Abstract
Whether preoperative proteinuria associates with adverse renal outcomes after cardiac surgery is unknown. Here, we performed a secondary analysis of a prospectively enrolled cohort of adult patients undergoing coronary artery bypass grafting (CABG) at a medical center and its two affiliate hospitals between 2003 and 2007. We excluded patients with stage 5 CKD or those who received dialysis previously. We defined proteinuria, measured with a dipstick, as mild (trace to 1+) or heavy (2+ to 4+). Among a total of 1052 patients, cardiac surgery–associated acute kidney injury (CSA-AKI) developed in 183 (17.4%) patients and required renal replacement therapy (RRT) in 50 (4.8%) patients. In a multiple logistic regression model, mild and heavy proteinuria each associated with an increased odds of CSA-AKI, independent of CKD stage and the presence of diabetes mellitus (mild: OR 1.66, 95% CI 1.09 to 2.52; heavy: OR 2.30, 95% CI 1.35 to 3.90). Heavy proteinuria also associated with increased odds of postoperative RRT (OR 7.29, 95% CI 3.00 to 17.73). In summary, these data suggest that preoperative proteinuria is a predictor of CSA-AKI among patients undergoing CABG.
Cardiac surgery–associated acute kidney injury (CSA-AKI) is one of the most significant and severe complications that can occur after cardiac surgery. The incidence of CAS-AKI is estimated to be 1% to 30%, on the basis of the definition used.1 The most severe form of CSA-AKI, requiring renal replacement therapy (RRT), leads to a mortality rate as high as 50% to 60%.1 In addition, even mild elevation of serum creatinine after surgery carries a significant risk of an adverse outcome.2 The development of AKI is associated with substantial cardiac surgery–associated morbidity and mortality independent of all other factors.1 In clinical practice, the most commonly used marker for renal function is serum creatinine level or estimated GFR (eGFR). Assessment of renal function, however, should not be limited to eGFR alone. On the basis of experience with chronic kidney disease (CKD), proteinuria (detected either by dipstick tests or albumin-creatinine ratios [ACR]) has been shown to be strongly associated with adverse outcomes, including renal disease progression, cardiovascular events, and long-term mortality.3–5 The widely used National Kidney Foundation staging system for CKD includes proteinuria only in the early stages (stage 1 and stage 2) and does not further classify the patients with proteinuria in advanced stages.6 Recent reports from large epidemiologic studies have shown that patients with proteinuria have a higher risk of adverse outcomes than those without proteinuria within the same CKD stage.7,8 These reports suggested that GFR and proteinuria should be used together to identify patients at risk.7,8 These findings may influence future modification of CKD staging systems and possibly improve the accuracy of CKD staging.
In CSA-AKI, the association between preoperative proteinuria, a marker of renal dysfunction, and renal outcome has not been systemically examined in the medical literature. We test the hypothesis that preoperative proteinuria is also associated with postoperative renal dysfunction, independent of preoperative eGFR and other comorbidities in patients undergoing cardiac surgery.
RESULTS
Among the 1235 adult patients who underwent coronary artery bypass grafting (CABG) during the period of January 2003 and December 2007, 50 patients had received dialysis before surgery, 36 patients were already CKD stage 5 before surgery, and 97 patients did not have urinalysis measurements before surgery. Thus, only 1052 patients were eligible in the final analysis. Their demographic characteristics are presented in Table 1.
Table 1.
Basic patient demographic characteristics, classified with estimated GFR or proteinuria
| All (n = 1052) | CKD Stage |
Proteinuria on Dipstick |
|||||
|---|---|---|---|---|---|---|---|
| Preserved eGFR (n = 631) | Stage 3 (n = 359) | Stage 4 (n = 62) | None (n = 599) | Mild (n = 315) | Heavy (n = 138) | ||
| Patient characteristics | |||||||
| male gender | 75.7% | 82.4% | 68.2%c | 50.0%c | 80.0% | 73.7%a | 61.6%c |
| age (years) | 65.7 ± 11.0 | 63.2 ± 11.3 | 69.7 ± 9.0c | 67.7 ± 11.5b | 64.8 ± 11.3 | 67.2 ± 10.4b | 66.0 ± 10.8 |
| BMI (kg/m2) | 25.0 ± 4.1 | 25.1 ± 3.6 | 25.0 ± 4.8 | 24.4 ± 5.3 | 25.1 ± 3.7 | 25.3 ± 4.4 | 24.7 ± 5.3a |
| Comorbidities | |||||||
| LVEF <60% | 47.6% | 42.6% | 51.0%a | 79.0%c | 41.7% | 51.4%b | 64.5%c |
| hypertension | 66.5% | 64.2% | 70.5%a | 67.7% | 65.4% | 66.7% | 71.0% |
| DM | 41.2% | 35.0% | 47.9%c | 64.5%c | 32.4% | 44.4%c | 71.7%c |
