Abstract
The conflicts in Iraq and Afghanistan have been epitomized by the insurgents' use of the improvised explosive device against vehicle-borne security forces. These weapons, capable of causing multiple severely injured casualties in a single incident, pose the most prevalent single threat to Coalition troops operating in the region. Improvements in personal protection and medical care have resulted in increasing numbers of casualties surviving with complex lower limb injuries, often leading to long-term disability. Thus, there exists an urgent requirement to investigate and mitigate against the mechanism of extremity injury caused by these devices. This will necessitate an ontological approach, linking molecular, cellular and tissue interaction to physiological dysfunction. This can only be achieved via a collaborative approach between clinicians, natural scientists and engineers, combining physical and numerical modelling tools with clinical data from the battlefield. In this article, we compile existing knowledge on the effects of explosions on skeletal injury, review and critique relevant experimental and computational research related to lower limb injury and damage and propose research foci required to drive the development of future mitigation technologies.
Keywords: blast injury, biomechanics, high strain rates, lower limb, finite-element modelling, impact testing
1. Introduction
The origins of anti-vehicular warfare can be traced back to ancient Byzantium. In 120 BC, Philo documented the burial of large empty earthenware jars as deadfalls around city walls to immobilize siege towers while not impeding pedestrian traffic during peace time [1]. In the twentieth century, the advent of the motorized transport provided armies with a new-found mobility [2]. To counter this, novel explosive devices were devised: the anti-vehicle (AV) landmine.
Since its inception in World War I, the AV mine has become the main threat to vehicles and their occupants, in both modern war and peace support operations [3]. Counter-insurgency operations have no frontline; insurgents merge with the general population and strike irregularly at widely scattered locations that cannot be readily anticipated. Ambush of patrols and convoys with direct fire from small arms and rocket-propelled grenades, and indirect mortar fire of fixed positions have been characteristic of previous insurgency operations [4–6]. In contrast, the signature weapon of the conflicts in Iraq and Afghanistan has been the roadside bomb or improvised explosive device (IED) [7–10]. Critically, injuries from IEDs are very different from those of gun-shot wounds (figure 1). The soft tissue injury combined with considerable foreign debris often requires aggressive surgery [10]. In a single incident, an IED can cause multiple casualties, with devastating injuries requiring multi-disciplinary intervention, subsequently placing a significant burden on field hospital surgical facilities.
Figure 1.
Lower limb injury following an under-vehicle explosion.
Survivability from battlefield injuries has increased from 69.7 per cent in World War II to 88.6 per cent most recently in Iraq [11]. This has been attributed to a number of factors including improved torso protection, enhanced pre-hospital care and rapid aero-evacuation to medical facilities capable of providing optimized resuscitation and damage control surgery. Consequently, there has been an increased incidence of severely injured casualties surviving with multiple extremity injuries. Recent studies from Iraq and Afghanistan have shown that extremity injuries are seen in over 70 per cent of casualties, with the lower limbs injured in 45 per cent of all casualties [9,12–14]. Furthermore, in a recent review of casualties from IEDs, 46/53 (87%) of casualties are reported to have sustained injuries to the lower limbs [8].
In view of the fact that IEDs pose the most prevalent single threat to UK and Coalition troops operating in both theatres of operation, and that the extremities are the most frequently injured body region, there is an urgent requirement to investigate and mitigate against the mechanism of lower limb injury caused by these devices. This article compiles existing knowledge on the effects of explosions on skeletal injury, critiques experimental and computational research related to injury of the lower limb in impact loading environments and proposes research foci required to drive the development of future mitigation technologies.
2. Interaction of explosion on vehicles and its occupants
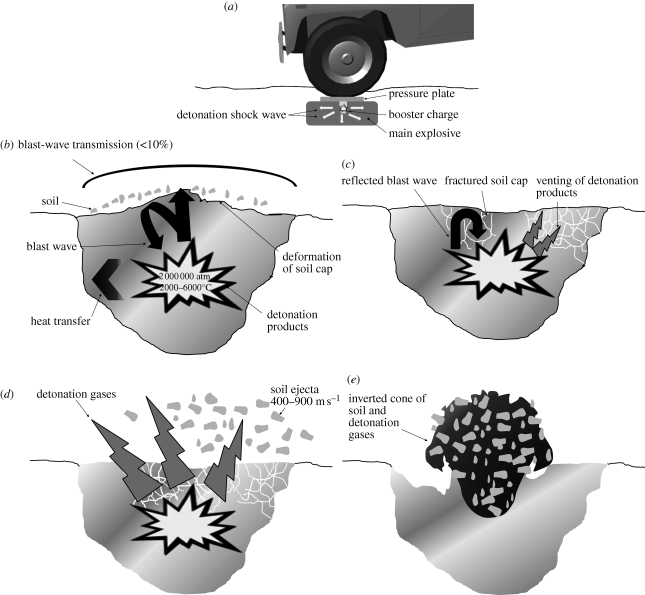
When a vehicle triggers a mine, the explosive detonates. Detonation is a shock wave process whereby the wave propagates through the explosive causing an instantaneous (less than 1 µs) chemical reaction (figure 2). Behind the detonation wave, the explosive has been converted to hot, high-pressure gas: the detonation products. Local pressures are typically in the range of 1 000 000–2 500 000 atm while temperatures are from 2000 to 6000°C [15]. This gas expands outwards at 3–4 km s−1, violently pushing material out of the way. Several physical processes then take place that determine the amount of energy transmitted to a target.
Figure 2.
The physics of a mine blast. (a) Triggering of the mine results in an exothermic reaction and formation of a blast wave. (b) The blast wave is mainly reflected at the soil interface and (c) causes fracture of the soil cap. (d) The detonation products are vented through the fractured soil cap, resulting in the release of the soil ejecta. (e) The overall result is an inverted hollow cone of super-heated detonation gases surrounded by the soil ejecta. They both then act on the floor of the vehicle, resulting in injury to the occupants.
For a landmine, these processes can be characterized by three distinct phases: (i) the explosive interacts with the soil, (ii) gas expands pushing material outwards from the surface, and (iii) the soil ejecta interacts with the vehicle [16].
(a). Interaction with soil
First, the wave processes are dominant; there is transmission of the pressure from the detonation wave to the immediate surroundings. The transmitted shock wave compresses the soil material. Upon reaching the soil–air interface, a small fraction of the incident shock wave (typically less than 10%) is transmitted into the air and a thin top-layer of loose soil is ejected upwards [17]. This shock wave produces a relatively minor load on the vehicle body unless the vehicle is in very close proximity to the soil/air interface [3].
