Abstract
Measles remains a leading cause of death worldwide among children because it suppresses immune function. The measles virus (MV) P gene encodes three proteins (P, V, and C) that interfere with innate immunity, controlling STAT1, STAT2, mda5, and perhaps other key regulators of immune function. We identified here three residues in the shared domain of the P and V proteins—tyrosine 110, valine 112, and histidine 115—that function to retain STAT1 in the cytoplasm and inhibit interferon transcription. This information was used to generate a recombinant measles virus unable to antagonize STAT1 function (STAT1-blind MV) differing only in these three residues from a wild-type strain of well-defined virulence. This virus was used to assess the relevance of P and V interactions with STAT1 for virulence in primates. When a group of six rhesus monkeys (Macaca mulatta) was inoculated intranasally with STAT1-blind MV, viremia was short-lived, and the skin rash and other clinical signs observed with wild-type MV were absent. The STAT1-blind virus less efficiently controlled the inflammatory response, as measured by enhanced transcription of interleukin-6 and tumor necrosis factor alpha in peripheral blood mononuclear cells from infected hosts. Importantly, neutralizing antibody titers and MV-specific T-cell responses were equivalent in hosts infected with either virus. These findings indicate that efficient MV interactions with STAT1 are required to sustain virulence in a natural host by controlling the inflammatory response against the virus. They also suggest that selectively STAT1-blind MV may have utility as vectors for targeted oncolysis and vaccination.
Innate immunity, and in particular the interferon (IFN) system, protects the host from viral infections. However, viruses have evolved multiple complementary strategies to evade or control the type I (α/β) IFN responses. They can interfere with gene expression and/or protein synthesis, minimize IFN induction by specifically blocking IFN induction cascades, inhibit IFN signaling, block the action of IFN-induced antiviral proteins, or have a replication strategy not sensitive to IFN action (19, 21, 24).
The IFN-α/β signaling pathway is well characterized: secreted IFN binds to its receptor, activating the tyrosine kinases JAK1 and Tyk2, which in turn phosphorylate the signal transducers and activators of transcription STAT1 and STAT2. Phosphorylated STAT1 and STAT2 form a stable heterodimer that interacts with the DNA-binding protein IRF-9. The IRF-9/STAT1/STAT2 heterotrimer, named IFN-stimulated gene factor 3 (ISGF3), translocates to the nucleus, and binds the IFN-stimulated response element (ISRE) in target promoters, resulting in transcriptional activation of multiple genes that establishes an antiviral state in infected and surrounding noninfected cells (11, 12).
Innate immunity control strategies can be remarkably sophisticated even for RNA viruses that have small genomes and a limited coding capacity. For example, the P gene of measles virus (MV), the enveloped nonsegmented negative strand RNA virus that causes measles, codes for three proteins, the phosphoprotein (P) and proteins V and C. These proteins have roles regulating viral replication and transcription and are necessary for controlling IFN responses (see references 20 and 25) for reviews). For example, P is a polymerase cofactor that also controls IFN signaling (15). V shares the first 231 amino acids with P but has a unique 68-residue cysteine-rich carboxyl-terminal zinc-binding domain (8, 36). The V protein inhibits the activity of mda5 (52) and blocks IFN signaling (7, 32, 34). Finally, the C protein also interferes with IFN induction (30, 31, 43, 47).
Mapping the domains and individual residues of MV proteins necessary for IFN control is the focus of intense research (6, 7, 32, 34, 46, 51). Characterization of amino acids sustaining specific interactions with the innate immune system would help elucidate the relevance of individual components of the IFN induction cascade in controlling virulence. Toward this goal, we sought here to generate a recombinant measles virus unable to antagonize STAT1 function (STAT1-blind MV) and characterize its virulence in a primate model. Rhesus monkeys (Macaca mulatta) efficiently reproduce the clinical signs of measles with MV infection (28; for a review, see reference 13).
One reason to focus initially on STAT1 is its central relevance in the innate response against viral and bacterial infections, as shown experimentally with STAT1-knockout mice (17, 29). It was also shown that knocking out STAT1 in mice expressing a MV receptor makes them more susceptible to MV infection (49). Conversely, we hypothesize that inactivating the STAT1-antagonistic function of both MV V and P proteins would strongly attenuate this virus. In order to generate a STAT1-blind MV that maintains all other functions of the V and P proteins, we sought to better characterize the interaction between V/P and components of the IFN cascade. In particular, we reasoned that conserved residues located near tyrosine 110 (Y110), which we previously characterized as being involved in blocking STAT1 phosphorylation (15), may also sustain the interaction.
Here we identified two additional amino acids in the P/V shared domain, V112 and H115, contributing to the STAT1 interaction. We then used this information to generate a MV differing from a wild-type strain of well-characterized virulence exclusively at three amino acids in the shared domain of the V and P proteins. STAT1-blind MV could not prevent nuclear translocation of STAT1 in infected cells. We then assessed its virulence in rhesus monkeys. STAT1-blind MV was attenuated and controlled inflammation less efficiently than wild-type MV, while still inducing strong adaptive immune responses.
MATERIALS AND METHODS
Cells and viruses.
Vero.hSLAM cells (33) and the helper 293-3-46 cell line (38) were maintained in Dulbecco modified Eagle medium (DMEM; Mediatech, Inc., Herndon, VA) supplemented with 10% fetal calf serum (FCS), 1% penicillin-streptomycin (Mediatech), and 0.5 and 1.2 mg of G418 (Mediatech)/ml, respectively. HeLa.hSLAM were maintained in DMEM-10% and 0.02 mg of Zeocine (Gibco/Invitrogen Corp., Grand Island, NY)/ml. Raji cells were maintained in RPMI medium containing 10% FCS.
Recombinant MVs were generated as described by Radecke et al. (38). Briefly, the helper cell line 293-3-46 expressing MV-N, MV-P, and T7 polymerase was transfected by calcium phosphate precipitation using a ProFection kit (Promega, Madison, WI) with two plasmids, one coding for the relevant MV genome and the other for the MV polymerase (pEMCLa). Three days after transfection, the helper cells were overlaid on Vero.hSLAM cells, the appearance of infectious centers was monitored, and single syncytia were picked and propagated on Vero.hSLAM cells. To prepare virus stocks, Vero.hSLAM cells were infected at a multiplicity of infection (MOI) of 0.03 and incubated at 32°C for 5 days (vaccine) or 37°C for 2 to 3 days (wild type). The cells were scraped into Opti-MEM (Gibco/Invitrogen Corp.), and particles were released by two freeze-thaw cycles.
Virus stock titers were determined by 50% endpoint dilution (50% tissue culture infectious dose [TCID50]) on Vero.hSLAM cells using the Spearman-Kärber method (23). The peak titers of MVvac2.STAT1blind and MVwt.STAT1blind were about 10 times lower than those of the parental viruses.
Viral growth kinetics were obtained by inoculating Vero.hSLAM or HeLa.hSLAM cells at an MOI of 0.05 TCID50/cell. At the indicated time points, infected cells were scraped and subjected to one freeze-thaw cycle. Virus titers were determined by TCID50 titration.
Expression plasmids and full-length infectious cDNA construction.