| PAD | 8.7% | 6.7% | 9.5% | 25.8%c | 6.5% | 8.6% | 18.8%c |
| CVA | 2.1% | 1.6% | 2.8% | 3.2% | 1.8% | 2.9% | 1.4% |
| CHF | 14.0% | 10.1% | 17.5%b | 32.3%c | 9.0% | 17.5%c | 27.5%c |
| COPD | 8.0% | 7.3% | 9.5% | 6.5% | 7.5% | 10.5% | 4.3% |
| recent MI | 18.8% | 16.6% | 20.6% | 30.6%b | 15.9% | 24.1%b | 19.6% |
| Perioperative condition | |||||||
| vasopressor dependence | 3.6% | 2.7% | 4.2% | 9.7% | 2.2% | 5.7%b | 5.1% |
| IABP | 8.0% | 6.8% | 9.2% | 12.9% | 6.7% | 7.9% | 13.8%b |
| ECMO | 3.9% | 3.0% | 4.7% | 8.1% | 2.8% | 4.8% | 6.5%a |
| nonelective surgery | 12.6% | 11.1% | 14.4% | 17.7%a | 8.2% | 18.6%c | 18.1%b |
| cardiopulmonary bypass | 13.9% | 12.2% | 15.0% | 24.2%a | 11.5% | 16.5%a | 18.1%a |
| aortic cross clamp time (min), (n) | 105 ± 42 | 80 ± 38 | 104 ± 60 | 105 ± 25 | 109 ± 69 | 109 ± 40 | 98 ± 29 |
| (34) | 18 | 13 | 3 | 13 | 16 | 5 | |
| cardiopulmonary bypass (min), (n) | 127 ± 57 | 128 ± 52 | 125 ± 73 | 129 ± 47 | 127 ± 62 | 130 ± 66 | 122 ± 35 |
| (146) | 81 | 49 | 16 | 63 | 55 | 28 | |
| Preoperative laboratory data | |||||||
| creatinine (mg/dl) | 1.26 ± 0.47 | 1.01 ± 0.16 | 1.47 ± 0.39c | 2.60 ± 0.53c | 1.16 ± 0.36 | 1.28 ± 0.42c | 1.67 ± 0.71c |
| eGFR (MDRD) | 64.5 ± 21.5 | 78.0 ± 14.8 | 47.7 ± 8.5c | 23.6 ± 4.0c | 69.6 ± 19.1 | 61.9 ± 21.5c | 48.4 ± 22.4c |
| hemoglobin (g/dl) | 12.9 ± 1.92 | 13.4 ± 1.6 | 12.4 ± 2.1c | 11.2 ± 1.9c | 13.2 ± 1.8 | 12.9 ± 2.0a | 11.9 ± 2.1c |
COPD, chronic obstructive pulmonary disease. Comparison of demographic characteristics of patients with preserved estimated GFR (≥60 ml/min per 1.73 m2) or no proteinuria:
aP < 0.05.
bP < 0.01.
cP < 0.001.
Patients with Impaired Renal Function (Low eGFR or Proteinuria)
Patients were stratified according to CKD stage or severity of proteinuria (Table 1). On the basis of the value of eGFR, 359 (34.1%) patients were classified as CKD stage 3, whereas 62 (5.9%) patients were classified as stage 4. According to univariate analysis, the patients with stage 3 CKD were more likely to be women and older and to have a lower hemoglobin concentration. They were also more likely to have impaired heart contractility, hypertension, diabetes mellitus (DM), and congestive heart failure (CHF) than patients with stage 1 or stage 2 CKD. Patients with stage 4 CKD were significantly older, and more likely to be women. The percentage of patients with impaired left ventricular contractility, DM, peripheral artery disease (PAD), anemia, CHF, and recent myocardial infarction (MI) was also higher than the percentage of patients with preserved GFR.
A total of 315 (29.9%) patients had mild proteinuria before surgery and 138 (13.1%) patients had heavy proteinuria. Those with mild proteinuria were more likely to be female and older. They were also more likely to have impaired heart contractility, DM, CHF, and recent MI. They were also more likely to receive vasopressors, to undergo nonelective surgery, and to receive cardiopulmonary bypass (CPB). These patients also had significantly lower eGFR and hemoglobin (Hb) than patients without proteinuria. Patients with heavy proteinuria were more likely to be female and have larger body mass index (BMI). They also had impaired heart contractility, DM, PAD, and CHF, and were more likely to require perioperative CPB, intra-aortic balloon pump (IABP), or extracorporeal membrane oxygenation (ECMO). In addition, their baseline creatinine levels were significantly higher and they tended to be anemic.
The percentage of patients with proteinuria in each category of CKD stage is listed in Table 2. In patients with preserved eGFR, 167 (26.5%) patients had mild proteinuria and 41 (6.5%) patients had heavy proteinuria. In stage 3 CKD patients, 133 (37.0%) had mild proteinuria and 65 (18.1%) had heavy proteinuria, and in stage 4 patients, 15 (24.2%) had mild proteinuria and 32 (51.6%) had heavy proteinuria.
Table 2.
Percentage of patients with proteinuria in groups stratified by CKD stage
| CKD Stages | Normal | Mild Proteinuria | Heavy Proteinuria | Subtotal |
|---|---|---|---|---|
| Preserved eGFR | 423 (67.0%) | 167 (26.5%) | 41 (6.5%) | 631 |
| Stage 3 | 161 (44.8%) | 133 (37.0%) | 65 (18.1%) | 359 |
| Stage 4 | 15 (24.2%) | 15 (24.2%) | 32 (51.6%) | 62 |
Preserved eGFR, eGFR ≥60 ml/min per 1.73 m2; stage 3, 30 to 59.9 ml/min per 1.73 m2; stage 4, 15 to 29.9 ml/min per 1.73 m2.
Adverse Outcomes
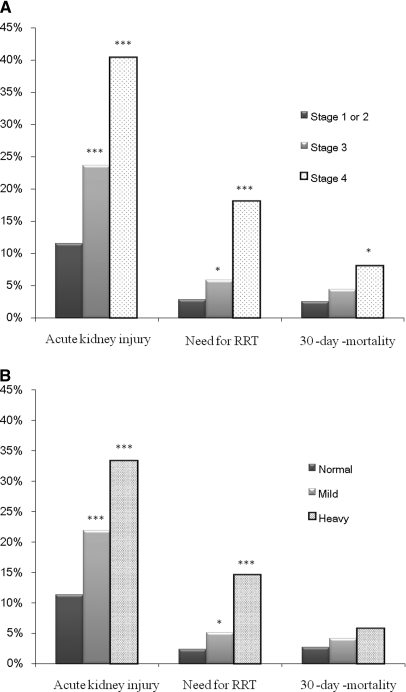
The unadjusted risk for catastrophic outcomes such as postoperative AKI and RRT were highest in patients with heavy proteinuria (Figure 1A) or lowest eGFR (Figure 1B). The risk stepped up for each corresponding classification.
