Abstract
On 11 June 2009, the World Health Organization (WHO) declared that the outbreaks caused by novel swine-origin influenza A (H1N1) virus had reached pandemic proportions. The pandemic H1N1 (H1N1pdm) virus is the predominant influenza virus strain in the human population. It has also crossed the species barriers and infected turkeys and swine in several countries. Thus, the development of a vaccine that is effective in multiple animal species is urgently needed. We have previously demonstrated that the introduction of temperature-sensitive mutations into the PB2 and PB1 genes of an avian H9N2 virus, combined with the insertion of a hemagglutinin (HA) tag in PB1, resulted in an attenuated (att) vaccine backbone for both chickens and mice. Because the new pandemic strain is a triple-reassortant (TR) virus, we chose to introduce the double attenuating modifications into a swine-like TR virus isolate, A/turkey/OH/313053/04 (H3N2) (ty/04), with the goal of producing live attenuated influenza vaccines (LAIV). This genetically modified backbone had impaired polymerase activity and restricted virus growth at elevated temperatures. In vivo characterization of two H1N1 vaccine candidates generated using the ty/04 att backbone demonstrated that this vaccine is highly attenuated in mice, as indicated by the absence of signs of disease, limited replication, and minimum histopathological alterations in the respiratory tract. A single immunization with the ty/04 att-based vaccines conferred complete protection against a lethal H1N1pdm virus infection in mice. More importantly, vaccination of pigs with a ty/04 att-H1N1 vaccine candidate resulted in sterilizing immunity upon an aggressive intratracheal challenge with the 2009 H1N1 pandemic virus. Our studies highlight the safety of the ty/04 att vaccine platform and its potential as a master donor strain for the generation of live attenuated vaccines for humans and livestock.
In the spring of 2009, the U.S. Centers for Disease Control and Prevention (CDC) announced the identification of a novel H1N1 strain (H1N1pdm) of influenza A virus causing acute respiratory disease in humans (17). The virus spread easily and sustainably among humans throughout the world, prompting the World Health Organization (WHO) to declare on 11 June 2009 the first influenza pandemic of the 21st century (1, 18). This new isolate was identified as a swine-origin influenza virus (S-OIV), because its RNA segments were most closely related to influenza viruses isolated from pigs in North America and Eurasia (19, 20). Specifically, six of its genomic segments (PB2, PB1, PA, hemagglutinin [HA], NP, and NS) are most similar to those of triple-reassortant (TR) influenza viruses currently circulating in North American pigs, whereas the neuraminidase (NA) and M gene segments are related to prevalent Eurasian H1N1 swine influenza virus (SIV) strains. This particular gene constellation has never been reported among swine or human influenza virus isolates from anywhere in the world, and the precise evolutionary pathway in the genesis of the pandemic H1N1 virus is currently unknown (17, 19, 20, 61).
Since 1998, the emergence of TR influenza viruses, whose genes are derived from human, swine, and avian strains, has caused a dramatic change in the epidemiology of influenza in pigs in North America (35-37, 51, 52, 78). Before 1997 to 1998, swine influenza in North America was caused almost exclusively by infection with classical H1N1 viruses, derivatives of the 1918 Spanish flu virus that were initially isolated from pigs in 1930 (60). Since their introduction in the late 1990s, TR swine influenza viruses have become endemic in North American swine. TR strains of the H3N2, H1N2, and H1N1 subtypes predominate in the U.S. swine population (72). TR swine viruses have demonstrated remarkable reassortment ability with classical swine H1N1 and human H1N1 and H3N2 viruses, generating at least seven different reassortant lineages in the past decade (35-37, 40, 42, 44, 52, 57, 74). A unique feature shared by all of these novel reassortants is the maintenance of the so-called triple-reassortant internal gene (TRIG) cassette, which consists of the avian-like PB2 and PA genes, the human-like PB1 gene, and the classical swine NP, M, and NS genes (43, 72). The TRIG cassette appears to accept multiple HA and NA types, which could provide a selective advantage to swine viruses possessing this internal gene constellation (43, 72). Although there have been sporadic human infections with the H1 TR swine influenza viruses in the United States, none of these events led to sustained human-to-human transmission until the emergence of the H1N1pdm virus (50, 59, 70). Outbreaks of H1N1pdm influenza in pigs in commercial swine operations have been reported in several countries, such as Canada, Argentina, Australia, Singapore, the United Kingdom, Ireland, Norway, the United States, Japan, and Iceland. In all incidents, epidemiological investigations have identified humans as the possible source of infection for the pigs (28, 30). Experimentally, it was established that the virus is pathogenic and is readily transmitted in pigs (9, 31, 39, 70, 75). It also induces clinical signs of disease and respiratory tract pathology similar to those induced by other influenza A viruses of swine (9, 31, 39, 70, 75). The natural outbreaks of the H1N1pdm virus and laboratory studies underscore the threat that the virus poses to the swine industry.
