Abstract
Symptomatic intradialytic hypotension is a common complication of hemodialysis (HD). The application of convective therapies to the outpatient setting may improve outcomes, including intradialytic hypotension. In this multicenter, open-label, randomized controlled study, we randomly assigned 146 long-term dialysis patients to HD (n = 70), online predilution hemofiltration (HF; n = 36), or online predilution hemodiafiltration (HDF; n = 40). The primary end point was the frequency of intradialytic symptomatic hypotension (ISH). Compared with the run-in period, the frequency of sessions with ISH during the evaluation period increased for HD (7.1 to 7.9%) and decreased for both HF (9.8 to 8.0%) and HDF (10.6 to 5.2%) (P < 0.001). Mean predialysis systolic BP increased by 4.2 mmHg among those who were assigned to HDF compared with decreases of 0.6 and 1.8 mmHg among those who were assigned to HD and HF, respectively (P = 0.038). Multivariate logistic regression demonstrated significant risk reductions in ISH for both HF (odds ratio 0.69; 95% confidence interval 0.51 to 0.92) and HDF (odds ratio 0.46, 95% confidence interval 0.33 to 0.63). There was a trend toward higher dropout for those who were assigned to HF (P = 0.107). In conclusion, compared with conventional HD, convective therapies (HDF and HF) reduce ISH in long-term dialysis patients.
Hemodialysis (HD) is not an effective treatment for long-term dialysis patients with stage 5 chronic kidney disease (CKD), and their comorbidities, including intradialytic symptomatic hypotension (ISH), are persistently very high,1 possibly contributing to their high mortality rate.2 Convective treatments (CTs)—increasing “middle molecule” removal and removing fluids by more physiologic convection—have been suggested for improving dialysis patient outcomes including the reduction of ISH.3,4 Observational studies have consistently suggested that high-flux treatments for long-term dialysis patients with stage 5 CKD are associated with reduced morbidity and mortality.5–8 The Hemodialysis (HEMO) Study,9 a landmark randomized, controlled trial designed to test the effect of membrane flux and dialysis dosage on mortality, showed that high-flux HD is associated with a nonsignificantly lower relative mortality risk of 8%, although a secondary analysis suggested a significant advantage of high-flux membranes in patient subgroups. More recently, the Membrane Permeability Outcome (MPO) study10 found that survival could be significantly improved by using high-flux as compared with low-flux membranes in high-risk patients identified by serum albumin of ≤4 g/dl as well as in patients with diabetes in a post hoc analysis. By extrapolating the experimental results of these multicenter studies, it can be hypothesized that the benefits could be even greater by further increasing convection in treating long-term dialysis patients with stage 5 CKD. The number of randomized, prospective trials that have compared CTs with standard HD is still very low, and no conclusive data are available concerning the effect of CTs in their various forms on morbidity and survival in long-term dialysis patients with stage 5 CKD.
It is very interesting to observe that the concept of dialysis adequacy has now widened to include not only urea kinetics11 but also middle and high molecule removal12,13 and biocompatibility.14 Locatelli et al.,15 in a controlled randomized multicenter study involving 380 patients, compared four treatment dialysis modalities: Low-flux Cuprophan HD, low-flux polysulfone HD, high-flux polysulfone HD, and high-flux polysulfone hemodiafiltration (HDF). Although a reduction in predialysis β-2 microglobulin levels in high-flux HD and HDF compared with low-flux HD was found, no differences were reported in treatment tolerance; however, the number of symptomatic treatments were far fewer than expected, thus reducing the statistical power of the study. Canaud et al.16 analyzed the data from Dialysis Outcomes and Practice Patterns Study (DOPPS) and reported that survival was associated with the amount of convection.
Two prospective clinical trials performed by the Sardinian Collaborative Group3,4 compared the clinical effects of (bicarbonate) high-flux HD and predilution online (bicarbonate) HF in clinically stable patients, with different3 and similar4 equilibrated Kt/V (eKt/V) and treatment times. Polyamide membranes, ultrapure fluid with similar electrolyte composition, and the same dialysis machine were used in both studies. These studies showed fewer symptoms, including hypotension in HF as compared with HD also in clinically stable small-sized patient groups. A third prospective collaborative study performed by the same collaborative group comparing HF with HDF17 in a group of 39 stable patients, after a run-in treatment period of 6 months on low-flux HD, found that HF was more effective in reducing the frequency of hypotension. On the basis of the results of these Sardinian studies, we planned a prospective, multicenter randomized study to compare low-flux HD with online predilution HF and/or HDF to evaluate the sessions with ISH of two different types and dosages of convection in comparison with HD, as routinely performed by investigators in day-to-day clinical practice.
Results
Baseline Characteristics
A total of 146 patients were enrolled and centrally randomly allocated to HD (70 patients), HF (36 patients), and HDF (40 patients) and followed up for a median of 1.5 years (interquartile range [IQR] 0.8 to 2.2). Table 1 summarizes the baseline demographic and clinical characteristics of the three patient groups, which were similar in terms of gender, body weight, prevalence of hypertension, ischemic cardiopathy, peripheral arteriopathy, previous transient ischemic attack (TIA), dialysis modality before the study, dialysis vintage, dialysis time, and ultrafiltration (UF) rate. There was an unbalanced age distribution, with the HF group having older patients than the other groups (71.3 versus 65.2 and 66.8 years of HD and HDF groups, respectively; P = 0.086) and an unbalanced diabetes prevalence, with the HDF group having more patients with diabetes (27.5 versus 17.1 and 8.3% of HD and HF groups, respectively; P = 0.091) and patients who had diabetes and were on insulin therapy (20 versus 0 and 11 of HD and HF groups, respectively; P = 0.020). No differences among groups were present for biochemical variables (Table 2) related to the dialysis dosage for small molecular weight solutes (eKt/V), equilibrated protein catabolic rate (ePCRn), electrolyte, sodium, potassium, bicarbonate, calcium, phosphorous, hemoglobin, C-reactive protein, albumin, total cholesterol, and triglycerides.
Table 1.