The bulk of the compression wave upon reaching the soil–air interface is largely reflected backwards towards the explosion centre as a release fan, owing to the large impedance mismatch at this interface [3] (figure 2b). The interaction of the shock pulse with the surface causes fracture of the soil cap. The strength of soils and of most geological materials is small compared with the detonation pressure and so the soil is rapidly damaged and accelerated. With the movement of the soil cap, fractures can further develop in the cap, through which some of the product gases can flow (figure 2c).
On longer time scales (milliseconds), there is some heat transfer from the gases to the soil adjacent to the bubble of detonation gases.
(b). Gas expansion
Detonation of the explosive results in the formation of large quantities of gas. As the detonation products expand, they eject the soil plug at supersonic speed. The high pressure of the gases will cause localized deformation of the floor of the vehicle if the flow is trapped under the vehicle. Some of the high-pressure gas also vents through the fractures in the soil, along the path of least resistance. This gas carries soil particles at speeds of between 1300 and 3200 km h−1 [3] (figure 2d).
(c). Soil ejecta
The soil ejecta phase manifests itself via two primary modes of action. First, a radial compression wave propagates outwards in the soil, pushing the plug of soil ahead and into the vehicle. The second mode of action takes place in the region that will form the boundary of the post-explosion crater. There, the flow shears the soil and soil particles are carried away in a net upward direction towards the vehicle. The net result is typically that a hollow inverted cone of soil ejecta is carried within the flow of expanding hot product gas (figure 2e). Impact of this ejecta with the vehicle will transfer some of the kinetic energy and cause rapid acceleration of the vehicle, resulting in significant injury to the occupants.
Hence, the two dominant load transfer mechanisms to the target vehicle are the expansion of the detonation products and the energy transfer from soil ejecta. The gas phase provides the first phase of this impulse. During this phase, any portion of the vehicle located in the expansion zone of the detonation products is exposed to a transient, high-pressure flow. This may cause rupture of the floor pan and endangers the occupants who are then exposed to secondary fragments and hot gases. Even in cases where floor rupture does not occur, rapid deflection of floor plates in localized regions presents a great danger to occupants. In the second phase, impact by the soil ejecta acts on the whole vehicle and results in aggressive acceleration of the vehicle.
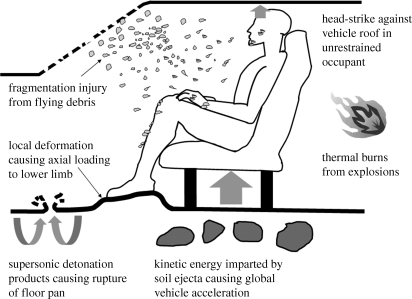
After being lifted by the blast, the vehicle will fall to the ground under the effects of gravity, potentially resulting in more injury, especially if the occupants are not appropriately restrained (figure 3).
Figure 3.
Vehicle occupant injury mechanisms.
AV-mine explosions cause injury through a variety of mechanisms. Classically, any injury from a generic explosion can be categorized into four types; primary, secondary, tertiary and quaternary blast injury [18–20]. The clinical manifestations of these effects and their likely injury potential are summarized in table 1 [21]. Of these, tertiary blast effects are the most significant injury mechanism in an under-vehicle explosion and development of countermeasures to attenuate this effect remain a key aim in reducing mortality and morbidity in vehicle occupants.
Table 1.
Summary of human effects from AV-mine blast. Reproduced with permission from Ramasamy et al. [21].
| blast injury | mechanism of injury | clinical effects | mitigation requirement | vehicle mitigation |
|---|---|---|---|---|
| primary | blast shock wave | traumatic amputation, soft tissue deformation, fractures via brisance effect, primary blast lung, gastrointestinal injury | reduce blast transfer | increased stand-off and improved gas dynamic characteristics mitigating brisance and the inclusion of blast-mitigating materials |
| secondary | fragments from mine products, energized soil ejecta and vehicle fragments | penetrating wounds particularly to the lower extremity and facial injuries from glass fragments; extremity fractures from direct impact of fragments | reduce fragments, or protect against fragments | improved armour protection of vehicle floor and improved personal protection |
| tertiary | global—vehicle acceleration; local—floor pan deformation | significant axial loading leading to lower limb (especially calcaneal), pelvic and spinal injuries; head injuries from collision with vehicle roof | reduce vehicle acceleration, reduce capture of pressure wave by vehicle, increase resistance to floor-plate geometrical changes | increased stand-off, V-shaped hull design, occupant restraints to prevent collision injuries |
| quaternary | thermal injuries | burns | protect against burns | fire-resistant materials in vehicles and fire-retardant clothing |
3. Clinical injury data
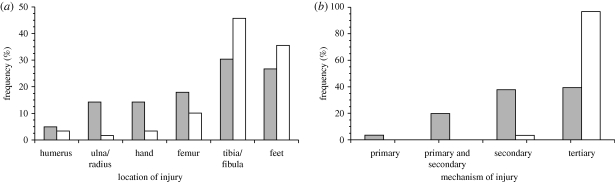
Using clinical data from casualties admitted to the Field Hospital in Southern Afghanistan, Ramasamy et al. [22] performed a forensic interpretation of radiographs of 62 consecutive casualties injured in an explosion. The predominant mechanism of injury was determined by identifying key features within the fracture patterns (table 2 and figure 4).
Table 2.
Injury mechanisms from explosion and its interaction with bone.
| explosion type | pathophysiology | fracture characteristics |
|---|---|---|
| primary | blast wave-mediated fracture [71,72] | traumatic amputation; short oblique/transverse fractures |
| secondary | direct impact of fragment [73] | highly comminuted multi-fragmentary fractures |
| primary and secondary | contact with seat of explosion, resulting in blast wave and fragment injury (e.g. anti-personnel landmine explosion) [74] | traumatic or sub-total amputation with significant soft tissue injury and fragments |
| tertiary | displacement of the casualty or objects near the casualty | axial loading, three-point bending, spiral fractures |
Figure 4.
Illustrative examples of fracture patterns caused by the different blast mechanisms.