The rapid spread of the H1N1pdm virus around the globe and its ability to cross the species barrier highlight the need to develop effective control strategies. In this regard, the development of safe and potent vaccines that are effective in more than one animal species would be highly desirable. Live attenuated influenza vaccines (LAIVs) closely mimic natural infection and have several advantages over inactivated vaccines. LAIVs trigger cell-mediated immunity (CMI) and mucosal immune responses, thereby providing longer-lasting immunity and broader antigenic coverage than conventional inactivated vaccines (16, 24, 29). In the United States, a trivalent live attenuated influenza vaccine (FluMist) containing two type A viruses (H1N1 and H3N2) and a type B virus has been licensed for use in humans since 2003 (2, 3). Moreover, human LAIVs have been used for many years in Russia without the emergence of new influenza virus reassortants, thus demonstrating the stability of these attenuating phenotypes (2, 3, 14, 38, 46). In veterinary medicine, an equine influenza virus LAIV (Flu Avert I.N. vaccine; Intervet) has been developed for horses and is available commercially in North America (53). Field experience with both the human and the equine live influenza vaccines have demonstrated the safety, effectiveness, and genetic and phenotypic stability of these vaccine platforms (7, 8, 11, 14, 41, 53, 56, 65, 67).
In swine medicine, however, temperature-sensitive (ts) LAIVs have not yet been developed, despite their demonstrated safety and efficacy for other animals. More recently, live attenuated vaccines based on deletions in the NS1 viral protein have been shown to provide protection in swine (58, 73). Currently, commercially available swine influenza vaccines are based on inactivated whole-virus preparations of the H1N1 and H3N2 subtypes. Vaccination has become a common practice to control swine influenza in the United States. Nonetheless, these commercially available vaccines provide limited protection against the antigenically diverse influenza viruses that circulate in North American pigs, and consequently, swine producers are forced to use autogenous inactivated vaccines with the hope of achieving better antigenic matching (71). However, it should be noted that the use of inactivated vaccines has been associated with enhanced pneumonia when immunized pigs are challenged with divergent viruses (71). Thus, the development of swine LAIVs has the potential to circumvent the drawbacks associated with commercial vaccines and to improve both homotypic and heterosubtypic protection in pigs against this important swine pathogen. Furthermore, the testing of newly developed LAIVs in swine offers the possibility of translating the findings to human medicine, given the similarity of influenza clinical signs, pathology, and distribution of sialic acid receptors between the two species (6, 49).
With the aim of developing temperature-sensitive LAIVs against the H1N1pdm virus, we have used reverse genetics to introduce attenuation markers into the polymerase genes of a swine-like TR H3N2 influenza virus, A/turkey/Ohio/313053/04 (H3N2) (ty/04) (66). We chose this isolate because it grows well in both eggs and cell culture-based substrates, displays a broad host range, and has internal genes similar to those of the H1N1pdm virus. These features highlight the potential of this backbone to induce strong immune responses in multiple animal species and possibly cross-protection against circulating TR strains in swine. We found that the genetically modified ty/04 backbone (ty/04 att) had impaired polymerase activity and viral growth at elevated temperatures. In vivo characterization in mice of two H1N1 vaccine candidates generated using this backbone demonstrated that this vaccine is attenuated, as indicated by the absence of any signs of disease upon vaccination, absent or limited replication in the respiratory tract, and minimum histopathological alterations in the lungs. More importantly, a single low dose of either of the H1N1 ty/04 att-based vaccines provided complete protection against a lethal H1N1pdm virus challenge in mice. Subsequently, we chose one of the ty/04 att-H1N1 vaccine candidates for further testing in swine and found that the vaccine was safe and conferred sterilizing immunity upon an aggressive intratracheal challenge of pigs with the 2009 H1N1 pandemic virus. Thus, the introduction of genetic signatures for att into the backbone of a swine-like TR influenza virus resulted in highly attenuated and efficacious live influenza vaccines with promising applications in both human and veterinary medicine.
MATERIALS AND METHODS
Ethics statement.
Animal studies were conducted under animal biosafety level 3 (ABSL-3) conditions, approved by the U.S. Department of Agriculture (USDA), according to protocols R-09-93 (“Transmissibility of Influenza A Viruses”), R-08-16 (“Transmissibility of Influenza A Viruses in Swine”), R-09-55 (“Evaluation of Attenuation and Protection Efficiency of Live Attenuated Influenza Vaccines”), and R-09-68 (“Evaluation of the Pathogenesis of Swine-Like Human H1N1 and Live Attenuated Vaccines in a Mouse Model”), approved by the Institutional Animal Care and Use Committee of the University of Maryland. In addition, swine studies were performed under Animal Care and Use protocol 3950 (“Influenza A Virus Pathogenesis and Host Response in Swine”), approved by the USDA Agricultural Research Service (ARS) Animal Care and Use Committee, Ames, IA. Animal studies adhered strictly to the U.S. Animal Welfare Act (AWA) laws and regulations.
Cell lines and virus strains.
Human embryonic kidney (293-T) cells were cultured in Opti-MEM I (Gibco, Grand Island, NY) containing 5% fetal bovine serum (FBS) and antibiotics. Madin-Darby canine kidney (MDCK) cells were maintained in modified Eagle's medium (MEM) (Sigma-Aldrich, St. Louis, MO) supplemented with 5% FBS ((Sigma-Aldrich, St. Louis, MO) and antibiotics.
A/turkey/Ohio/313053/04 (H3N2) (ty/04) has been described previously and was kindly provided by Yehia Saif, Ohio State University, Wooster (66). A/California/04/09 (H1N1) (Ca/04) was kindly provided by the CDC, Atlanta, GA. The lethal mouse-adapted Ca/04 (ma-Ca/04) strain was generated in our laboratory by adapting wild type Ca/04 in DBA/2 mice through a single lung passage (77). The recombinant viruses used in this paper were generated from cloned cDNAs and are described below and in Table 1. All experiments using the pandemic H1N1 virus or its wild-type reassortants were performed under ABSL-3 conditions approved by the USDA.
