Abstract
Objective
To examine factors associated with emotional well-being in women with spontaneous primary ovarian insufficiency
Design
Cross-sectional and case control
Setting
Clinical research center, national US health research facility
Patient(s)
Women diagnosed with spontaneous 46,XX primary ovarian insufficiency (N=100) at a mean age of 32.4 years and healthy control women of similar age (N=60)
Intervention(s)
Administration of validated self-reporting instruments
Main Outcome Measure(s)
Illness Uncertainty, Stigma, Goal Disengagement/Reengagement, Purpose in Life, Positive and Negative Affect Schedule, Center of Epidemiologic Studies Depression Scale, State-Trait Anxiety Inventory
Result(s)
Compared to controls, women with spontaneous primary ovarian insufficiency scored adversely on all measures of affect. Illness Uncertainty and Purpose in Life were significant independent factors associated with Anxiety (R2=0.47), Stigma and Purpose in Life were the significant independent factors associated with Depression (R2=0.51), and Goal Reengagement and Purpose in Life were significantly and independently associated with Positive Affect (R2=0.43).
Conclusion(s)
This evidence supports the need for prospective studies. Our findings are consistent with the hypothesis that clinicians could improve the emotional well-being of their patients with primary ovarian insufficiency by a) informing them better about their condition, b) helping them to feel less stigmatized by the disorder, and c) assisting them in developing alternative goals with regard to family planning as well as other goals.
Keywords: Primary ovarian insufficiency, hypergonadotropic hypogonadism, premature ovarian failure, premature menopause, infertility, illness uncertainty, stigma, goal flexibility
Introduction
Spontaneous primary ovarian insufficiency (also known as hypergonadotropic hypogonadism, premature ovarian failure, and premature menopause) involves the cessation of normal ovarian function before age 40. Our preferred term for the condition is “primary ovarian insufficiency” (POI) as first introduced by Fuller Albright in 1942 (1,2). The condition is associated with amenorrhea, symptoms of estrogen deficiency, infertility and general health concerns (3–5). It affects approximately 1% of women by age 40 (6). Research has demonstrated that patients with POI have reduced self-esteem, increased shyness, increased social anxiety, and more symptoms of depression than healthy control women (7).
In most cases of infertility, women discover that they are infertile in a gradual manner after many failed attempts at conception. In cases of POI, by contrast, frequently women learn suddenly of their likely inability to conceive even before they have contemplated or attempted conception (8–11). The emotional response to the sudden unexpected loss of the ability to conceive in this clinical situation in some ways parallels the grief response to an acute death of a loved one (9). Grief is essentially an emotion that draws us toward something or someone that is missing; the loss creates a discrepancy between the world that is and the world that “should be” (12). In the case of inability to conceive, the experience may be one of "disenfranchised grief," which occurs when (1) the loss has no legitimacy, is socially unrecognized or unacknowledged; (2) the loss is not recognized as significant to others in the social network or culture; and (3) the griever is not recognized as having suffered a loss and is unjustified in grieving (13).
Viewed from this perspective, it seems appropriate to consider patients who receive a diagnosis of POI as embarking upon a “psychosocial transition” that requires adaptation (12,14–16). Significant loss events in life are associated with increased frequency of major depressive disorder and other psychopathology (17–23). Losses that are most likely to lead to affective disorders a) are unexpected or unanticipated so that there is little opportunity for preparation; b) require people to undertake a major revision of their assumptions about the world, and c) have lasting implications (12). Learning the diagnosis of POI meets all of these criteria. In general, successful adaptation to loss relates to a) the extent to which the loss has been correctly anticipated, b) available support, and c) available opportunities and resources to address the loss (12).
In an earlier investigation with a different cohort of women, we conducted structured interviews in 100 women with POI, and found that 84% of the women felt emotionally unprepared to receive the diagnosis and 86% felt that they should have been given more information about the disorder (11). Overall, 71% of women were unsatisfied with how they were informed about the diagnosis, 49% felt the clinician informing them was insensitive to their emotional needs, and 89% reported experiencing moderate to severe emotional distress at the time. The degree of reported emotional distress was positively correlated with the degree of dissatisfaction with the manner in which the women had been informed of the diagnosis. By patient report, only 2% of clinicians provided a plan for managing emotional and mental health as part of informing them about the diagnosis (11).
In the present study, a case-control investigation, we addressed two primary questions. First, are there differences in emotional distress and well-being between women with and without POI, and second, are there psychosocial attributes that correlate with women’s ability to sustain well-being as they cope with the POI diagnosis. In particular, we examined whether women's emotional health is related to the uncertainty and stigma they experience as a result of the POI diagnosis, and to the positive psychological resources they possess, including goal flexibility and purpose in life. Uncertainty and a lack of understanding regarding one's condition have been associated with greater depression and anxiety and less effective coping in patients with a variety of chronic health problems, including endometriosis (24,25). Moreover, because we have evidence that patients with POI report a need to be provided more information about their condition (11), we predicted that higher levels of illness uncertainty would be related to greater emotional distress.
Medical and psychological conditions with no clear pathophysiology also have been associated with a sense of stigmatization, which in turn, is associated with greater social isolation and lower levels of emotional well-being (26–30). In the case of POI, stigma would be expected to create barriers to obtaining needed social support to cope with this diagnosis. In view of this, we evaluated whether stigma associated with the disorder is related to greater emotional distress.
Women with inability to conceive face a disruption in their pursuit of a central life goal for many individuals, that of childbearing (31). The ability to disengage from the goal of bearing children and develop new goals may be particularly adaptive for these individuals (32). Indeed, finding new opportunities in life is a way to successfully navigate psychosocial transitions (32–36). Thus, we assess goal flexibility as a factor expected to be related to greater emotional well-being in women with POI. Finally, in a previous study, we demonstrated that functional well-being in women with POI correlates significantly with meaning and purpose in life as measured on a validated spiritual well-being scale (37). Therefore, we expected a positive relation between purpose in life and emotional well-being in the current study.
In summary, we hypothesized that patients with POI would report lower levels of emotional well-being and higher levels of negative affect relative to healthy controls. We also predicted that emotional health in patients would be negatively associated with both uncertainty and feelings of stigma regarding their illness, and positively associated with goal flexibility and purpose in life.