An expression plasmid coding for the P protein but not for the C protein, pCG-Pvac (15), was mutagenized by using the QuikChange system (Stratagene, La Jolla, CA). The control plasmid P-inv was produced by cloning the inverted sequence of the P gene into the pCG vector. To produce the STAT1blind full-length cDNA, site-directed mutagenesis was performed on pCGHpaI-MVvac-NheI and pCGPmeI-MVwt-PmeI (14, 15), where the mutations of interest were introduced. Full-length cDNA p(+)MVvac2STAT1blind and p(+)MVwtSTAT1blind were obtained by transferring the mutated BssHII-BstEII fragment into the full-length cDNA of pB(+)MVvac2 or p(+)MVIC323, respectively (15, 42, 45). The integrity of the plasmid and full-length constructs was verified by sequencing.
Luciferase assays.
Cells (293, 4 × 104 per well) were plated in 96-well plates. One day later, each well was transfected with 40 ng of pRL-CMV (Promega) plus 300 ng of pISRE-luc (Stratagene) plus 300 ng of the indicated P- or V-expressing plasmids. Transfection was performed with Lipofectamine 2000 (Invitrogen) according to the manufacturer's protocol. After 24 h, IFN-α was added to the medium at 2,000 U/ml, the cells were incubated for an additional 18 h. The luciferase activity was measured by using a Dual-Glo luciferase assay system (Promega) according to the manufacturer's protocol in a TopCountNXT luminescence counter (Packard Instrument Company, Meriden, CT). Each transfection was carried out in triplicate, and each experiment was performed at least twice. Variations in the transfection efficiency were accounted for by calculating the ratio of firefly luciferase activity to Renilla luciferase activity in each sample.
Immunoblot analysis of cell extracts.
The cells (2 × 105) were transfected with the mutant plasmids using Lipofectamine 2000 (Invitrogen, Carlsbad, CA). After 36 h, the cells were processed as described earlier (15). After fractionation on 4 to 15% sodium dodecyl sulfate-polyacrylamide gels (Bio-Rad, Hercules, CA) and transfer to polyvinylidene difluoride membranes (Immobilon-P [Millipore, Billerica, MA]), the samples were subjected to enhanced chemiluminescence detection using mouse anti-P (kindly provided by D. Gerlier), rabbit anti-V (15), and anti-β-actin (Sigma-Aldrich, St. Louis, MO) as a loading control.
Confocal microscopy.
Cells (3 × 104 cells in chamber slides (Lab Tek II chamber slide system [Nalge Nunc International Corp., Naperville, IL]) were either infected with MV at an MOI of 0.03 or transfected with expression plasmid coding for P protein according to manufacturer's protocol (Lipofectamine 2000; Invitrogen). At 30 h postinfection or transfection, cells were treated with IFN-α (2,000 U/ml) for 30 min at 37°C, washed once with phosphate-buffered saline (PBS), and fixed with PBS-2% paraformaldehyde (PFA). The cells were then permeabilized with PBS-2% PFA-0.1% Triton X-100 for 20 min, washed with PBS, incubated for 1 h in blocking solution (PBS-2% FCS), and immunostained for STAT1 protein and for P or N protein. A mouse monoclonal anti-P antibody (kindly provided by D. Gerlier), the commercially available fluorescein isothiocyanate-labeled mouse monoclonal anti-N antibody (Chemicon, Temecula, CA), and rabbit antibodies directed against STAT1α p91 (C-24; Santa Cruz Biotechnology) were used. Incubations were performed in PBS-2% FCS for 1 h at 37°C, and five washes were performed after incubation with primary and secondary antibodies. After the last washes, cells were mounted with Vectashield (Vector Laboratories, Burlingame, CA) containing DAPI (4′,6′-diamidino-2-phenylindole) and analyzed as a single optical cut with a Zeiss LSM 510 confocal microscope.
Rhesus monkey infections.
MV-seronegative M. mulatta monkeys were housed at the California National Primate Research Center in accordance with the regulations of the Association for the Assessment and Accreditation of Laboratory Animal Care. MV infection was as described previously (28, 53): six monkeys were challenged by conjunctival/intranasal inoculation of 104.5 TCID50 of MV.wtSTAT1blind. The animals were monitored daily for anorexia, depression, coughing, diarrhea, and skin rash. They were bled on days 0, 3, 7, 14, and 28 postchallenge. Viremia was quantified by endpoint dilution coculture with Vero.hSLAM cells. Briefly, serial 10-fold dilutions of peripheral blood mononuclear cells (PBMC) were made in RPMI 1640 medium supplemented with 5% FCS. Four replicates of 101 to 105 PBMC were cocultured with 4 × 104 Vero.hSLAM cells per well in 96-well plates (Fisher Scientific). The cultures were maintained for 14 days, monitored for syncytium formation. The limit of detection was 1 infectious unit in 106 PBMC.
Characterization of the humoral immune response in monkeys.
Neutralizing antibodies to MV were measured as described previously (41). Titers were determined in a plaque reduction assay by incubating serum dilutions with 50 TCID50 of MVvac(GFP)N expressing green fluorescence protein (GFP) and expressed as the reciprocal of 90% plaque reduction fluorescence-forming units. MVvac(GFP)N was generated by transferring an additional transcription unit coding for GFP located upstream of the N gene from p(+)MVeGFP (16) to pB(+)MVvac (15).
Cell-mediated immunity.
MV-specific T cells were counted by using an IFN-γ enzyme-linked immunospot (ELISPOT) assay as described previously (14, 37). Briefly, PBMC were stimulated overnight with live MV Edmonston (American Type Culture Collection). After overnight incubation, the cells were transferred to a 96-well ELISPOT plate coated with antibody to rhesus IFN-γ (U-Cytech BV, Utrecht, Netherlands) and developed according to the manufacturer. Spot-forming cells (SFC) were counted, and the number of spots in duplicate wells was averaged. A positive result was at least 10 spots per well and greater than or equal to the mean plus two standard deviations (SD) of the medium control. The spot number in medium control wells was subtracted from the experimental spot count, and the number of SFC was adjusted to 106 PBMC.
Amplification of cytokine and interferon mRNA by real-time reverse transcription-PCR.
Total RNA was isolated from monkey PBMC cells with TRIzol (Invitrogen) according to the manufacturer's protocol, reverse transcribed, and PCR amplified as previously described (1, 2, 14). Primer-probe sequences for rhesus IFN-α, IFN-β, tumor necrosis factor alpha (TNF-α), interleukin 6 (IL-6), OAS, MxA, IL-2, IL-4, IL-12, and IFN-γ were used (1, 2).
Statistical analysis.
Statistical analyses of the cytokines mRNA data were performed by using the Wilcoxon rank sum test with the software JMP8 (JMP, Cary, NC), and a Student t test was used for the luciferase assay.
RESULTS
Three P protein amino acids, Y110, V112, and H115 are involved in the control of IFN signaling.
