Abstract
Limited health literacy is common in the United States and associates with poor clinical outcomes. Little is known about the effect of health literacy in patients with advanced kidney disease. In this prospective cohort study we describe the prevalence of limited health literacy and examine its association with the risk for mortality in hemodialysis patients. We enrolled 480 incident chronic hemodialysis patients from 77 dialysis clinics between 2005 and 2007 and followed them until April 2008. Measured using the Rapid Estimate of Adult Literacy in Medicine, 32% of patients had limited (<9th grade reading level) and 68% had adequate health literacy (≥9th grade reading level). Limited health literacy was more likely in patients who were male and non-white and who had fewer years of education. Compared with adequate literacy, limited health literacy associated with a higher risk for death (HR 1.54; 95% CI 1.01 to 2.36) even after adjustment for age, sex, race, and diabetes. In summary, limited health literacy is common and associates with higher mortality in chronic hemodialysis patients. Addressing health literacy may improve survival for these patients.
The worldwide epidemic of kidney disease continues to grow in parallel to chronic conditions such as diabetes, hypertension, and obesity.1 In the United States it is estimated by 2020 there will be more than 750,000 people with ESRD, and on the basis of current practice 68% will be treated with hemodialysis therapy.2 Kidney disease is the ninth leading cause of death in the United States, and despite advances in dialysis technology and treatment of associated conditions such as anemia, mineral metabolism, and malnutrition, mortality risk, both cardiovascular and noncardiovascular, of chronic hemodialysis patients remains high—8 times greater than people in the general population.2–4 Early identification of hemodialysis patients with a higher risk for death is critical to customize therapies needed to reduce this risk, and identification of novel risk factors may guide new approaches to care delivery.
In the United States, 90 million people are estimated to have basic or below basic literacy skills.5 Health literacy, or the “ability to obtain, process, and understand basic health information to make appropriate health decisions about one's health and medical care,”6 has been associated with many health outcomes and characterized as contributing to disparities in health care. Limited health literacy has been associated with lower patients' knowledge of complex diseases, less self-care behaviors such as medication adherence, and also poorer clinical outcomes such as glycemic control in patients with diabetes.7–9
Recently, it was suggested that health literacy may be an important factor in the care of patients with kidney disease.10 There is little research characterizing health literacy, and examining the relationship between literacy and health outcomes, in patients with kidney disease. With an estimated 26 million people in the United States with chronic kidney disease,11 it is important to identify and establish all possible factors related to kidney disease progression, and to premature death in patients with advanced kidney disease. The objectives of this study were to characterize the prevalence and associated patient characteristics of limited health literacy, and to examine the risk of all-cause mortality by health literacy level in patients initiating chronic hemodialysis (HD) therapy.
RESULTS
In 480 incident chronic hemodialysis patients, the median age was 62.0 (interquartile range [IQR]: 51.0 to 72.0) years, 56% were male, 52% were white, and the median number of years of education was 12.0 (IQR: 11.0 to 13.0) (Table 1). Half of the patients had diabetes mellitus. The median Rapid Estimate of Adult Literacy in Medicine (REALM) score was 64 (IQR: 56 to 66), with 32% having a <9th grade reading level. At initiation, 78% of patients were using a catheter for dialysis access. Compared with those with adequate literacy skills, patients with limited health literacy were more likely to be male (58 versus 55%; P = 0.001), were less likely to be white (30 versus 63%; P < 0.001), have fewer years of education (11.0 [IQR: 8.0 to 12.0] versus 12.0 [IQR: 12.0 to 14.0]; P < 0.001), and have a lower serum albumin (3.5 [IQR: 3.0 to 3.9] versus 3.6 [3.2 to 3.9]; P = 0.066) (Table 1). There was no statistically significant difference in age, diabetes mellitus status, body mass index, or other clinical baseline laboratory measures by health literacy level. The only exception was for estimated dry weight, where those with limited health literacy had a lower dry weight than patients with adequate health literacy (76.8 [IQR: 64.0 to 92.0] versus 79.8 [IQR: 68.0 to 94.0]; P = 0.021), but in adjusted analyses this did not remain statistically significant (P = 0.66).
Table 1.