Comparison of casualties injured out in the open to those injured in an enclosed space (e.g. under cover or in a vehicle) demonstrated that there was a higher proportion of lower limb injuries in the enclosed group (81 versus 52%, p < 0.01; figure 5a) and tertiary blast effects predominated, accounting for 96 per cent of injuries (57/59, p < 0.001; figure 5b). In contrast, there were no primary or combined primary and secondary injuries and only two secondary blast injuries in the enclosed group [22].
Figure 5.
Effect of environment on (a) fracture location and (b) mechanism of injury. Grey bars, open; white bars, enclosed.
4. Current clinical focus
One of the significant deficits in vehicle explosion mitigation research has been a dearth of clinical information on the injury profile of injured vehicle occupants. To date, clinical information related to these incidents has been limited to a single case series of injuries over a five year period in Croatia [23]. Of the 42 casualties described in that report, six casualties sustained either unilateral or bilateral traumatic amputations of the lower limb and a further four casualties sustained calcaneal injuries. However, there was no clear description of the lower limb injury pattern, nor were there any results on the outcomes of these injuries. As a result, researchers in the field have resorted to extrapolating injury profiles from studies based on automotive impact loading conditions [24,25]. Based on these cadaveric studies, current NATO guidelines stipulate that the critical injury threshold for AV-mine tests is 5.4 kN, measured in the tibia component of a Hybrid III anthropometric test device [26]. This value was determined by recording the load likely to result in a lower limb injury with an abbreviated injury score (AIS) greater than 2. The AIS scoring system was developed to score individual injuries on a scale of 1–6, based on the likelihood of the event causing a fatal injury [27]. As lower limb injuries are rarely fatal, the whole spectrum of injuries is scored between a narrow range of 1 (e.g. simple contusion) and 3 (e.g. below knee amputation), negating the resolution required to differentiate between injuries that result in poor outcomes [28].
(a). Introduction to development of models on injury
Full-vehicle blast experiments offer the most realistic simulation of AV-mine blasts. Bird [29] placed AV landmines equivalent to 10 kg of trinitrotoluene (TNT) under a series of military vehicles and mounted displacement transducers to the vehicles' floors, but unfortunately no data on deformation or velocity of deformation were reported. Owing to their nature, full-vehicle blast experiments are expensive, frequently result in instrumentation failure, show poor repeatability, have many uncontrolled variables and are always limited to small sample sizes owing to cost limitations. In addition, the reality of defence AV-mine research is that cadaveric experiments involving blast are not ethically or politically feasible. Alternative routes have therefore been sought in order to replicate the effects of blast on the vehicle occupant. Experimental and computational models of blast, as well as surrogate and computational models for the human, have been developed, driven primarily by research into commercial automotive safety. In the following paragraphs, experimental and computational approaches to model the effects of blast on skeletal injury are reviewed.
(b). Experimental models of blast injury
(i). Scaled-blast simulations
The test rig for occupant safety system (TROSS) is a vehicle floor simulant, which uses scaled detonations to provide the same blast parameters to a vehicle occupant as those occurring in an underbelly vehicle blast of 2–10 kg of TNT [26]. This has been used as a test-bed to evaluate the biofidelity of surrogates in AV-mine blast and to define input loading conditions for controlled laboratory experiments with cadavers or surrogates [30–32]. There is no scientific literature presenting cadaveric testing with TROSS.
Wang et al. [33] built an in-house rig to test the effect of a false floor on the lower limb. This used a surrogate leg mounted vertically on the floor and an under-floor explosion of 200 g of PE4 buried into 50 mm of dry sand at a stand-off of 600 mm. They found that a false floor prevented fracture of both ankle and lower tibia alike.
(ii). Traumatic injury simulators (impact rigs)
Naturally, blast tests are limited by small sample sizes owing to cost limitations and also suffer from poor repeatability and data loss through instrumentation failure. Therefore, impact rigs have been developed to look into vehicle-occupant injury that can produce repeatable data within a laboratory setting.
In the automotive industry, research aimed at studying injuries arising from frontal vehicle collisions has used pendulums, drop rigs, pneumatic rigs, hydraulic rigs and accelerated sleds [24,25,34–39]. Although these impact rigs simulate high-impulse impacts, they apply a frontal/multi-axial load at 2–6 m s−1 within 100 ms, whereas AV-mine blasts have been estimated to apply an axial load at floor-plate velocities of 7–30 m s−1 within 6–10 ms [33,40,41] (R. Bird 2009, personal communication). This discrepancy renders a number of the engineering solutions applicable to automotive research impractical for AV-mine blast research in a laboratory environment, as the resultant impulse morphology interacts with the vehicle in a different manner.
Current experimental rigs designed to simulate AV-mine blast effects on vehicle occupants operate at the lower end of the estimated floor-plate velocity range. McKay & Bir [40] mounted cadaveric lower legs to a Hybrid III pelvis and impacted the foot with a 36.7 kg plate at 7, 10 and 12 m s−1. Peak loads in the tibia of between 4.5 and 6.1 kN were measured using a load cell mounted along the tibial axis by removing 90 mm of the tibia. At 7 m s−1, there were no bone fractures observed. Calcaneal fractures were observed at 10 and 12 m s−1 in all samples; additionally, talar, ankle joint and tibial fractures occurred in some of the samples. The authors claim that these injuries are in-line with what is observed in theatre. However, removal of bone to house the load cell and use of elderly samples (the average age was 67 years) are likely to have reduced the validity of this assurance. Furthermore, the presence of footwear was not taken into account, and this has been previously shown to reduce significantly peak forces in the tibia [32,42] as well as possibly shielding the calcaneus from fracture. Wang et al. [33] used a bungee-assisted drop rig to measure the effect of a false floor on reducing the forces transmitted by an AV-mine blast through the floor to metal surrogate legs. Unfortunately, the authors did not report the velocity or energy at impact. They concluded that a false floor can protect the limb from fracture.
Both scaled-blast and traumatic injury simulators offer a means to look into injury owing to AV-mine blasts. The scaled-blast simulators may be a realistic approximation of the phenomenon as they include actual explosive detonations, but are expensive, show poor repeatability and are limited to use surrogate samples. The impact rigs may simulate realistically the effects of an AV-mine blast to the lower limb in a more controlled and repeatable manner and allow for cadaveric testing. However, input parameters (force/energy/velocity/impulse) for the operation of the impact rig have not been rigorously identified through scaled or other blast experiments. It remains unclear which variable or set-up is key in order to realistically replicate the injuries seen in theatre.