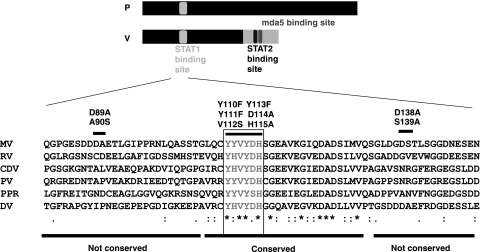
We previously used a luciferase assay based on an IFN-activatable promoter to show that Y110 contributes to the P protein-STAT1 interaction (15). The promoter used in this assay consists of a pentameric ISGF3 binding site controlled by the STAT1 and STAT2 transcription factors. Having noted that a hexapeptide including Y110 is conserved between all morbilliviruses (Fig. 1), we tested whether additional amino acids in this hexapeptide are important for the control of IFN function. We mutated the five conserved residues downstream of Y110 as shown in Fig. 1. As negative controls, we also mutated two charged (D89 and D138) and two noncharged (A90 and S139) residues in the nonconserved upstream or downstream regions (Fig. 1). To limit structural interference, charged and polar residues were substituted by alanine (A), apolar residues by serine (S), and tyrosines by phenylalanine (F). Plasmids expressing the inverted P gene (invP) or the parental P gene were used as negative control and expression standard, respectively, and immunoblots showed similar levels of expression for all mutant proteins (Fig. 2E).
FIG. 1.
P and V mutant proteins. (Top) Schematic drawing illustrating the open reading frames of the P and V proteins (from the top). (Bottom) Sequence alignments of amino acids 81 to 150 in the shared segment of six Morbilliviruses P and V proteins. Gene bank numbers for each sequence are: AAF85668.1 (MV), CAA48389.1 (Rinderpest virus [RV]), AAQ96296.1 (canine distemper virus [CDV]), BAA01203.1 (phocine distemper virus [PV]), CAH61253.1 (Peste des petits ruminants [PPR]), and CAE55654.1 (dolphin morbillivirus [DV]). Sequence alignments were performed at the Swiss Institute of Bioinformatics using the BLAST network service, NCBI BLAST 2 software (3) and the CLUSTAL W program. The Yrich sequence is boxed. *, Residues identical in all sequences; “:” and “.”, conservative and semiconservative substitutions, respectively. Introduced amino acid mutations are indicated above the sequences.
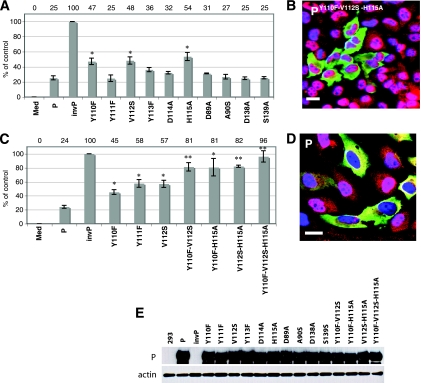
FIG. 2.
Three amino acids Y110, V112, and H115 contribute to the STAT1-inhibiting function of the P protein. (A and C) ISRE promoter activity after transfection with the plasmids indicated below each bar along with pISRE-luc and pCMV-RL. The firefly and Renilla luciferase activities, reflecting ISRE promoter activation and transfection efficiency, were measured. The y axis indicates the percentage of luciferase expression compared to the control plasmids (P and invP). The data represent the mean values ± the SD for triplicate samples. Med, medium; InvP, inverted P. One or two asterisks indicate statistical significance compared to the P control with a P < 0.05 and a P ≤ 0.001, respectively. (B and D) Nuclear translocation of STAT1. HeLa cells were transfected with an expression plasmid encoding the triple mutated P protein (B) or the standard P protein (D). After stimulation with IFN-α, the cells were fixed, permeabilized, and stained with antibody to P protein (green), STAT1 (red), and DAPI (blue). Merged sections of the three stains are shown. The overlap of red and green staining yields yellow, and the overlap of red and blue staining yields pink. Scale bar, 20 μm. (E) Immunoblot analysis of 293 cells transfected with the indicated plasmids. Membranes were blotted with antibodies against the phosphoprotein (P), as indicated on the left. Actin was used as a loading control.
Figure 2A documents the efficacy of different mutants in blocking IFN signaling by quantifying the levels of luciferase expression driven by the activation of the IFN-stimulated response element (ISRE). Expression of standard P protein reduced luciferase expression by 75% compared to the negative control plasmid (Fig. 2A, compare second and third bar). Mutating Y110, V112, and H115 significantly restored luciferase expression from 25% to levels of 47, 48, and 54%, respectively (P < 0.05), whereas mutations of Y111, Y113, and D114 had nonsignificant effects on the control of ISRE promoter function, as did the mutation of residues 89, 90, 138, and 139 in the nonconserved regions. These results suggest that V112 and H115, in addition to Y110, are important for the P protein control of IFN signaling.
Since Y110, V112, and H115 each promoted only partial recovery of luciferase expression, we produced double (Y110/V112, Y110/H115, and V112/H115) and triple (Y110/V112/H115) mutants and tested their ability to block transcription from the ISRE promoter. As shown in Fig. 2C, the double mutants allowed significant luciferase expression up to 81 to 82% of the negative control (P < 0.05 or P < 0.001 as indicated by one or two asterisks, respectively), and the triple mutant allowed 96% ISRE promoter function (P < 0.001). The triple mutant protein was then tested for its ability to block STAT1 nuclear translocation. Indeed, STAT1 translocation was observed after IFN treatment in cells expressing the PY110/V112/H115 protein, as shown by the pink staining in the nucleus (Fig. 2B, pink nuclei of transfected green cells). In contrast, no translocation of STAT1 was observed in cells expressing standard P (Fig. 2D, blue nuclei of transfected green cells).
Y110, V112, and H115 also sustain control of IFN signaling by the V protein.
We have previously shown that both P and V proteins control ISRE-dependent transcription, V more efficiently than P (15). After confirming this effect for a flagged version of V (Fig. 3A, compare the third and fourth bars), we assessed whether the three amino acids identified in P are functionally important in the V protein. We produced single mutants (Y110, V112, and H115), the three double mutants, the triple mutant, and two control mutants (D89 and S139) in a Flag-V protein. Immunoblots documented similar levels of expression for all mutant proteins (Fig. 3C). We observed that the single, double, and triple mutants all allowed 5 to 8 times higher luciferase expression than the standard V-expressing plasmid (Fig. 3B), whereas the mutants in the nonconserved region had no effect on luciferase expression (Fig. 3B).
FIG. 3.
Y110, V112, and H115 contribute to IFN transcription control by the V protein. (A and B) Cells were transfected with the plasmids indicated below the bars, along with pISRE-luc and pCMV-RL. The firefly and Renilla luciferase activities, reflecting ISRE promoter activation and transfection efficiency, were measured. The y axis indicates the percentage of luciferase expression compared to the control plasmid. Note that in panels A and B different scales are used for the vertical axis. One or two asterisks indicate statistical significance compared to the P control with a P < 0.05 and a P ≤ 0.001, respectively. (C) Immunoblot analysis of 293 cells transfected with the indicated plasmids. Membranes were blotted with antibodies against the V protein (V), as indicated on the left. Actin was used as a loading control.
Vaccine and wild-type MV with the Y110, V112, and H115 mutations cannot control STAT1 function.