Figure 1.
Unadjusted risk for postoperative AKI, RRT, and 30-day all-cause mortality in patients with different severities of proteinuria and CKD stage. The unadjusted risk for adverse outcomes (AKI, RRT, and 30-day all-cause mortality) increased stepwise in each group of CKD stage (A) and severity of proteinuria (B). Comparison of patients with CKD stage 4 or normal proteinuria: *P < 0.05; ***P < 0.001.
We further stratified patients by CKD stage and degree of proteinuria. Patients with preserved eGFR and without proteinuria had the lowest rates of postoperative AKI (9.5%) and RRT (1.4%). The severity of proteinuria showed a dose response–type increasing risk for AKI and for RRT in patients with preserved eGFR, and CKD stage 3, but not for stage 4. When we focused on mortality as the endpoint, this effect only appeared in patients with preserved eGFR. The details of adverse outcomes in each group of patients are presented in Table 3.
Table 3.
Adverse outcomes in 1051 patients with CABG with various CKD stages and degrees of proteinuria
| CKD Stages | Outcomes |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AKI (n = 183) |
Need for RRT (n = 50) |
30-Day Mortality (n = 37) |
||||||||||
| Normal | Mild | Heavy | Pb | Normal | Mild | Heavy | Pb | Normal | Mild | Heavy | Pb | |
| Preserved eGFR (n = 631) | 9.5% | 13.8% | 24.4% | 0.010 | 1.4% | 4.2% | 12.2% | 0.001 | 2.1% | 1.8% | 9.8% | 0.010 |
| Stage 3 (n = 359) | 13.0% | 30.1% | 36.9% | 0.001 | 3.1% | 6.0% | 12.3% | 0.029 | 3.1% | 6.8% | 3.1% | 0.266 |
| Stage 4 (n = 62) | 46.7% | 40.0% | 37.5% | 0.836 | 20.0% | 6.7% | 22.6% | 0.410 | 13.3% | 6.7% | 6.3% | 0.690 |
| Pa | 0.008 | 0.009 | 0.349 | 0.006 | 0.743 | 0.359 | 0.028 | 0.029 | 0.355 | |||
Preserved eGFR, eGFR ≥60 ml/min per 1.73 m2. P, the tests for linear trend across CKD categories (Pa) and across proteinuria categories (Pb).
Multivariate Stepwise Logistic Regression Model for Postoperative AKI
We included variables listed in Table 1 into regression analysis to identify important factors associated with postoperative AKI. CKD stages were used to be representative of preoperative renal function, as stated in Concise Methods. As presented in Table 4, the stepwise logistic regression model revealed that mild proteinuria (odds ratio [OR] = 1.66, P = 0.018), heavy proteinuria (OR = 2.30, P = 0.01), stage 3 CKD (OR = 1.68, P = 0.021), and stage 4 CKD (OR = 3.01, P < 0.001) were significantly associated with postoperative AKI. In addition, the interaction terms between CKD and proteinuria (P = 0.161), CKD and DM (P = 0.593), and proteinuria and DM (P = 0.530) did not show significant effects on CSI-AKI. The final multiple logistic regression model had a high discrimination power (estimated area under the curve of receiver operating characteristics [eAUC-ROC] = 0.82) and it fitted the observed binary data well (adjusted generalized R2 = 0.30 and Hosmer-Lemeshow goodness of fit [GOF] test P = 0.94).
Table 4.
Factors associated with postoperative acute kidney injury defined by the Acute Kidney Injury Network Criteria (n = 1052)
| Covariate | OR (95% CI) | P |
|---|---|---|
| Age (years) | 1.03 (1.01 to 1.05) | 0.001 |
| DM | 1.66 (1.14 to 2.44) | <0.001 |
| Recent MI | 1.78 (1.16 to 2.72) | 0.009 |
| IABP | 3.56 (1.83 to 6.96) | <0.001 |
| Nonelective surgery | 3.66 (2.15 to 6.25) | <0.001 |
| Proteinuria | ||
| no proteinuria | 1 | |
| mild proteinuria | 1.66 (1.09 to 2.52) | 0.018 |
| heavy proteinuria | 2.30 (1.35 to 3.90) | 0.002 |
| CKD stage | ||
| preserved eGFR | 1 | |
| stage 3 | 1.68 (1.12 to 2.52) | 0.012 |
| stage 4 | 3.01 (1.57 to 6.03) | 0.001 |
Preserved eGFR, eGFR ≥60 ml/min per 1.73 m2. Mild proteinuria was defined as +/− to 1+ on urine dipstick examination; heavy proteinuria was defined as 2+ to 4+ on urine dipstick examination. Multiple logistic regression model: n = 1052, adjusted generalized R2 = 0.30, estimated area under the ROC curve = 0.82, and Hosmer-Lemeshow goodness-of-fit test P = 0.94 > 0.05 (degree of freedom = 8).