TABLE 1.
Influenza viruses used in this study
| Virus | Abbreviation in main text |
|---|---|
| A/California/04/09 (H1N1)a | Ca/04 |
| Mouse-adapted A/California/04/09 (H1N1)b | ma-Ca/04 |
| A/turkey/Ohio/313053/04 (H3N2)c | ty/04 WT |
| Reverse-genetics A/turkey/Ohio/313053/04 (H3N2)d | ty/04 RG |
| A/turkey/Ohio/313053/04 (H3N2) atte | OH 2:6 ty/04 att |
| Surface genes from A/New York/18/09 (H1N1) in ty/04 att backbonef | NY 2:6 ty/04 att |
| Surface genes from A/Netherlands/602/09 (H1N1) in ty/04 att backboneg | NL 2:6 ty/04 att |
| Surface genes from A/Netherlands/602/09 (H1N1) in ty/04 WT backboneh | NL 2:6 ty/04 WT |
| A/Netherlands/602/09 (H1N1)i | NL WT |
GenBank taxonomy ID2, 641501.
Lethal for BALB/c mice.
GenBank taxonomy ID, 533026.
Generated entirely from cloned cDNA.
A/turkey/Ohio/313053/04 (H3N2) carrying temperature-sensitive mutations in both PB2 and PB1 and an HA tag in the carboxyl terminus of PB1.
A 2:6 reassortant containing the surface genes of A/New York/18/09 (H1N1) (GenBank taxonomy ID2, 643545) and the internal genes from the attenuated ty/04 att virus.
A 2:6 reassortant containing the surface genes of A/Netherlands/602/09 (H1N1) (GenBank taxonomy ID2, 643212) and the internal genes from the attenuated ty/04 att virus.
A 2:6 reassortant containing the surface genes of A/Netherlands/602/09 (H1N1) (GenBank taxonomy ID2, 643212) and the internal genes from unmodified ty/04 WT.
A/Netherlands/602/09 (H1N1) (GenBank taxonomy ID2, 643212) generated entirely from cloned cDNA.
Generation of recombinant viruses.
The A/turkey/Ohio/313053/04 (H3N2) (ty/04) strain was generated by reverse genetics (RG) using a previously described method (26). Briefly, viral RNA (vRNA) was extracted from stock virus by using the RNeasy kit (Qiagen, Valencia, CA) according to the manufacturer's instructions. Reverse transcription was carried out with the uni-12 primer (5′-AGCAAAAGCAAAGG-3′) and avian myeloblastosis virus (AMV) reverse transcriptase (Promega, Madison, WI), and the viral genes were PCR amplified using a set of universal primers (27). Purified PCR products were digested with either BsaI or BsmBI and were cloned into the pDP2002 vector, which is derived from the pHW-2000 vector (26), in which a spacer sequence of 444 bp was cloned between the two BsmBI sites to allow visual monitoring of vector digestion efficiency through agarose gel electrophoresis. The resulting clones were fully sequenced and were compared to the wild-type (WT) viral consensus sequence. Primer sequences are available upon request. The entire plasmid set for A/Netherlands/602/09 (H1N1) (NL WT) was kindly provided by Ron A. Fouchier, Erasmus Medical Center, Rotterdam, Netherlands, whereas the HA and NA RG plasmids for A/New York/18/09 (H1N1) (NY) were kindly provided by Ruben Donis, Influenza Division, Centers for Disease Control and Prevention, Atlanta, GA.
The genetic signatures for attenuation of an avian influenza virus have been described previously (63). Here the same modifications were introduced into the PB2 and PB1 genes of ty/04. Briefly, the ts mutations in PB1 and PB2 were introduced by site-directed mutagenesis using a commercially available kit (Stratagene, La Jolla, CA), whereas the HA tag epitope was introduced by subcloning this sequence from WF10 att (63) into the PB1 gene of ty/04 to generate ty/04 att. The recombinant WT viruses, as well as the 2:6 surface gene reassortants, were generated by transfecting the RG plasmids into cocultured 293T and MDCK cells as previously reported (26). NL 2:6 ty/04 WT is a 2:6 reassortant with the surface genes from the NL virus and the internal genes from the wild-type ty/04 virus. NY 2:6 ty/04 att and NL 2:6 ty/04 att are surface gene reassortants between the NY or NL virus, respectively, and the ty/04 att internal genes. All viruses were amplified in MDCK cells to produce viral stocks.
Viral ribonucleoprotein (vRNP) reconstitution assay for the study of polymerase activity.
