Abstract
Blast injuries are becoming increasingly common in military conflicts as the nature of combat changes from conventional to asymmetrical warfare and counter-insurgency. This article describes a retrospective database review of cases from the UK joint theatre trauma registry from 2003 to 2009, containing details of over 3000 patients, mainly injured in Iraq and Afghanistan. During this period, 1678 patients were injured by explosion of whom 113 had evidence of blast lung injury. Of the 50 patients who survived to reach a medical facility, 80 per cent required ventilatory support. Injuries caused by explosion are increasing when compared with those caused by other mechanisms, and blast lung represents a significant clinical problem in a deployed military setting. Management of these patients should be optimized from point of wounding to definitive care.
Keywords: blast injuries, explosions, lung injury, adult respiratory distress syndrome
1. Introduction
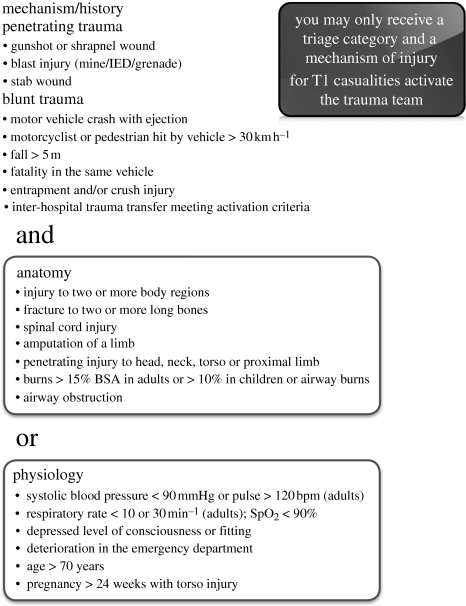
Since April 2003, the UK armed forces have been deployed overseas in combat operations with field hospital medical support. Data on all seriously injured patients (including UK military, coalition forces, detainees and local civilians) treated by UK Defence Medical Services in these facilities are collected by the deployed clinical team and returned to the UK Joint Theatre Trauma Registry (JTTR), maintained by the Academic Department of Military Emergency Medicine (ADMEM) at the Royal Centre for Defence Medicine (RCDM) in Birmingham. Data are prospectively collected from clinical notes, trauma charts and, in the case of death, post-mortem findings. The JTTR holds continuous data on this cohort from 2003, coinciding with the start of hostilities in Iraq. Returns are electronic (where deployed IT systems allow), with hard copy accompanying UK military patients evacuated to RCDM for definitive care. The default entry criterion for the UK JTTR is a casualty who triggers trauma team activation in a deployed field hospital or Primary Casualty Receiving Facility afloat. Trauma team activation criteria are described in figure 1. The entry criteria were expanded in 2007 to include all trauma patients returned to RCDM for definitive treatment, irrespective of whether a trauma team response was mandated.
Figure 1.
Trauma team activation criteria (extract from Clinical Guidelines for Operations, Joint Service Publication 4-03.1). BSA, body surface area.
Primary blast injuries result from the effects of the shock wave of an explosion, which travels through the tissues depositing energy particularly where there is a gas–liquid interface. Because of their air-filled alveoli and delicate vascular structure, the lungs are particularly vulnerable to this form of injury, the consequences of which are termed blast lung. The incidence and extent of primary blast injury depends on both the level of peak overpressure experienced and the duration of exposure. The magnitude of the peak overpressure diminishes exponentially (by an inverse cube relationship) with distance from the centre of the explosion, while fragments retain lethal energy for much greater distances. Consequently, in an open environment secondary injuries from fragments represent the principal mechanism of injury in the majority of casualties. However, with increasing effectiveness of body armour to protect against fragments, casualties can survive closer to the source of the explosion and hence are more likely to suffer primary blast injury.
Injury patterns have changed during the conflicts in which we have been engaged. Hostile forces have changed their tactics, from direct confrontation to guerrilla style warfare and ambush with an increase in the use of improvised explosive devices (IEDs) and mines. There has been evidence from previous studies that the ratio of gun shot wounds to wounds caused by explosion (blast injuries) has been steadily reducing [1–5].