Materials and Methods
Setting
This study was conducted at the National Institutes of Health (NIH) Clinical Center in Bethesda, Maryland. The study is part of an ongoing longitudinal investigation designed to identify psychosocial factors (including personality, social environment, and coping responses) that contribute to emotional health in women with spontaneous 46,XX POI. This report assesses how psychosocial measures at baseline are related to affective disturbance. Subsequent analyses of this data set will address the broader array of psychosocial measures that predict adaptation over time.
Patients
The Institutional Review Board of the National Institute of Child Health and Human Development approved the study. All participants gave written informed consent. We prospectively planned to enroll 100 patients for this study. Between June 2005 and February 2006 we recruited women with spontaneous POI by published advertisement and by Internet. Patients were recruited to a general screening protocol on POI and then offered enrollment in this study. One woman dropped out after enrollment and we recruited another patient to bring the total to 100. Subsequently a woman was found to have a 46,XY karyotype and was excluded from analysis, leaving data from 99 patients available for analyses.
For this study we defined spontaneous POI as the development before age 40 years of at least 4 months of amenorrhea or menstrual irregularity associated with two serum FSH levels in the menopausal range as defined by the individual local assay (sampled at least 1 month apart). We originally defined spontaneous POI as the development before age 40 years of at least 4 months of amenorrhea. We have since dropped the requirement for absolute amenorrhea for 4 months because it is now known that many patients with POI in fact have intermittent ovarian function to a degree that they have occasional irregular menses (38). Referring clinicians made the diagnosis of POI, and we required documentation of the above findings for admission to the protocol. Women with POI as a result of surgery, radiation, chemotherapy, or known karyotype abnormalities were not included. All women underwent a complete history and physical examination and baseline clinical and laboratory testing as described elsewhere as well as testing for the FMR1 premutation and the presence of adrenal antibodies (39). Patients were aged 18 to 42 years.
Controls
Control women were recruited by local advertisement and compensated according to NIH guidelines. They were between the ages of 18 and 42 years, described themselves as healthy, free of chronic disease, non pregnant, and regularly menstruating (cycles between 21 and 35 days). We stratified control recruitment by age and race so as to match proportionately with the makeup of our patient population based on prior experience (11,39,40).
Instruments
We administered the Center of Epidemiologic Studies Depression Scale (CES-D) (41), the state anxiety subscale of the State-Trait Anxiety Inventory (STAI). (42) We also administered the positive and negative affect subscales from the Positive and Negative Affect Schedule (PANAS) (43), and the purpose in life subscale from the Positive Mental Well-Being Inventory (44).
To assess illness uncertainty in women with POI, we administered the Mishel Uncertainty in Illness Scale (45). This includes items such as “I don’t know what is wrong with me” and “Because of the unpredictability of my condition I cannot plan for the future.” To assess perceived stigma we modified a previously established chronic disorder instrument developed by Lennon et al., to refer specifically to POI (46). This Modified Lennon Stigma scale includes items such as “Having this medical condition has made me feel very different from other people” and “I often feel totally alone with my condition.” To assess goal flexibility we administered the Goal Disengagement and Reengagement Scales with pregnancy as the goal (47). The disengagement scale includes items such as “It’s easy for me to reduce my efforts toward the goal” and “I find it difficult to stop trying to achieve the goal” (reverse scored). The reengagement scale includes items such as “I convince myself that I have other meaningful goals to pursue” and “I seek other meaningful goals.”
The internal consistency of the instruments, as measured by Chronbach’s alpha, was as follows: Goal Disengagement 0.86, Goal Reengagement 0.93, Illness Uncertainty 0.86, Stigma 0.73, Purpose in Life 0.87, CES-D 0.90, STAI 0.93, Negative Affect (PANAS) 0.85, and Positive Affect (PANAS) 0.92.
Analysis
Hypotheses
The a priori primary hypotheses to be tested were: 1) Compared to healthy controls, women with POI will report lower levels of emotional well-being (positive affect, purpose in life) and higher levels of negative affect (negative affect, state anxiety, depressive symptoms). 2) For women with POI, lower measures of illness uncertainty, lower measures of stigma, and higher measures of the ability to disengage from the goal of getting pregnant and to reengage with other goals will predict greater well-being and less negative affect. Alpha was set at p < 0.05 (two-tailed) for all analyses. With alpha set at p < 0.05 (two-tailed), power for comparisons between patients and controls was 0.80 to detect a moderately sized effect (i.e., d=0.45, as described by Cohen, 1992). Power was 0.80 to detect small to moderately large effect sizes (i.e., r=0.27) between study variables within the patient group.
Statistical Methods
All data were analyzed using SAS (Statistical Analysis System) version 9 (SAS Institute Inc., Cary, NC), and StatXact version 4.0.1 software (Cytel Software Corporation, Cambridge, MA). Internal consistency of the instruments was evaluated using Cronbach alpha raw scores. For demographic interval data we report mean ± standard deviation, and percentages for nominal and ordinal data. Chi-square or exact tests were used for categorical data, and the Kruskal-Wallis nonparametric test for singly ordered contingency tables was used for comparing ordered categorical data. We used Wilcoxon rank-sum tests to compare instrument scores between patients and controls, and Spearman correlations to explore relations between instruments. We used multiple linear regression, two-way analysis of variance, and analysis of covariance to explore the contributions of more than one independent variable to an outcome measure.
Because many instrument variables were not normally distributed, SAS PROC TRANSREG was used for Box-Cox transformations of dependent variables for regression analyses (48). To address possible multicollinearity among response variables and interplay between response and predictor variables, extensive univariate and multivariate modeling was employed, and q-q normality plots and histograms of potential Box-Cox transformations were examined to arrive at a consensus transformation for each response variable. Predictor variables with a ratio of maximum/minimum greater than 10 were transformed to logarithms (49). Collinearity diagnostics were performed on regression analyses and the resulting variance inflation factors, tolerances and condition indexes were examined. Regression model residuals were also examined using q-q normality plots and by plotting residuals versus predicted values. Transformed variables were used in two-way analysis of variance and analysis of covariance models.