Patient characteristics associated with limited health literacy
| Characteristica | All Patients (n = 480) | Limited Health Literacy (<9th Grade) (n = 154) | Adequate Health Literacy (≥9th Grade) (n = 326) | P | Adjusted Pb |
|---|---|---|---|---|---|
| Age (years) | 62.0 [51.0, 72.0] | 64.0 [50.2, 72.0] | 60.0 [51.2, 71.8] | 0.947 | 0.742 |
| Male | 269 (56%) | 90 (58%) | 179 (55%) | 0.401 | 0.001 |
| White (n = 433) | 224 (52%) | 42 (30%) | 182 (63%) | <0.001 | <0.001 |
| Education (years) (n = 461) | 12.0 [11.0, 13.0] | 11.0 [8.0, 12.0] | 12.0 [12.0, 14.0] | <0.001 | <0.001 |
| Married | 219 (46%) | 57 (37%) | 162 (50%) | 0.001 | 0.022 |
| REALM [0 to 66] | 64.0 [56.0, 66.0] | ||||
| <9th grade reading level | 154 (32%) | ||||
| Diabetes mellitus | 239 (50%) | 69 (45%) | 170 (52%) | 0.113 | 0.436 |
| Body mass index (kg/m2) (n = 379) | 27.4 [23.5, 33.2] | 26.8 [23.3, 33.2] | 27.6 [23.7, 33.2] | 0.181 | 0.546 |
| Dry weight (kg) | 79.0 [65.5, 93.6] | 76.8 [64.0, 92.0] | 79.8 [68.0, 94.0] | 0.021 | |
| Kt/V (n = 447) | 1.4 [1.2, 1.6] | 1.4 [1.2, 1.6] | 1.4 [1.2, 1.6] | 0.838 | 0.724 |
| Albumin (g/dl) (n = 479) | 3.6 [3.1, 3.9] | 3.5 [3.0, 3.9] | 3.6 [3.2, 3.9] | 0.012 | 0.066 |
| Transferrin saturation (%) (n = 477) | 17.0 [14.0, 23.0] | 17.0 [14.0, 22.0] | 17.0 [13.0, 23.0] | 0.712 | |
| Hemoglobin (g/dl) | 10.7 [9.6, 11.9] | 10.8 [9.8, 12.0] | 10.7 [9.5, 11.8] | 0.510 | |
| Phosphorus (mg/dl) | 5.1 [4.1, 6.3] | 5.1 [4.0, 6.5] | 5.0 [4.2, 6.3] | 0.725 | |
| Calcium (mg/dl) (n = 479) | 8.7 [8.2, 9.2] | 8.8 [8.1, 9.2] | 8.7 [8.2, 9.2] | 0.274 | |
| Calcium/phosphorus product | 45.0 [36.5, 55.3] | 45.6 [36.1, 55.8] | 45.0 [36.9, 55.2] | 0.531 | |
| Intact-parathyroid hormone (pg/ml) (n = 470) | 217 [121, 406] | 217 [124, 388] | 217 [121, 418] | 0.455 | |
| Access (n = 473) | |||||
| catheter | 367 (78%) | 115 (75%) | 252 (79%) | 0.220 | |
| arteriovenous fistula or graft | 106 (22%) | 38 (25%) | 68 (21%) |
aMedian [IQR] or n (%).
bAdjusted for age, gender, race, education, marital status, diabetes mellitus status, body mass index, Kt/V, and serum albumin.