The aim of this study was to establish the epidemiology of blast injuries since the onset of hostilities in 2003 among patients presenting to UK field hospitals, and within the group injured as a result of explosion to establish the incidence of blast lung.
2. Methods
A retrospective database review was performed, using the JTTR database from 1 January 2003 to 1 October 2009. Inclusion criteria included all trauma patients in the JTTR from 1 January 2003 to 1 October 2009. This included UK military, coalition military, civilians and local security forces. Exclusion criteria were disease (non-injury) classifications.
From the overall database, filters were applied to limit the search to only those injured by explosive blast, then those with evidence of thoracic injury from blast. Finally, the search was limited to those with injury coding (using AIS 2005 military) of blast lung or pulmonary contusion caused by blast. All cases in the subsequent group were examined individually to ascertain if they had pulmonary blast injury. All thoracic injury categories were examined for relevant cases, but those with an obvious alternative cause for their thoracic injuries, such as penetrating cardiac wounds, were excluded from the analysis.
Limits to the database search were applied sequentially:
— mechanism—explosion
— thoracic injury
— coded for blast lung or pulmonary contusion.
3. Results
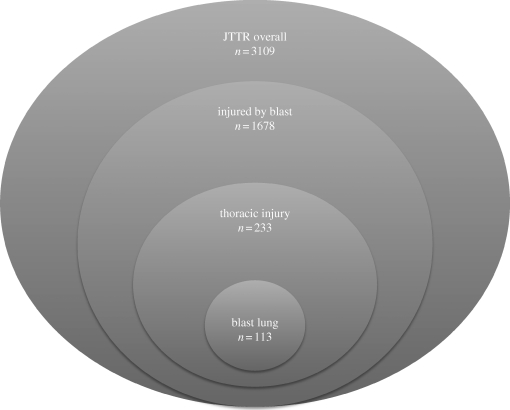
Overall during the study period there were 3109 cases in the JTTR, of whom 1678 suffered injuries as a result of an explosion. Of this group, 233 patients sustained thoracic injuries as a result of blast injury, and when the search was further limited to those coded as blast lung or pulmonary contusion the final study group was made up of 113 cases (figure 2). The mean injury severity score (ISS) of this group was 52.6, with 92 per cent of cases having an ISS greater than 15 (95% of cases had a new injury severity score (NISS) greater than 15).
Figure 2.
Breakdown of number of cases.
The number of cases of major trauma presenting to UK military hospitals rose during the study period, with peaks in Iraq in 2007 and in Afghanistan in 2009.
Fifty (44%) of these cases survived to reach a medical facility but 12 (24%) of the initial survivors died of their wounds.
Fourteen patients had evidence of severe hypoxia (oxygen saturation less than 92%) on arrival at a medical facility suggesting significant respiratory compromise early in the pre-hospital phase of their blast injury.
Of the 50 patients surviving to medical support, eight (16%) underwent rapid sequence induction of anaesthesia and intubation (RSI) pre-hospital (performed by the medical emergency response team, MERT), 25 (50%) underwent RSI in the emergency department (ED), seven (14%) were intubated and ventilated in the operating theatre and 10 (20%) did not require ventilatory support. The majority of those undergoing RSI and ventilation underwent surgery and were subsequently transferred for ongoing respiratory support to the intensive care unit (ICU). Many of these patients required surgery for other injuries sustained from secondary fragmentation injuries, particularly limb injuries.
4. Discussion
This study highlights that injuries caused by explosion, and in particular blast lung, are an increasing problem for UK forces deployed overseas on military operations. There is a substantial fatality rate among those subjected to blast injury, which has led to calls for a review of the management of such patients and optimization of their treatment from point of wounding to critical care. This study indicates that blast injuries, and blast lung in particular, are proving to be a significant clinical issue for deployed UK field hospitals during the current conflict. By far the commonest cause of these explosions was the IED, which is being used more frequently by insurgents in Afghanistan in particular.
