symptom control toward mechanism-specific pharmacologic management. Ann. Intern. Med. 140, 441–451 [DOI] [PubMed] [Google Scholar]
- 42.Woolf C. J., Decosterd I. 1999. Implications of recent advances in the understanding of pain pathophysiology for the assessment of pain in patients. Pain 82(suppl 1), S141–S147 [DOI] [PubMed] [Google Scholar]
- 43.Kehlet H., Jensen T. S., Woolf C. J. 2006. Persistent postsurgical pain: risk factors and prevention. Lancet 367, 1618–1625 (doi:10.1016/S0140-6736(06)68700-X) [DOI] [PubMed] [Google Scholar]