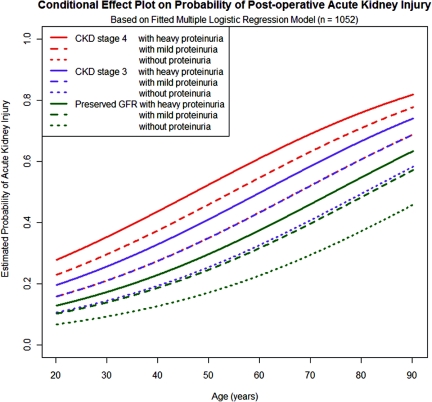
We did a conditional effect plot of the estimated risk for postoperative AKI against patient's age, stratified by CKD stage and severity of proteinuria, and with the values of the other factors fixed as drawn in Figure 2. The risk of postoperative AKI was the highest in patients with stage 4 CKD and heavy proteinuria and the lowest in patients with preserved eGFR and without proteinuria. The risk of postoperative AKI for patients with preserved eGFR and mild proteinuria was comparable to that for patients with stage 3 CKD without proteinuria. Similarly, those with stage 3 CKD and mild proteinuria had the risk of postoperative AKI comparable to patients with stage 4 CKD without proteinuria.
Figure 2.
Conditional effect plot of baseline CKD stage and severity of proteinuria on estimated probability of AKI in 1052 patients with postcoronary artery bypass grafting surgery. The condition effect plot was drawn under the following conditions: patients with diabetes mellitus, recent myocardial infarction, and nonelective surgery but without IABP. Patients with mild or heavy proteinuria had a higher risk of postoperative AKI, even after adjusting for CKD stage.
Multivariate Stepwise Logistic Regression Model for Postoperative RRT
We did another regression analysis with variables listed in Table 1, to identify important factors associated with postoperative RRT. Also, preoperative CKD stages were used to be representative of preoperative renal function. In the final model, heavy proteinuria (OR = 7.29, P = 0.004) was significantly associated with postoperative RRT (Table 5) but not for mild proteinuria (OR = 1.443, 95% confidence interval [CI] 0.596 to 3.499, P = 0.416). The other significant factors associated with postoperative RRT were older age, low left ventricular ejection fraction (LVEF), ECMO, nonelective surgery, and use of CPB. The final multiple logistic regression model had a very high discrimination power (eAUC-ROC = 0.93) and it fitted the observed binary data quite well (adjusted generalized R2 = 0.47 and Hosmer-Lemeshow GOF test P = 0.26). Heavy proteinuria was associated with a higher risk of postoperative RRT than those with DM alone, whereas the values of the other factors were held fixed.
Table 5.
Factors associated with postoperative AKI needing RRT (n = 1052)
| Covariate | Odds Ratio (95% CI) | P |
|---|---|---|
| Age (years) | 1.06 (1.02 to 1.10) | 0.003 |
| Low LVEF | 3.31 (1.36 to 8.79) | 0.009 |
| ECMO | 15.75 (6.01 to 41.26) | <0.001 |
| Nonelective surgery | 6.49 (2.84 to 14.86) | <0.001 |
| Cardiopulmonary bypass | 3.90 (1.86 to 8.20) | <0.001 |
| Heavy proteinuria | 7.29 (3.00 to 17.73) | <0.001 |
Low LVEF, defined as <60%. Heavy proteinuria was defined as 2+ to 4+ on urine dipstick examination. Multiple logistic regression model: n = 1052, adjusted generalized R2 = 0.469, estimated area under the ROC curve = 0.93, and Hosmer-Lemeshow goodness-of-fit test P = 0.26 > 0.05 (degree of freedom = 8).
Several sensitivity analyses were undertaken. We compared the characteristics of the 97 patients without preoperative urinalysis with the patients included in data analysis. Similar results were seen in age (P = 0.910), gender (P = 0.999), CKD stages (P = 0.886), DM (P = 0.235), AKI (P = 0.181), need for RRT (P = 0.410), and 30-day mortality (P = 0.634). Because initiation of RRT is relatively a subjective decision, we also did sensitivity analysis for severe CSA-AKI defined as more than two stages with the AKIN criteria. Heavy proteinuria was also an independent risk factor of severe AKI (OR = 3.24, 95% CI 1.42 to 7.38, P = 0.005).
DISCUSSION
The results clearly demonstrated that preoperative proteinuria is an important, yet neglected, predictor for AKI after cardiac surgery. The risk of AKI was higher in patients with more severe proteinuria. In addition, heavy proteinuria, regardless of baseline eGFR or other comorbidities, was independently associated with severe AKI requiring RRT, the most fatal form of CSA-AKI. This finding has not been reported in the medical literature previously, and existing risk scoring systems have not taken this into consideration. Also, to the best of our knowledge, this is the first report to systemically investigate the relationship between proteinuria and postoperative renal outcomes and demonstrate its strong association with adverse renal outcomes.
Risk Factors of CSA-AKI
In clinical practice, an accurate risk prediction model can help clinicians identify high-risk patients for more favorable treatment options, more meticulous care, and potential preventive interventions. Preventive interventions have been most studied in patients at high risk because high-risk patients benefit more from such interventions than low-risk patients.9 Thus, it is very important to develop an inclusive and accurate staging system, especially for patients who are undergoing a procedure associated with significant risks, such as cardiac surgery. The novelty of our study is the identification of heavy proteinuria as an overlooked important risk factor of CAS-AKI. This has not been considered in past scoring systems for outcome prediction. Documented proteinuria with dipstick results of more than 1+ preadmission have been reported to be associated with the risk of hospital-acquired AKI.10 In our logistic regression model, this risk was found to be greater in patients with DM. Although DM has been identified as an independent risk factor for postoperative RRT, heavy proteinuria was actually a more significant factor in our study. In previous risk scoring systems, such as Mehta's bedside tools and the Cleveland Clinic Foundation Acute Renal Failure Scoring system, patients with diabetes are classified into two groups: those receiving oral hypoglycemic agents and those receiving insulin.11,12 Of these two groups, the risk of AKI is higher in the latter. Patients with long-standing DM usually have greater end-organ damage. Proteinuria has been identified as a marker of renal damage, regardless of whether the etiology of the primary disease is DM, hypertension, or another form of glomerulopathy. In our analysis, there was also a substantial proportion of patients with proteinuria who did not have DM (Table 1), so the effect of overt proteinuria on CSA-AKI was beyond that associated with DM. It is therefore reasonable to use proteinuria as an independent factor to better detect patients at risk of CSA-AKI.