Clinical characteristics of enrolled patients at baseline
| Characteristic | Total (N = 146) | HD (n = 70) | Pre-HF (n = 36) | Pre-HDF (n = 40) | P |
|---|---|---|---|---|---|
| Gender (n [%]) | 0.646 | ||||
| male | 84 (57.5) | 43 (61.4) | 19 (52.8) | 22 (55.0) | |
| female | 62 (42.5) | 27 (38.6) | 17 (47.2) | 18 (45.0) | |
| Age (years; median [IQR]) | 67.4 (58.1 to 73.3) | 65.2 (58.1 to 70.8) | 71.3 (60.6 to 74.4) | 66.8 (54.6 to 74.3) | 0.086 |
| Body weight (kg; median [IQR]) | 64.9 (55.9 to 70.8) | 65.5 (57.9 to 70.8) | 62.3 (53.3 to 66.6) | 66.8 (55.4 to 76.9) | 0.115 |
| Hypertension (n [%]) | 83 (56.8) | 39 (55.7) | 20 (55.6) | 24 (60) | 0.894 |
| Diabetes (n [%]) | 26 (17.8) | 12 (17.1) | 3 (8.3) | 11 (27.5) | 0.091 |
| Insulin therapy (n [%]) | 16 (11.0) | 8 (11.4) | 0 (0.0) | 8 (20.0) | 0.020 |
| Ischemic cardiopathy (n [%]) | 32 (21.9) | 16 (22.9) | 6 (16.7) | 10 (25.0) | 0.658 |
| Peripheral arteriopathy (n [%]) | 14 (9.6) | 8 (11.4) | 3 (8.3) | 3 (7.5) | 0.763 |
| Previous TIA (n [%]) | 17 (11.6) | 7 (10.0) | 4 (11.1) | 6 (15.0) | 0.729 |
| Dialysis technique before study (n [%]) | 0.296 | ||||
| HD | 124 (84.9) | 61 (87.1) | 32 (88.9) | 31 (77.5) | |
| HDF | 22 (15.1) | 9 (12.9) | 4 (11.1) | 9 (22.5) | |
| Dialysis vintage (years; median [IQR]) | 3.0 (1.4 to 7.7) | 2.5 (1.2 to 9.0) | 4.1 (1.4 to 7.7) | 3.1 (1.5 to 6.1) | 0.636 |
| Dialysis time (minutes; median [IQR]) | 240 (210 to 240) | 240 (210 to 240) | 240 (210 to 240) | 240 (221 to 240) | 0.650 |
| Net UF (L/session; median [IQR]) | 2.8 (2.5 to 3.4) | 2.9 (2.5 to 3.3) | 2.6 (2.0 to 2.9) | 2.8 (2.5 to 3.7) | 0.055 |
| Net UF (% of dry body wt; median [IQR]) | 4.3 (3.9 to 5.0) | 4.4 (3.9 to 5.0) | 4.2 (3.8 to 4.9) | 4.4 (3.8 to 5.1) | 0.448 |
Table 2.
Laboratory characteristics of enrolled patients at baseline
| Characteristic | Total (N = 146) | HD (n = 70) | HF (n = 36) | HDF (n = 40) | P |
|---|---|---|---|---|---|
| Urea at start of session (mg/dl) | 170 (145 to 194) | 170 (147 to 195) | 169 (138 to 194) | 169 (146 to 186) | 0.851 |
| Hemoglobin (g/dl) | 11.6 (11.0 to 12.1) | 11.5 (10.9 to 12.1) | 11.5 (10.7 to 11.9) | 11.8 (11.2 to 12.2) | 0.108 |
| Sodemia (mMol/L) | 138.0 (136.5 to 140.5) | 138.0 (136.7 to 140.1) | 138.9 (136.7 to 140.8) | 137.5 (134.7 to 139.5) | 0.113 |
| Kaliemia (mMol/L) | 5.55 (5.21 to 5.99) | 5.58 (5.22 to 5.93) | 5.60 (5.21 to 6.29) | 5.50 (5.19 to 5.79) | 0.654 |
| Bicarbonatemia (mMol/L) | 19.9 (18.7 to 21.7) | 19.9 (18.6 to 22.2) | 19.9 (18.5 to 21.5) | 20.0 (19.0 to 21.4) | 0.889 |
| Calcemia (mMol/L) | 1.14 (1.08 to 1.20) | 1.13 (1.08 to 1.17) | 1.16 (1.11 to 1.20) | 1.17 (1.06 to 1.23) | 0.162 |
| Phosphoremia (mMol/L) | 1.61 (1.32 to 1.85) | 1.59 (1.31 to 1.88) | 1.61 (1.31 to 1.89) | 1.62 (1.39 to 1.81) | 0.926 |
| C-reactive protein (mg/dl) | 0.8 (0.3 to 2.3) | 0.7 (0.3 to 2.2) | 0.7 (0.3 to 2.4) | 0.9 (0.3 to 2.6) | 0.935 |
| Plasma albumin (g/dl) | 3.95 (3.65 to 4.20) | 3.95 (3.59 to 4.20) | 3.90 (3.71 to 4.20) | 3.85 (3.70 to 4.35) | 0.958 |
| Total cholesterol (mg/dl) | 161 (138 to 191) | 160 (138 to 189) | 162 (141 to 188) | 164 (128 to 193) | 0.988 |
| Triglycerides (mg/dl) | 154 (100 to 217) | 162 (115 to 255) | 138 (92 to 200) | 154 (94 to 196) | 0.381 |
| eKt/V | 1.27 (1.14 to 1.42) | 1.28 (1.15 to 1.43) | 1.22 (1.13 to 1.39) | 1.19 (1.14 to 1.40) | 0.317 |
| ePCRn (g/kg per day) | 1.13 (0.97 to 1.28) | 1.15 (1.02 to 1.33) | 1.12 (0.95 to 1.22) | 1.10 (0.96 to 1.25) | 0.425 |
ePCRn, equilibrated protein catabolic rate.
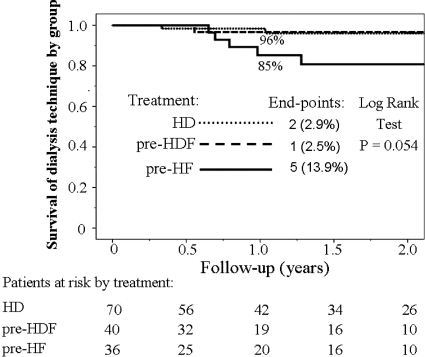
Dropouts
Table 3 shows the frequency and causes of dropouts among groups. No differences were present for dropouts caused by death or kidney transplantation. Fifteen (10.3%) patients died during the study, with no differences between the groups (P = 0.403); with 195.3 person-years of follow-up in the experimental period, the mortality rate was 7.7% per year. The causes of death were infection (four patients); acute myocardial infarction (three patients); cachexia (two patients); pulmonary embolism (two patients); and postoperative complication, cardiovascular disease, acute pulmonary edema, and acute cerebral bleeding (one patient each). Thirteen (8.9%) patients underwent transplantation with a cadaveric kidney without a different distribution between groups (P = 0.273). A nonsignificant trend to a higher dropout rate was present in the HF group: 52.8% of patients reached the end of study in comparison with 71.4 and 72.5% of other two groups (P = 0.107). The shift from HF (five [13.9%] of 36 patients: one patient for high-transmembrane pressure and consequent inability to obtain the UF target, two patients for vascular access problems, one patient shifted to acetate free biofiltration for choice of the attendant physician, and one patient increased the dialysis frequency to four sessions per week) was significantly higher compared with the shift from HDF (one [2.5%] of 40 patients, for patient choice) and from HD (two [2.9%] of 70 patients, for patient choice) (P = 0.038). For the same reason, the survival of the dialysis modality was significantly lower for HF (85% at 1 year) as compared with the other two modalities (96% at 1 year) (P = 0.054, log-rank test; Figure 1).