A comparison of cases from Iraq and Afghanistan shows that there were peaks of injuries caused by explosion in Iraq in 2007, and Afghanistan in 2009. The incidence of blast lung during the Iraq peak was 7.3 per cent. This figure is slightly higher than that quoted in a series of patients injured by explosions on recent US military operations, which showed an increase in the incidence of blast lung between 2003 and 2006 [6,7].
The incidence of injuries consistent with blast lung during the Afghanistan peak was found to be 11 per cent, showing an increase (from 7.3% in Iraq) although this was not statistically significant (p = 0.31, Chi-squared test); this was twice that reported in a previous series [7]. Although it is impossible to ascribe a reason for this change, it is clear that the clinical burden is increasing, and that treatment strategies need to take this into account.
Following an explosion, the blast wave causes immediate lung injury, characterized by rupture of alveolar capillaries and subsequent intrapulmonary haemorrhage and oedema, similar to pulmonary contusion from blunt chest trauma [8,9]. The presence of free blood and haemoglobin in the alveoli leads to the formation of free radicals, oedema and an augmented early inflammatory response. This in turn leads to leucocyte accumulation and subsequently epithelial cell damage (at 12–24 h), endothelial cell damage (24–56 h) and the late oedema typical of adult respiratory distress syndrome (ARDS). Histological examination reveals prominent perivascular oedema and extensive alveolar haemorrhage during the first 12 h, and thereafter, epithelial cell damage with detachment from the basement membrane [10]. The extent of lung damage is related to the magnitude of the blast exposure, with effects ranging from sub-clinical microscopic petechiae to large areas of confluent frank haemorrhage.
Other pulmonary effects include pneumothorax or haemothorax (or a combination), which may occur due to the shearing force of the primary blast injury causing damage to the peripheral alveoli (causing pneumothorax) and pulmonary vessels (causing haemothorax). These complications may also be related to secondary or tertiary blast injury.
The clinical features of primary blast lung injury are shortness of breath, cough, haemoptysis, cyanosis and tachypnoea. Hypoxia is a universal finding, although this may develop later over the first few hours following injury, and may not be evident initially, as demonstrated by our findings that only 28 per cent had hypoxia at initial presentation.
Management of patients with blast lung is in the main supportive, with limited scope for mediation of symptoms caused by pulmonary haemorrhage. If patients survive the initial phase of injury, outcome has been reported as good, with 76 per cent of patients in one study reporting no symptoms at follow-up telephone interview [11]. Novel strategies for the management of blast lung are needed if these patients, who as demonstrated are becoming increasingly common in deployed medical units, are to be treated optimally.
Limitations of this study are evident from the method of data collection, and the problems with the definition of blast lung. The JTTR only captures those patients who have data submitted from the field hospitals, or who have post-mortem data from repatriation and coroners' post-mortem findings in the UK. No data are collected on civilians or other non-UK patients who die at scene or in the pre-hospital stages of their resuscitation, as post-mortem examination is not routinely carried out on this group of patients.
5. Conclusion
Blast injuries are an increasingly prevalent cause of considerable morbidity and mortality, particularly (although not exclusively) in the forward military environment. The sequelae of such injuries are being felt not only in Iraq and Afghanistan, but also in the hospitals in the UK that receive such patients through the evacuation chain. Priority should be given to optimizing management of these patients.
Acknowledgements
Many thanks to Dr Emrys Kirkman for his advice and guidance during the preparation of this manuscript.
Footnotes
One contribution of 20 to a Theme Issue ‘Military medicine in the 21st century: pushing the boundaries of combat casualty care’.