A model vRNA, consisting of the Gaussia luciferase (GLuc) open reading frame flanked by the noncoding regions of the influenza virus NS segment (pGLuc-NS), was used to assess polymerase activity in a minigenome reconstitution assay (Fig. 1A). Briefly, 293T cells were seeded in 6-well plates and were transfected with 1 μg of the reporter plasmid along with 1 μg each of the pDP2002 plasmids encoding PB2, PB1, PA, and NP by using the TransIT-LT1 (Mirus, Madison, WI) reagent according to the recommendations of the manufacturer. In addition, the pCMV/SEAP plasmid, which encodes a secreted alkaline phosphatase (SEAP) gene, was cotransfected into the cells to normalize the transfection efficiency. At the indicated time points, supernatants from transfected cells were harvested and assayed for both luciferase and secreted alkaline phosphatase activities by using the BioLux Gaussia luciferase assay kit (New England Biolabs, Ipswich, MA) and the Phospha-Light secreted alkaline phosphatase reporter gene assay system (Applied Biosystems, Foster City, CA) according to the manufacturers' protocols. Relative polymerase activity was calculated as the ratio of luciferase luminescence to SEAP luminescence for three independent experiments.
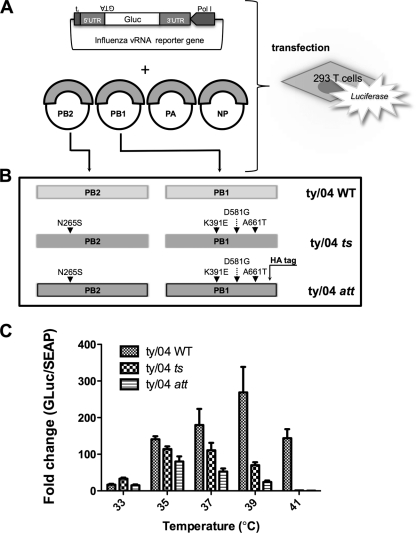
FIG. 1.
Viral ribonucleoprotein reconstitution assay to study the polymerase activities of ty/04 WT and its mutants. (A) 293-T cells were transfected with plasmids encoding the minimal components required for viral transcription and replication (the PB1, PB2, and PA polymerase subunits, NP, and a vRNA influenza virus-driven luciferase reporter replicon). The influenza virus reporter plasmid contains the open reading frame of Gaussia luciferase (GLuc) flanked by the 5′ and 3′ untranslated regions (UTR) of the influenza virus NS segment. This cassette was inserted between the human polymerase I promoter (Pol I) and terminator (tI) sequences. The presence of luciferase protein in the supernatant is measured by a luciferase assay. (B) Schematic representation of the ty/04 PB2 and PB1 constructs for the generation of ts and att mutant viruses. Site-directed mutagenesis was used to introduce 1 temperature-sensitive (ts) mutation into the PB2 gene (N265S) and 3 ts mutations into the PB1 gene (K391E, D581G, and A661T) of A/turkey/Ohio/313053/04 (H3N2) to generate ty/04 ts. The PB1 gene was further modified by incorporating an HA tag into the carboxy terminus of PB1 to generate ty/04 att. (C) Polymerase activities of WT ty/04 and its mutants at different temperatures. 293-T cells were transfected with 1 μg each of the influenza virus-driven luciferase reporter plasmid and the PB2, PB1, PA, and NP plasmids and were incubated at different temperatures as shown. pCMV/SEAP, which encodes secreted alkaline phosphatase, was cotransfected into the cells to normalize the transfection efficiency. At 24 h posttransfection, the supernatant was harvested and assayed for both luciferase and phosphatase activities. Normalized polymerase activities (means ± standard errors) were determined from three independent experiments.
Replication of recombinant viruses at different temperatures.
The ts phenotypes of WT and att viruses were evaluated by titrating the stock viruses at 33, 35, 37, 39, and 41°C by the 50% tissue culture infective dose (TCID50) method in MDCK cells as previously described (15, 32, 34). Replicates of 10 wells were used for each dilution. Cells were incubated at the respective temperatures for 3 days, and the presence of virus in each well was determined by an HA assay. The ts phenotype of a virus was defined by a 2 log10 reduction in the titer at 39°C from the titer at 33°C (63).
Immunization and challenge studies in mice.
Seven-week-old female BALB/c mice (Charles River Laboratories, Frederick, MD) were anesthetized with isoflurane prior to intranasal inoculation. Mice were inoculated with 50 μl containing 105 TCID50 of recombinant virus in phosphate-buffered saline (PBS)/mouse. Each experimental group contained 10 animals. Group 1 received PBS alone as a vaccine negative control. Groups 2, 3, 4, and 5 were inoculated with NY 2:6 ty/04 att, NL 2:6 ty/04 att, NL 2:6 ty/04 WT, and NL WT, respectively. Groups 4 and 5 served as positive controls for the vaccine and as references with which to evaluate the attenuation of the ty/04 att-based vaccines. Mice were bled using the submandibular bleeding method (22) prior to inoculation and at days 7, 21, 28, and 42 after immunization. At 3 days postinoculation (3 dpi), 3 animals from each group were humanely euthanized, and tissues were harvested for virus titration and histopathological evaluation.
Mice (n = 7) were challenged at 21 dpi with 20 50% mouse lethal doses (MLD50) of the lethal ma-Ca/04 strain by the intranasal route. At 5 days postchallenge (5 dpc), 3 mice from each group were euthanized, and their lungs were collected for histopathological analysis and measurement of the levels of the challenge virus. Tissue homogenates were prepared in PBS, clarified by centrifugation, and stored at −70°C until use. Clinical signs of disease, body weight, and mortality were monitored daily in the remaining mice.
Attenuation phenotype and efficacy of ty/04 att-based vaccines in swine.