Table 3.
Dropout causes according to the adaptation and evaluation periods
| Parameter | Total | Treatment |
P | ||
|---|---|---|---|---|---|
| HD | HF | HDF | |||
| Dropouts in the adaptation period | |||||
| deaths | 2 | 2 | 0 | 0 | |
| kidney transplant | 4 | 2 | 1 | 1 | |
| thrombosis or vascular access infection | 1 | 0 | 1 | 0 | |
| withdrawal of consent | 2 | 0 | 2 | 0 | |
| transfer to another center | 1 | 0 | 1 | 0 | |
| no. of patients | 10 | 4 | 5 | 1 | 0.127 |
| Dropouts in the evaluation period | |||||
| deaths | 13 | 6 | 5 | 2 | |
| kidney transplant | 9 | 3 | 1 | 5 | |
| transfer to another modality | 8 | 2 | 5 | 1 | |
| thrombosis or vascular access infection | 3 | 2 | 1 | 0 | |
| withdrawal of consent | 2 | 1 | 0 | 1 | |
| transfer to another center | 1 | 0 | 0 | 1 | |
| transfer to another study | 1 | 1 | 0 | 0 | |
| infection | 1 | 1 | 0 | 0 | |
| no. of patients | 38 | 16 | 12 | 10 | 0.500 |
| Total (n [%]) | |||||
| end of the study | 98 (67.1) | 50 (71.4) | 19 (52.8) | 29 (72.5) | 0.107 |
| death | 15 (10.3) | 8 (11.4) | 5 (13.9) | 2 (5.0) | 0.403 |
| kidney transplant | 13 (8.9) | 5 (7.1) | 2 (5.6) | 6 (15.0) | 0.273 |
| transfer to another technique | 8 (5.5) | 2 (2.9) | 5 (13.9) | 1 (2.5) | 0.038 |
| thrombosis or vascular access infection | 4 (2.7) | 2 (2.9) | 2 (5.6) | 0 (0.0) | |
| withdrawal of consent | 4 (2.7) | 1 (1.4) | 2 (5.6) | 1 (2.5) | |
| transfer to another center | 2 (1.4) | 0 (0.0) | 1 (2.8) | 1 (2.5) | |
| transfer to another study | 1 (0.7) | 1 (1.4) | 0 (0.0) | 0 (0.0) | |
| infection | 1 (0.7) | 1 (1.4) | 0 (0.0) | 0 (0.0) | |
| no. of patients | 146 | 70 | 36 | 40 | |
Figure 1.
More patients shift out of HF than other treatment modalities. Survival function in pre-HF group was lower (85% at 1-year follow-up) as compared with the other groups (96% at 1-year follow-up). P = 0.054, log rank test.
According to the protocol, although patient dropouts were 48 (32.9%) altogether, only 10 (6.8%) patients—four in HD, one in HDF, and five in HF groups (P = 0.127)—were not included in the final analysis because they dropped out during the 3-month adaptation period. Thus, the main analysis was performed on 136 (93.2%) patients: 66 in HD, 39 in HDF, and 31 in HF groups.
Dialysis Dosage and Flux
As expected, the median dialysis dosage for small molecular weight solutes measured by the eKt/V index decreased significantly (P < 0.001) in HF from 1.22 (IQR 1.13 to 1.39) to 1.13 (IQR 1.01 to 1.17) in comparison with increased values in HDF from 1.19 (IQR 1.14 to 1.40) to 1.34 (IQR 1.25 to 1.48) and with constant values in HD from 1.28 (IQR 1.15 to 1.43) to 1.30 (IQR 1.14 to 1.44). During the evaluation period, total median reinfusion in predilution mode was equal to 60.4 L per session (IQR 50.2 to 69.9) in HF (106% of dry body weight) and to 39.9 L per session (IQR 28.2 to 51.0) in HDF (64% of dry body weight).
Symptomatic Hypotension, BP, and Antihypertensive Therapy
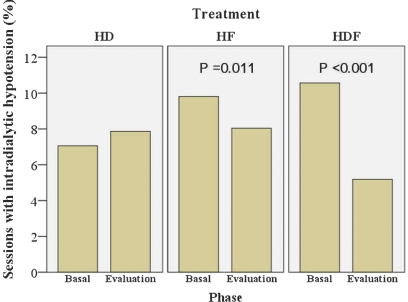
Over a total of 28,950 sessions, 2169 (7.5%) were complicated by ISH. In the evaluation period compared with the run-in period (Table 4), there was a small absolute increase of 0.8% in the frequency of sessions with ISH in HD (from 7.1 to 7.9%; relative increase 9.9%) and an absolute decrease of 1.8% in HF (from 9.8 to 8.0%; relative decrease 18.4%; P = 0.011) and of 5.4% in HDF (from 10.6 to 5.2%; relative decrease 50.9%; P < 0.001; Figure 2). By contrast, there was a mean increase of 4.2 mmHg of predialysis systolic BP (SBP) values in HDF compared with the other groups (−0.6 and −1.8 mmHg in HD and HF, respectively; P = 0.038).
Table 4.