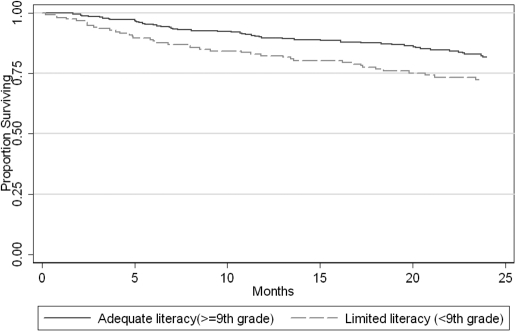
Through April 2008, there were 103 deaths (21%), 29 (6%) received a kidney transplant, and 18 (4%) were administratively censored because they were no longer cared for at a participating dialysis unit. Kaplan-Meier estimates of survival showed a higher risk of death in incident HD patients with limited health literacy compared with adequate health literacy (Figure 1). There is a significant difference in survival rates between the two groups (log-rank test: P = 0.029). Unadjusted Cox proportional hazard regression analysis showed that patients with limited health literacy had a risk of death 54% higher than patients with adequate literacy skills (hazard ratio [HR], 95% confidence interval [CI]: 1.54 [1.04 to 2.28]; P = 0.031) (Table 2). This persisted even after adjustment for age, sex, race, and diabetes (P = 0.043). If dialysis adequacy was included, similar results were obtained (P = 0.043). If baseline serum albumin was included in the model, the finding was also similar with a trend toward statistical significance (HR [95% CI]: 1.51 [0.99 to 2.30]; P = 0.057). When evaluated as a continuous measure, REALM score continued to be associated with mortality in this cohort. In adjusted analyses, each 10 point decrease in REALM score (with lower score indicating lower literacy skill) was associated with a 16% higher risk of death (HR [95% CI]: 1.16 [1.04 to 1.28]; P = 0.005) (Table 2). We also performed an analysis further adjusting for reported years of education. We found that limited literacy showed a similar association with mortality (HR [95% CI]: 1.13 [0.99 to 1.3]; P = 0.071) with a trend toward statistical significance.
Figure 1.
Kaplan-Meier survival estimates show a higher risk of death in those with limited literacy compared to adequate literacy.
Table 2.
Cox regression analysis of association between health literacy and mortality risk
| Health Literacy Level | Unadjusted HR [95% CI] | P | Adjusteda HR [95% CI] | P | Adjustedb HR [95% CI] | P |
|---|---|---|---|---|---|---|
| Limited literacy versus adequate literacy | 1.54 [1.04 to 2.28] | 0.031 | 1.54 [1.01 to 2.35] | 0.043 | 1.51 [0.99 to 2.30] | 0.057 |
| REALM score (per 10 points lower) | 1.18 [1.07 to 1.30] | 0.001 | 1.16 [1.04 to 1.29] | 0.005 | 1.15 [1.04 to 1.28] | 0.008 |
Limited literacy, <9th grade reading level; adequate literacy, ≥9th grade reading level.
aAdjusted for age (nonlinear), gender, race, and diabetes status.
bAdjusted for age (nonlinear), gender, race, diabetes status, and baseline serum albumin.
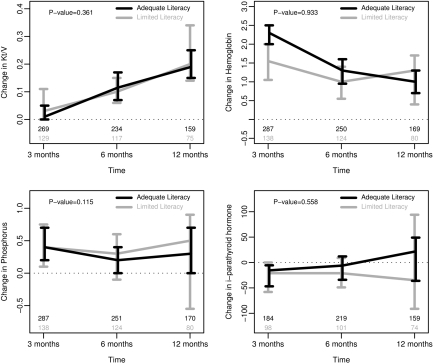
Several clinical laboratory measures are recommended as important target goals for optimal care and reduction in mortality risk for chronic HD patients, including dialysis adequacy (Kt/V), anemia, and bone-mineral assessments.12 Although there was a difference in baseline serum albumin by health literacy, there was no significant difference by health literacy level in the laboratory measures of Kt/V, hemoglobin, transferrin saturation, phosphorus, calcium, calcium-phosphorus product, or intact-parathyroid hormone at 3, 6, or 12 months after dialysis initiation. Additionally, there was no difference by health literacy level in the change of Kt/V, hemoglobin, phosphorus, or intact-parathyroid hormone over this period (Figure 2).
Figure 2.
Literacy does not associate with change in clinical outcomes at 3, 6, and 12 months after dialysis initiation: Kt/V, hemoglobin, phosphorus, and intact-parathyroid hormone. Medians and 95% bootstrap confidence intervals. Number values represent observations not missing for that time point. Models adjusted for age, race, and diabetes status.
DISCUSSION
Limited health literacy is common in patients initiating chronic hemodialysis therapy. Similar to other studies, participants in our sample who are male, who have fewer years of education, and who are of non-white race were more likely to have lower health literacy skills. To our knowledge this is the first study to examine the effect of health literacy on mortality risk in a cohort of patients recently initiated on hemodialysis. We found that lower health literacy is moderately associated with a higher risk of death and may be an important contributor to mortality in this high-risk patient population.