Swine studies were conducted in the high-containment facilities of the National Animal Disease Center (NADC), Ames, IA, by following protocols approved by the NADC and the University of Maryland animal care and use committees. In both studies, 3-week-old crossbred pigs were obtained from a high-health herd free of swine influenza virus (SIV) and porcine reproductive and respiratory syndrome virus. All pigs were treated with ceftiofur crystalline free acid (Pfizer Animal Health, New York, NY) to reduce the level of bacterial contaminants prior to the start of the experiment. Animals that received the inactivated Ca/04 vaccine were housed under ABSL-2 conditions, and those that received the NY 2:6 ty/04 att vaccine or challenge Ca/04 virus were maintained under ABSL-3 conditions.
Safety of ty/04 att-based vaccines in pigs.
Twenty-five pigs were randomly divided into five treatment groups of five animals each and were housed in separate isolation rooms. To further evaluate the safety of the ty/04 att backbone in swine, groups of pigs were intranasally inoculated with 105 TCID50/animal of either the OH 2:6 ty/04 att (a virus that carries the surface genes of ty/04 WT and the internal genes of ty/04 att) or the NY 2:6 ty/04 att vaccine diluted in 2 ml of MEM. Two other groups were similarly inoculated with ty/04 WT or ty/04 RG and served as controls for comparison of the attenuation phenotype of the modified ty/04 att backbone, whereas a fifth group was mock vaccinated with PBS alone. Clinical observations and rectal temperatures were recorded individually on day −2 through day zero in order to establish normal baseline values for each animal. Nasal swabs were collected before vaccination and daily for 3 days as previously described (69, 70). Following inoculation, rectal temperatures and clinical signs of disease were monitored daily until the terminus of the experiment (3 dpi), when the animals were humanely euthanized and necropsy was performed.
Efficacy of H1N1 ty/04 att vaccines in pigs.
Forty pigs were randomly divided into four groups of 10 pigs each (see Table 4). Group 1 was vaccinated with 105 TCID50/animal of NY 2:6 ty/04 att by the intranasal route, whereas group 2 was vaccinated intramuscularly with 2 ml of an adjuvanted UV-inactivated Ca/04 vaccine (UVadj-Ca/04) as previously described (69). Briefly, the inactivated experimental vaccine was prepared from WT Ca/04 at 8 HA units per 50 μl (or 105 TCID50/ml) with inactivation by UV irradiation and addition of a commercial adjuvant (Emulsigen D; MVP Laboratories) at a virus-to-adjuvant ratio of 4:1 (vol/vol). Group 3, nonvaccinated and challenged (NV + Ca/04), and group 4, nonvaccinated and mock challenged (NV + Mock), were also included in the vaccine trial. At 2 weeks after primary immunization, the pigs were boosted using the same vaccines, doses, and routes as described for primary vaccination. Fourteen days postboost (14 dpb), pigs from groups 1 to 3 were challenged intratracheally with 2 ml of 1 × 105 TCID50 of Ca/04 as previously described (69). Following challenge, pigs were monitored daily for hyperthermia and clinical signs of disease for 5 days, at which time the animals were euthanized and necropsied. Virus shedding in nasal secretions was measured at 3 and 5 dpc. Blood samples were collected at day −3 (prebleed), at 14 days postvaccination (14 dpv), and at 0 dpc and 5 dpc for analysis of the humoral antibody response against Ca/04.
Pathological examination of swine lungs after vaccination and challenge.
At necropsy, lungs were removed in toto and were evaluated to determine the percentage of the lung affected with purple-red, consolidated lesions, which are typical of influenza virus infection in pigs. The percentage of the lung affected with pneumonia was estimated visually for each lobe, and a total percentage for the entire lung was calculated based on weighted proportions of each lobe to the total lung volume as previously described (23). Each lung was then lavaged with 50 ml MEM to obtain bronchoalveolar lavage fluid (BALF). Tissue samples from the trachea and right cardiac lung lobe and from other affected lobes were taken for histopathological examination. Lung sections were given a score from zero to 3 to reflect the severity of bronchial epithelial injury by using previously described methods (57).
HI assay.
Serum samples were treated with receptor-destroying enzyme (Accurate Chemical and Scientific Corp., Westbury, NY) to remove nonspecific inhibitors, and the antiviral antibody titers were evaluated using the hemagglutination inhibition (HI) assay method outlined by the WHO animal influenza training manual (75a). HI assays were performed using turkey red blood cells (RBC) with NY 2:6 ty/04 att and wild-type Ca/04 as the HI antigens. Log2 transformations were analyzed and reported as geometric mean titers (GMT).
Quantification of antibody isotypes in porcine BALF samples.
The presence of Ca/04-specific IgG and IgA antibodies in porcine BALF was detected by enzyme-linked immunosorbent assays (ELISAs) as previously described (69). Briefly, concentrated Ca/04 virus was resuspended in Tris-EDTA basic buffer, pH 7.8, and diluted to an HA concentration of 100 HA units/50 μl. Immulon-2HB 96-well plates (Dynex, Chantilly, VA) were coated with 100 μl of antigen solution and were incubated at room temperature overnight. Plates were blocked for 1 h with 100 μl of 10% bovine serum albumin (BSA) in PBS and were washed three times with 0.05% Tween 20 in PBS prior to the addition of test BALF. The assays were performed on each BALF sample in triplicate. Peroxidase-labeled goat anti-swine IgA (Bethyl, Montgomery, TX) or IgG (Kirkegaard & Perry Laboratories, Gaithersburg, MD) were used as secondary antibodies. Antibody levels are reported as mean optical densities (ODs), and the mean ODs of the different treatment groups are compared after the triplicate samples of each animal have been averaged.