In order to assess the effects of Y110, V112, and H115 on viral infection and virulence, we generated MV containing the three mutations in the vaccine and wild-type genetic backgrounds. The vaccine strain background was a necessary control because the original mutagenesis was done in a vaccine-lineage P gene. The wild-type background was chosen for testing virulence in monkeys, since the vaccine strain is not virulent in rhesus monkeys (42). Both viruses, MVvac2.STAT1blind and MVwt.STAT1blind, were rescued and tested for their ability to control STAT1 nuclear translocation. We note that it was not possible to mutate the P/V protein without mutating the overlapping C protein and that the mutations I105F, F107L, and T110P were introduced in C. Therefore, we cannot exclude that some of the effects observed with this virus are due at least in part to C protein mutations.
Nuclear translocation was assessed after infection of HeLa.hSLAM cells. As expected, when cells were infected with the control vaccine or wild-type strains (MVvac2 or MVwt, Fig. 4A or C, respectively), STAT1 nuclear translocation was blocked after treatment with IFN-α (red staining in the cytoplasm of the infected green cells). In contrast, when cells were infected with MVvac2.STAT1blind or MVwt.STAT1blind (Fig. 4B or D, respectively) STAT1 accumulated in the nucleus (pink nuclear staining in the green infected cells), indicating that these viruses could not efficiently block STAT1 translocation.
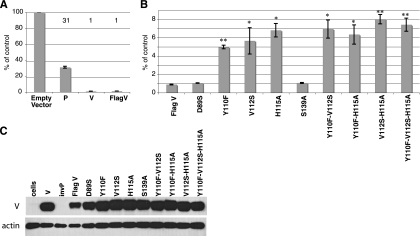
FIG. 4.
Vaccine and wild-type STAT1blind viruses do not block STAT1 nuclear translocation. (A, B, C, and D) Confocal microscopy analysis of STAT1 translocation. HeLa.hSLAM cells were infected with either MVvac2 (A), MVvac2.STAT1blind (B), MVwt (C), or MVwt.STAT1blind (D). After stimulation with IFN-α cells were fixed, permeabilized, and stained with antibody to N protein (green), STAT1 (red) and counterstained with DAPI (blue). A merge of the three staining is shown. The overlaps of red and green staining yield yellow, and the overlaps of red and blue staining yield pink. Scale bars, 20 μm. We note that MVvac2 and derivated strains form only small syncytia. (E and F) Characteristics of the STAT1-blind virus in IFN-producing or deficient cells infected with the vaccine (E) or wild-type (F) viruses. HeLa and Vero cells expressing hSLAM were infected with recombinant viruses MVvac2 (black symbols) or MVvac.STAT1blind (empty symbols). Virus titers in IFN-deficient cells (Vero, squares) or IFN-producing (HeLa, circles) cells were determined at the time indicated by TCID50 titration. The data are averages of three experiments.
To compare the replication of the parental and STAT 1-blind viruses we infected IFN-deficient (Vero) or IFN-producing (HeLa) cells (Fig. 4E and F, squares and circles, respectively). Both parental viruses MVvac2 (Fig. 4E) and MVwt (Fig. 4F) reached higher titers on Vero.hSLAM cells (black squares) than in HeLa.hSLAM cells (black circles). The STAT1-blind viruses (empty symbols) reached 3- to 30-times-lower peak titers than the parental viruses (black symbols), although during the first 24 h the growth kinetics of matched viral pairs were equivalent. Thus, growth of the STAT1-blind viruses is restricted, but restriction becomes apparent only in late infection phases.
Attenuation of STAT1-blind wild-type MV in rhesus monkeys.
To assess whether the STAT1blind virus retains virulence, a group of six rhesus monkeys was inoculated by the conjunctival/intranasal route with 104.5 TCID50 of MVwt.STAT1blind; these inoculation conditions were identical to those previously used to infect another group of monkeys with isogenic MVwt (14). After infection, the monkeys were monitored for multiple parameters of disease such as the measles skin rash, anorexia (weight loss greater than 10%) or diarrhea with bacterial or parasitic dysentery (4, 48, 53). None of the monkeys infected with MVwt.STAT1blind developed any of these signs (data not shown); in contrast rashes were observed in 2 of 6 monkeys and other signs observed in 3 of 6 monkeys inoculated with MVwt (14).
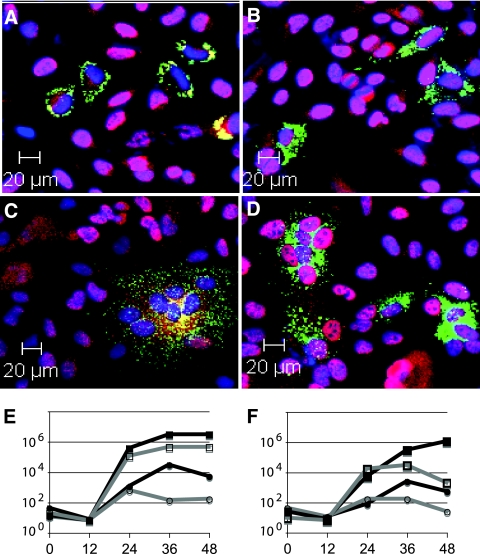
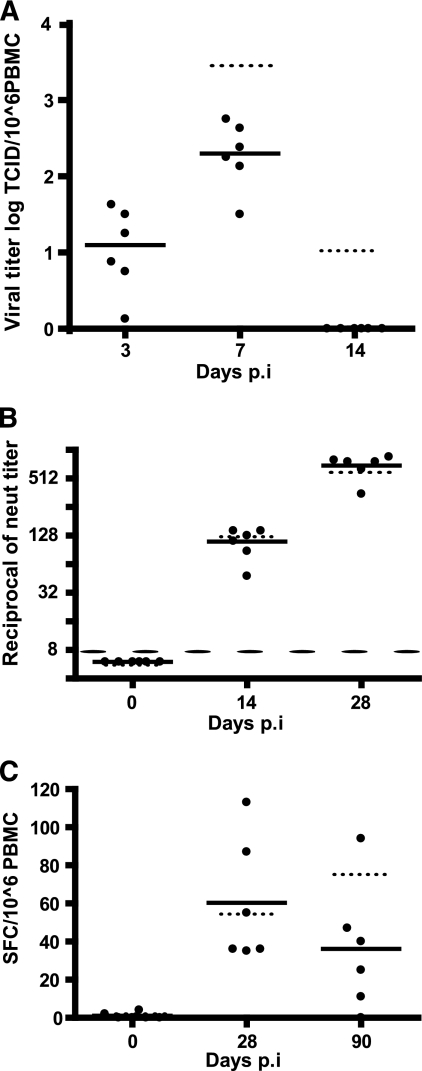
Viremia was assayed in PBMC collected 3, 7, and 14 days postinfection. As shown in Fig. 5A, there were on average 10 infected cells per million PBMC in animals infected with MVwt.STAT1blind 3 days postinfection, 30 to 600 cells 7 days postinfection, and no infected cells 14 days postinfection. Comparative data for MVwt infections are available only for days 7 and 14. At day 7, average MVwt.STAT1blind titers were more than 10-fold lower than those observed in MVwt-infected animals, a significant difference (P = 0.005) (Fig. 5A, day 7, dotted line). By day 14, none of the animals infected with MVwt.STAT1blind had detectable viremia, while five animals infected with the MVwt still had detectable virus titers. Altogether, these results indicate that replication of MVwt.STAT1blind in rhesus monkeys is attenuated.