Intradialytic symptomatic hypotension, BP values, and antihypertensive therapy by phase and treatment groups
| Parameter | Treatment |
P | |||||
|---|---|---|---|---|---|---|---|
| Run-in Phase |
Evaluation Phase |
||||||
| HD | HF | HDF | HD | HF | HDF | ||
| No. of patients | 66 | 31 | 39 | 66 | 31 | 39 | |
| No. of sessions | 2096 | 1203 | 1249 | 11942 | 6502 | 5958 | |
| Sessions with symptomatic hypotension (n [%]) | 148 (7.1) | 118 (9.8) | 132 (10.6) | 939 (7.9) | 523 (8.0) | 309 (5.2) | |
| Symptomatic hypotension variation (%) | +0.8 | −1.8 | −5.4 | <0.001 | |||
| SBP (mmHg; mean ± SD) | 140.5 ± 17.6 | 139.9 ± 18.0 | 137.3 ± 18.9 | 140.5 ± 15.5 | 137.3 ± 18.6 | 141.5 ± 18.8 | |
| mean difference by phase (mmHg) | −0.0 | −2.6 | +4.2 | 0.038 | |||
| DBP (mmHg; mean ± SD) | 76.7 ± 10.2 | 75.8 ± 9.8 | 74.5 ± 12.6 | 75.4 ± 9.3 | 72.6 ± 9.4 | 74.7 ± 11.4 | |
| mean difference by phase (mmHg) | −1.3 | −3.2 | +0.2 | 0.096 | |||
| Heart rate (bits/min; mean ± SD) | 74.5 ± 8.2 | 72.7 ± 6.8 | 74.3 ± 10.4 | 73.9 ± 9.2 | 73.4 ± 6.9 | 75.4 ± 9.0 | |
| mean difference by phase (bits/m) | −0.6 | +0.7 | +0.9 | 0.250 | |||
| No. of antihypertensive drugs (median [IQR]) | 1.0 (0.0 to 2.0) | 1.0 (0.0 to 2.5) | 1.0 (0.7 to 2.0) | 1.0 (0.0 to 1.8) | 0.9 (0.0 to 2.0) | 1.0 (0.6 to 2.0) | 0.385 |
| Patients treated with antihypertensive drugs (%) | 48.6 | 58.3 | 75.0 | 56.1 | 62.1 | 75.9 | |
| difference by phase (%) | +7.5 | +3.8 | +0.9 | 0.676 | |||
| Postdialysis body weight (kg; mean ± SD) | 64.9 ± 9.7 | 60.7 ± 10.1 | 65.8 ± 12.9 | 64.8 ± 10.0 | 60.2 ± 10.3 | 65.2 ± 12.9 | |
| mean difference by phase (kg) | −0.1 | −0.5 | −0.6 | 0.508 | |||
| Net UF (L/session; mean ± SD) | 2.7 ± 0.7 | 2.4 ± 0.7 | 2.9 ± 0.7 | 2.7 ± 0.7 | 2.4 ± 0.7 | 2.9 ± 0.9 | |
| mean difference by phase (L/session) | −0.0 | −0.0 | −0.0 | 0.893 | |||
| Predialysis sodemia (mEq/L; mean ± SD) | 138.3 ± 3.3 | 138.9 ± 2.9 | 137.3 ± 3.2 | 138.0 ± 3.2 | 138.8 ± 2.8 | 137.3 ± 2.9 | |
| mean difference by phase (mEq/L) | −0.3 | −0.1 | −0.0 | 0.942 | |||
| Postdialysis sodemia (mEq/L; mean ± SD) | 139.0 ± 3.4 | 139.7 ± 3.0 | 138.7 ± 3.4 | 138.7 ± 3.2 | 139.1 ± 2.6 | 138.8 ± 2.7 | |
| mean difference by phase (mEq/L) | −0.3 | −0.6 | −0.1 | 0.808 | |||
| ΔSession sodemia (mEq/L; mean ± SD) | 0.7 ± 3.3 | 0.8 ± 2.6 | 1.4 ± 2.8 | 0.7 ± 2.6 | 0.3 ± 1.7 | 1.5 ± 2.1 | |
| mean difference by phase (mEq/L) | −0.0 | −0.5 | −0.1 | 0.848 | |||
Components of sodium balance (body weight, net UF, pre/postsodiemia values, and Δpost/presession sodiemia values) were also shown. Intradialytic symptomatic hypotension ameliorated in pre-HF (P = 0.011) and in pre-HDF (P < 0.001) groups compared with the HD group, but predialysis SBP values rose in the pre-HDF group as compared with the other groups (P = 0.038).
Figure 2.
7.5% of all of the 28,950 sessions were complicated by ISH. In the evaluation period compared with the basal run-in, there was a statistically significant decrease of sessions with ISH in HF (9.8 to 8.0%, decrease of 18.4%; P = 0.011) and in HDF (10.6 to 5.2%, decrease of 50.9%; P < 0.001) compared with low-flux HD group (7.1 to 7.9%, increase of 9.9%).
The antihypertensive therapy, estimated by the number of antihypertensive classes, and the percentage of patients who were treated with antihypertensive drugs were not significantly different between groups (P = 0.385 and P = 0.676, respectively). There were no statistical differences on the estimated sodium removal among the three modalities, as suggested by the postdialysis body weight (P = 0.508), the amount of net UF (P = 0.893), and the pre/postsession plasma sodium concentration (P = 0.848; Table 4). No significant differences between groups were present for the intradialytic variations of SBP and diastolic BP (DBP) values and heart rate, from the run-in period to the evaluation period (data not shown).
Multivariate Logistic Regression
Table 5 summarizes the results of the multivariate logistic regression analysis of the effect of HF and HDF on ISH, independent of other relevant covariates listed in the Concise Methods section. This model was applied to a total of 28,950 sessions (run-in and evaluation periods). The risk for sessions with ISH was higher in patients with diabetes (odds ratio [OR] 1.68; 95% confidence interval [CI] 1.48 to 1.90), in older patients (OR 1.02 for each 1-year increase in age; 95% CI 1.02 to 1.03), in patients with chronic ischemic cardiopathy (OR 1.64; 95% CI 1.47 to 1.83), in patients with chronic ischemic arteriopathy (OR 1.54; 95% CI 1.34 to 1.77), in patients with a previous TIA (OR 2.04; 95% CI 1.80 to 2.32), and in patients with high values of predialysis DBP (OR 1.01 for each 1-mmHg increase; 95% CI 1.002 to 1.012), whereas it was lower in patients with high values of predialysis SBP (OR 0.98 for each 1-mmHg increase; 95% CI 0.97 to 0.98). The value of net UF rate (in dl/h) was also associated to sessions with ISH (OR 1.14; 95% CI 1.12 to 1.16), meaning an increasing risk of 14% for each dl/h. Taking into account all of these covariates, the beneficial effect of CTs was present for both HF (OR 0.69; 95% CI 0.51 to 0.92; P = 0.011) and HDF (OR 0.46; 95% CI 0.33 to 0.63; P < 0.001), with a significant risk reduction of 31 and 54%, respectively.
Table 5.