Impaired preoperative renal function with low eGFR (<60 ml/min per 1.73 m2) and preoperative proteinuria were significantly associated with dialysis requiring AKI.10 In our analyses, when we focused on postoperative AKI, patients with impaired eGFR and proteinuria were found to have a greater risk than those without proteinuria. Even mild proteinuria (trace to 1+) increased the risk of a patient with stage 3 CKD to the same risk as stage 4 CKD (Figure 2). Most strikingly, a patient with preserved GFR (≥60 ml/min per 1.73 m2) had a risk comparable to a patient with stage 3 CKD, if even mild proteinuria (trace to 1+) was present (Figure 2). These types of patients have previously been neglected, although they made up 33.0% (208 in 631 patients) of our cohort. This means that one third of patients undergoing surgery who are at an increased risk are not identified by the current risk scoring systems only based on serum creatinine or GFR measurements. However, the absence of an interaction effect of CKD and proteinuria in the prediction of mortality was notable because a very small amount of protein in urine was associated with a significant mortality risk in the patients with CKD.13 These findings should motivate clinicians to become more concerned about the presence of low quantities of protein in urine.
Proteinuria and CSA-AKI
There is some evidence in the medical literature that overt albuminuria might be associated with tubulointerstitial damage. Normally, only a small amount of albumin is filtered across the glomeruli, and nearly all filtered albumin is reabsorbed by means of apical receptors in proximal tubules. Resorption of albumin may upregulate some mediators such as enothelin-1,14 monocyte chemoattractant protein-1 (MCP-1),15 IL-8,16 and RANTES.17 These factors may result in renal cell proliferation, activation of macrophages and monocytes, deposition of matrixes, and finally tubulointerstitial damage.14–17 Studies in vivo have also demonstrated that chronic proteinuric nephropathy leads to interstitial inflammation primarily via NF-κB or MCP-1 upregulation.18 In addition, proteinuria also activates the complement cascade in the proximal tubules, and membrane attack complex (C5b-9) leads to further extracellular matrix deposition.19 These events ultimately lead to tubulointerstitial inflammation and fibrosis in long-standing proteinuric nephropathy. Patients with documented proteinuria have less physiologic adaptability and are less able to tolerate kidney hemodynamic changes and other nephrotoxic insults.10
The pathogenesis of CSA-AKI is complex. Toxins, metabolic factors, ischemia-reperfusion injury, neurohormonal activation, inflammation, and oxidative stress may all contribute to CSA-AKI.20 The final events of insults caused by these factors are tubular damage and loss of GFR.1,20 A proinflammatory status results from CPB, ischemic-reperfusion injury, endotoxemia, and operative trauma,1,21 and it has been proposed that inflammation plays a central role in CSA-AKI.21–23 Tubulointerstitial damage and fibrosis induced by proteinuria may predispose to CSA-AKI because of pre-existing tubulointerstitial inflammation.
Preoperative proteinuria not only is a marker of chronic renal insults but also may serve as a surrogate of acute damage. In our analysis, there were more patients with proteinuria in the IABP or ECMO group, which implies that these patients actually have acute proteinuria secondary to renal insults. We propose that preoperative proteinuria within 2 days before surgery is highly predictive of postoperative AKI, irrespective of acute or chronic insults.
Study Limitations
There are some limitations to this study that should be considered. First, proteinuria detection was performed with dipsticks. Although ACR is preferred for the detection of CKD and more accurate quantification of albuminuria,24,25 the urine dipstick examination is inexpensive and readily performed and interpreted. In addition, the differences between the dipstick test and ACR in risk assessment of CSA-AKI were not examined in this study. Second, because of the noninterventional nature of the study, the decision to initiate RRT depended on an individual physician; thus, bias in risk factor analysis may have been introduced. However, the identified risk factors were comparable to previous studies, and the logistic models had both good discrimination and calibration. Third, we used a creatinine and urine output–based criteria (the AKIN criteria) for the diagnosis of AKI. Blood loss, hemodilution, and premorbid conditions may affect the diagnosis of AKI. However, a previous study showed the AKIN criteria is predictive in this cohort.26
In conclusion, this study showed that proteinuria, detected by urine dipstick, is also an important risk factor of CSA-AKI in patients undergoing cardiac surgery. A substantial proportion of patients undergoing cardiac surgery have an elevated risk of adverse outcome that is not apparent from the current risk scoring systems. Thus, the study highlights the flaws of current risk predicting systems and it may contribute to the future development of risk stratification systems. The inclusion of proteinuria in risk scoring systems may lead to improved patient outcomes.