FIG. 5.
Viremia and adaptive immune responses of monkeys infected with MVwt.STAT1blind. (A) Viremia. Each dot represents an animal, and the horizontal line indicates the mean. Mean value of previously published data from monkeys infected with MVwt (dotted horizontal line) are also shown. MVwt data are not available for day 3. (B) Neutralizing antibody response. Sera obtained at 0, 14, and 28 days postinoculation were assayed for MV neutralization. Symbols are as described above. The results are presented as reciprocals of the neutralizing (neut) titer. Each dot represents an animal. The detection limit is indicated by a thin dashed line. (C) MV-specific IFN-γ-secreting T cells. The symbols are as described above. At 28 and 90 days postinfection, PBMC were stimulated with live MV. The results are presented as SFC per million PBMC.
MVwt.STAT1blind and MVwt elicit similar adaptive immune responses.
To assess the quality of the adaptive immune responses elicited by MVwt.STAT1blind, two parameters were measured: neutralizing anti-MV antibody titers and the number of MV-specific IFN-γ-secreting T cells. Figure 5B documents the MV-neutralization titers 0, 14, and 28 days after inoculation with MVwt.STAT1blind. At day 14, neutralizing antibodies were observed for all animals, with titers ranging from 1:48 to 1:144; these titers increased ∼4-fold by day 28. At both time points, average titers were similar for monkeys infected with MVwt (Fig. 5B, compare continuous and dotted lines).
To assess the strength of the cell-mediated immune (CMI) response, MV-specific IFN-γ-secreting T cells were counted by ELISPOT 1 and 3 months after challenge (Fig. 5C). At 1 month postinfection, all animals infected with MVwt.STAT1blind showed CMI responses equivalent to those observed in animals infected with MVwt (Fig. 5C, group averages of 60 and 57 SFC/106 PBMC for MVwt.STAT1blind and MVwt, continuous and dotted lines, respectively). This response appeared to be slightly reduced 3 months after infection in monkeys infected with the STAT1blind virus compared to MVwt (Fig. 5C, group averages of 44 and 74 SFC/106 PBMC for MVwt.STAT1blind and MVwt, respectively), although the difference was not statistically significant (P = 0.26). Thus, a STAT1-blind MV elicited adaptive immune responses as strong as those elicited by wild-type MV.
MVwt.STAT1-blind elicits stronger inflammatory responses than MVwt.
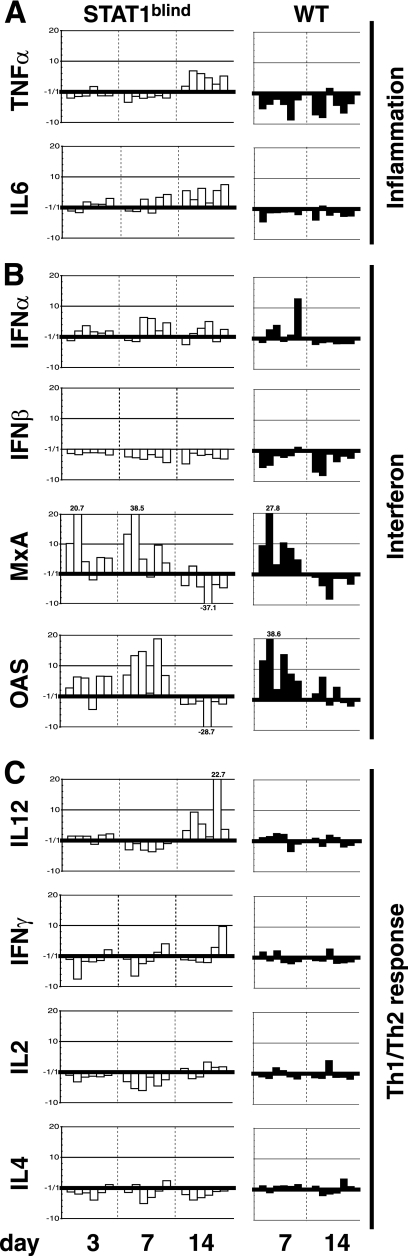
To assess the consequences of uninhibited STAT1 activation for the systemic immune system, we analyzed the transcription of genes controlling the inflammatory response (TNF-α and IL-6), the innate immune response (IFN-α, IFN-β, OAS, and MxA), and the Th1/Th2 balance (IL-12, IFN-γ, IL-2, and IL-4) in PBMC collected from monkeys 3, 7, or 14 days postinfection. Figure 6 shows the mRNA levels of the 10 genes expressed as the fold change compared to levels on the day of inoculation (day 0), normalized to 1 for each host. The data from individual monkeys inoculated with MVwt.STAT1blind are shown on the left, and comparative data previously obtained from MVwt-infected monkeys (14) are shown on the right.
FIG. 6.
Inflammatory, IFN, and Th1/Th2 responses in monkeys infected with MVwt.STAT1blind or MVwt. Changes in mRNA expression levels in PBMC are shown as bar histograms. The results from MVwt. STAT1blind-infected monkeys are shown on the left panels; previously published results for MVwt-infected monkeys are shown on the right panels (14). The level of mRNA for each cytokine was normalized to 1 at day 0 for each monkey. Each histogram shows the fold change in mRNA levels at days 3, 7, and 14 postinfection. The results of individual monkeys are shown in the same order for all cytokines and time points. The data for MVwt-infected monkeys are only available for days 7 and 14. (A) Cytokines relevant for inflammation (TNF-α and IL-6). (B) IFN type I (IFN-α and IFN-β) and IFN-stimulated genes (MxA and OAS). (C) Cytokines involved in the Th1 and Th2 response (IL-12, IFN-γ, IL-2, and IL-4).
Animals infected with MVwt.STAT1blind showed a strong increase in TNF-α transcription at days 7 and 14 compared to the animals infected with MVwt, which showed a strong downregulation at both time points (P = 0.025 and 0.004, respectively). Moreover, IL-6 transcription was elevated in most animals infected with MVwt.STAT1blind, while it was at or below baseline in animals infected with MVwt. This upregulation was observed as early as days 3 and 7 postinfection in 4 of 6 of the MVwt.STAT1blind infected monkeys and was significantly elevated over baseline by day 14 (P = 0.004) postinfection.
To assess the IFN response, we documented the transcription levels of IFNα, IFN-β, and the IFN-stimulated genes OAS and MxA (Fig. 6B) but did not observe significant differences between the experimental groups. On the other hand, analysis of the transcription of cytokines involved in the control of the Th1/Th2 balance revealed upregulated levels of IL-12 mRNA in monkeys infected with MVwt.STAT1blind by day 14 (P = 0.016) (Fig. 6C). IL-12 transcript levels were not significantly different at day 7, however (P = 0.055). The levels of other Th1 or Th2 cytokines tested, including IL-2, IFN-γ, or IL-4, were similar to those observed in PBMC of MVwt-infected monkeys. Taken together, these analyses reveal pronounced and sustained differences in the strength of the inflammatory responses, but not innate immune responses or Th1/Th2 balance, between hosts infected with these viruses.