Predictors associated with symptomatic intradialytic hypotension by means of multiple logistic regression
| Parameter | B | P | OR | 95% CI |
|---|---|---|---|---|
| Diabetes | 0.517 | <0.001 | 1.680 | 1.480 to 1.900 |
| Age (years) | 0.024 | <0.001 | 1.020 | 1.020 to 1.030 |
| SBP (mmHg) | −0.025 | <0.001 | 0.975 | 0.972 to 0.978 |
| DBP (mmHg) | 0.007 | 0.011 | 1.010 | 1.002 to 1.012 |
| Ischemic cardiopathy | 0.493 | <0.001 | 1.640 | 1.470 to 1.830 |
| Chronic ischemic arteriopathy | 0.430 | <0.001 | 1.540 | 1.340 to 1.770 |
| Previous TIA | 0.715 | <0.001 | 2.040 | 1.800 to 2.320 |
| Net UF rate (dl/h) | 0.130 | <0.001 | 1.140 | 1.120 to 1.160 |
| Experimental treatment | <0.001 | |||
| HF | −0.378 | 0.011 | 0.690 | 0.510 to 0.920 |
| HDF | −0.782 | <0.001 | 0.460 | 0.330 to 0.630 |
This model was applied to a total of 28,950 sessions in run-in and evaluation periods. Overall, symptomatic intradialytic hypotension was present in 7.5% of cases. The beneficial effect of HF and HDF, compared with the reference HD and adjusted for the effect of the other covariates included in the model, was highly significant (P = 0.011 and P < 0.001, respectively). B, regression coefficient.
Discussion
Systems for the online production of large amounts of ultrapure dialysis and/or substitution fluids have been in place for many years18,19 to apply convection economically and at the highest efficiency. Performance of online HDF with substitution fluid reinfusion in pre-, post-, and prepostdilution mode20 is now common clinical practice in some centers, providing high-dosage convection together with powerful clearance of low molecular weight substances. Online HF21 potentially gives the highest dosage of convection, although it is less popular, possibly because it is less effective than HDF in removal of low molecular weight molecules; therefore, HF is usually reserved for hemodynamically unstable patients.22 Nevertheless, the role of pure convection as in HF and the convection mixed with diffusion as in HDF on ISH remains to be established because no studies have simultaneously compared these treatments with a concurrent experimental randomized, controlled study design.
To our knowledge, our study is the first multicenter, randomized, controlled trial to compare simultaneously three extracorporeal treatments with different levels of convection and diffusion on intradialytic cardiovascular stability of long-term HD patients. The main finding of this study is the demonstration of a lower frequency of ISH in patients who were treated with pure (HF) or mixed (HDF) convection in comparison with patients who were treated with a diffusive technique (low-flux HD; Figure 2). This effect was more pronounced in online predilution HDF; this lower frequency of ISH was associated, in HDF, with a significant increase in predialysis SBP values (from 137.3 to 141.5 mmHg), possibly clinically relevant in the long term. Thus, the beneficial effect of a 54% reduction of ISH should be balanced with a mean increase in predialysis SBP of 4.2 mmHg.
The clinical importance of sodium removal in the prevention of ISH in HD patients23 is widely known. Apparently, in our study, there were no major differences in the sodium removal among the three modalities (Table 4), as suggested by the similar pre- and posttreatment plasma sodium concentrations, the similar amount of UF rate, and the similar dry body weight behavior during the trial follow-up; however, this was a crude estimation of the dialytic sodium removal, so the possibility of a more positive sodium balance during CTs could not be ruled out,23 at least in HDF, as suggested by the increase in predialysis SBP.
It is also widely known that the cold dialysate and/or infusate can reduce the frequency of ISH24–26; however, we chose the online mode for both HF and HDF to reduce the effects of a cold infusate. Nevertheless, it has been reported that the cold effect is still present in online HDF.27
Our idea was to reproduce as closely as possible what physicians do in everyday clinical practice when using different techniques, independent of the pathophysiologic interpretation of the ISH; therefore, we decided not to give the investigators strict guidelines as to how to perform the treatments, thereby enhancing the general applicability of the results. The protocol clearly underlined, however, that the temperature and the composition of dialysate/infusate, including sodium, potassium, calcium, and bicarbonate, should be kept constant during the trial follow-up.
Another important message of this study is a great difficulty not only in performing HF but also in maintaining patients on HF (Figure 1), even in a trial on CTs such as ours, in which the selection bias of the participating centers and investigators is highly likely. This aspect is supported by the significantly lower frequency of the patients who ended the trial on HF (52.8%) as compared with either HD (71.4%) or HDF (72.5%) and further underlined by the significantly higher percentage of patients who switched from HF to another modality (13.9%), as compared with from HD (2.9%) and from HDF (2.5%; Table 3); however, it is important to underline that no relevant adverse effects were seen in patients who were treated with HF during the trial follow-up.
The relatively low mortality (7.7%/year) in the study population as a whole suggests that enrolled patients were possibly healthier than the general dialysis population, as a result of the inclusion of clinically stable patients without infections, malignancies, active systemic diseases, active hepatitis or cirrhosis, instable diabetes, or vascular access dysfunction. Thus we could speculate a higher beneficial effect of CTs in the case of their application to patients with more comorbidity and a higher ISH prevalence than the 7.5% found in this study.
The study has some weaknesses but also some relevant strengths. The major weakness is that we did not enroll the number of patients foreseen by the protocol, possibly because of the competition of this investigator-independent trial with the concurrent-industry sponsored trials with large grants; however, that we found a statistical difference between diffusive treatments and CTs reduces this criticism related to lower sample size because an underpower of a study is important in case of negative results.
The strengths of this study include the randomized trial design, the randomization stratified by center, the multicenter involvement, the use of the adaptation period, and a prospective run-in period of 2 months. This last point permitted a within-patient contrast of the intradialysis hypotension frequency between the evaluation and the run-in periods, thereby increasing the power of the study and adjusting for confounding dialysis conditions, such as dialysate/infusate temperature and sodium and calcium concentrations, which were maintained stable by the protocol's moving from the run-in to the experimental phase.
In conclusion, this multicenter, randomized study showed a lower ISH frequency in patients who were treated with CTs (HDF and HF) as compared with patients who were treated with a diffusion technique (low-flux HD), with no relevant adverse effects. This beneficial effect was more pronounced in HDF, associated with a significant increase in predialysis SBP. These results may have important clinical implications.