CONCISE METHODS
Study Population
This is a secondary analysis of a prospectively collected database. Patients undergoing CABG surgery at the National Taiwan University Hospital (NTUH) and its two branches from January 2003 to December 2007 were enrolled. Inclusion criteria were age ≥18 years and first-time cardiac surgery, whereas the exclusion criteria were history of preoperative RRT with any modality and estimated GFR <15 ml/min as calculated with the four-variable Modification of Diet in Renal Disease (MDRD) equation.27 Patients having no urinalysis reports within 48 hours before surgery were also excluded. Patient data collected from the NSARF database included basic demographic characteristics, perioperative laboratory investigations, type and timing of surgery, and postoperative renal outcome.28,29 This study was approved by the Institutional Review Board of National Taiwan University Hospital (NTUH). Because it was a nonconcurrently prospective study, informed consent was not required.
Risk Factors
Preoperative variables such as age, gender, BMI, LVEF measured by echocardiography or angiography, hypertension (BP ≥140/90 mmHg or using antihypertensive medications), DM (using oral hypoglycemic agents or insulin), PAD determined by clinical diagnosis or imaging results, previous cerebral vascular accident (CVA) (ischemic or hemorrhagic), NY Heart Association (NYHA) functional class III or IV CHF, chronic obstructive pulmonary disease requiring long-term bronchodilators or steroids, recent MI (i.e., <30 days before surgery), and preoperative laboratory data (hemoglobin [Hb] concentration and serum creatinine concentration) were all collected. Perioperative vasopressor (adrenaline, dopamine, dobutamine, norepinephrine, or isoproterenol) dependence, use of ECMO, or IABP before surgery were noted. Patients who underwent emergent or urgent operations were considered as nonelective surgery. Utilization of CPB during surgery was also recorded.
Preoperative GFR and Proteinuria
Three parameters were used to be representative of preoperative GFR: serum creatinine, eGFR, and CKD stage (preserved eGFR, stage 3 or stage 4, according to eGFR). The baseline creatinine of each patient was determined according to the following criteria: (1) data obtained at hospital discharge from the previous admission in those who had more than one admission within a year before the index admission;30 (2) the lowest creatinine value during the index admission (after excluding data during emergency room stay).31,32 The eGFR in each patient was calculated using the four-variable MDRD equation.27 CKD stages were determined using the NKF definition: Patients with 15 ml/min per 1.72 m2 ≤ eGFR < 30 ml/min per 1.72 m2 were classified as stage 4 and eGFR 30 ml/min per 1.72 m2 ≤ eGFR <60 ml/min per 1.72 m2 were stage 3.24 Patients with eGFR ≥60 ml/min per 1.72 m2 had preserved GFR. High correlation among CKD stages, eGFRs, and serum creatinine levels were identified. Therefore, we used CKD stages to be representative of preoperative renal function.
Proteinuria was measured using a dipstick within 2 days before surgery. To classify the severity of proteinuria, we defined negative as “no proteinuria,” trace to 1+ as “mild proteinuria,” and 2+ to 4+ as “heavy proteinuria.” The test strips were measured by an automatic dipstick autoanalyzer (AUTION MAX, AX-4030; ARKRAY Inc., Kyoto, Japan) with automatic correction of the specific gravity using the pH test pad in a routine laboratory environment. This classification was adopted in a large epidemiologic study in Alberta, Canada.8 Although ACR is favored for proteinuria detection, dipstick examinations remain the most convenient and inexpensive choice for screening.8 If there was more than one measurement in 2 days before surgery, we chose the most severe for analysis.
Outcomes
The primary outcome was AKI occurring within 48 hours after surgery. The definition of AKI was based on the Acute Kidney Injury Network (AKIN) criteria and has been well validated in cardiac surgery patients for in-hospital mortality prediction.26 AKI was defined as serum creatinine elevated ≥1.5 times baseline value, absolute elevation ≥0.3 mg/dl, or urine output <0.5 ml/kg per hour for ≥6 hours in the first 48 hours postoperatively. In the NSARF database, serum creatinine values were recorded daily after surgery. Urine output was recorded every hour in the critical care setting.
The secondary outcome was requirement of RRT during the ICU stay. The indications for RRT initiation in the NSARF database were as follows:33 (1) azotemia (blood urea nitrogen >80 mg/dl and creatinine >2 mg/dl) with uremic symptoms (encephalopathy, nausea, vomiting, etc.); (2) oliguria (urine output <200 ml per 8 hours) or anuria refractory to diuretics; (3) fluid overload refractory to diuretics use with a central venous pressure (CVP) > 12 mmHg or pulmonary edema with a partial pressure of arterial oxygen/fraction of inspired oxygen ratio (Pao2/Fio2) <300 mmHg; (4) hyperkalemia (K+ >5.5 mmol/L) refractory to medical treatment; and (5) metabolic acidosis (pH <7.2 in arterial blood gas). The decision to initiate RRT depended on the individual nephrologist, intensivist, or surgeon. All-cause 30-day mortality was also documented by matching unique identity numbers with the National Mortality Registry (Department of Health, Taiwan).
Statistical Analysis
Statistical analyses were performed using the SAS software, version 9.1.3 (SAS Institute Inc., Cary, NC), and the R software, version 2.10.0 (Free Software Foundation, Inc., Boston, MA). Two-sided P ≤ 0.05 was considered statistically significant. Continuous variables were presented as mean and SD (mean ± SD) or median and interquartile range (IQR) as appropriate. Categorical variables were summarized as frequency and percentage. Group difference in demographic characteristics was examined between each renal dysfunction group (impaired eGFR or proteinuria) and the preserved renal function group by two-sample t test or χ2 test as appropriate.