DISCUSSION
Since STAT1-knockout mice are exquisitely sensitive to viral and bacterial infections, we postulated that recombinant MV unable to antagonize STAT1 function would be attenuated compared to wild-type MV. To test this hypothesis, we generated a selectively STAT1-blind MV in the genetic background of a wild-type MV with well-characterized virulence. Indeed, this virus was attenuated in primate host, the rhesus monkey. STAT1-blind MV was significantly less virulent and controlled inflammation less efficiently than wild-type MV but still induced an equally strong adaptive immune response.
Mechanisms of STAT suppression.
The V protein of MV interacts with different key regulators of innate immunity, including the transcriptional activators STAT1 and STAT2, the RNA helicase mda5, and possibly additional proteins (5-7, 10, 15, 32, 34, 35, 40, 46). The STAT2 and mda5 interactions map to the V-unique zinc-binding domain, while it was previously shown that STAT1 interacts with Y110, a tyrosine located in the domain shared by P and V. We show here that the P/V shared residues V112 and H115 are also involved in the STAT1 interaction.
The V protein of MV downregulates the function of the ISRE promoter used here about 100 times, while P is about 20 times less active, suggesting different mechanisms of action. Moreover, when Y110F, V112S, and H115A mutations are combined in P, the protein completely loses its 4- to 5-fold ISRE promoter inhibition function, while the V protein carrying the three mutations remains capable of partial inhibition of the ISRE function. Thus, another domain of V must contribute to its remarkably efficient ISRE promoter silencing effect. Since the zinc-binding domain interacts with STAT2 (6, 40), simultaneous interactions of V with both STAT1 and STAT2 may explain its remarkable efficiency in interfering with ISRE-dependent transcription, which relies on both STAT1 and STAT2 proteins (22). Expressing V proteins with mutations in both the STAT1 and the STAT2 interaction sites can test this hypothesis formally. Alternatively, the zinc-binding domain of V may contribute to efficient ISRE-promoter silencing through an interaction, direct or indirect, with another mediator of signal transduction.
A STAT1-blind MV cannot control inflammation.
A strong inflammatory response was documented in the PBMC of monkeys infected with MVwt.STAT1blind: transcription of IL-6 was elevated at days 7 and 14 postinfection, and transcription of TNF-α was elevated at day 14 postinfection. In contrast, 7 and 14 days after infection with MVwt, transcription levels were lower than preinfection baseline, an indication that wild-type MV effectively antagonizes inflammation (14). These data imply that more PBMC expressing IL-6 and TNF-α are available in monkeys infected with MVwt.STAT1blind compared to MVwt, even though the infection of PBMC by MVwt.STAT1blind is markedly reduced. The presence of these cells in the blood likely reflects a local immune response to MVwt.STAT1blind replication in the respiratory tract and lymphatic tissue (27). Questions regarding the mechanisms sustaining this strong inflammatory response could not be addressed here due to the limited availability of blood and tissue samples, but future studies ideally would include analyses of cytokine protein quantity and function at early time points and in multiple tissues.
In view of the very small number of infected PBMC, it is not surprising that nonsignificant deviations from normal levels of transcription of the IFN-α gene were detected in PBMC of monkeys infected with MVwt or MVwt.STAT1blind and that in both infections IFN-β transcription was fully controlled. On the other hand, transcription of the IFN-stimulated genes MxA and OAS was elevated 1 week after infection with both viruses but returned to preinoculation levels 1 week later. Thus, transcription of these genes may be a more sensitive reporter of activation of the IFN system. These observations, and the analysis of MxA and OAS transcription at day 3, document that activation of the IFN system can be detected in PBMC only in the early phases of infection.
Finally, the transcription levels of three of the four cytokines controlling the Th1/Th2 balance remained similar to preinfection baseline levels. The exception was IL-12, which was upregulated in the PBMC of monkeys infected with MVwt.STAT1blind 2 weeks after inoculation, but not in monkeys infected with MVwt. The significance of this last observation is unclear, but altogether the cytokine analyses indicate that initiation of inflammatory responses against MV infection depends on STAT1 function, which is efficiently antagonized by MVwt, but not MVwt.STAT1blind, in rhesus monkeys.
A STAT1-blind MV is attenuated: implications for vaccination and oncolysis.
The STAT1-blind MV generated here is attenuated but remains immunogenic in monkeys, as does another MV mutant with a V protein deletion (14). This is remarkable, because whereas the V knockout virus can still interact with STAT1 through the P protein, it cannot interfere with STAT2 or mda5 because it does not express the V-unique zinc-binding domain. Thus, these results underscore the central relevance of the interaction of P and V with STAT1 for promoting virulence. Combinatorial usage of well-defined mutations (14, 26, 27), including those of the STAT1-blind virus, would allow the generation of viruses with graded attenuation capable of extending vaccination opportunities to patient groups currently excluded from measles vaccination. Moreover, a STAT1-blind virus may have utility as oncolytic vector for cancers with documented STAT1 deficiency, such as lymphoma and melanoma (39, 44, 50), thus extending the scope of oncolytic MV-based clinical trials currently limited to ovarian cancer, glioblastoma, and myeloma (9, 18).
Acknowledgments
We thank Denis Gerlier for the anti-P antibody, Ross A. Dierhising for statistical analysis, Tanner Miest and Veronika von Messling for reading the manuscript, and Mary Bennett for excellent secretarial assistance.
The National Institutes of Health (1R21AI076462 to P.D., R01AI63476 to R.C., and RR11069 to the California National Primate Research Center) and the Mayo Clinic CTSA supported this research.
Footnotes
Published ahead of print on 27 October 2010.