Results
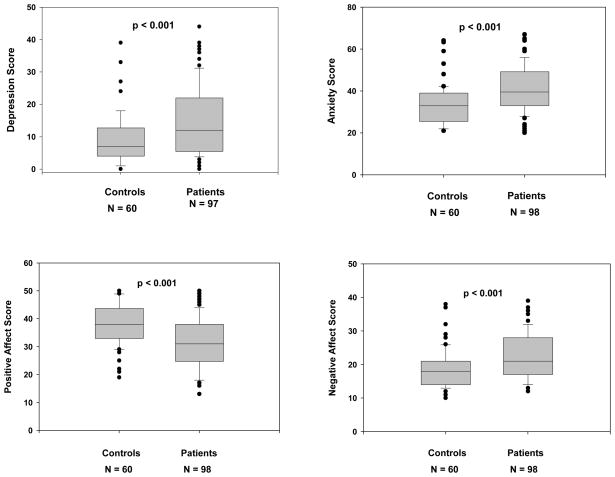
Table 1 depicts the demographic characteristics of patients and controls, and shows that patients did not differ significantly from controls with regard to age, race, ethnicity, education level,, or whether or not they have children. A significantly higher percentage of patients were married/partnered (vs single/divorced/other) as compared to controls (61.6% vs 43.3% respectively, p=0.03). In our main analyses comparing women with POI and controls on measures of negative affect and well-being, results showed that patients tended to fare worse on most outcomes. As shown in Figure 1, compared to control women, women with spontaneous POI had significantly higher median (interquartile range) scores on the CES-D depression scale [12 (6–22), vs 7(4–12.5), p<0.001], on the STAI anxiety scale [39.5 (33–49) vs 33 (26–39), p<0.001], and on the Negative Affect scale [21 (17–28) vs 18(14–21), p<0.001]. They also scored lower on the Positive Affect scale [31 (25–38) vs 38 (33–43.5), p<0.001].
Table 1.
Demographics of women with primary ovarian insufficiency (POI) and control women.
| POI (N=99) | Controls (N=60) | P | |
|---|---|---|---|
| Age in years (mean ± SD) | 32.4. ±5.2 | 31.0 ±6.9 | 0.25 |
| Race (%) | 0.86 | ||
| White | 76.7 | 78.3 | |
| Black / African American | 12.1 | 10.0 | |
| Hawaiian / Pacific Islander | 2.0 | 0.0 | |
| Asian | 4.0 | 5.0 | |
| Unreported | 5.1 | 6.7 | |
| Ethnicity (%) | 1.00 | ||
| Hispanic / Latino | 6.1 | 6.7 | |
| Non-Hispanic / Latino | 93.9 | 93.3 | |
| Married/Partnered (%) | 61.6 | 43.3 | 0.03 |
| Have one child or more (%) | 29.8 | 33.3 | 0.72 |
| Education Level (%) | 0.61 | ||
| High school | 3.0 | 1.7 | |
| Some college | 12.1 | 15.0 | |
| College degree | 45.5 | 43.3 | |
| Master’s degree | 31.3 | 20.0 | |
| Doctoral degree | 8.1 | 20.0 |
Figure 1.
Comparison of affective outcome measures between control women and women with spontaneous 46,XX primary ovarian insufficiency. Measures were assessed by the Center of Epidemiologic Studies Depression Scale, the state anxiety subscale of the State-Trait Anxiety Inventory, and the Positive and Negative Affect Schedule. Whiskers represent 10 and 90th percentiles and lines in the boxes represent median and inter-quartile range. Each dot represents a data point outside of these ranges. N represents the number of completed instruments.
Patients were also more likely than controls to report depressive and high anxiety states when assessed categorically. As shown in Table 2, patients more often scored above cutoff values for clinical levels of depression on the CESD (41), and more often reported anxiety scores greater than one standard deviation above the norm for individuals in this age group (42). Compared to control women, women with POI had somewhat lower scores on the Purpose in Life scale [46 (39–51) vs 48.5 (43–51), p. =0.08], but the difference was not statistically significant.
Table 2.
Comparison of control women and women with spontaneous 46,XX primary ovarian insufficiency (POI) with regard to frequency of mild, moderate, and severe depressive states as assessed by the Center for Epidemiologic Studies Depression Scale (CES-D) and high anxiety state as assessed by the State-Trait Anxiety Inventory.
| POI (N=98) N (%) | Controls (N=60) N (%) | P | |
|---|---|---|---|
| Depression1 | <0.0022 | ||
| None (CES-D< 16) | 57 (58.8) | 49 (81.7) | |
| Mild (CES-D 16 -20) | 14 (14.4) | 6 (10.0) | |
| Moderate (CES-D 21–26) | 8 (8.3) | 2 (3.3) | |
| Severe (CES-D ≥ 27) | 18 (18.6) | 3 (5.0) | |
| High Anxiety3 (> 44) | 37 (37.8) | 5 (8.3) | < 0.0014 |
Scores may range from 0 to 60, with higher scores reflecting greater depression.
Kruskal-Wallis test for singly ordered contingency tables.
Scores may range from 20 to 80, with higher scores reflecting greater anxiety.
Fisher’s exact test.
Among women with POI 18/94 (19%) were currently taking medications for anxiety or depression compared to 3/60 (5%) of controls (p=0.02), and 38/94 (40%) had a history of taking such medications as compared to 12/60 (20%) of controls (p<0.01). With regard to mental health counseling, 13/93 (14%) of patients were currently receiving counseling compared to 3/60 (5%) of controls (p=.10) and 50/93 (54%) of patients had a history of seeking counseling as compared to 15/60 (25%) of controls (p<0.001).
We conducted analyses to examine whether study variables were related to demographic factors in patients and controls and to identify potential covariates in our comparisons between groups. For both women with POI and controls, scores on the CES-D, STAI, Positive Affect, Negative Affect, and Purpose in Life scales did not differ by whether or not participants had children, and scores on the CES-D, STAI, Positive Affect, and Purpose in Life scale did not differ by whether or not participants were married/partnered when analyzed as a dichotomy. However, married/partnered patients scored lower on the Negative Affect scale compared to single/divorced/other patients(p=0.05), whereas among control women, marital status was unrelated to negative affect. Including marital status as a covariate in comparisons of patients with controls did not alter the findings reported above (data not shown).