(c). Biofidelic surrogates
Owing to logistic and ethical limitations associated with cadaveric testing, biofidelic surrogates have been developed as an alternative. These have been designed to have approximate human dynamic response to collision [43]. Two types of surrogates have been used in mine-blast research; those that are multi-use (originally designed for automotive safety applications) and those that are single-use (specific for blast-related research).
(i). Multi-use surrogates
The two most widely used surrogates in the automotive industry are the Hybrid III 50th percentile male dummy and the test device for human occupant restraint (THOR) [43,44]. Horst et al. [31] claim that the Hybrid III dummy can be successfully used to measure occupant loading during an AV-mine blast. However, later experimental data suggested that the THOR-Lx (the lower extremity element of the THOR) provides more accurate correlation with cadaveric test data than the Hybrid III at low explosive loads and that there is a loss of biofidelity in both Hybrid III and THOR-Lx at higher explosive loads [30]. These findings suggest that neither of these surrogates can be used for evaluation of AV-mine blast injuries.
(ii). Single-use surrogates
Single-use surrogate lower limbs specifically designed to assess the effects of blasts include the complex lower leg (CLL) and the frangible surrogate leg (FSL) [32,45,46]. The CLL has been tested at the TROSS set-up and was claimed to show realistic injury patterns and biofidelic response under foot-plate velocities of 3.4–8.5 m s−1 [32]. The FSL has been compared with human cadaveric data in a landmine experimental set-up; the findings showed good correlation with respect to gross bony damage, but low biofidelity in soft tissue and cancellous bone [47].
The use of surrogates for experimental testing offers a means to investigate AV-mine blast without the need for cadavers; this, consequently, reduces sample variability and offers the possibility of re-use in some cases. However, there is no cadaveric data from AV-mine blast experiments against which surrogate response can be compared to enable validation of surrogate biofidelity in AV-mine blast. Hence, one must be cautious when drawing conclusions regarding injury patterns predicted by surrogates. Cadaveric testing in a controlled, repeatable manner with instrumentation and mounting that does not interfere with the biofidelity of the specimen itself may offer a suitable means of analysing injury mechanics in AV-mine blast. Still, any testing regime using surrogate or cadaveric tissue should be comprehensively compared against injury data seen in theatre.
(d). Computational models
The development of accurate, validated numerical/computational models can allow a cost-effective alternative to expensive experimental set-ups, as well as allow the simulation of multiple scenarios by altering modelling input parameters, specifically geometric, material, loading and boundary.
There is no computational study in the literature that specifically asks the question of lower limb response to high strain-rate loading owing to an AV-mine blast or similar. Nevertheless, computational modelling of the lower limb at high strain rates has historically been developed for safety in the automotive industry, often simulating pedestrian or vehicle-occupant lower limb injury. A comprehensive review of these can be found in Yang et al. [48]. All such models use explicit dynamic finite-element codes, such as Pam-Crash (ESI Group, Paris, France), Radioss (Altair Engineering Inc., MI, USA) and LS-Dyna (Livermore Software Technology Corp. CA, USA). Geometrical data are acquired from dummy data or MR and CT imaging data, but material-property data for hard and soft tissues vary significantly among studies. All use simplified material models, such as linearly elastic, linearly plastic and isotropic or transversely isotropic models, with only very few modelling viscoelastic effects in soft tissues. Importantly, the material coefficients assigned in most of the models have been derived from experimental data conducted at quasi-static strain rates. It has been shown that hard and soft tissue material behaviour is dependent upon strain rate (this is discussed in detail below) and that at least some measured outcomes of mechanical behaviour are strongly dependent upon the numerical value of material parameters [49]. This fact highlights the fundamental challenges in the development of accurate numerical models: the lack of data on material behaviour of skeletal tissues under high loading rate conditions and the difficulty of validating numerical models against relevant experimental data.
(e). Material properties of skeletal tissue
The reality is that current skeletal tissue research has been motivated by civilian injury and degenerative changes with age. Very few experiments have been conducted on bone at high strain rates. Seminal work was conducted by McElhaney [50] who tested fresh bovine and embalmed human bone samples in compression at strain rates up to 1500 s−1. He found that modulus, strength and brittleness of bone increased with strain rate, a common trend seen in high strain-rate studies. Attempts since have produced variable results. For example, Ferreira et al. [51] used a split Hopkinson bar apparatus, showing a trend of decrease in stiffness and increase in strength of bovine cortical bone up to strain rates of 1000 s−1, which contradicts the findings of McElhaney [50]. In contrast, and in agreement with the findings of McElhaney [50], Hansen et al. [52] showed a trend of increase in modulus of human cortical bone up to 30 s−1 in compression but could not explain inconsistencies of their results when compared with other studies. It is known that brittle materials are very dependent on size, geometry and initial points of weakness or defects. Sample preparation and inherent variability may explain some of the differences.
The general consensus is that above 20 s−1 bone behaves as a brittle material. Most studies show compressive strength and modulus of bone to increase with strain rate; the situation for tensile results is variable. Therefore, numerous questions on bone behaviour at high loading rates remain unanswered; the failure mechanism has not been investigated, numerical results on strength and stiffness vary significantly between studies both in trend and in numerical values alike and very little work has been performed on human samples.
Material behaviour of ligaments, tendons, articular cartilage and skin has also been shown to depend on strain rate. The compressive modulus of articular cartilage increases with strain rates up to 0.05 s−1 and is practically insensitive from then on and up to 1000 s−1 [53]. This finding is supported by others [54], and can be explained by the fact that the water content of the tissue does not have time to flow when loads are applied faster than a threshold rate. The stiffness of lapine patellar tendon has been shown to be practically insensitive to strain rate, but its strength has been shown to increase by 77 per cent from strain rates of 0.0057–12.5 s−1 [55]. Lapine ligament material properties have been shown to increase by up to 40 per cent when tested from strain rates of 0.0001–2 s−1 [56]. Furthermore, failure properties of human cervical spine ligaments tested at strain rates of 150 s−1 were up to five times greater than when tested at approximately 0.05 s−1 [57]. Most recently, the tensile modulus of porcine skin has been shown to increase with strain rate up to 0.1 s−1 and decrease with temperature [58].