The prevalence of limited health literacy in our study is similar to that described in other, smaller studies in patients receiving dialysis,13,14 and also reflects findings similar to the general population. Because patients were administered the assessment of health literacy if they were suspected of having limited skills, then it is possible that this may be an overestimate of limited health literacy for the entire population of patients receiving chronic hemodialysis. The prevalence of limited health literacy among patients with less advanced chronic kidney disease remains unknown. Predictors of limited health literacy in hemodialysis patients, such as education and race, are similar to those in patients with other chronic diseases.15 Limited health literacy, potentially the result of limited access to health information and care, may be a significant barrier for patients to learn about their disease and may in part explain the racial disparities observed related to less knowledge about dialysis care.16,17
Health literacy has been associated with mortality in older patients within the general population.18,19 There are several possible mechanisms where a patient's literacy level may influence their health and mortality, such as increased knowledge about their disease, improved communication with their providers, and ultimately, greater self-efficacy and effective self-care related to kidney disease.10 Reading comprehension and health literacy may correspond to the self-care demands that are required in dialysis care, including adherence with complex medication and dialysis schedules, and following specific dietary recommendations. Greater patient dialysis knowledge may improve phosphate control, adherence to dialysis prescriptions, and type of dialysis access used.16,20,21 Print materials are commonly used to educate patients regarding self-care recommendations; however, many materials do not follow clear communication guidelines and are written at high reading levels, which may present a learning barrier for patients with limited health literacy.22
It has been previously suggested that evaluations of health literacy and a patient's reading ability may simply be a measurement of cognitive function, and therefore, it is poor cognitive function that is associated with a higher risk of mortality and not specifically health literacy.23,24 In a large international cohort of hemodialysis patients, a diagnosis of dementia has been shown to be associated with a 1.8-fold increased risk of death among incident patients and a 1.4-fold increased risk of death among prevalent dialysis patients.25 It is a limitation of this study that we do not have a specific measure of cognitive function. However, a previous study of 3260 community-dwelling older adults showed that both cognition and health literacy independently were significantly associated with mortality risk.26 It has been previously recommended not to adjust for educational attainment because of concerns about possible high collinearity between education and health literacy, and overfitting statistical models.27 Despite these concerns, years of education is the only proxy of cognitive function available in our study, and our findings remained similar.
Another consideration may be that patients with low heath literacy may be more likely to have more severe comorbid conditions that are in worse control compared with patients with adequate health literacy levels. This has been suggested in previous studies where patients with lower health literacy had worse glycemic control,9 more hospitalizations, and less participation in preventative health care such as cancer screening and vaccinations.7 In our cohort at enrollment, patients with lower health literacy did have a small, but significantly, lower serum albumin level. Although we adjusted for this difference in our analyses, the etiology of the lower serum albumin was not determined in this study. It may reflect several possible pathways, including higher levels of inflammation or malnutrition in patients with lower health literacy, that were not accounted for in this study. We did, however, evaluate other clinical assessments over time that have been associated with mortality risk including dialysis adequacy, anemia, and bone-mineral metabolism and none of these were found to differ by literacy level in this study. Therefore, despite similar laboratory quality measures patients with lower literacy were still more likely to die, suggesting that other areas of care need to be addressed to further reduce mortality risk in hemodialysis patients.
A known risk factor associated with higher mortality risk is presenting late for nephrology care before the initiation of dialysis therapy.28 It may be that patients with lower health literacy are less likely to be aware of their kidney disease, are less likely to be referred for nephrology care, and therefore present late for dialysis initiation. In a study of primary care patients who all either had or were at high risk of chronic kidney disease, low health literacy was independently associated with a low perceived susceptibility to chronic kidney disease.29 Our study is limited as we do not have a measure of nephrology care before initiation of dialysis, although it may be suggested that predialysis care may have been inadequate regardless of health literacy as the majority of patients initiated dialysis using a catheter rather than a permanent arteriovenous access.