Within the sample of 99 women with POI, 20 women had children by their own conception, 3 women had adopted children, 3 women had children by ovum donation, 1 woman had a child by embryo donation, 1 woman had children by both conception and adoption, and 5 declined to answer. In addition, 38 reported a previous pregnancy; 19 reported a previous elective termination of pregnancy; and 8 reported a previous spontaneous abortion. Of the 99 patients, 21 had thyroid-related disorder, 3 had an adrenal disorder, and 6 had an FMR1 permutation. Twelve women had primary amenorrhea.
To identify potential covariates in our analyses of emotional health among patients, we examined whether demographic or illness-related characteristics were related to psychosocial attributes and outcomes in women with POI. Higher education was significantly associated with lower Illness Uncertainty (r=−0.20, p = .0477) and lower Negative Affect (r=−0.23, p<0.025) but had no significant association with scores on Depression, Anxiety, Positive Affect, Purpose in Life, Stigma, or Goal Disengagement/Reengagement. We also found no significant associations between age, race, age at diagnosis, or time since diagnosis (on average, they had been diagnosed with POI 39.5 months prior to enrollment in the study) and scores of Depression, Anxiety, Positive or Negative Affect, Illness Uncertainty, Perceived Stigma, Purpose in Life or Goal Reengagement/Disengagement. Endocrine abnormalities, parity, and experience of elective or spontaneous abortion also were unrelated to any of the five study outcomes (i.e., anxiety, depression, positive affect, negative affect, and well-being). However, we did find that women with a premutation in the FMR1 gene (n=6) scored significantly higher on positive affect than did women without this permutation (p=0.03).
Table 3 displays the inter-correlations among key variables for women with POI. Not surprisingly, the psychosocial risk factors of Illness Uncertainty and Stigma were positively related, and the resource factors Goal Disengagement and Reengagement were positively related. Purpose in Life was positively related to Goal Reengagement but unrelated to Goal Disengagement. The majority of risk and resilience factors were also inversely related to one another. Consistent with our main hypothesis, psychosocial risk and resource factors were related to emotional well-being and negative affect measures in women with POI. Stigma and Illness Uncertainty scores were significantly positively correlated with Depression and Anxiety, and negatively correlated with Positive Affect. Resource factors showed the opposite pattern. Goal Reengagement and Purpose in Life were significantly positively correlated with Positive Affect, and negatively correlated with Negative Affect, Depression, and Anxiety. Goal Disengagement was inversely related only to Depression.
Table 3.
Spearman correlations assessing the association between affective outcome measures and measures of Illness Uncertainty, Stigma, Goal Disengagement and Goal Reengagement in women with spontaneous 46,XX primary ovarian insufficiency (N=99). Measures were assessed by the Mishel Uncertainty in Illness Scale, a modified Lennon Stigma scale, the Purpose in Life subscale from the Positive Mental Well-Being Inventory, the Goal Disengagement and Reengagement Scales with pregnancy as the goal, the Positive and Negative Affect Schedule, the Center of Epidemiologic Studies Depression Scale, and the state anxiety subscale of the State-Trait Anxiety Inventory.
| Factor | IU | S | GD | GR | PIL | PA | NA | D | A |
|---|---|---|---|---|---|---|---|---|---|
| Illness Uncertainty (IU) | - | 0.61*** | −0.18 | −0.24* | −0.23* | −0.27** | 0.38*** | 0.46*** | 0.53*** |
| Stigma (S) | - | −0.26** | −0.25* | −0.34*** | −0.26* | 0.46*** | 0.59*** | 0.51*** | |
| Goal Disengagement (GD) | - | 0.48*** | 0.07 | 0.14 | −0.17 | −0.22* | −0.20 | ||
| Goal Reengagement (GR) | - | 0.24* | 0.41*** | −0.20* | −0.26* | −0.33** | |||
| Purpose in Life (PIL) | - | 0.58*** | −0.46*** | −0.58*** | −0.53*** | ||||
| Positive Affect (PA) | - | −0.35*** | −0.67*** | −0.48*** | |||||
| Negative Affect (NA) | - | 0.61*** | 0.68*** | ||||||
| Depression (D) | - | 0.64*** | |||||||
| Anxiety (A) | - |
p<0.05,
p<0.01,
p<0.001
To examine the unique contributions of risk and resource factors to emotional health in women with POI, we included a set of four predictor variables (Purpose in Life, Stigma, Illness Uncertainty, and Goal Reengagement) in four separate forward multiple regression analyses for outcome variables: Anxiety, Depression, Negative Affect, and Positive Affect. To summarize the findings: 1) Illness Uncertainty and Purpose in Life were significant independent factors associated with Anxiety (R2= 0.47), 2) Stigma and Purpose in Life were the significant independent factors associated with Depression (R2=0.51) and Negative Affect (R2=0.33), and 3) Goal Reengagement and Purpose in Life were significantly and independently associated with Positive Affect (R2=0.43). The magnitude of the relations between main predictor variables and their outcomes in these final models were not altered when we included potentially confounding variables: history of elective or spontaneous abortion, parity, time since diagnosis, premutation in FMR1 gene, and endocrine disorder variables such as thyroid or adrenal disorder. Of note, in three instances, potentially confounding variables were also marginally associated with the outcome: 1) history of elective abortion was marginally associated with decreased Positive Affect (p=0.06), 2) presence of any thyroid disease and of any endocrine disorder were both associated with increased Negative Affect (p=0.052 and p=0.039, respectively). None of the tests for collinearity detected the presence of multicollinearity.
Discussion
We had two aims for this study, 1) to compare measures of emotional health in women with POI and healthy controls, and 2) to examine associations of risk and resource factors with emotional health among patients with POI. In comparison with controls, patients in this study had increased prevalence of depression and anxiety, and lower levels of positive affect. We previously found that 84% of women with spontaneous 46,XX POI reported that the diagnosis caused them a moderate or severe degree of emotional suffering (11). Findings here are consistent with our earlier qualitative findings, and with a previous report demonstrating that women with this condition have increased symptoms of depression compared to normal control women (7). We extend these findings to demonstrate that, compared to controls, women with spontaneous 46,XX POI report not only increased distress, but also decreased positive affect. The current results suggest that clinicians should assess both positive and negative affective experiences to more fully understand the emotional well-being of their patients.