Concise Methods
Study Design
This multicenter, open-label, randomized study was conducted in 27 Italian dialysis centers. The study protocol was approved by the institutional review board of each center, and all patients gave written informed consent. Details of the study protocol have been published elsewhere.28 Eligible patients were randomly assigned 1:1 by e-mail to receive low-flux HD or CTs (1:1 to online predilution HF or online predilution HDF) using a central computer-generated randomization list that was stratified by center and prepared in advance by one author (S.A.), who e-mailed the assigned random treatment to the participating center. In some Centers, where HF was unavailable, the patients were randomized to HD or online predilution HDF on a 1:1 ratio. The planned duration of the recruitment period was initially 1 year; thereafter, it was increased to 4 years because of difficulty in enrolling patients. As described in the study protocol,28 after a 2-month run-in period, the planned 2-year duration of the experimental phase was divided into two periods: a fixed 3-month adaptation period and a subsequent 21-month evaluation period. Patients who did not complete the adaptation period according to the protocol were excluded from the intention-to-treat analysis.
Participants
Patients were eligible after giving written consent when they were aged 18 to 80 years, were on thrice-weekly HD or HDF for at least 6 months, had a body weight ≤90 kg, and were in stable clinical condition. Patients with clinically relevant infections, malignancies, active systemic diseases, active hepatitis or cirrhosis, instable diabetes, diuresis >200 ml/24 h, or a dysfunction of vascular access, with blood flow rate <300 ml/min, were excluded from the study.
Treatment Parameters Valid for All Patients
HD, HF, and HDF machines all were provided by a dialysis fluid UF system for the production of ultrapure dialysate and sterile nonpyrogen substitution fluid, checked at monthly intervals. Dialysate/infusate conductivity, dialysate/infusate calcium and bicarbonate concentrations and the dialysate/infusate temperatures, food ingestion habits during the study, and the use of antihypertensive drugs before the dialysis session were kept constant according to the center's policy, to follow everyday clinical practice as much as possible. Blood flow was between 300 and 400 ml/min, and the treatment time was between 3.0 and 4.5 hours for each session. Dialysate/infusate compositions were sodium 133 to 152 mEq/L, potassium 1 to 3 mEq/L, calcium 2.5 to 4.0 mEq/L, acetate 4 mEq/L, bicarbonate 26 to 38 mEq/L, and glucose 1 g/L.
Specific Characteristics of the Three Treatments
HD was performed with a low-flux membrane and with a dialysate flow rate of 500 ml/min. HF was performed with a synthetic high-flux membrane and an infusate/blood flow ratio of 1. HDF was performed with a synthetic high-flux membrane with an infusate/blood flow ratio of 0.6 and a dialysate plus infusate rate of 700 ml/min.
Clinical Data
At baseline, comorbidity conditions were recorded according to a formatted detailed form. At each session, ISH, defined as a rapid symptomatic fall of SBP by at least 30 mmHg or that required nursing and/or medical intervention, was specifically recorded. Pre- and postsession data on body weight, BP, and heart rate were recorded, together with dialysis parameters, such as filter type, blood flow, dialysis time, and total infusion (in CT).
Dialysis Schedule
All data related to the dialysis prescription, evaluated according to the assessment of the attending physician (dry body weight, dialysis time, dialysis modality, dialysate/infusate composition, and heparin dosage), were recorded monthly.
Therapy
The following therapies were recorded for each session: quality and quantity of saline infusions, erythropoiesis-stimulating agent treatments, and iron and any other drug orally or intravenously administered either during or at end of the session. All interdialysis therapies were recorded.
Laboratory Data
The predialysis levels of hemoglobin; serum electrolytes, including sodium, potassium, bicarbonate, calcium, and phosphate; urea; and creatinine were checked each month. Urea and sodium were evaluated monthly also at the end of the session. C-reactive protein and albumin were checked every 3 months. Cholesterol and triglycerides were checked every 6 months.
Dialysis Dosage
According to the center's policy, sampling was performed in the first or in the second session of the week. The blood sample for the determination of the final plasma urea concentration was drawn from the arterial line 10 seconds after reducing the blood flow to 100 ml/min with dialysate flow in bypass and by clamping the venous line after venous bubble trap. eKt/V and equilibrated protein catabolic rate (ePCRn) values were calculated monthly using procedures and simplified equations according to Daugirdas.29
Statistical Analysis
The descriptive analysis was based on the median and IQRs or mean and SD values for normally distributed continuous variables or counts and percentages for categorical variables. Differences at baseline in clinical and laboratory variables among the three groups were tested using variance analysis for normally distributed continuous variables, the nonparametric Kruskal-Wallis test for non-normally distributed continuous variables, and the χ2 test for categorical variables. BP was evaluated at four levels: (1) change in the frequency of ISH; (2) change in predialysis BP values; (3) change in intradialytic BP values; and (4) change in the number of the antihypertensive drugs. Multivariate logistic ISH regression was used to test the effect of experimental treatments (predilution HF and predilution HDF) compared with the reference HD and to find the predictors related to ISH including diabetes, age, predialysis SBP and DBP, chronic ischemic cardiopathy, chronic ischemic arteriopathy, previous TIA, and UF rate (level 1). The general linear model for repeated measures of ANOVA was used for the other dependent variables (levels 2 through 4). The main interpatient factor was the random assigned group. The group effect was tested using the group-by-time interaction. The group of HD was considered the reference. All of the statistical analyses were performed using SPSS 17.02 for Windows (SPSS, Chicago, IL).
Sample Size Calculation
The sample size was calculated considering the ISH as the main response variable and its reduction with CTs (pre-HF or pre-HDF) compared with standard low-flux HD. An absolute 3% reduction in the dialysis sessions with ISH was considered as clinically relevant. The calculated sample size of 246 patients was based on a significance level (α error) of 0.05, a β error of 0.1, a power (1 − β) of 0.9, and an estimated dropout rate of 30%. For ruling out bias as a result of adaptation to the new technique and any possible carryover effect of previous treatments, the sessions that were considered in the analysis were those after the first 3 months of the experimental phase (evaluation phase). Moreover, patients who dropped out before the planned duration of the study (2 years) were considered for the analysis on the intention-to-treat basis, when their follow-up on the experimental phase was longer than 3 months.
Outcome Measures
The primary end point of the study was the possible beneficial effect of pure (HF) and/or mixed convection (HDF) compared with diffusion (HD) on cardiovascular stability of long-term dialysis patients with stage 5 CKD, estimated by the difference in the frequency of ISH between the evaluation period and the previous 2-month run-in period.
Disclosures
None.
Acknowledgments
Members of the Steering Committee are as follows: Francesco Locatelli (chairman: Lecco), Paolo Altieri (co-chairman: Cagliari), Simeone Andrulli (Lecco), Carlo Basile (Acquaviva delle Fonti), Piergiorgio Bolasco (Cagliari), Salvatore Di Filippo (Lecco), Mariano Feriani (Mestre), Luciano Alberto Pedrini (Seriate), Salvatore David (Parma), Antonio Santoro (Bologna), Francesco Pizzarelli (Firenze), and Carmine Zoccali (Reggio Calabria).