Despite the variability in outcome of the various studies reported in the literature, it is clear that the material behaviour of most skeletal tissue depends on the loading rate it is subjected to, at least up to some threshold; it is unknown what happens at much higher rates. In order to better understand the injury patterns caused at loading rates seen in AV-mine blasts and provide input data for computational modelling, tissue testing at velocities of at least 15 m s−1 needs to be conducted; this might correspond to strain rates of up to 10 000 s−1. Traumatic injury simulators that are developed for whole limbs might conceivably be modified for testing human tissue rigorously at strain rates seen in AV-mine blasts.
(f). Cellular and molecular properties
Little is known about how the cellular and molecular properties of skeletal tissue are altered in response to shock waves at magnitudes that correspond to conditions that would result in a blast injury. However, there is a considerable body of literature on the use of low-energy shock waves in extracorporeal shock wave therapy (ESWT) in orthopaedic applications (see reviews by [59,60]), but the magnitude of therapeutic shock waves is reduced by approximately six orders of magnitude [61]. A range of biological changes have been observed at a molecular level using animal models and cells that indicate a key effect of ESWT is to stimulate osteogenesis through signalling processes and/or growth factor production [60]. For example, studies of human osteoblasts stimulated with therapeutic-level shock waves demonstrated alterations in the regulation of genes involved in cellular proliferation and differentiation [62]. Increasing the energy above treatment thresholds, but still many orders of magnitude below blast conditions, can result in bone fractures with accompanying damage to periosteal soft tissue and the bone marrow cavity [63,64]. Damage to vascular and nerve tissues is among the known complications associated with ESWT (reviewed in [59]). The molecular basis for this damage, however, remains largely uncharacterized.
With the advent of genomic methods, there is considerable scope for developing an understanding of the cellular and molecular changes that are associated with blast injuries. Cobb & O'Keefe [65] have discussed some limitations in our understanding of the biological and physiological effects of the systemic and localized effects that arise in response to traumatic injury, including the paradox of balancing pro- and anti-inflammatory responses. In addition, they point out the potential of using genomic methods including transcriptomic and proteomic analyses, as a means of providing new genome-wide information that can be used to advance treatments and improve the prognosis of those suffering severe injuries. Research in the area of blast traumatic brain injury has already expanded to include proteomics [66] and identification of biomarker candidates [67] that can be used to profile damage-induced molecular and cellular changes. Recent examples that use reverse transcription–polymerase chain reaction studies to follow fracture healing in mice [68] or the effects of low-energy shock waves upon osteoblasts [69] demonstrate that genomic methods are being used to follow biomarker profiles in bone damage and repair processes. The potential to use similar methodologies to study blast-damaged skeletal tissue at a cellular and molecular level is evident, but is also highly dependent upon the availability of physiologically meaningful experimental models.
5. Future research foci
The signature weapon of current peace support operations, and efforts to mitigate against fatality, has increased the burden of management of long-term clinical sequelae of extremity injury. Indeed, the character of this injury has become more apparent in recent times despite descriptions in every conflict of the twentieth century. It is the multi-modal mechanism through which blast injuries are caused that drives the development of complex clinical paradigms in its management; the in-vehicle blast scenario, however, arguably acts to limit those injury mechanisms to a system that can potentially be modelled in a laboratory in order to develop evidence-based clinical management.
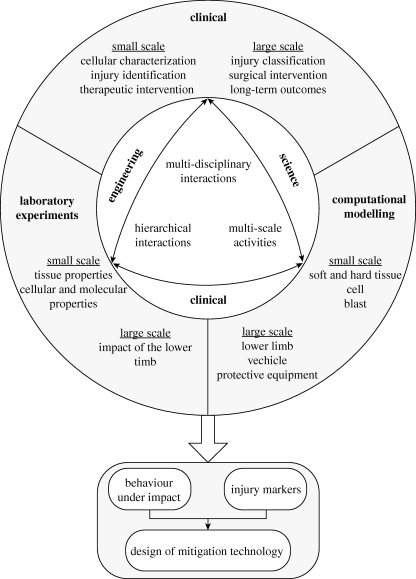
The approach required to unravel complex injury types and develop effective therapeutic options in the necessarily short timeframe associated with military research requires an ontological interaction between disparate schools of thought. Linking molecular and cellular events with physiological dysfunction will ultimately require an effective system of continuum modelling, from genome to proteome to cellular interactions, with a universal markup language. However, while these technologies develop, the opportunities to investigate and intervene at individual levels of the continuum are plentiful.
In order to determine reliable markers of injury, simulate the behaviour of tissue under impact and guide the development of mitigation technologies, an understanding of the clinical reality of current operations is required (figure 6). As such, there exists an urgent requirement to develop a comprehensive trauma database of extremity injuries from vehicle explosions in order to fully understand the injury profile of casualties and their long-term clinical sequelae. Using prospectively collected military trauma databases, such as the UK Joint Theatre Trauma Registry [70], and combining these with radiological data and clinical outcomes, it will be possible to deconstruct complex lower limb injuries into component elements, thereby enabling injury characterization and prognostication. This ongoing research will provide the foundations of future modelling work; representative experimental design will allow validation of computational models, ensuring that simulation research remains focused on the injury patterns managed in current and future theatres of operation.
Figure 6.
Research strategy for lower limb blast injury.
We believe that a collaborative approach between clinicians, natural scientists and engineers, combining physical and numerical modelling tools with experimentally derived data from models of blast injury, can form the basis in mitigating the injury burden suffered by the combat casualty. Not only are the opportunities great at present, but in the medium term these opportunities will develop apace.
Footnotes
One contribution of 20 to a Theme Issue ‘Military medicine in the 21st century: pushing the boundaries of combat casualty care’.