Among patients with POI, we explored the extent to which psychosocial risk and resource factors might explain levels of emotional symptoms and well-being. With regard to risk factors, we found that those patients who feel more uncertainty and more stigmatization regarding their condition report higher levels of anxiety and depressive symptoms. Purpose in life scores were also significantly related to lower anxiety and depression symptoms, and to greater positive affect. Clearly, women's understanding of and sense of stigmatization about their condition, and ability to sustain a sense of life purpose, are highly related to the levels of distress, consistent with patterns observed in other individuals with chronic health conditions (24,25,29,50,51).
In our prior work, patients told us that getting thorough and accurate information about POI helped them cope with the diagnosis (11). The relationships we find here between disease uncertainty and affective distress are consistent with this earlier finding and suggest that clinicians may be able to reduce the emotional suffering experienced by patients with POI by providing them with thorough and accurate information about their condition. The process begins when the clinician initially informs the patient of the diagnosis. In this situation, the clinician is confronted with communicating information about a sudden, unexpected diagnosis that is life-altering. How bad news is communicated can have a profound effect on quality of life (52) and other health outcomes (53–61). Over 75% of women with POI feel unprepared to hear the news, (11) which suggests there is room for improvement in this clinical skill. Women with POI also perceive a need for clinicians to spend more time with them and provide more information (11). Over 40% of the women are informed of the diagnosis by telephone, often when they are at their workplace, and this suggests that many clinicians underestimate the potential emotional significance of this diagnosis (11). Clinicians may benefit from training that develops their skills to more effectively deliver troubling news (62–66). There may also be a need to develop a cadre of nurse educators for POI, following a model that has been applied to the management of diabetes (67,68).
Our findings also point to the importance of stigmatization as a factor that may contribute to the emotional well-being of women with POI. Cross cultural evidence has indicated that the desire for children is considered the norm and infertility is stigmatized (69,70). Slade et al. found that stigma was significantly positively correlated not only with infertility-related distress, but also with symptoms of anxiety and depression (30). In our sample of women with POI we found that stigma explained significant unique variance in symptoms of depression. An important component of stigma captured by the measure we employed here is social alienation, reflecting a sense of isolation and withdrawal from social relationships. Existing evidence points to the value of educational interventions as a means by which to reduce stigma (71–73). Our findings suggest that helping women to decrease stigmatization by sustaining their connection with their social networks may be a means of facilitating adaptation.
In addition to the importance of risk factors such as illness uncertainty and stigma, the current findings also highlight the potential importance of psychosocial resources for women with POI. We found that being able to pursue goals unrelated to childbearing (i.e., goal reengagement) and sustain a general sense of a purpose in life were strongly related to greater positive affect, together accounting for 43% of the variance. Our findings parallel those from earlier work demonstrating that substituting other life goals for the goal of childbearing is associated with greater positive affect among women past childbearing age (74). Interestingly, it seems that there is little need for women with POI to give up on the goal of getting pregnant; the ability to disengage from this goal was not strongly associated with measures of either distress or well-being. A psychosocial transition that involves grief has generally been viewed as a process by which one must detach from a loss in order to free up energy to reconnect with new attachments (75). However, accruing evidence, including findings from the present study, challenge this notion (76–79). The role of goal reengagement in promoting positive affect for women with POI deserves further investigation, as positive affect is a potent resource that contributes to an individual's capacity to recover following difficult experiences (80).
The study has several limitations that constrain interpretation of the findings. Because we employed a cross-sectional design, we are unable to conclude that the relations we observed are causal. Moreover, we cannot examine the dynamic changes that are likely to occur over time as women live with and adjust to their diagnosis. Also because we employed a sample of convenience, our findings may not generalize to all women with this condition. Finally, our comparison group of healthy women was recruited in a manner different from the patient sample, which may have introduced systematic differences between groups beyond the difference in presence or absence of a diagnosis of POI. Nonetheless, analysis of cross-sectional data can prove very useful in generating hypotheses to be tested by prospective controlled studies.
In summary, clinicians who convey a diagnosis of POI to women are presenting them with life-altering information. The findings we present here provide insight into the factors that relate to the emotional health of these women, and suggest potential targets for interventions. In particular, reducing women's uncertainty and stigmatization regarding their condition, assisting them in developing other meaningful goals, and encouraging them to sustain a sense of purpose may improve their functional well-being and quality of life. The study highlights the need to prospectively develop and test interventions that will enhance a woman's capacity to navigate this difficult life transition.
Acknowledgments
We thank the women with POI and the normal control women for participating.
Supported by the Intramural Research Program of the National Institute of Child Health and Human Development, National Institutes of Health. Vien H. Vanderhoof and Lawrence M. Nelson are Commissioned Officers in the United States Public Health Service.