Several other limitations to this study should be noted. First, there may be residual confounding variables related to health literacy and mortality in hemodialysis patients, such as comorbid conditions other than diabetes mellitus, which were not measured in this study. For example, the type of dialysis access used over the history of a patient's dialysis therapy may have an effect on mortality and may be associated with health literacy. We did not have this information available to include in this analysis. We did, however, adjust for serum albumin as a marker of overall nutritional status as this variable has been previously demonstrated to be associated with mortality in patients receiving hemodialysis.30–32 These adjustments had little effect on the association between limited literacy and higher risk of death in this study. Second, this study enrolled incident hemodialysis patients who were English-speaking and who were determined to be eligible for participation in an education and disease management program. Therefore, these findings may not be generalizable to all dialysis patients. Patients who do not speak English may have significant challenges navigating the health care system,33 including dialysis care, and further study is needed in this at-risk patient population.
Although health literacy appears to be an important predictor of poor health behaviors and outcomes, addressing health literacy is not the responsibility of patients but rather that of the multidisciplinary system of health care delivery. Several recent randomized trials of literacy and numeracy-sensitive interventions indeed suggest an improvement in diabetes mellitus, congestive heart failure, and depression care.34–36 Dialysis units and providers can improve communication to all patients by evaluating their practices to use clear communication strategies and to consider addressing health literacy in educational print materials as well as via oral communication.37
CONCLUSIONS
Our findings illustrate that limited health literacy among hemodialysis patients is common and is associated with a higher risk of death. As suggested by previous studies, limited health literacy may also be associated with other potentially important outcomes such as hospitalization, access to transplantation, and quality of life. Addressing health literacy may be an important avenue to ensure delivery, interpretation, and application of key clinical recommendations by patients to improve health outcomes in the care of those with complex kidney disease.
CONCISE METHODS
Setting and Study Participants
In this prospective cohort from May 2005 to February 2007, 2325 incident chronic HD patients were enrolled in a multidisciplinary case management program38 at 86 dialysis units from across the United States. Patients were selected if they were age 18 years or older and determined to be eligible to participate in a patient education program by local nephrology clinical care staff. Exclusion criteria included seasonal or transient patients, and those with a known diagnosis of severe cognitive impairment, or dementia, with the majority being nursing home residents. Also, patients who were non–English-speaking were excluded from this cohort. Participants were then followed until April 30, 2008. Health literacy was measured in patients where low health literacy was suspected by the case manager of the facility program, for example, when patients exhibited difficulty completing enrollment tasks. This study includes participants who remained on chronic hemodialysis (i.e., did not recover kidney function) and who were enrolled in the case management program within 90 days of dialysis initiation.
The Institutional Review Board of Vanderbilt University Medical Center approved this as an exempted study as all data were pre-existing in the clinical record before analysis.
Measures
Within 1 month of initiating hemodialysis, all baseline measures included in this study were collected. Participant demographic information was collected from the electronic medical record. Health literacy was assessed by trained clinical staff using REALM, a well-validated measure of reading ability that correlates with reading comprehension.39 Health literacy assessment was performed in a private clinic space either before, during, or after dialysis as preferred by the patient. Date of death was determined by the reporting of the individual dialysis units in the electronic medical record. Additional possible reasons for discontinuation of hemodialysis, such as transplantation, were also determined from the medical records. Clinical measures including hematocrit, serum albumin, phosphorus, transferrin saturation, and intact-parathyroid hormone were collected from the medical record at enrollment and 3, 6, and 12 months after hemodialysis initiation.
Statistical Analysis
Descriptive statistics of patient characteristics including health literacy level were performed and presented as either median (interquartile range) or proportion of the total patient population. We examined hemodialysis patient characteristics by comparing limited health literacy (REALM score 0 to 60: <9th grade reading level) to adequate health literacy (REALM score 61 to 66: ≥9th grade reading level) using proportional odds regression analyses. This allowed for determination of both unadjusted and adjusted associations between patient characteristics and health literacy. These analyses were then further adjusted for age, sex, race, education, diabetes mellitus status, marital status, body mass index, and either baseline hemodialysis adequacy (Kt/V) or serum albumin level.