References
- 1.Hodgetts T., et al. 2007. Operational mortality of UK service personnel in Iraq and Afghanistan: a one year analysis 2006–7. J. R. Army Med. Corps 153, 252–254 [DOI] [PubMed] [Google Scholar]
- 2.Montgomery S. P., Swiecki C. W., Shriver C. D. 2005. The evaluation of casualties from Operation Iraqi Freedom on return to the continental United States from March to June 2003. J. Am. Coll. Surg. 201, 7–12 10.1016/j.jamcollsurg.2005.03.038 (doi:10.1016/j.jamcollsurg.2005.03.038) [DOI] [PubMed] [Google Scholar]
- 3.Nelson T. J., Wall D. B., Stedje-Larsen E. T., Clark R. T., Chambers L. W., Bohman H. R. 2006. Predictors of mortality in close proximity blast injuries during Operation Iraqi Freedom. J. Am. Coll. Surg. 202, 418–422 10.1016/j.jamcollsurg.2005.11.011 (doi:10.1016/j.jamcollsurg.2005.11.011) [DOI] [PubMed] [Google Scholar]
- 4.Plotkin A. J., Wade C. E., Jenkins D. H., Smith K. A., Noe J. C., Park M. S., Perkins J. G., Holcomb J. B. 2008. A reduction in clot formation rate and strength assessed by thrombelastography is indicative of transfusion requirements in patients with penetrating injuries. J. Trauma 64(Suppl. 2), S64–S68 10.1097/TA.0b013e318160772d (doi:10.1097/TA.0b013e318160772d) [DOI] [PubMed] [Google Scholar]
- 5.Rush R. M., Jr, Stockmaster N. R., Stinger H. K., Arrington E. D., Devine J. G., Atteberry L., Starnes B. W., Place R. J. 2005. Supporting the Global War on Terror: a tale of two campaigns featuring the 250th Forward Surgical Team (Airborne). Am. J. Surg. 189, 564–570 10.1016/j.amjsurg.2005.01.035 (doi:10.1016/j.amjsurg.2005.01.035) [DOI] [PubMed] [Google Scholar]
- 6.Champion H. R., Holcomb J. B., Young L. A. 2009. Injuries from explosions: physics, biophysics, pathology, and required research focus. J. Trauma 66, 1468–1477 10.1097/TA.0b013e3181a27e7f (doi:10.1097/TA.0b013e3181a27e7f) [DOI] [PubMed] [Google Scholar]
- 7.Ritenour A. E., Blackbourne L. H., Kelly J. F., McLaughlin D. F., Pearse L. A., Holcomb J. B., Wade C. E. 2010. Incidence of primary blast injury in US military overseas contingency operations: a retrospective study. Ann. Surg. 251, 1140–1144 10.1097/SLA.0b013e3181e01270 (doi:10.1097/SLA.0b013e3181e01270) [DOI] [PubMed] [Google Scholar]
- 8.Brown R. F., Cooper G. J., Maynard R. L. 1993. The ultrastructure of rat lung following acute primary blast injury. Int. J. Exp. Pathol. 74, 151–162 [PMC free article] [PubMed] [Google Scholar]
- 9.Gorbunov N. V., Elsayed N. M., Kisin E. R., Kozlov A. V., Kagan V. E. 1997. Air blast-induced pulmonary oxidative stress: interplay among hemoglobin, antioxidants, and lipid peroxidation. Am. J. Physiol. 272, L320–L334 [DOI] [PubMed] [Google Scholar]
- 10.Gorbunov N. V., McFaul S. J., Januszkiewicz A., Atkins J. L. 2005. Pro-inflammatory alterations and status of blood plasma iron in a model of blast-induced lung trauma. Int. J. Immunopathol. Pharmacol. 18, 547–556 [DOI] [PubMed] [Google Scholar]
- 11.Avidan V., Hersch M., Armon Y., Spira R., Aharoni D., Reissman P., Schecter W. P. 2005. Blast lung injury: clinical manifestations, treatment, and outcome. Am. J. Surg. 190, 945–950 10.1016/j.amjsurg.2005.08.022 (doi:10.1016/j.amjsurg.2005.08.022) [DOI] [PubMed] [Google Scholar]