Footnotes
Where the work was done: National Institutes of Health, Bethesda, Maryland, USA,
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Albright F, Smith PH, Fraser R. A syndrome characterized by primary ovarian insufficiency and decreased stature. American Journal of the Medical Sciences. 1942;204:625–648. [Google Scholar]
- 2.Welt CK. Primary ovarian insufficiency: a more accurate term for premature ovarian failure. Clin Endocrinol (Oxf) 2008;68:499–509. doi: 10.1111/j.1365-2265.2007.03073.x. [DOI] [PubMed] [Google Scholar]
- 3.Rebar RW, Connolly HV. Clinical features of young women with hypergonadotropic amenorrhea. Fertil Steril. 1990;53:804–810. [PubMed] [Google Scholar]
- 4.Conway GS, Kaltsas G, Patel A, Davies MC, Jacobs HS. Characterization of idiopathic premature ovarian failure. Fertil Steril. 1996;65:337–341. doi: 10.1016/s0015-0282(16)58095-9. [DOI] [PubMed] [Google Scholar]
- 5.Nelson LM, Covington SN, Rebar RW. An update: spontaneous premature ovarian failure is not an early menopause. Fertil Steril. 2005;83:1327–1332. doi: 10.1016/j.fertnstert.2004.11.059. [DOI] [PubMed] [Google Scholar]
- 6.Coulam CB, Adamson SC, Annegers JF. Incidence of premature ovarian failure. Obstet Gynecol. 1986;67:604–606. [PubMed] [Google Scholar]
- 7.Schmidt PJ, Cardoso GM, Ross JL, Haq N, Rubinow DR, Bondy CA. Shyness, social anxiety, and impaired self-esteem in Turner syndrome and premature ovarian failure. JAMA. 2006;295:1374–1376. doi: 10.1001/jama.295.12.1374. [DOI] [PubMed] [Google Scholar]
- 8.Pasquali EA. The impact of premature menopause on women's experience of self. J Holist Nurs. 1999;17:346–364. doi: 10.1177/089801019901700404. [DOI] [PubMed] [Google Scholar]
- 9.Orshan SA, Furniss KK, Forst C, Santoro N. The lived experience of premature ovarian failure. J Obstet Gynecol Neonatal Nurs. 2001;30:202–208. doi: 10.1111/j.1552-6909.2001.tb01536.x. [DOI] [PubMed] [Google Scholar]
- 10.Alzubaidi NH, Chapin HL, Vanderhoof VH, Calis KA, Nelson LM. Meeting the needs of young women with secondary amenorrhea and spontaneous premature ovarian failure. Obstet Gynecol. 2002;99:720–725. doi: 10.1016/s0029-7844(02)01962-2. [DOI] [PubMed] [Google Scholar]
- 11.Groff AA, Covington SN, Halverson LR, Fitzgerald OR, Vanderhoof V, Calis K, et al. Assessing the emotional needs of women with spontaneous premature ovarian failure. Fertil Steril. 2005;83:1734–1741. doi: 10.1016/j.fertnstert.2004.11.067. [DOI] [PubMed] [Google Scholar]
- 12.Parkes C. Bereavement as a psychosocial transition: processes of adaptation to change. J Social Issues. 1988;44:53–65. [Google Scholar]
- 13.Harvey JH. Disenfranchised Grief: New Directions, Challenges, and Strategies for Practice. Champaign, IL: Research Press; 2002. [Google Scholar]
- 14.Greil AL. Infertility and psychological distress: a critical review of the literature. Soc Sci Med. 1997;45:1679–1704. doi: 10.1016/s0277-9536(97)00102-0. [DOI] [PubMed] [Google Scholar]
- 15.Riley LP, LaMontagne LL, Hepworth JT, Murphy BA. Parental grief responses and personal growth following the death of a child. Death Stud. 2007;31:277–299. doi: 10.1080/07481180601152591. [DOI] [PubMed] [Google Scholar]
- 16.Lechner L, Bolman C, van DA. Definite involuntary childlessness: associations between coping, social support and psychological distress. Hum Reprod. 2007;22:288–294. doi: 10.1093/humrep/del327. [DOI] [PubMed] [Google Scholar]
- 17.Clayton PJ. Mortality and morbidity in the first year of widowhood. Arch Gen Psychiatry. 1974;30:747–750. doi: 10.1001/archpsyc.1974.01760120013002. [DOI] [PubMed] [Google Scholar]
- 18.Raphael B. The management of pathological grief. Aust N Z J Psychiatry. 1975;9:173–180. doi: 10.3109/00048677509159845. [DOI] [PubMed] [Google Scholar]
- 19.Jacobs S, Hansen F, Kasl S, Ostfeld A, Berkman L, Kim K. Anxiety disorders during acute bereavement: risk and risk factors. J Clin Psychiatry. 1990;51:269–274. [PubMed] [Google Scholar]
- 20.Downey G, Silver RC, Wortman CB. Reconsidering the attribution-adjustment relation following a major negative event: coping with the loss of a child. J Pers Soc Psychol. 1990;59:925–940. doi: 10.1037//0022-3514.59.5.925. [DOI] [PubMed] [Google Scholar]
- 21.Horowitz MJ. A model of mourning: change in schemas of self and other. J Am Psychoanal Assoc. 1990;38:297–324. doi: 10.1177/000306519003800202. [DOI] [PubMed] [Google Scholar]
- 22.Stroebe M, Stroebe W. Does "grief work" work? J Consult Clin Psychol. 1991;59:479–482. doi: 10.1037//0022-006x.59.3.479. [DOI] [PubMed] [Google Scholar]
- 23.Prigerson HG, Frank E, Kasl SV, Reynolds CF, III, Anderson B, Zubenko GS, et al. Complicated grief and bereavement-related depression as distinct disorders: preliminary empirical validation in elderly bereaved spouses. Am J Psychiatry. 1995;152:22–30. doi: 10.1176/ajp.152.1.22. [DOI] [PubMed] [Google Scholar]
- 24.Reich JW, Johnson LM, Zautra AJ, Davis MC. Uncertainty of illness relationships with mental health and coping processes in fibromyalgia patients. J Behav Med. 2006;29:307–316. doi: 10.1007/s10865-006-9054-7. [DOI] [PubMed] [Google Scholar]
- 25.LeMaire GS. More than just menstrual cramps: symptoms and uncertainty among women with endometriosis. J Obstet Gynecol Neonatal Nurs. 2004;33:71–79. doi: 10.1177/0884217503261085. [DOI] [PubMed] [Google Scholar]
- 26.Link BG, Struening EL, Rahav M, Phelan JC, Nuttbrock L. On stigma and its consequences: evidence from a longitudinal study of men with dual diagnoses of mental illness and substance abuse. J Health Soc Behav. 1997;38:177–190. [PubMed] [Google Scholar]