Kaplan-Meier estimates of survival were compared by health literacy level. Log-rank test was used to determine statistical significance between the two groups. Cox proportional hazard regression analyses, adjusting for age, sex, race, and either serum albumin or Kt/V, were applied to describe limited health literacy and its association with the risk of death. These variables were selected based upon an a priori determined model and an evaluation of patient characteristics associated with limited health literacy. A sensitivity analysis was performed, adding years of education to the model, although it has been previously suggested not to adjust for education given its strong correlation with literacy and risk for overadjustment.27 Survival time was calculated from the date of entry into the cohort until death or last date of available follow-up data (April 30, 2008), when the patient was censored if they were alive. Patients were also censored if they received a kidney transplant, or were lost to follow-up because of a change in their dialysis unit. Literacy was quantified as both binary using an a priori defined cut-off level (<9th grade reading level versus ≥9th grade reading level) as this level has been previously demonstrated to affect health outcomes in diabetes,37 and also as a continuous variable based on the raw score of the REALM (range 0 to 66). Nonlinearity of the relationship between continuous REALM score and risk of death was examined and not observed in this analysis. Multiple imputation methods40 were used for missing values of race, albumin, and Kt/V. Because albumin was measured at 3, 6, 9, and 12 months in addition to baseline, we performed a sensitivity analysis modeling albumin as a time-varying covariate in the Cox regression. Results of this analysis remained similar to the main analysis (HR [95% CI]: 1.16 [1.05 to 1.29]; P = 0.005 for the effect of literacy). We also conducted a sensitivity analysis controlling for the effect of facility in the Cox regression. Frailty option was used in the Cox regression to model facility as a random effect. The results were very similar and the effect of literacy remained unchanged (HR [95% CI]: 1.17 [1.04 to 1.29]; P = 0.007). For Cox regression models there was no evidence of collinearity among covariates. All tests were two-tailed and a P value of <0.05 was considered statistically significant. All statistical analyses were performed with STATA 8.0 (StataCorp, College Station, TX) and R, version 2.6.0 (www.r-project.org).
DISCLOSURES
The funders of this study did not participate in the (1) design and conduct of the study, (2) collection, management, analysis, and interpretation of the data, nor (3) preparation, review, or approval of the manuscript. Although AMGEN supported the initial RightStart program, they did not provide support for this project, nor did they review the data, findings, or manuscript.
Acknowledgments
K.C. is supported by a National Kidney Foundation Young Investigator Grant and grant K23 DK080952-02, R.R. by grant K23DK065294, T.A.I. by grant K24 DK62849, and T. E. by grants K24 DK77875 and P60 DK 020593 from the National Institute of Diabetes and Digestive and Kidney Diseases. M.H. is supported by KL2 RR025006 from the National Center for Research Resources.
We thank James Thomas for assistance with data management.
Part of this material was presented in abstract form at the annual meetings of the American Society of Nephrology; October 31 through November 5, 2007; San Francisco, CA; and November 4 through 9, 2008; Philadelphia, PA.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1. Szczech LA, Harmon W, Hostetter TH, Klotman PE, Powe NR, Sedor JR, Smedberg P, Himmelfarb J: World Kidney Day 2009: Problems and challenges in the emerging epidemic of kidney disease. J Am Soc Nephrol 20: 453–455, 2009 [DOI] [PubMed] [Google Scholar]
- 2. Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Ishani A, Kasiske B, Liu J, Mau LW, McBean M, Murray A, St Peter W, Guo H, Li Q, Li S, Li S, Peng Y, Qiu Y, Roberts T, Skeans M, Snyder J, Solid C, Wang C, Weinhandl E, Zaun D, Arko C, Chen SC, Dalleska F, Daniels F, Dunning S, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L: United States Renal Data System 2008 Annual Data Report Abstract. Am J Kidney Dis 53[1 Suppl] : vi–vii, S8–S374, 2009 [DOI] [PubMed] [Google Scholar]