Titration of virus stocks and virus present in biological samples.
Viral stocks and virus present in animal samples (clarified tissue homogenates, nasal swabs, or BALF) were titrated on MDCK cells, and the TCID50 per milliliter was determined by the method of Reed and Muench (55). Briefly, samples were serially diluted 10-fold in serum-free medium containing antibiotics and 1 μg/ml tosylsulfonyl phenylalanyl chloromethyl ketone (TPCK)-trypsin (Sigma, St. Louis, MO). Next, 100 or 200 μl of the inoculum was overlaid onto confluent monolayers of MDCK cells seeded in 96-well plates. The cells with samples were incubated for 3 days, and the endpoint viral titer was determined by an HA assay or immunostaining with a monoclonal antibody against influenza A virus nucleoprotein as previously described (69).
Histopathology.
Nasal turbinate, lung, and trachea samples were fixed in 10% buffered formalin and were embedded in paraffin by following standard histopathological procedures. Sections (thickness, 5 μm) were cut from the lung and were stained with hematoxylin and eosin (H&E). The degree of microscopic lesions was determined, and representative pictures were taken from each slide.
Statistical analysis.
All statistical analyses were performed using GraphPad Prism software, version 5.00 (GraphPad Software Inc., San Diego, CA). Comparisons between two treatment means were carried out using a two-tailed Student t test, whereas multiple comparisons were carried out by analysis of variance (ANOVA) using Tukey's posthoc test, unless otherwise specified. Correlations were determined with bivariate correlation procedures (Pearson's correlation procedure). The differences were considered statistically significant at a P value of <0.05.
RESULTS
The swine-like TR influenza virus att backbone has impaired polymerase activity at elevated temperatures.
The molecular features that control the ts phenotype of the master donor virus (MDV) A/Ann Arbor/6/60 (H2N2) have been mapped to five mutations distributed in the PB2 (N265S), PB1 (K391E, E581G, and A661T), and NP (D34G) segments (32). In previous studies, we showed that these genetic signatures can be transferred to an H9N2 avian influenza virus and impart the same ts phenotype. However, the ts avian influenza virus was not sufficiently attenuated in chickens, which raised potential safety concerns (63). Thus, an additional genetic modification, an HA tag epitope in the C terminus of the PB1 gene, was introduced to enhance the ts phenotype in vitro and the att phenotype in birds and mammals (25, 63). Moreover, viruses carrying the ts loci along with the HA tag, here designated att viruses, were both genetically and phenotypically stable, a critical feature in the development of live att influenza vaccines.
In this study, we wanted to ascertain whether our dual-attenuation approach could be introduced into the swine-like TR genetic backbone of the A/turkey/Ohio/313053/04 (H3N2) (ty/04) strain. The ty/04 strain is an ideal candidate for an att vaccine backbone, because this virus has been shown to replicate in several animal species, such as chickens, turkeys, and swine (76). We altered the PB2 and PB1 genes of ty/04 by incorporating ts mutations in both genes, and we also incorporated the HA tag into PB1 (Fig. 1A and B). Additionally, the WT ty/04 PB1 gene encodes aspartic acid at position 581, in contrast to the WT PB1 gene of A/Ann Arbor/6/60, which encodes glutamic acid.
The ts effect of mutations in the polymerase complex of ty/04 was analyzed at different temperatures by using a viral ribonucleoprotein (vRNP) reconstitution assay as described above (Fig. 1A). 293-T cells were cotransfected with plasmids encoding the ty/04 PB2, PB1, PA, and NP genes and the influenza replicon carrying a secreted luciferase (GLuc). Transfection efficiency was normalized using a plasmid encoding the secreted alkaline phosphatase (SEAP) gene. The extent of influenza virus polymerase activity is expressed as the relative fold change in the level of GLuc versus SEAP. Transfections were performed at different temperatures (33, 35, 37, 39, and 41°C), and the supernatants were harvested 24 h posttransfection for quantification of reporter gene expression. The introduction of ts and att mutations into the PB2 and PB1 genes of ty/04 led to significantly lower polymerase activities than those of WT genes at nonpermissive temperatures (Fig. 1C). In addition, the temperatures at which the viruses with different backbones reached maximal polymerase activity, as indicated by luciferase activity, also differed. The highest polymerase activity of ty/04 att was detected at 35°C, whereas polymerase activity peaked at 39°C for ty/04 WT and between 35 and 37°C for ty/04 ts (Fig. 1C). More importantly, the introduction of the HA epitope into PB1 had a deleterious effect in combination with the four ts mutations in PB1 and PB2, as evidenced by the fact that the att backbone showed the most marked reduction in polymerase activity at temperatures above 37°C. Taken together, these results indicate that the ts phenotype displayed by the modified human and avian influenza virus strains can be transferred to a swine-like TR backbone and that the inclusion of an HA epitope in PB1 enhances this phenomenon in human cells.
Genetically modified ty/04 att vaccines display restricted growth at nonpermissive temperatures.