- 27.Link BG, Phelan JC. Stigma and its public health implications. Lancet. 2006;367:528–529. doi: 10.1016/S0140-6736(06)68184-1. [DOI] [PubMed] [Google Scholar]
- 28.Looper KJ, Kirmayer LJ. Perceived stigma in functional somatic syndromes and comparable medical conditions. J Psychosom Res. 2004;57:373–378. doi: 10.1016/j.jpsychores.2004.03.005. [DOI] [PubMed] [Google Scholar]
- 29.Markowitz FE. The effects of stigma on the psychological well-being and life satisfaction of persons with mental illness. J Health Soc Behav. 1998;39:335–347. [PubMed] [Google Scholar]
- 30.Slade P, O'Neill C, Simpson AJ, Lashen H. The relationship between perceived stigma, disclosure patterns, support and distress in new attendees at an infertility clinic. Hum Reprod. 2007;22:2309–2317. doi: 10.1093/humrep/dem115. [DOI] [PubMed] [Google Scholar]
- 31.Menning BE. The emotional needs of infertile couples. Fertil Steril. 1980;34:313–319. doi: 10.1016/s0015-0282(16)45031-4. [DOI] [PubMed] [Google Scholar]
- 32.Heckhausen J, Wrosch C, Fleeson W. Developmental regulation before and after a developmental deadline: the sample case of "biological clock" for childbearing. Psychol Aging. 2001;16:400–413. doi: 10.1037//0882-7974.16.3.400. [DOI] [PubMed] [Google Scholar]
- 33.Haythornthwaite JA, Menefee LA, Heinberg LJ, Clark MR. Pain coping strategies predict perceived control over pain. Pain. 1998;77:33–39. doi: 10.1016/S0304-3959(98)00078-5. [DOI] [PubMed] [Google Scholar]
- 34.Cheng C. Cognitive and motivational processes underlying coping flexibility: a dual-process model. J Pers Soc Psychol. 2003;84:425–438. [PubMed] [Google Scholar]
- 35.Cheng C, Cheung MW. Cognitive processes underlying coping flexibility: differentiation and integration. J Pers. 2005;73:859–886. doi: 10.1111/j.1467-6494.2005.00331.x. [DOI] [PubMed] [Google Scholar]
- 36.Cheng C, Yang FC, Jun S, Hutton JM. Flexible coping psychotherapy for functional dyspeptic patients: a randomized, controlled trial. Psychosom Med. 2007;69:81–88. doi: 10.1097/01.psy.0000249734.99065.6f. [DOI] [PubMed] [Google Scholar]
- 37.Ventura JL, Fitzgerald OR, Koziol DE, Covington SN, Vanderhoof VH, Calis KA, et al. Functional well-being is positively correlated with spiritual well-being in women who have spontaneous premature ovarian failure. Fertil Steril. 2007;87:584–590. doi: 10.1016/j.fertnstert.2006.07.1523. [DOI] [PubMed] [Google Scholar]
- 38.Nelson LM, Anasti JN, Kimzey LM, Defensor RA, Lipetz KJ, White BJ, et al. Development of luteinized Graafian follicles in patients with karyotypically normal spontaneous premature ovarian failure. J Clin Endocrinol Metab. 1994;79:1470–1475. doi: 10.1210/jcem.79.5.7962345. [DOI] [PubMed] [Google Scholar]
- 39.Kim TJ, Anasti JN, Flack MR, Kimzey LM, Defensor RA, Nelson LM. Routine endocrine screening for patients with karyotypically normal spontaneous premature ovarian failure. Obstet Gynecol. 1997;89:777–779. doi: 10.1016/s0029-7844(97)00077-x. [DOI] [PubMed] [Google Scholar]
- 40.Bakalov VK, Anasti JN, Calis KA, Vanderhoof VH, Premkumar A, Chen S, et al. Autoimmune oophoritis as a mechanism of follicular dysfunction in women with 46,XX spontaneous premature ovarian failure. Fertil Steril. 2005;84:958–965. doi: 10.1016/j.fertnstert.2005.04.060. [DOI] [PubMed] [Google Scholar]
- 41.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 42.Spielberger CD. State-Trait Axiety Inventory: A Comprehensive Bibliography. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 43.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. J Pers Soc Psychol. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 44.Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Pers Soc Psychol. 1995;69:719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 45.Mishel MH. The measurement of uncertainty in illness. Nurs Res. 1981;30:258–263. [PubMed] [Google Scholar]
- 46.Lennon MC, Link BG, Marbach JJ, Dohrenwend BP. The stigma of chronic facial pain and its impact on social relationships. Social Problems. 1989;36:117–133. [Google Scholar]
- 47.Wrosch C, Scheier MF, Miller GE, Schulz R, Carver CS. Adaptive self-regulation of unattainable goals: goal disengagement, goal reengagement, and subjective well-being. Pers Soc Psychol Bull. 2003;29:1494–1508. doi: 10.1177/0146167203256921. [DOI] [PubMed] [Google Scholar]
- 48.Box GEP, Cox DR. An analysis of transformations. Journal of the Royal Statistical Society, Series B. 1964;26:211–252. [Google Scholar]
- 49.Weisberg S. Applied linear regression. 2. New York: Wiley; 1985. [Google Scholar]
- 50.Reich JW, Olmsted ME, van Puymbroeck CM. Illness uncertainty, partner caregiver burden and support, and relationship satisfaction in fibromyalgia and osteoarthritis patients. Arthritis Rheum. 2006;55:86–93. doi: 10.1002/art.21700. [DOI] [PubMed] [Google Scholar]
- 51.Johnson LM, Zautra AJ, Davis MC. The role of illness uncertainty on coping with fibromyalgia symptoms. Health Psychol. 2006;25:696–703. doi: 10.1037/0278-6133.25.6.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fallowfield L. The ideal consultation. Br J Hosp Med. 1992;47:364–367. [PubMed] [Google Scholar]
- 53.Molleman E, Krabbendam PJ, Annyas AA, Koops HS, Sleijfer DT, Vermey A. The significance of the doctor-patient relationship in coping with cancer. Soc Sci Med. 1984;18:475–480. doi: 10.1016/0277-9536(84)90003-0. [DOI] [PubMed] [Google Scholar]