Simeone Andrulli (Lecco), Piergiorgio Bolasco (Cagliari), Salvatore Di Filippo (Lecco) were responsible for database and clinical record form; Giovanna Sau (Cagliari) and Simeone Andrulli (Lecco) were responsible for quality control; and Simeone Andrulli (Lecco) was responsible for statistical analysis.
The following centers participated in this study: Cagliari, S. Michele (Paolo Altieri, Giovanna Sau, Amalia P. Menneas, Cristìna M. Mereu, Valeria Matta, Roberto Sardara), Lecco (Francesco Locatelli, Celestina Manzoni, Salvatore Di Filippo, Simeone Andrulli, Marco Pozzi, Carla Maria Bigi, Angelo Pedraglio), Pavia, Fondazione Maugeri (Siro Segagni, Giuseppe Villa, Giovanni Montagna, Franca Dell'Acqua, Maria Tomaselli), Solofra (Raffaele Biagio Di Iorio), Quartu Sant'Elena (Piergiorgio Bolasco, Patrizia Scotto, Angelica M. Frongia, Giuseppe Peddio), Napoli, Federico II (Bruno Memoli, Alfredo Capuano, Vittorio Serio), Biella (Pietro Bajardi, Raffaella Cravero, Piero Dionisio, Cristina Zublena, Miriam Borin), Acireale (Giovanni Battaglia, Filippo Milone, Salvatore Urso, Maurizio Garozzo, Grazia D'Antonio, Margherita Saraceno), Alghero (Domenica Maria Casu, Angelo Piras), Cagliari, SS.Trinità (Rocco Ferrara, Isabella Pillosu), Aosta (Sandro Alloatti, Eugenio Pier Nebiolo, Valentina Pellu, Virna Paroli), Tempio Pausania (Mario Passaghe, Giorgio Chiarelli, Rita Cossu), Nuoro (Francesco Cadinu, Giovanni Mattana, Rita Pusceddu, Rosalia Pala, Susanna Fadda), Sorgono e Isili (Franco Logias, Paola Maria Esposito, Antonietta Musu, Marco Murru, Antioco Tolu, Loretta Noli, Franco Onali, Salvatore Serra), Melito e Scilla (Onofrio Marzolla, Eleonora Barreca), Pinerolo (Ugo Malcangi, Ernesto Reina), Ravenna (Maurizio Fusaroli, Augusto Montanari, Elisabetta Isola, Vasi Rosetta), Olbia (Gianfranco Fundoni, Lucia Burrai), Reggio Calabria (Carmine Zoccali, Giuseppe Curatola, Maurizio Postorino, Grazia Caridi, Pietro Romeo, Francesco Marino, Antonio Cogliandro, Francesco Siclari), Seriate (Alberto Luciano Pedrini, Pio Ruggiero), Acquaviva delle Fonti (Carlo Basile, Maurizio Antonelli, Maria Anna Avella, Michele Lassandro), Parma (Carlo Buzio, Salvatore David), Mantova (Renzo Tarchini, Cosimo Damiano Marseglia, Emanuela Bottini, Ernesto Talassi, Marisa Baruffaldi), Mestre (Mariano Feriani, Agostino Fracasso, Rosangela Genchi, Luigi Boldrin), Milano, Multimedica (Silvio Bertoli, Silvia Tedoldi, Giovanni Maio, Alberto Arienti), La Maddalena (Luanna Gazzanelli, Salvatorica Renga), Ozieri (Marino Ganadu, Luciangela Calvisi).
We thank all of the physicians, nurses, and patients of the participating centers for data recording and Gambro-Hospal for the logistic support given to the investigator meetings.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1. Andrulli S, Colzani S, Mascia F, Lucchi L, Stipo L, Bigi MC, Crepaldi M, Redaelli B, Albertazzi A, Locatelli F: The role of blood volume reduction in the genesis of intradialytic hypotension. Am J Kidney Dis 40: 1244–1254, 2002 [DOI] [PubMed] [Google Scholar]
- 2. Tislér A, Akócsi K, Borbás B, Fazakas L, Ferenczi S, Görögh S, Kulcsár I, Nagy L, Sámik J, Szegedi J, Tóth E, Wágner G, Kiss I: The effect of frequent or occasional dialysis-associated hypotension on survival of patients on maintenance haemodialysis. Nephrol Dial Transplant 18: 2601–2605, 2003 [DOI] [PubMed] [Google Scholar]
- 3. Altieri P, Sorba GB, Bolasco PG, Bostrom M, Asproni E, Ferrara R, Bolasco F, Cossu M, Cadinu F, Cabiddu GF, Casu D, Ganadu M, Passaghe P, Pinna M: On line predilution hemofiltration versus ultrapure high-flux hemodialysis: A multicenter prospective study in 23 patients. Blood Purif 15: 169–181, 1997 [DOI] [PubMed] [Google Scholar]
- 4. Altieri P, Sorba GB, Bolasco PG, Asproni E, Ledevo I, Cossu M, Ferrara R, Ganadu M, Cadinu M, Serra G, Cabiddu G, Sau G, Casu D, Passaghe M, Bolasco F, Pistis R, Ghisu T: Predilution haemofiltration: The Second Sardinian Multicentre Study—Comparison between haemofiltration and haemodialysis during identical Kt/V and session times in a long-term cross-over study. Nephrol Dial Transplant 16: 1207–1213, 2001 [DOI] [PubMed] [Google Scholar]
- 5. Hornberger JC, Chernew M, Petersen J, Garber AM: A multivariate analysis of mortality and hospital admissions with high flux dialysis. J Am Soc Nephrol 3: 1227–1237, 1992 [DOI] [PubMed] [Google Scholar]
- 6. Hakim RM, Held PJ, Stannard DC, Wolfe RA, Port FK, Daugirdas JT, Agodoa L: Effect of the dialysis membrane on mortality of chronic haemodialysis patients. Kidney Int 50: 566–570, 1996 [DOI] [PubMed] [Google Scholar]
- 7. Locatelli F, Marcelli D, Conte F, Limido A, Malberti F, Spotti D. Registro Lombardo Dialisi e Trapianto: Comparison of mortality in ESRD patients on convective and diffusive extracorporeal treatments. Kidney Int 55: 286–293, 1999 [DOI] [PubMed] [Google Scholar]
- 8. Leypoldt JK, Cheung AK, Carroll CE, Stannard DC, Pereira BJ, Agodoa LY, Port FK: Effect of dialysis membranes and middle molecule removal on chronic hemodialysis patient survival. Am J Kidney Dis 33: 349–355, 1999 [DOI] [PubMed] [Google Scholar]