References
- 1.Toy S. 1955. A history of fortification from 3000 BC to AD 1700. London, UK: Heinemann [Google Scholar]
- 2.Guderian H. W. 1937. ‘Achtung-Panzer!’ Die Entwicklung der panzerwaffe, ihre kampftaktik und ihre operativen maglichkeiten. Stuttgart, Germany: Arms and Armor Press [Google Scholar]
- 3.Tremblay J. E., Bergeron D. M., Gonzalez R. 1998. Key technical activity 1–29: protection of soft-skinned vehicle occupants from landmine effects. In Technical cooperation program. Val-Belair, Canada: Defence Research Establishment Valcartier [Google Scholar]
- 4.Boyd N. A. 1975. A military surgical team in Belfast. Ann. R. Coll. Surg. Engl. 56, 15–25 [PMC free article] [PubMed] [Google Scholar]
- 5.Melsom M. A., Farrar M. D., Volkers R. C. 1975. Battle casualties. Ann. R. Coll. Surg. Engl. 56, 289–303 [PMC free article] [PubMed] [Google Scholar]
- 6.Palinkas L. A., Cohen P. 1985. Combat casualties among US Marine Corps personnel in Vietnam: 1964–1972. San Diego, CA: Naval Health Research Centre [Google Scholar]
- 7.Owens B. D., Kragh J. F., Jr, Macaitis J., Svoboda S. J., Wenke J. C. 2007. Characterization of extremity wounds in operation Iraqi freedom and operation enduring freedom. J. Orthop. Trauma 21, 254–257 (doi:10.1097/BOT.0b013e31802f78fb) [DOI] [PubMed] [Google Scholar]
- 8.Ramasamy A., Harrisson S. E., Clasper J. C., Stewart M. P. M. 2008. Injuries from roadside improvised explosive devices. J. Trauma 65, 910–914 (doi:10.1097/TA.0b013e3181848cf6) [DOI] [PubMed] [Google Scholar]
- 9.Ramasamy A., Harrisson S. E., Stewart M. P., Midwinter M. J. 2009. Penetrating missile injuries during the Iraqi insurgency. Ann. R. Coll. Surg. Engl. 91, 551–558 (doi:10.1308/003588409X464720) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramasamy A., Hill A. M., Clasper J. C. 2009. Improvised explosive devices: pathophysiology, injuries and management. J. R. Army Med. Corps 155, 265–274 [DOI] [PubMed] [Google Scholar]
- 11.Mazurek M. T., Ficke J. R. 2006. The scope of wounds encountered in casualties from the global war on terrorism: from the battlefield to the tertiary treatment facility. J. Am. Acad. Orthop. Surg. 14, S18–S23 [DOI] [PubMed] [Google Scholar]
- 12.Owens B. D., Kragh J. F., Jr, Wenke J. C., Macaitis J., Wade C. E., Holcomb J. B. 2008. Combat wounds in operation Iraqi Freedom and operation enduring freedom. J. Trauma 64, 295–299 (doi:10.1097/TA.0b013e318163b875) [DOI] [PubMed] [Google Scholar]
- 13.Ramasamy A., Harrisson S., Lasrado I., Stewart M. P. 2009. A review of casualties during the Iraqi insurgency 2006—a British field hospital experience. Injury 40, 493–497 (doi:10.1016/j.injury.2008.03.028) [DOI] [PubMed] [Google Scholar]
- 14.Ramasamy A., Hinsley D. E., Edwards D. S., Stewart M. P., Midwinter M. J., Parker P. J. 2010. Skillsets and competencies for the modern military surgeon: lessons from UK militrary operations in southern Afghanistan. Injury 41, 453–459 (doi:10.1016/j.injury.2009.11.012) [DOI] [PubMed] [Google Scholar]
- 15.Baker W. 1983. Explosion hazards and evaluation. Amsterdam, The Netherlands: Elsevier [Google Scholar]
- 16.Grujicic M., Pandurangan B., Zhao C. L., Cheeseman B. A. 2007. A computational investigation of various water-induced explosion mitigation mechanisms. Multidiscip. Model. Mater. Struct. 3, 185–212 (doi:10.1163/157361107780744405) [Google Scholar]
- 17.Grujicic M., Pandurangan B., Haque I., Cheeseman B. A., Roy W. N., Skaggs R. R. 2007. Computations analysis of mine blast on a commercial vehicle structure. Multidiscip. Model. Mater. Struc. 3, 431–460 (doi:10.1163/157361107782106348) [Google Scholar]
- 18.Bowen I. G., Fletcher E. R., Richmond D. R. 1968. Estimate of man's tolerance to the direct effects of air blast. Washington, DC: Headquarters Defence Atomic Support Agency [Google Scholar]
- 19.DePalma R. G., Burris D. G., Champion H. R., Hodgson M. J. 2005. Blast injuries. N. Engl. J. Med. 352, 1335–1342 (doi:10.1056/NEJMra042083) [DOI] [PubMed] [Google Scholar]
- 20.Zuckerman S. 1952. Vulnerability of human targets to fragmenting and blast weapons. In Textbook of air armament (ed. Zuckerman S.), pp. 1–243 London, UK: HMSO [Google Scholar]
- 21.Ramasamy A., Hill A. M., Hepper A. E., Bull A. M. J., Clasper J. C. 2009. Blast mines: a background for clinicians on physics, injury mechanisms and vehicle protection. J. R. Army Med. Corps 155, 258–264 [DOI] [PubMed] [Google Scholar]
- 22.Ramasamy A., Hill A. M., Masouros S. D., Mountain A., Gibb I., Bull A. M. J., Clasper J. C. 2009. Explosion-mediated fracture patterns relate to environment: a forensic biomechanical approach. Honolulu, HI: Society of Military Orthopaedic Surgeons [Google Scholar]
- 23.Radonic V., Giunio L., Biocic M., Tripkovic A., Lukcic B., Primorac D. 2004. Injuries from Antitank mines in southern Croatia. Mil. Med. 169, 320–324 [DOI] [PubMed] [Google Scholar]
- 24.Funk J. R., Crandall J. R., Tourret L. J., MacMahon C. B., Bass C. R., Patrie J. T., Khaewpong N., Eppinger R. H. 2002. The axial injury tolerance of the human foot/ankle complex and the effect of Achilles tension. J. Biomech. Eng. 124, 750–757 (doi:10.1115/1.1514675) [DOI] [PubMed] [Google Scholar]
- 25.Yoganandan N. 1996. Dynamic axial tolerance of the human footankle complex. Albuquerque, NM: Society of Automotive Engineers; 40th Stapp Car Crash Conf [Google Scholar]
- 26.NATO 2007. Test methodology for protection of vehicle occupants against anti-vehicular landmine effects. TR-HFM-090, NATO, Rijswijk, The Netherlands [Google Scholar]