In order to study the effects of the att mutations in the context of the viral life cycle, we compared the replication of WT and att H1N1pdm viruses in MDCK cells at different temperatures. Four different 2:6 reassortant viruses were tested: NY 2:6 ty/04 att, NL 2:6 ty/04 att, NL 2:6 ty/04 WT, and NL WT (Table 2). The NL 2:6 ty/04 WT and NL WT viruses replicated equally well at temperatures ranging from 33° to 39°C (Table 2). In agreement with the minigenome assay results, the two H1N1 ty/04 att viruses had at least a 100-fold reduction in virus titers at 39°C from those at 33°C, confirming the ts phenotype of this genetically modified vaccine backbone. In addition, the ty/04 att viruses were unable to replicate at 41°C, in contrast to NL 2:6 ty/04 WT and NL WT, which showed significant growth at 41°C (titers about 4 to 5 log10 units lower than those at 33°C). Thus, the two H1N1 ty/04 att vaccines displayed the expected ts phenotypes in a canine cell line.
TABLE 2.
Replication of recombinant viruses at different temperaturesa
| Virus | Log10 titerb at: |
||||
|---|---|---|---|---|---|
| 33°C | 35°C | 37°C | 39°C | 41°C | |
| NY 2:6 ty/04 att | 6.0 | 6.0 | 5.0 | 4.0 | BLD |
| NL 2:6 ty/04 att | 6.0 | 6.0 | 6.0 | 4.0 | BLD |
| NL 2:6 ty/04 WT | 7.8 | 8.3 | 8.0 | 7.8 | 4.2 |
| NL WT | 7.1 | 6.7 | 6.2 | 6.5 | 2.1 |
MDCK cells were inoculated with WT or att viruses and were incubated for 3 days at increasing temperatures (33, 35, 37, 39, and 41°C). The presence of the virus in each well was detected by an HA assay, and the log10 titer was determined by the TCID50 method.
Representative data from two independent experiments. Values in boldface indicate that the virus is temperature sensitive (100-fold reduction in virus titer at 39°C from that at 33°C). BLD, below the detection limit (0.6 log10 TCID50/ml).
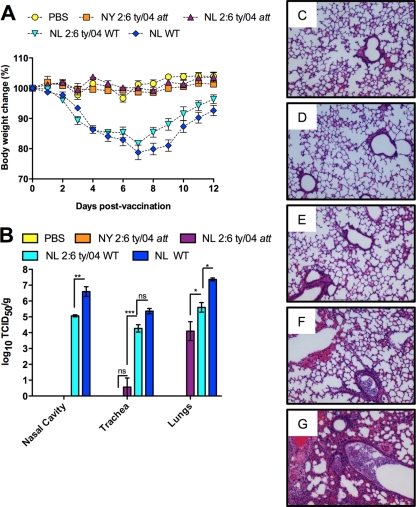
Genetically modified ty/04 att vaccines are attenuated in mice.
To evaluate whether the reductions in the polymerase activity and virus replication of the ty/04 att-based viruses at nonpermissive temperatures would translate into an attenuated phenotype in vivo, we assessed weight loss, the levels of viral replication in the respiratory tract, and the extent of pulmonary pathology in BALB/c mice inoculated with these viruses. Groups of 10 mice were inoculated with 105 TCID50 of the recombinant viruses (Fig. 2) through the intranasal route. At 3 dpi, 3 animals from each group were humanely euthanized, and organs were collected for virus titration and histopathology. Body weight changes over 12 dpi were monitored daily as a parameter of influenza morbidity. The 2 ty/04 att vaccines were highly attenuated in mice, as demonstrated by the absence of clinical disease signs and the lack of change in body weight. In contrast, mice inoculated with a virus with the WT ty/04 backbone (NL 2:6 ty/04 WT) showed significant body weight loss (≤20%) by 7 dpi, although they eventually recovered. As expected, a noticeable reduction in body weight was also observed when mice received NL WT, and recovery was slightly delayed in comparison to that for the NL 2:6 ty/04 WT group (Fig. 2A). Upon examination of tissue tropism and viral replication, the NY 2:6 ty/04 att virus was not detected in any of the organs sampled (nasal cavity, trachea, or lungs). Lung sections from the NY 2:6 ty/04 att group were indistinguishable from those of mock-inoculated controls at the microscopic level, corroborating that the ty/04 att LAIV is highly attenuated (Fig. 2C and D). Although mice inoculated with NL 2:6 ty/04 att showed no signs of disease upon vaccination, there was limited viral replication in the lower respiratory tracts of these animals. However, replication in the trachea was detected only in a single individual (17 TCID50/g of tissue), and the titers in the lungs were significantly lower than those obtained for the NL 2:6 ty/04 WT group (Fig. 2B). Only mild histopathological alterations were detected in the lungs of a single mouse inoculated with the NL 2:6 ty/04 att virus, suggesting that pulmonary replication of this att vaccine virus does not lead to significant pathological damage in the lungs (Fig. 2B and E). In contrast, mice inoculated with NL 2:6 ty/04 WT had high viral replication (104 to 106 TCID50) in the entire respiratory tract and moderate histopathological alterations in the lungs, characterized by necrotizing bronchitis, bronchiolitis, and various degrees of hemorrhage (Fig. 2B and F). Infection with NL WT resulted in 10- to 100-fold higher viral titers in the respiratory tract (105 to 107 TCID50) than those for the NL 2:6 ty/04 WT group (Fig. 2B). Consistently, the NL WT-inoculated group showed more-severe pathology in the lungs than the NL 2:6 ty/04 WT group (Fig. 2G), suggesting that the internal genes from the H1N1pdm virus are more virulent in mice than the internal genes from the North American TR viruses. Taking these findings together, the double-attenuation strategy resulted in a swine-like TR backbone that displayed desirable safety properties in the mouse influenza model.