- 3. Heron MP, Hoyert DL, Murphy SL, Xu J, Kochaneck KD, Tejada-Vera B: Deaths: Final Data for 2006. Natl Vital Stat Rep 2009: 1–80, 2009 [PubMed] [Google Scholar]
- 4. de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LM, Ansell D, Collart F, Finne P, Heaf JG, De Meester J, Wetzels JF, Rosendaal FR, Dekker FW: Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA 302: 1782–1789, 2009 [DOI] [PubMed] [Google Scholar]
- 5. Kutner M, Greenberg E, Jin Y, Paulsen C: The Health Literacy of America's Adults: Results From the 2003 National Survey of Adult Literacy, Washington DC, National Center for Education Statistics, U.S. Department of Education, 2006. (NCES 2006-483) [Google Scholar]
- 6. Nielsen-Bohlman LT, Panzer AM, Hamlin B, Kindig DA. (Eds.): Health Literacy: A Prescription to End Confusion, Washington DC, Committee on Health Literacy, Board on Neuroscience and Behavioral Health, National Academies Press, 2004 [PubMed] [Google Scholar]
- 7. Dewalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP: Literacy and health outcomes: A systematic review of the literature. J Gen Intern Med 19: 1228–1239, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Osborn CY, Paasche-Orlow MK, Davis TC, Wolf MS: Health literacy: An overlooked factor in understanding HIV health disparities. Am J Prev Med 33: 374–378, 2007 [DOI] [PubMed] [Google Scholar]
- 9. Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, Palacios J, Sullivan GD, Bindman AB: Association of health literacy with diabetes outcomes. JAMA 288: 475–482, 2002 [DOI] [PubMed] [Google Scholar]
- 10. Devraj R, Gordon EJ: Health literacy and kidney disease: Toward a new line of research. Am J Kidney Dis 53: 884–889, 2009 [DOI] [PubMed] [Google Scholar]
- 11. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS: Prevalence of chronic kidney disease in the United States. JAMA 298: 2038–2047, 2007 [DOI] [PubMed] [Google Scholar]
- 12. Rocco MV, Frankenfield DL, Hopson SD, McClellan WM: Relationship between clinical performance measures and outcomes among patients receiving long-term hemodialysis. Ann Intern Med 145: 512–519, 2006 [DOI] [PubMed] [Google Scholar]
- 13. Grubbs V, Gregorich SE, Perez-Stable EJ, Hsu CY: Health literacy and access to kidney transplantation. Clin J Am Soc Nephrol 4: 195–200, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pollock JB, Jaffery JB: Knowledge of phosphorus compared with other nutrients in maintenance dialysis patients. J Ren Nutr 17: 323–328, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Paasche-Orlow MK, Parker RM, Gazmararian JA, Nielsen-Bohlman LT, Rudd RR: The prevalence of limited health literacy. J Gen Intern Med 20: 175–184, 2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Cavanaugh KL, Wingard RL, Hakim RM, Elasy TA, Ikizler TA: Patient dialysis knowledge is associated with permanent arteriovenous access use in chronic hemodialysis. Clin J Am Soc Nephrol 4: 950–956, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Finkelstein FO, Story K, Firanek C, Barre P, Takano T, Soroka S, Mujais S, Rodd K, Mendelssohn D: Perceived knowledge among patients cared for by nephrologists about chronic kidney disease and end-stage renal disease therapies. Kidney Int 74: 1178–1184, 2008 [DOI] [PubMed] [Google Scholar]
- 18. Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J: Health literacy and mortality among elderly persons. Arch Intern Med 167: 1503–1509, 2007 [DOI] [PubMed] [Google Scholar]
- 19. Sudore RL, Yaffe K, Satterfield S, Harris TB, Mehta KM, Simonsick EM, Newman AB, Rosano C, Rooks R, Rubin SM, Ayonayon HN, Schillinger D: Limited literacy and mortality in the elderly: The health, aging, and body composition study. J Gen Intern Med 21: 806–812, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Ford JC, Pope JF, Hunt AE, Gerald B: The effect of diet education on the laboratory values and knowledge of hemodialysis patients with hyperphosphatemia. J Ren Nutr 14: 36–44, 2004 [DOI] [PubMed] [Google Scholar]
- 21. Juergensen PH, Gorban-Brennan N, Finkelstein FO: Compliance with the dialysis regimen in chronic peritoneal dialysis patients: Utility of the pro card and impact of patient education. Adv Perit Dial 20: 90–92, 2004 [PubMed] [Google Scholar]