REFERENCES
- 1.Abel, K., M. J. Alegria-Hartman, K. Zanotto, M. B. McChesney, M. L. Marthas, and C. J. Miller. 2001. Anatomic site and immune function correlate with relative cytokine mRNA expression levels in lymphoid tissues of normal rhesus macaques. Cytokine 16:191-204. [DOI] [PubMed] [Google Scholar]
- 2.Abel, K., L. La Franco-Scheuch, T. Rourke, Z.-M. Ma, V. De Silva, B. Fallert, L. Beckett, T. A. Reinhart, and C. J. Miller. 2004. Gamma interferon-mediated inflammation is associated with lack of protection from intravaginal simian immunodeficiency virus SIVmac239 challenge in simian-human immunodeficiency virus 89.6-immunized rhesus macaques. J. Virol. 78:841-854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Altschul, S. F., T. L. Madden, A. A. Schaffer, J. Zhang, Z. Zhang, W. Miller, and D. J. Lipman. 1997. Gapped BLAST and PSI-BLAST: a new generation of protein database search programs. Nucleic Acids Res. 25:3389-3402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Auwaerter, P. G., P. A. Rota, W. R. Elkins, R. J. Adams, T. DeLozier, Y. Shi, W. J. Bellini, B. R. Murphy, and D. E. Griffin. 1999. Measles virus infection in rhesus macaques: altered immune responses and comparison of the virulence of six different virus strains. J. Infect. Dis. 180:950-958. [DOI] [PubMed] [Google Scholar]
- 5.Berghall, H., J. Siren, D. Sarkar, I. Julkunen, P. B. Fisher, R. Vainionpaa, and S. Matikainen. 2006. The interferon-inducible RNA helicase, mda-5, is involved in measles virus-induced expression of antiviral cytokines. Microbes Infect. 8:2138-2144. [DOI] [PubMed] [Google Scholar]
- 6.Caignard, G., M. Bourai, Y. Jacob, F. Tangy, P.-O. Vidalain, et al. 2009. Inhibition of IFN-alpha/beta signaling by two discrete peptides within measles virus V protein that specifically bind STAT1 and STAT2. Virology 383:112-120. [DOI] [PubMed] [Google Scholar]
- 7.Caignard, G., M. Guerbois, J.-L. Labernardiere, Y. Jacob, L. M. Jones, F. Wild, F. Tangy, P.-O. Vidalain, et al. 2007. Measles virus V protein blocks Jak1-mediated phosphorylation of STAT1 to escape IFN-alpha/beta signaling. Virology 368:351-362. [DOI] [PubMed] [Google Scholar]
- 8.Cattaneo, R., K. Kaelin, K. Baczko, and M. A. Billeter. 1989. Measles virus editing provides an additional cysteine-rich protein. Cell 56:759-764. [DOI] [PubMed] [Google Scholar]
- 9.Cattaneo, R., T. Miest, E. V. Shashkova, and M. A. Barry. 2008. Reprogrammed viruses as cancer therapeutics: targeted, armed and shielded. Nat. Rev. Microbiol. 6:529-540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Childs, K., N. Stock, C. Ross, J. Andrejeva, L. Hilton, M. Skinner, R. Randall, and S. Goodbourn. 2007. mda-5, but not RIG-I, is a common target for paramyxovirus V proteins. Virology 359:190-200. [DOI] [PubMed] [Google Scholar]
- 11.Darnell, J. E. J. 1997. STATS and gene regulation. Science 277:1630-1635. [DOI] [PubMed] [Google Scholar]
- 12.Der, S. D., A. Zhou, B. R. Williams, and R. H. Silverman. 1998. Identification of genes differentially regulated by interferon alpha, beta, or gamma using oligonucleotide arrays. Proc. Natl. Acad. Sci. U. S. A. 95:15623-15628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeSwart, R. L. 2009. Measles studies in the macaque model. Curr. Top. Microbiol. Immunol. 330:55-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Devaux, P., G. Hodge, M. B. McChesney, and R. Cattaneo. 2008. Attenuation of V- or C-defective measles viruses: infection control by the inflammatory and interferon responses of rhesus monkeys. J. Virol. 82:5359-5367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Devaux, P., V. von Messling, W. Songsungthong, C. Springfeld, and R. Cattaneo. 2007. Tyrosine 110 in the measles virus phosphoprotein is required to block STAT1 phosphorylation. Virology 360:72-83. [DOI] [PubMed] [Google Scholar]
- 16.Duprex, W. P., S. McQuaid, L. Hangartner, M. A. Billeter, and B. K. Rima. 1999. Observation of measles virus cell-to-cell spread in astrocytoma cells by using a green fluorescent protein-expressing recombinant virus. J. Virol. 73:9568-9575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Durbin, J. E., R. Hackenmiller, M. C. Simon, and D. E. Levy. 1996. Targeted disruption of the mouse Stat1 gene results in compromised innate immunity to viral disease. Cell 84:443-450. [DOI] [PubMed] [Google Scholar]
- 18.Galanis, E., L. C. Hartmann, W. A. Cliby, H. J. Long, P. P. Peethambaram, B. A. Barrette, J. S. Kaur, P. J. Haluska, Jr., I. Aderca, P. J. Zollman, J. A. Sloan, G. Keeney, P. J. Atherton, K. C. Podratz, S. C. Dowdy, C. R. Stanhope, T. O. Wilson, M. J. Federspiel, K.-W. Peng, and S. J. Russell. 2010. Phase I trial of intraperitoneal administration of an engineered strain of measles virus modified to express carcinoembryonic antigen for recurrent ovarian cancer. Cancer Res. 70:875-882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Garcia-Sastre, A., and C. A. Biron. 2006. Type 1 interferons and the virus-host relationship: a lesson in detente. Science 312:879-882. [DOI] [PubMed] [Google Scholar]
- 20.Gerlier, D., and H. Valentin. 2009. Measles virus interaction with host cells and impact on innate immunity. Curr. Top. Microbiol. Immunol. 329:163-191. [DOI] [PubMed] [Google Scholar]
- 21.Hengel, H., U. H. Koszinowski, and K.-K. Conzelmann. 2005. Viruses know it all: new insights into IFN networks. Trends Immunol. 26:396-401. [DOI] [PubMed] [Google Scholar]
- 22.Horvath, C. M. 2004. Weapons of STAT destruction. Interferon evasion by paramyxovirus V protein. Eur. J. Biochem. 271:4621-4628. [DOI] [PubMed] [Google Scholar]
- 23.Kärber, G. 1931. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Arch. Exp. Pathol. Pharmakol. 162:480-483. [Google Scholar]
- 24.Katze, M. G., Y. He, and M. Gale, Jr. 2002. Viruses and interferon: a fight for supremacy. Nat. Rev. Immunol. 2:675-687. [DOI] [PubMed] [Google Scholar]
- 25.Lamb, R. A., and G. D. Parks. 2007. Paramyxovirus: the viruses and their replication, p. 1305-1340. In D. M. Knipe, P. M. Howley, D. E. Griffin, R. A. Lamb, M. A. Martin, B. Roizman, and S. E. Straus (ed.), Fields virology, 5th ed. Lippincott-Raven Publishers, Philadelphia, PA.