- 9. Eknoyan G, Beck GJ, Cheung AK, Daugirdas JT, Greene T, Kusek JW, Allon M, Bailey J, Delmez JA, Depner TA, Dwyer JT, Levey AS, Levin NW, Milford E, Ornt DB, Rocco MV, Schulman G, Schwab SJ, Teehan BP, Toto R: Effect of dose and membrane flux in maintenance hemodialysis. N Engl J Med 347: 2010–2019, 2002 [DOI] [PubMed] [Google Scholar]
- 10. Locatelli F, Martin-Malo A, Hannedouche T, Loureiro A, Papadimitriou M, Wizemann V, Jacobson SH, Czekalski S, Ronco C, Vanholder R: Effect of membrane permeability on survival of hemodialysis patients. J Am Soc Nephrol 20: 645–654, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gotch FA, Sargent JA: A mechanistic analysis of the National Cooperative Dialysis Study (NCDS). Kidney Int 28: 526–534, 1985 [DOI] [PubMed] [Google Scholar]
- 12. Pedrini LA, De Cristofaro V: On-line mixed hemodiafiltration with a feedback for ultrafiltration control: Effect on middle-molecule removal. Kidney Int 64: 1505–1513, 2003 [DOI] [PubMed] [Google Scholar]
- 13. Cheung AK, Rocco MV, Yan G, Leypoldt JK, Levin NW, Greene T, Agodoa L, Bailey J, Beck GJ, Clark W, Levey AS, Ornt DB, Schulman G, Schwab S, Teehan B, Eknoyan G: Serum beta-2 microglobulin levels predict mortality in dialysis patients: Results of the HEMO study. J Am Soc Nephrol 17: 546–555, 2006 [DOI] [PubMed] [Google Scholar]
- 14. Hakim RM: Clinical implications of hemodialysis membrane biocompatibility. Kidney Int 44: 484–494, 1993 [DOI] [PubMed] [Google Scholar]
- 15. Locatelli F, Mastrangelo F, Redaelli B, Ronco C, Marcelli D, La Greca G, Orlandini G: Italian Cooperative Dialysis Group: Effect of different membranes and dialysis technologies on patient treatment tolerance and nutritional parameters. Kidney Int 50: 1293–1302, 1996 [DOI] [PubMed] [Google Scholar]
- 16. Canaud B, Bragg-Gresham JL, Marshall MR, Desmeules S, Gillespie BW, Depner T, Klassen P, Port FK: Mortality risk for patients receiving hemodiafiltration versus hemodialysis: European results from the DOPPS. Kidney Int 69: 2087–2093, 2006 [DOI] [PubMed] [Google Scholar]
- 17. Altieri P, Sorba G, Bolasco P, Ledebo I, Ganadu M, Ferrara R, Menneas A, Asproni E, Casu D, Passaghe M, Sau G, Cadinu F: Comparison between hemofiltration and hemodiafiltration in a long-term prospective cross-over study. Sardinian Study Group on Hemofiltration On-line. J Nephrol 17: 414–422, 2004 [PubMed] [Google Scholar]
- 18. Ledebo I: Predilution hemofiltration: A new technology applied to an old therapy. Int J Artif Organs 18: 735–742, 1995 [PubMed] [Google Scholar]
- 19. David S, Boström M, Cambi V: Predilution hemofiltration: Clinical experience and removal of small molecular weight solutes. Int J Artif Organs 18: 743–750, 1995 [PubMed] [Google Scholar]
- 20. Pedrini LA, Feliciani A, Zerbi S, Cozzi G, Ruggiero P: Optimization of mid-dilution haemodiafiltration: Technique and performance. Nephrol Dial Transplant 24: 2816–2824, 2009 [DOI] [PubMed] [Google Scholar]
- 21. David S, Tagliavini D, Cambi V: Pre-postdilution haemofiltration. Nephrol Dial Transplant 4: 37–40, 1989 [PubMed] [Google Scholar]
- 22. Quellhorst EA, Schuenemann B, Mietzsch G: Long-term hemofiltration in “poor risk” patients. ASAIO Trans 33: 758–764, 1987 [PubMed] [Google Scholar]
- 23. Di Filippo S, Manzoni C, Andrulli S, Tentori F, Locatelli F: Sodium removal during pre-dilution haemofiltration. Nephrol Dial Transplant 18[Suppl 7]: 31–36, 2003 [DOI] [PubMed] [Google Scholar]
- 24. Sherman RA, Rubin MP, Cody RP, Eisinger RP: Amelioration of hemodialysis-associated hypotension by the use of cool dialysate. Am J Kidney Dis 5: 124–127, 1985 [DOI] [PubMed] [Google Scholar]
- 25. Maggiore Q, Pizzarelli F, Santoro A, Panzetta G, Bonforte G, Hannedouche T, Alvarezde Lara MA, Tsouras I, Loureiro A, Ponce P, Sulkova S, van Roost G, Brink H, Kwan JT: The effects of control of thermal balance on vascular stability in hemodialysis patients: Results of the European randomized clinical trial. Am J Kidney Dis 40: 280–290, 2002 [DOI] [PubMed] [Google Scholar]
- 26. van der Sande FM, Wystrychowski G, Kooman JP, Rosales L, Raimann J, Kotanko P, Carter M, Chan CT, Leunissen KM, Levin NW: Control of core temperature and blood pressure stability during hemodialysis. Clin J Am Soc Nephrol 4: 93–98, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Donauer J, Schweiger C, Rumberger B, Krumme B, Böhler J: Reduction of hypotensive side effects during online-haemodiafiltration and low temperature haemodialysis. Nephrol Dial Transplant 18: 1616–1622, 2003 [DOI] [PubMed] [Google Scholar]
- 28. Bolasco P, Altieri P, Andrulli S, Basile C, Di Filippo S, Feriani M, Pedrini L, Santoro A, Zoccali C, Sau G, Locatelli F: Convection versus diffusion in dialysis: An Italian prospective multicentre study. Nephrol Dial Transplant 18[Suppl 7]: 50–54, 2003 [DOI] [PubMed] [Google Scholar]
- 29. Daugirdas JT: Simplified equations for monitoring Kt/V, PCRn, eKt/V and ePCRn. Adv Ren Replace Ther 2: 295–304, 1995 [DOI] [PubMed] [Google Scholar]