- 27.Baker S. P., O'Neill B., Haddon W., Long W. B. 1974. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J. Trauma 14, 187–196 (doi:10.1097/00005373-197403000-00001) [PubMed] [Google Scholar]
- 28.Manoli A., Prasad P., Levine R. S. 1997. Foot and ankle severity scale (FASS). Foot Ankle Int. 18, 598–602 [DOI] [PubMed] [Google Scholar]
- 29.Bird R. 2001. Protection of vehicles against landmines. J. Battlefield Tech. 4, 14–17 [Google Scholar]
- 30.Bir C., Barbir A., Dosquet F., Wilhelm M., van der Horst M., Wolfe G. 2008. Validation of lower limb surrogates as injury assessment tools in floor impacts due to anti-vehicular land mines. Mil. Med. 173, 1180–1184 [DOI] [PubMed] [Google Scholar]
- 31.Horst M. J., Simms C. K., Maasdam R. V. 2005. Occupant lower leg injury assessment in landmine detonations under a vehicle. In Proc. IUTAM Symp. Impact Biomechanics: from Fundamental Insights to Applications, Dublin, Ireland pp. 41–49 Amsterdam, The Netherlands: Springer [Google Scholar]
- 32.Manseau J., Keown M. 2005. Development of an assessment methodology for lower leg injuries resulting from anti-vehicular blast landmines. IUTAM Proc. Impact Biomechanics: from Fundamental Insights to Applications Dublin, Ireland (eds Gladwell G. M. L., Gilchrist M. D.), pp. 33–40 Amsterdam, The Netherlands: Springer [Google Scholar]
- 33.Wang J. J., Bird R., Swinton B., Krstic A. 2001. Protection of lower limbs against floor impact in army vehicles experiencing landmine explosion. J. Battlefield Tech. 4, 11–15 [Google Scholar]
- 34.Bass C. R. 1997. A system for simulating structural intrusion in automobile full-frontal and frontal-offset crashes in the laboratory sled test environment. PI Mech. Eng. D-J Aut. 211, 325–336 (doi:10.1243/0954407971526470) [Google Scholar]
- 35.McMaster J., Parry M., Wallace W. A., Wheeler L., Owen C., Lowne R., Oakley C., Roberts A. K. 2000. Biomechanics of ankle and hindfoot injuries in dynamic axial loading. Stapp Car Crash J. 44, 357–377 [DOI] [PubMed] [Google Scholar]
- 36.Pilkey W. D., Sieveka E. M., Crandall J. R., Klopp G. 1994. The influence of foot placement and vehicular intrusion on occupant lower limb injury in full frontal and frontal offset crashes. Proceedings of the 14th International Technical Conference on Enhanced Safety Vehicles, Munich, Germany, pp. 734–741 [Google Scholar]
- 37.Seipel R. C., Pintar F. A., Yoganandan N., Boynton M. D. 2001. Biomechanics of calcaneal fractures: a model for the motor vehicle. Clin. Orthop. Relat. Res. 388, 218–224 (doi:10.1097/00003086-200107000-00030) [PubMed] [Google Scholar]
- 38.Yoganandan N., Pintar F. A., Kumaresan S., Boynton M. 1997. Axial impact biomechanics of the human foot–ankle complex. J. Biomech. Eng. 119, 433–437 (doi:10.1115/1.2798290) [DOI] [PubMed] [Google Scholar]
- 39.Yoganandan N., Pintar F. A., Seipel R. C. 2000. Experimental production of extra- and intra-articular fractures of the os calcis. J. Biomech. 33, 745–749 (doi:10.1016/S0021-9290(00)00017-8) [DOI] [PubMed] [Google Scholar]
- 40.McKay B. J., Bir C. A. 2009. Lower extremity injury criteria for evaluating military vehicle occupant injury in underbelly blast events. Stapp Car Crash J. 53, 229–249 [DOI] [PubMed] [Google Scholar]
- 41.Williams K., Gourdeau F. F. 2002. Numerical simulation of light armored vehicle occupant vulnerability to anti-vehicle mine blast. 7th Int. LS-DYNA Users Conf. Dearborn, MI [Google Scholar]
- 42.Geurts J., van der Horst M. J., Leerdam P.-J., Bir C., van Dommelen H., Wismans J. 2006. Occupant safety: mine detonation under vehicles a numerical lower leg injury assessment. Proceedings of International Conference of Biomechanics Impact, Madrid, Spain, pp. 373–376 [Google Scholar]
- 43.Mertz H. J. 2002. Anthropometric test devices. Accidental injury biomechanics and prevention (eds Nahum A. M., Melvin J. W.), pp. 89–102 New York, NY: Springer-Verlag [Google Scholar]
- 44.Backaitis S., Mertz H., Harold J. 1993. Hybrid III: the first human-like crash test dummy. Warrendale, PA: Society of Automotive Engineers [Google Scholar]
- 45.Bergeron D. M., Coley G. G., Fall R. W. 2006. Assessment of lower leg injury from land mine blast—phase 1. Valcartier, Canada: Defence Research and Development Canada [Google Scholar]
- 46.Cronin D. S., Salisbury C., Worswick M. J., Pick R. J., Williams K. V., Bourget D. 2001. Appropriate material selection for surrogate leg models subjected to blast loading. In Fundamental issues and applications of shock-wave and high strain rate phenomena (eds Staudhammer K. P., Murr L. E., Meyers M. A.), pp. 201–208 Amsterdam, The Netherlands: Elsevier [Google Scholar]
- 47.Bergeron D. M., Coley G. G., Rountree M. S., Anderson I. B., Harris R. M. 2001. Assessment of foot protection against anti-personnel landmine blast using a frangible surrogate leg. In UXO Forum, New Orleans, LA. [Google Scholar]
- 48.Yang K., Hu J., White N., King A., Chou C., Prasad P. 2006. Development of numerical models for injury biomechanics research: a review of 50 years of publications in the Stapp car crash conference. Stapp Car Crash J. 50, 429–490 [DOI] [PubMed] [Google Scholar]
- 49.Beillas P., Lee S. W., Tashman S., Yang K. H. 2007. Sensitivity of the tibio-femoral response to finite element modeling parameters. Comput. Meth. Prog. Biol. 10, 209–221 [DOI] [PubMed] [Google Scholar]
- 50.McElhaney J. H. 1966. Dynamic response of bone and muscle tissue. J. Appl. Physiol. 21, 1231–1236 [DOI] [PubMed] [Google Scholar]
