A 69-year-old man was admitted for acute hemoptysis secondary to an aortobronchial fistula that was associated with a descending thoracic aortic aneurysm. He underwent the urgent deployment of a thoracic aortic stent-graft (GORE® TAG® Thoracic Endoprosthesis, W.L. Gore & Associates, Inc.; Flagstaff, Ariz). At the end of the procedure, placement of a chest tube was necessary to drain a left pleural effusion that had been seen on intraoperative chest radiography (Fig. 1). Immediately after the drain insertion, the patient developed severe oxygen desaturation and became hypotensive. More than 1,000 mL of blood drained in a few seconds. Injection of contrast medium through the drainage unit revealed a perforation of the left pulmonary artery (Fig. 2). An emergent left thoracotomy was performed, followed by left pneumonectomy. The patient died of multiorgan failure on the 1st postoperative day.
Fig. 1 Intraoperative chest radiograph shows a massive left pleural effusion.
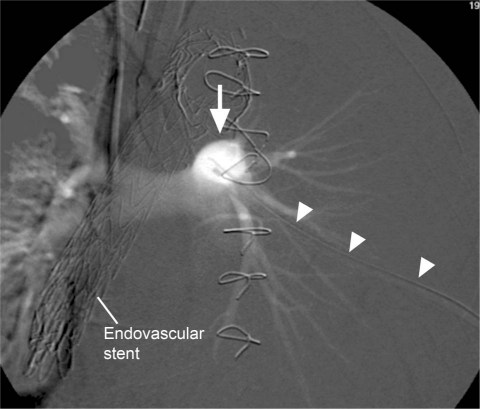
Fig. 2 Injection of contrast medium through the chest-drainage unit reveals a left pulmonary artery perforation (arrow) that was caused by insertion of the tube (arrowheads).
Comment
Chest tubes and their accompanying drainage units present challenges in regard to their optimal use. Large-bore chest tubes are typically required for patients with pneumothoraces regardless of cause, for patients who are supported by mechanical ventilation, and for those who require drainage of viscous pleural liquids, such as blood. The most important complications associated with chest-tube insertion include bleeding and hemothorax due to intercostal artery perforation, perforation of the visceral organs (a lung, the heart, the diaphragm, or an intra-abdominal organ), perforation of major vascular structures such as the aorta or the subclavian vessels, intercostal neuralgia because of trauma to neurovascular bundles, subcutaneous emphysema, re-expansion pulmonary edema, infection of the drainage site, pneumonia, and empyema.1-3 Technical problems, such as incorrect positioning of the tube or intermittent tube blockage by clotted blood, pus, or debris, can cause ineffective drainage.
Pulmonary artery rupture is probably the most devastating complication that is associated with use of the pulmonary artery catheter.4 However, pulmonary artery damage is extremely rare during the insertion of thoracic percutaneous drainage tubes. The image presented here is an excellent illustration of such an occurrence.
Footnotes
Address for reprints: Antonio Bozzani, MD, Division of Vascular Surgery, Foundation I.R.C.C.S. Policlinico San Matteo, P. le Golgi 19, 27100 Pavia, Italy
E-mail: a.bozzani@smatteo.pv.it
References
- 1.Miller KS, Sahn SA. Chest tubes. Indications, technique, management and complications. Chest 1987;91(2):258–64. [DOI] [PubMed]
- 2.Laws D, Neville E, Duffy J; Pleural Diseases Group, Standards of Care Committee, British Thoracic Society. BTS guidelines for the insertion of a chest drain. Thorax 2003;58 Suppl 2:ii53–9. [DOI] [PMC free article] [PubMed]
- 3.Tang AT, Velissaris TJ, Weeden DF. An evidence-based approach to drainage of the pleural cavity: evaluation of best practice. J Eval Clin Pract 2002;8(3):333–40. [DOI] [PubMed]
- 4.Bussieres JS. Iatrogenic pulmonary artery rupture. Curr Opin Anaesthesiol 2007;20(1):48–52. [DOI] [PubMed]