Logistic regression analysis with stepwise variable selection procedure were applied, using all available variables (CKD stages were used to be representative of preoperative renal function), to identify important factors associated with postoperative AKI or RRT. Yet there is a significant positive relationship between proteinuria level and CKD stage (P < 0.001) and the risk of AKI might be different in patients with and without DM.34 Thus, the interaction effects between proteinuria, CKD stage, and diabetes on adverse outcomes were also considered. The GOF of fitted multiple logistic regression model was assessed by the estimated area under the ROC curve, the adjusted generalized R2, and the Hosmer-Lemeshow GOF test. Yet the value of the adjusted generalized R2 for logistic regression model is usually low. Larger P values of the Hosmer-Lemeshow GOF test indicate better fits. To help visualize analysis results, conditional effect plots for outcome prediction were drawn on the basis of the fitted final logistic regression model. It plots the estimated probability of having an adverse outcome against a chosen continuous covariate, with the values of the other discrete and continuous covariates held in constant.
Finally, sensitivity analyses were conducted. We compared the basic demography and outcomes of the 97 patients without preoperative urinalysis with the study patients. And we performed the same logistic regression analysis on the patients with severe CSA-AKI defined by the AKIN criteria more than two stages.
DISCLOSURES
None.
Acknowledgments
This study was supported by The Ta-Tung Kidney Foundation and Taiwan National Science Council (Grant NSC 96-2314-B-002-164, NSC 96-2314-B-002-033-MY3, NSC 97-2314-B-002-155-MY2, NSC 98-2314-B-002-155-MY4) and NTUH 098-001177 and 100-001667. The authors thank the staff of the Second and Eighth Core Lab of the Department of Medical Research in National Taiwan University Hospital for technical assistance. We express our sincere gratitude to all participants of the NSARF.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
REFERENCES
- 1. Rosner MH, Okusa MD: Acute kidney injury associated with cardiac surgery. Clin J Am Soc Nephrol 1: 19–32, 2006 [DOI] [PubMed] [Google Scholar]
- 2. Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M: Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: A prospective cohort study. J Am Soc Nephrol 15: 1597–1605, 2004 [DOI] [PubMed] [Google Scholar]
- 3. Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, Appleyard M, Jensen JS: Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension, and diabetes. Circulation 110: 32–35, 2004 [DOI] [PubMed] [Google Scholar]
- 4. Mann JF, Gerstein HC, Pogue J, Bosch J, Yusuf S: Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: The HOPE randomized trial. Ann Intern Med 134: 629–636, 2001 [DOI] [PubMed] [Google Scholar]
- 5. Hillege HL, Fidler V, Diercks GF, van Gilst WH, de Zeeuw D, van Veldhuisen DJ, Gans RO, Janssen WM, Grobbee DE, de Jong PE: Urinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general population. Circulation 106: 1777–1782, 2002 [DOI] [PubMed] [Google Scholar]
- 6. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis 39: S1–S266, 2002 [PubMed] [Google Scholar]
- 7. Hallan SI, Ritz E, Lydersen S, Romundstad S, Kvenild K, Orth SR: Combining GFR and albuminuria to classify CKD improves prediction of ESRD. J Am Soc Nephrol 20: 1069–1077, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hemmelgarn BR, Manns BJ, Lloyd A, James MT, Klarenbach S, Quinn RR, Wiebe N, Tonelli M: Relation between kidney function, proteinuria, and adverse outcomes. JAMA 303: 423–429, 2010 [DOI] [PubMed] [Google Scholar]
- 9. Bove T, Landoni G, Calabro MG, Aletti G, Marino G, Cerchierini E, Crescenzi G, Zangrillo A: Renoprotective action of fenoldopam in high-risk patients undergoing cardiac surgery: A prospective, double-blind, randomized clinical trial. Circulation 111: 3230–3235, 2005 [DOI] [PubMed] [Google Scholar]
- 10. Hsu CY, Ordonez JD, Chertow GM, Fan D, McCulloch CE, Go AS: The risk of acute renal failure in patients with chronic kidney disease. Kidney Int 74: 101–107, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mehta RH, Grab JD, O'Brien SM, Bridges CR, Gammie JS, Haan CK, Ferguson TB, Peterson ED: Bedside tool for predicting the risk of postoperative dialysis in patients undergoing cardiac surgery. Circulation 114: 2208–2216;quiz 2208, 2006 [DOI] [PubMed] [Google Scholar]
- 12. Thakar CV, Arrigain S, Worley S, Yared JP, Paganini EP: A clinical score to predict acute renal failure after cardiac surgery. J Am Soc Nephrol 16: 162–168, 2005 [DOI] [PubMed] [Google Scholar]
- 13. Wen CP, Cheng TY, Tsai MK, Chang YC, Chan HT, Tsai SP, Chiang PH, Hsu CC, Sung PK, Hsu YH, Wen SF: All-cause mortality attributable to chronic kidney disease: A prospective cohort study based on 462 293 adults in Taiwan. Lancet 371: 2173–2182, 2008 [DOI] [PubMed] [Google Scholar]