- 51.Ferreira F., Vaz M. A., Simoes J. A. 2006. Mechanical properties of bovine cortical bone at high strain rate. Mater. Charact. 57, 71–79 (doi:10.1016/j.matchar.2005.11.023) [Google Scholar]
- 52.Hansen U., Zioupos P., Simpson R., Currey J. D., Hynd D. 2008. The effect of strain rate on the mechanical properties of human cortical bone. J. Biomech. Eng. 130, 011011 (doi:10.1115/1.2838032) [DOI] [PubMed] [Google Scholar]
- 53.Oloyede A., Flachsmann R., Broom N. D. 1992. The dramatic influence of loading velocity on the compressive response of articular cartilage. Connect. Tissue Res. 27, 211–224 (doi:10.3109/03008209209006997) [DOI] [PubMed] [Google Scholar]
- 54.Shepherd D. E., Seedhom B. B. 1997. A technique for measuring the compressive modulus of articular cartilage under physiological loading rates with preliminary results. PI Mech. Eng. D-J Aut. 211, 155–165 (doi:10.1243/0954411971534278) [DOI] [PubMed] [Google Scholar]
- 55.Yamamoto N., Hayashi K. 1998. Mechanical properties of rabbit patellar tendon at high strain rate. Biomed. Mater. Eng. 8, 83–90 [PubMed] [Google Scholar]
- 56.Woo S. L. Y., Peterson R. H., Ohland K. J., Sites T. J., Danto M. I. 1990. The effects of strain rate on the properties of the medial collateral ligament in skeletally immature and mature rabbits: a biomechanical and histological study. J. Orthop. Res. 8, 712–721 (doi:10.1002/jor.1100080513) [DOI] [PubMed] [Google Scholar]
- 57.Bass C. R., Lucas S. R., Salzar R. S., Oyen M. L., Planchak C., Shender B. S., Paskoff G. 2007. Failure properties of cervical spinal ligaments under fast strain rate deformations. Spine 32, E7–E13 (doi:10.1097/01.brs.0000251058.53905.eb) [DOI] [PubMed] [Google Scholar]
- 58.Zhou B., Xu F., Chen C. Q., Lu T. J. 2010. Strain rate sensitivity of skin tissue under thermomechanical loading. Phil. Trans. R. Soc. A 368, 679–690 (doi:10.1098/rsta.2009.0238) [DOI] [PubMed] [Google Scholar]
- 59.McClure S. R., Van Sickle D., White M. R. 2004. Effects of extracorporeal shock wave therapy on bone. Vet. Surg. 33, 40–48 (doi:10.1111/j.1532-950x.2004.04013.x) [DOI] [PubMed] [Google Scholar]
- 60.Zelle B. A., Gollwitzer H., Zlowodzki M., Bühren V. 2010. Extracorporeal shock wave therapy: current evidence. J. Orthop. Trauma 24, S66–S70 (doi:10.1097/BOT.0b013e3181cad510) [DOI] [PubMed] [Google Scholar]
- 61.Ogden J. A., Alvarez R. G., Levitt R., Marlow M. 2001. Shock wave therapy (orthotripsy (R)) in musculoskeletal disorders. Clin. Orthop. Relat. Res. 387, 22–40 (doi:10.1097/00003086-200106000-00005) [DOI] [PubMed] [Google Scholar]
- 62.Hofmann A., Ritz U., Hessmann M. H., Alini M., Rommens P. M., Rompe D. 2008. Extracorporeal shock wave-mediated changes in proliferation, differentiation, and gene expression of human osteoblasts. J. Trauma 65, 1402–1410 (doi:10.1097/TA.0b013e318173e7c2) [DOI] [PubMed] [Google Scholar]
- 63.Maier M., et al. 2002. Influence of extracorporeal shock-wave application on normal bone in an animal model in vivo: scintigraphy, MRI and histopathology. J. Bone Joint Surg. (Br) 84-B, 592–599 [DOI] [PubMed] [Google Scholar]
- 64.Valchanou V. D., Michailov P. 1991. High energy shock waves in the treatment of delayed and nonunion of fractures. Int. Orthop. 15, 181–184 [DOI] [PubMed] [Google Scholar]
- 65.Cobb J. P., O'Keefe G. E. 2004. Injury research in the genomic era. Lancet 363, 2076–2083 (doi:10.1016/S0140-6736(04)16460-X) [DOI] [PubMed] [Google Scholar]
- 66.Agoston D. V., Gyorgy A., Eidelman O., Pollard H. B. 2009. Proteomic biomarkers for blast neurotrauma: targeting cerebral edema, inflammation, and neuronal death cascades. J. Neurotrauma 26, 901–911 (doi:10.1089/neu.2008.0724) [DOI] [PubMed] [Google Scholar]
- 67.Svetlov S. I., Larner S. F., Kirk D. R., Atkinson J., Hayes R. L., Wang K. K. 2009. Biomarkers of blast-induced neurotrauma: profiling molecular and cellular mechanisms of blast brain injury. J. Neurotrauma 26, 913–921 (doi:10.1089/neu.2008.0609) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Dean D. B., Watson J. T., Jin W., Peters C., Enders J. T., Chen A., Moed B. R., Zhang Z. 2010. Distinct functionalities of bone morphogenetic protein antagonists during fracture healing in mice. J. Anat. 216, 625–630 (doi:10.1111/j.1469-7580.2010.01214.x) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Muzio G., et al. In press Shock waves induce activity of human osteoblast-like cells in bioactive scaffolds. J. Trauma. 68, 1439–1444 [DOI] [PubMed] [Google Scholar]
- 70.Smith J., Hodgetts T. J., Mahoney P., Russell R., Davies S., McLeod J. 2007. Trauma governance in the UK defence medical services. J. R. Army Med. Corps 153, 239–242 [DOI] [PubMed] [Google Scholar]
- 71.Hull J. B. 1992. Traumatic amputation by explosive blast: pattern of injury in survivors. Br. J. Surg. 79, 1303–1306 (doi:10.1002/bjs.1800791220) [DOI] [PubMed] [Google Scholar]
- 72.Hull J. B., Cooper G. J. 1996. Pattern and mechanism of traumatic amputation by explosive blast. J. Trauma 40, S198–S205 (doi:10.1097/00005373-199603001-00044) [DOI] [PubMed] [Google Scholar]
- 73.Huelke D. F., Buege L. J., Harger J. H. 1967. Bone fractures produced by high velocity impacts. Am. J. Anat. 120, 123–132 (doi:10.1002/aja.1001200110) [Google Scholar]
- 74.Nechaev E. A., Gritsanov A. I., Fomin N. F., Minnullin I. P. 1984. Mine blast trauma. St Petersberg, Russia: Russian Federation, Ministry of Public Health and Medical Industry [Google Scholar]