- 54.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27:S110–S127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 55.Fallowfield LJ, Hall A, Maguire GP, Baum M. Psychological outcomes of different treatment policies in women with early breast cancer outside a clinical trial. Brit Med J. 1990;301:575–580. doi: 10.1136/bmj.301.6752.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Simpson M, Buckman R, Stewart M, Maguire P, Lipkin M, Novack D, et al. Doctor-patient communication: the Toronto consensus statement. Brit Med J. 1991;303:1385–1387. doi: 10.1136/bmj.303.6814.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Sardell AN, Trierweiler SJ. Disclosing the cancer diagnosis. Procedures that influence patient hopefulness. Cancer. 1993;72:3355–3365. doi: 10.1002/1097-0142(19931201)72:11<3355::aid-cncr2820721135>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 58.Roberts CS, Cox CE, Reintgen DS, Baile WF, Gibertini M. Influence of physician communication on newly diagnosed breast patients' psychologic adjustment and decision-making. Cancer. 1994;74:336–341. doi: 10.1002/cncr.2820741319. [DOI] [PubMed] [Google Scholar]
- 59.Omne-Ponten M, Holmberg L, Sjoden PO. Psychosocial adjustment among women with breast cancer stages I and II: six-year follow-up of consecutive patients. J Clin Oncol. 1994;12:1778–1782. doi: 10.1200/JCO.1994.12.9.1778. [DOI] [PubMed] [Google Scholar]
- 60.Parle M, Jones B, Maguire P. Maladaptive coping and affective disorders among cancer patients. Psychol Med. 1996;26:735–744. doi: 10.1017/s0033291700037752. [DOI] [PubMed] [Google Scholar]
- 61.Fogarty LA, Curbow BA, Wingard JR, McDonnell K, Somerfield MR. Can 40 seconds of compassion reduce patient anxiety? J Clin Oncol. 1999;17:371–379. doi: 10.1200/JCO.1999.17.1.371. [DOI] [PubMed] [Google Scholar]
- 62.Buckman R. How to Break Bad News - A Guide for Health Care Professionals. Baltimore, MD: The Johns Hopkins University Press; 1992. [Google Scholar]
- 63.Greenberg LW. Delivering bad news. JAMA. 1996;276:1801. doi: 10.1001/jama.276.22.1801b. [DOI] [PubMed] [Google Scholar]
- 64.Greenberg LW, Ochsenschlager D, O'Donnell R, Mastruserio J, Cohen GJ. Communicating bad news: a pediatric department's evaluation of a simulated intervention. Pediatrics. 1999;103:1210–1217. doi: 10.1542/peds.103.6.1210. [DOI] [PubMed] [Google Scholar]
- 65.Towle A, Hoffman J. An advanced communication skills course for fourth-year, post-clerkship students. Acad Med. 2002;77:1165–1166. doi: 10.1097/00001888-200211000-00033. [DOI] [PubMed] [Google Scholar]
- 66.Farber NJ, Urban SY, Collier VU, Weiner J, Polite RG, Davis EB, et al. The good news about giving bad news to patients. J Gen Intern Med. 2002;17:914–922. doi: 10.1046/j.1525-1497.2002.20420.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Johnson CL. Regaining self-esteem: strategies and interventions for the infertile woman. J Obstet Gynecol Neonatal Nurs. 1996;25:291–295. doi: 10.1111/j.1552-6909.1996.tb02574.x. [DOI] [PubMed] [Google Scholar]
- 68.Funnell MM, Anderson RM, Nwankwo R, Gillard ML, Butler PM, Fitzgerald JT, et al. A study of certified diabetes educators: influences and barriers. Diabetes Educ. 2006;32:359–6. 368. doi: 10.1177/0145721706288041. [DOI] [PubMed] [Google Scholar]
- 69.Rosenblatt PC, Peterson P, Portner J, Cleveland M, Mykkanen A, Foster R, et al. A cross-cultural study of responses to childlessness. Cross-Cultural Research. 1973;8:221–231. [Google Scholar]
- 70.Whiteford LM, Gonzalez L. Stigma: the hidden burden of infertility. Soc Sci Med. 1995;40:27–36. doi: 10.1016/0277-9536(94)00124-c. [DOI] [PubMed] [Google Scholar]
- 71.Griffiths KM, Christensen H, Jorm AF, Evans K, Groves C. Effect of web-based depression literacy and cognitive-behavioural therapy interventions on stigmatising attitudes to depression: randomised controlled trial. Br J Psychiatry. 2004;185:342–349. doi: 10.1192/bjp.185.4.342. [DOI] [PubMed] [Google Scholar]
- 72.Finkelstein J, Lapshin O. Reducing depression stigma using a web-based program. Int J Med Inform. 2007;76:726–734. doi: 10.1016/j.ijmedinf.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 73.Finkelstein J, Lapshin O, Wasserman E. Randomized study of different anti-stigma media. Patient Educ Couns. 2008;71:204–214. doi: 10.1016/j.pec.2008.01.002. [DOI] [PubMed] [Google Scholar]
- 74.Heckhausen J, Wrosch C, Fleeson W. Developmental regulation before and after a developmental deadline: the sample case of "biological clock" for childbearing. Psychol Aging. 2001;16:400–413. doi: 10.1037//0882-7974.16.3.400. [DOI] [PubMed] [Google Scholar]
- 75.Worden JW. Grief counseling and grief therapy a handbook for the mental health practitioner. 3. New York: Springer Pub; 2002. [Google Scholar]
- 76.Klass D. Solace and immortality: Bereaved parents' continuing bonds with their children. Death Stud. 1993;17:343–368. [Google Scholar]
- 77.Russac RJ, Steighner NS, Canto AI. Grief work versus continuing bonds: a call for paradigm integration or replacement? Death Stud. 2002;26:463–478. doi: 10.1080/074811802760138996. [DOI] [PubMed] [Google Scholar]
- 78.Murphy SA, Johnson LC, Chung IJ, Beaton RD. The prevalence of PTSD following the violent death of a child and predictors of change 5 years later. J Trauma Stress. 2003;16:17–25. doi: 10.1023/A:1022003126168. [DOI] [PubMed] [Google Scholar]
- 79.Shear K, Shair H. Attachment, loss, and complicated grief. Dev Psychobiol. 2005;47:253–267. doi: 10.1002/dev.20091. [DOI] [PubMed] [Google Scholar]
- 80.Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol. 2004;86:320–333. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]