- 14. Zoja C, Morigi M, Figliuzzi M, Bruzzi I, Oldroyd S, Benigni A, Ronco P, Remuzzi G: Proximal tubular cell synthesis and secretion of endothelin-1 on challenge with albumin and other proteins. Am J Kidney Dis 26: 934–941, 1995 [DOI] [PubMed] [Google Scholar]
- 15. Wang Y, Chen J, Chen L, Tay YC, Rangan GK, Harris DC: Induction of monocyte chemoattractant protein-1 in proximal tubule cells by urinary protein. J Am Soc Nephrol 8: 1537–1545, 1997 [DOI] [PubMed] [Google Scholar]
- 16. Tang S, Leung JC, Abe K, Chan KW, Chan LY, Chan TM, Lai KN: Albumin stimulates interleukin-8 expression in proximal tubular epithelial cells in vitro and in vivo. J Clin Invest 111: 515–527, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Zoja C, Donadelli R, Colleoni S, Figliuzzi M, Bonazzola S, Morigi M, Remuzzi G: Protein overload stimulates RANTES production by proximal tubular cells depending on NF-kappa B activation. Kidney Int 53: 1608–1615, 1998 [DOI] [PubMed] [Google Scholar]
- 18. Donadelli R, Abbate M, Zanchi C, Corna D, Tomasoni S, Benigni A, Remuzzi G, Zoja C: Protein traffic activates NF-kB gene signaling and promotes MCP-1-dependent interstitial inflammation. Am J Kidney Dis 36: 1226–1241, 2000 [DOI] [PubMed] [Google Scholar]
- 19. Abbate M, Zoja C, Remuzzi G: How does proteinuria cause progressive renal damage? J Am Soc Nephrol 17: 2974–2984, 2006 [DOI] [PubMed] [Google Scholar]
- 20. Bellomo R, Auriemma S, Fabbri A, D'Onofrio A, Katz N, McCullough PA, Ricci Z, Shaw A, Ronco C: The pathophysiology of cardiac surgery-associated acute kidney injury (CSA-AKI). Int J Artif Organs 31: 166–178, 2008 [DOI] [PubMed] [Google Scholar]
- 21. Paparella D, Yau TM, Young E: Cardiopulmonary bypass induced inflammation: Pathophysiology and treatment. An update. Eur J Cardiothorac Surg 21: 232–244, 2002 [DOI] [PubMed] [Google Scholar]
- 22. Karkouti K, Wijeysundera DN, Yau TM, Callum JL, Cheng DC, Crowther M, Dupuis JY, Fremes SE, Kent B, Laflamme C, Lamy A, Legare JF, Mazer CD, McCluskey SA, Rubens FD, Sawchuk C, Beattie WS: Acute kidney injury after cardiac surgery: Focus on modifiable risk factors. Circulation 119: 495–502, 2009 [DOI] [PubMed] [Google Scholar]
- 23. Laffey JG, Boylan JF, Cheng DC: The systemic inflammatory response to cardiac surgery: Implications for the anesthesiologist. Anesthesiology 97: 215–252, 2002 [DOI] [PubMed] [Google Scholar]
- 24. K/DOQI clinical practice guidelines for chronic kidney disease. Am J Kidney Dis 39: S1–S266, 2002 [PubMed] [Google Scholar]
- 25. Ciavarella A, Silletti A, Forlani G, Morotti L, Borgnino LC, D'Apote M, Vannini P: A screening test for microalbuminuria in type 1 (insulin-dependent) diabetes. Diabetes Res Clin Pract 7: 307–312, 1989 [DOI] [PubMed] [Google Scholar]
- 26. Haase M, Bellomo R, Matalanis G, Calzavacca P, Dragun D, Haase-Fielitz A: A comparison of the RIFLE and Acute Kidney Injury Network classifications for cardiac surgery-associated acute kidney injury: A prospective cohort study. J Thorac Cardiovasc Surg 138: 1370–1376, 2009 [DOI] [PubMed] [Google Scholar]
- 27. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D: A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med 130: 461–470, 1999 [DOI] [PubMed] [Google Scholar]
- 28. Wu VC, Ko WJ, Chang HW, Chen YS, Chen YW, Chen YM, Hu FC, Lin YH, Tsai PR, Wu KD: Early renal replacement therapy in patients with postoperative acute liver failure associated with acute renal failure: Effect on postoperative outcomes. J Am Coll Surg 205: 266–276, 2007 [DOI] [PubMed] [Google Scholar]
- 29. Wu VC, Ko WJ, Chang HW, Chen YW, Lin YF, Shiao CC, Chen YM, Chen YS, Tsai PR, Hu FC, Wang JY, Lin YH, Wu KD: Risk factors of early redialysis after weaning from postoperative acute renal replacement therapy. Intensive Care Med 34: 101–108, 2008 [DOI] [PubMed] [Google Scholar]
- 30. Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C: An assessment of the RIFLE criteria for acute renal failure in hospitalized patients. Crit Care Med 34: 1913–1917, 2006 [DOI] [PubMed] [Google Scholar]
- 31. Hobson CE, Yavas S, Segal MS, Schold JD, Tribble CG, Layon AJ, Bihorac A: Acute kidney injury is associated with increased long-term mortality after cardiothoracic surgery. Circulation 119: 2444–2453, 2009 [DOI] [PubMed] [Google Scholar]
- 32. Palevsky PM, Zhang JH, O'Connor TZ, Chertow GM, Crowley ST, Choudhury D, Finkel K, Kellum JA, Paganini E, Schein RM, Smith MW, Swanson KM, Thompson BT, Vijayan A, Watnick S, Star RA, Peduzzi P: Intensity of renal support in critically ill patients with acute kidney injury. N Engl J Med 359: 7–20, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Wu VC, Wang CH, Wang WJ, Lin YF, Hu FC, Chen YW, Chen YS, Wu MS, Lin YH, Kuo CC, Huang TM, Chen YM, Tsai PR, Ko WJ, Wu KD: Sustained low-efficiency dialysis versus continuous veno-venous hemofiltration for postsurgical acute renal failure. Am J Surg 199: 466–476, 2010 [DOI] [PubMed] [Google Scholar]
- 34. Parfrey PS, Griffiths SM, Barrett BJ, Paul MD, Genge M, Withers J, Farid N, McManamon PJ: Contrast material-induced renal failure in patients with diabetes mellitus, renal insufficiency, or both. A prospective controlled study. N Engl J Med 320: 143–149, 1989 [DOI] [PubMed] [Google Scholar]