- 22. Hill-Briggs F, Smith AS: Evaluation of diabetes and cardiovascular disease print patient education materials for use with low-health literate populations. Diabetes Care 31: 667–671, 2008 [DOI] [PubMed] [Google Scholar]
- 23. Barnes DE, Tager IB, Satariano WA, Yaffe K: The relationship between literacy and cognition in well-educated elders. J Gerontol A Biol Sci Med Sci 59: 390–395, 2004 [DOI] [PubMed] [Google Scholar]
- 24. Manly JJ, Schupf N, Tang MX, Stern Y: Cognitive decline and literacy among ethnically diverse elders. J Geriatr Psychiatry Neurol 18: 213–217, 2005 [DOI] [PubMed] [Google Scholar]
- 25. Kurella M, Mapes DL, Port FK, Chertow GM: Correlates and outcomes of dementia among dialysis patients: The Dialysis Outcomes and Practice Patterns Study. Nephrol Dial Transplant 21: 2543–2548, 2006 [DOI] [PubMed] [Google Scholar]
- 26. Baker DW, Wolf MS, Feinglass J, Thompson JA: Health literacy, cognitive abilities, and mortality among elderly persons. J Gen Intern Med 23: 723–726, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. DeWalt DA, Pignone MP: Reading is fundamental: The relationship between literacy and health. Arch Intern Med 165: 1943–1944, 2005 [DOI] [PubMed] [Google Scholar]
- 28. Kinchen KS, Sadler J, Fink N, Brookmeyer R, Klag MJ, Levey AS, Powe NR: The timing of specialist evaluation in chronic kidney disease and mortality. Ann Intern Med 137: 479–486, 2002 [DOI] [PubMed] [Google Scholar]
- 29. Boulware LE, Carson KA, Troll MU, Powe NR, Cooper LA: Perceived susceptibility to chronic kidney disease among high-risk patients seen in primary care practices. J Gen Intern Med 10: 1123–1129, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Foley RN, Parfrey PS, Harnett JD, Kent GM, Murray DC, Barre PE: Hypoalbuminemia, cardiac morbidity, and mortality in end-stage renal disease. J Am Soc Nephrol 7: 728–736, 1996 [DOI] [PubMed] [Google Scholar]
- 31. Kalantar-Zadeh K, Kilpatrick RD, Kuwae N, McAllister CJ, Alcorn H, Jr, Kopple JD, Greenland S: Revisiting mortality predictability of serum albumin in the dialysis population: time dependency, longitudinal changes and population-attributable fraction. Nephrol Dial Transplant 20: 1880–1888, 2005 [DOI] [PubMed] [Google Scholar]
- 32. Owen WF, Jr, Lew NL, Liu Y, Lowrie EG, Lazarus JM: The urea reduction ratio and serum albumin concentration as predictors of mortality in patients undergoing hemodialysis. N Engl J Med 329: 1001–1006, 1993 [DOI] [PubMed] [Google Scholar]
- 33. Pearson WS, Ahluwalia IB, Ford ES, Mokdad AH: Language preference as a predictor of access to and use of healthcare services among Hispanics in the United States. Ethn Dis 18: 93–97, 2008 [PubMed] [Google Scholar]
- 34. Cavanaugh K, Wallston KA, Gebretsadik T, Shintani A, Huizinga MM, Davis D, Gregory RP, Malone R, Pignone M, Dewalt D, Elasy TA, Rothman RL: Addressing literacy and numeracy to improve diabetes care: Two randomized controlled trials. Diabetes Care 32: 2149–2155, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. DeWalt DA, Malone RM, Bryant ME, Kosnar MC, Corr KE, Rothman RL, Sueta CA, Pignone MP: A heart failure self-management program for patients of all literacy levels: A randomized, controlled trial [ISRCTN11535170]. BMC Health Serv Res 6: 30, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, Weinberger M, Pignone M: Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA 292: 1711–1716, 2004 [DOI] [PubMed] [Google Scholar]
- 37. Paasche-Orlow MK, Schillinger D, Greene SM, Wagner EH: How health care systems can begin to address the challenge of limited literacy. J Gen Intern Med 21: 884–887, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Wingard RL, Pupim LB, Krishnan M, Shintani A, Ikizler TA, Hakim RM: Early intervention improves mortality and hospitalization rates in incident hemodialysis patients: RightStart program. Clin J Am Soc Nephrol 2: 1170–1175, 2007 [DOI] [PubMed] [Google Scholar]
- 39. Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, Crouch MA: Rapid estimate of adult literacy in medicine: a shortened screening instrument. Fam Med 25: 391–395, 1993 [PubMed] [Google Scholar]
- 40. Harrell FE: Regression Modeling Strategies: With Applications to Linear Models, Logistic Regression and Survival Analysis, New York, Springer-Verlag, 2001 [Google Scholar]