- 26.Leonard, V. H. J., G. Hodge, J. Reyes del Valle, M. B. McChesney, and R. Cattaneo. 2010. Signaling lymphocytic activation molecular (SLAM, CD150)-blind measles virus is attenuated and induces strong adaptive immune responses in rhesus monkeys. J. Virol. 84:3280-3286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Leonard, V. H. J., P. L. Sinn, G. Hodge, T. Miest, P. Devaux, N. Oezguen, W. Braun, P. B. McCray, M. B. McChesney, and R. Cattaneo. 2008. Measles virus blind to its epithelial cell receptor remains virulent in rhesus monkeys but cannot cross the airway epithelium and is not shed. J. Clin. Invest. 118:2448-2458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McChesney, M. B., C. J. Miller, P. A. Rota, Y. D. Zhu, L. Antipa, N. W. Lerche, R. Ahmed, and W. J. Bellini. 1997. Experimental Measles. I. Pathogenesis in the normal and the immunized host. Virology 233:74-84. [DOI] [PubMed] [Google Scholar]
- 29.Meraz, M. A., J. M. White, K. C. Sheehan, E. A. Bach, S. J. Rodig, A. S. Dighe, D. H. Kaplan, J. K. Riley, A. C. Greenlund, D. Campbell, K. Carver-Moore, R. N. DuBois, R. Clark, M. Aguet, and R. D. Schreiber. 1996. Targeted disruption of the Stat1 gene in mice reveals unexpected physiologic specificity in the JAK-STAT signaling pathway. Cell 84:431-442. [DOI] [PubMed] [Google Scholar]
- 30.Nakatsu, Y., M. Takeda, S. Ohno, R. Koga, and Y. Yanagi. 2006. Translational inhibition and increased interferon induction in cells infected with C protein-deficient measles virus. J. Virol. 80:11861-11867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nakatsu, Y., M. Takeda, S. Ohno, Y. Shirogane, M. Iwasaki, and Y. Yanagi. 2008. Measles virus circumvents the host interferon response by different actions of the C and V proteins. J. Virol. 82:8296-8306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ohno, S., N. Ono, M. Takeda, K. Takeuchi, and Y. Yanagi. 2004. Dissection of measles virus V protein in relation to its ability to block alpha/beta interferon signal transduction. J. Gen. Virol. 85:2991-2999. [DOI] [PubMed] [Google Scholar]
- 33.Ono, N., H. Tatsuo, Y. Hidaka, T. Aoki, H. Minagawa, and Y. Yanagi. 2001. Measles viruses on throat swabs from measles patients use signaling lymphocytic activation molecule (CDw150) but not CD46 as a cellular receptor. J. Virol. 75:4399-4401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palosaari, H., J. P. Parisien, J. J. Rodriguez, C. M. Ulane, and C. M. Horvath. 2003. STAT protein interference and suppression of cytokine signal transduction by measles virus V protein. J. Virol. 77:7635-7644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Parisien, J.-P., D. Bamming, A. Komuro, A. Ramachandran, J. J. Rodriguez, G. Barber, R. D. Wojahn, and C. M. Horvath. 2009. A shared interface mediates paramyxovirus interference with antiviral RNA helicases MDA5 and LGP2. J. Virol. 83:7252-7260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Paterson, R. G., G. P. Leser, M. A. Shaughnessy, and R. A. Lamb. 1995. The paramyxovirus SV5 V protein binds two atoms of zinc and is a structural component of virions. Virology 208:121-131. [DOI] [PubMed] [Google Scholar]
- 37.Premenko-Lanier, M., P. A. Rota, G. H. Rhodes, W. J. Bellini, and M. B. McChesney. 2004. Protection against challenge with measles virus (MV) in infant macaques by an MV DNA vaccine administered in the presence of neutralizing antibody. J. Infect. Dis. 189:2064-2071. [DOI] [PubMed] [Google Scholar]
- 38.Radecke, F., P. Spielhofer, H. Schneider, K. Kaelin, M. Huber, C. Dotsch, G. Christiansen, and M. A. Billeter. 1995. Rescue of measles viruses from cloned DNA. EMBO J. 14:5773-5784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ralph, S. J., B. D. Wines, M. J. Payne, D. Grubb, I. Hatzinisiriou, A. W. Linnane, and R. J. Devenish. 1995. Resistance of melanoma cell lines to interferons correlates with reduction of IFN-induced tyrosine phosphorylation. Induction of the antiviral state by IFN is prevented by tyrosine kinase inhibitors. J. Immunol. 154:2248-2256. [PubMed] [Google Scholar]
- 40.Ramachandran, A., J. P. Parisien, and C. M. Horvath. 2008. STAT2 is a primary target for measles virus V protein-mediated IFNα/β signaling inhibition. J. Virol. 82:8330-8338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reyes-del Valle, J., G. Hodge, M. B. McChesney, and R. Cattaneo. 2009. Protective anti-hepatitis B virus responses in rhesus monkeys primed with a vectored measles virus and boosted with a single dose of hepatitis B surface antigen. J. Virol. 83:9013-9017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Reyes del Valle, J., P. Devaux, G. Hodge, N. J. Wegner, M. B. McChesney, and R. Cattaneo. 2007. A vectored measles virus induces hepatitis B surface antigen antibodies while protecting macaques against measles virus challenge. J. Virol. 81:10597-10605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shaffer, J. A., W. J. Bellini, and P. A. Rota. 2003. The C protein of measles virus inhibits the type I interferon response. Virology 315:389-397. [DOI] [PubMed] [Google Scholar]
- 44.Sun, W. H., C. Pabon, Y. Alsayed, P. P. Huang, S. Jandeska, S. Uddin, L. C. Platanias, and S. T. Rosen. 1998. Interferon-alpha resistance in a cutaneous T-cell lymphoma cell line is associated with lack of STAT1 expression. Blood 91:570-576. [PubMed] [Google Scholar]
- 45.Takeda, M., K. Takeuchi, N. Miyajima, F. Kobune, Y. Ami, N. Nagata, Y. Suzaki, Y. Nagai, and M. Tashiro. 2000. Recovery of pathogenic measles virus from cloned cDNA. J. Virol. 74:6643-6647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Takeuchi, K., S. I. Kadota, M. Takeda, N. Miyajima, and K. Nagata. 2003. Measles virus V protein blocks interferon (IFN)-alpha/beta but not IFN-gamma signaling by inhibiting STAT1 and STAT2 phosphorylation. FEBS Lett. 545:177-182. [DOI] [PubMed] [Google Scholar]
- 47.Toth, A. M., P. Devaux, R. Cattaneo, and C. E. Samuel. 2009. Protein kinase PKR mediates the apoptosis induction and growth restriction phenotypes of C protein-deficient measles virus. J. Virol. 83:961-968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.van Binnendijk, R. S., R. W. van der Heijden, G. van Amerongen, F. G. UytdeHaag, and A. D. Osterhaus. 1994. Viral replication and development of specific immunity in macaques after infection with different measles virus strains. J. Infect. Dis. 170:443-448. [DOI] [PubMed] [Google Scholar]
- 49.Welstead, G. G., C. Iorio, R. Draker, J. Bayani, J. Squire, S. Vongpunsawad, R. Cattaneo, and C. D. Richardson. 2005. Measles virus replication in lymphatic cells and organs of CD150 (SLAM) transgenic mice. Proc. Natl. Acad. Sci. U. S. A. 102:16415-16420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wong, L. H., K. G. Krauer, I. Hatzinisiriou, M. J. Estcourt, P. Hersey, N. D. Tam, S. Edmondson, R. J. Devenish, and S. J. Ralph. 1997. Interferon-resistant human melanoma cells are deficient in ISGF3 components, STAT1, STAT2, and p48-ISGF3γ. J. Biol. Chem. 272:28779-28785. [DOI] [PubMed] [Google Scholar]
- 51.Yokota, S., H. Saito, T. Kubota, N. Yokosawa, K. Amano, and N. Fujii. 2003. Measles virus suppresses interferon-alpha signaling pathway: suppression of Jak1 phosphorylation and association of viral accessory proteins, C and V, with interferon-alpha receptor complex. Virology 306:135-146. [DOI] [PubMed] [Google Scholar]
- 52.Yoneyama, M., M. Kikuchi, K. Matsumoto, T. Imaizumi, M. Miyagishi, K. Taira, E. Foy, Y.-M. Loo, M. Gale, Jr., S. Akira, S. Yonehara, A. Kato, and T. Fujita. 2005. Shared and unique functions of the DExD/H-box helicases RIG-I, MDA5, and LGP2 in antiviral innate immunity. J. Immunol. 175:2851-2858. [DOI] [PubMed] [Google Scholar]
- 53.Zhu, Y. D., J. Heath, J. Collins, T. Greene, L. Antipa, P. Rota, W. Bellini, and M. McChesney. 1997. Experimental measles. II. Infection and immunity in the rhesus macaque. Virology 233:85-92. [DOI] [PubMed] [Google Scholar]