FIG. 2.
Safety of ty/04 att H1N1 vaccines in BALB/c mice. Groups of 10 mice each were inoculated intranasally with 105 TCID50s of the recombinant virus. One group received PBS and served as a vaccine negative control. (A) Percentage of change in body weight as a measure of morbidity following intranasal inoculation of mice with either a ty/04 WT or a ty/04 att virus. Mice were weighed daily for 12 days. (B) Replication and tissue tropism of WT and att H1N1 viruses in the respiratory tracts of mice. At 3 dpi, three animals from each group were euthanized, and virus titers in the respiratory tract were determined by standard TCID50 in MDCK cells. Log10 titers for each group are plotted as means ± standard errors. *, P < 0.05; **, P < 0.01; ***, P < 0.001; ns, not significant. (C, D, E, F, and G) Lung histopathology of mice inoculated with ty/04 WT or ty/04 att viruses at 3 dpi. A representative image from each treatment group is shown. (C) Lung of a control mouse showing normal bronchiole and alveoli. (D and E) Lungs from animals inoculated with NY 2:6 ty/04 att or NL 2:6 ty/04 att, respectively, are indistinguishable from those of mock-infected animals. (F) Lung of a mouse infected with the NL 2:6 ty/04 WT virus, showing moderate histopathological lesions, including necrotizing bronchiolitis, the presence of cell debris, and various degrees of hemorrhage. (G) Lung of a mouse infected with NL WT, displaying more-severe histopathology characterized by necrotizing bronchiolitis, the presence of cell debris and inflammatory infiltrates, hyperemia, and hemorrhage.
The ty/04 att-based vaccines are attenuated in swine.
In order to further evaluate the safety of the ty/04 att vaccine backbone, groups of pigs (n = 5) were inoculated intranasally with ty/04 att vaccines containing either H1N1 or H3N2 surfaces. The H1N1 surface genes were derived from A/New York/18/09 (H1N1), whereas the H3N2 genes were from the A/turkey/Ohio/313053/04 (H3N2) isolate (Table 1). ty/04 WT and ty/04 RG viruses were included as nonattenuated virus controls. Clinical signs of disease and rectal temperatures were monitored, and nasal swabs were collected daily to quantify virus shedding in nasal secretions. At 3 dpi, pigs were euthanized; the degree of lung pathology was determined; and the presence of virus in BALF samples was titrated. Pigs inoculated with nonattenuated ty/04 viruses developed a febrile response (>40°C) that peaked 24 h postinoculation (24 hpi) (Fig. 3A) and shed large amounts of virus (3 to 5 log10 TCID50/ml) in nasal secretions (Fig. 3B). Similarly, viral titers in BALF collected at 3 dpi ranged from 105 to 106 TCID50/ml (Fig. 3C). At necropsy, as much as 15% of the total lung area for animals inoculated with these viruses (mean percentages, 7.5 and 7.4% for ty/04 WT and ty/04 RG, respectively) displayed pneumonic lesions typical of influenza infection in pigs (Fig. 3D). In general, the gross lesions were marked, plum-colored consolidated areas located mainly in the cranioventral lobes of the lung. Microscopically, lesions in lungs were typical of influenza virus infection in pigs and were characterized by multifocal to widespread necrotizing bronchitis and bronchiolitis, light peribronchiolar lymphocytic cuffing, and mild multifocal interstitial pneumonia with various degrees of alveolar involvement (Fig. 3E). Clinical signs of disease, lung pathology, and viral replication in biological samples were indistinguishable between the ty/04 WT and RG viruses, confirming that the ty/04 virus generated through RG displays a phenotype identical to that of the WT virus. In contrast, none of the animals inoculated with H3N2 or H1N1 ty/04 att viruses developed a fever, cough, or other clinical signs following vaccination, indicating that the ty/04 att viruses were safe for administration to pigs (Fig. 3A). Correspondingly, 100- to 1,000-fold less virus was shed from the noses of pigs vaccinated with ty/04 att viruses than from those of pigs vaccinated with unmodified ty/04 viruses. In general, NY 2:6 ty/04 att-vaccinated pigs shed less virus than H3N2 OH 2:6 ty/04 att-inoculated pigs (Fig. 3B). In addition, viral titers in BALF were significantly lower (P < 0.01) in ty/04 att-vaccinated pigs than in ty/04 WT-infected pigs (Fig. 3C). Although both vaccines caused mild gross and microscopic lesions in the lungs, the percentage of lung involvement was not significantly different from that for mock-vaccinated pigs (P > 0.05 by Dunnett's test), corroborating the clinical findings that these vaccines are sufficiently attenuated in pigs (Fig. 3D and E). Histopathologically, the nasal turbinates and tracheae obtained from pigs immunized with either vaccine were similar to those of control animals, in contrast to those of the WT-inoculated pigs (Fig. 3E). Thus, modified ty/04 viruses displayed an att phenotype in swine, in agreement with the mouse studies.
FIG. 3.
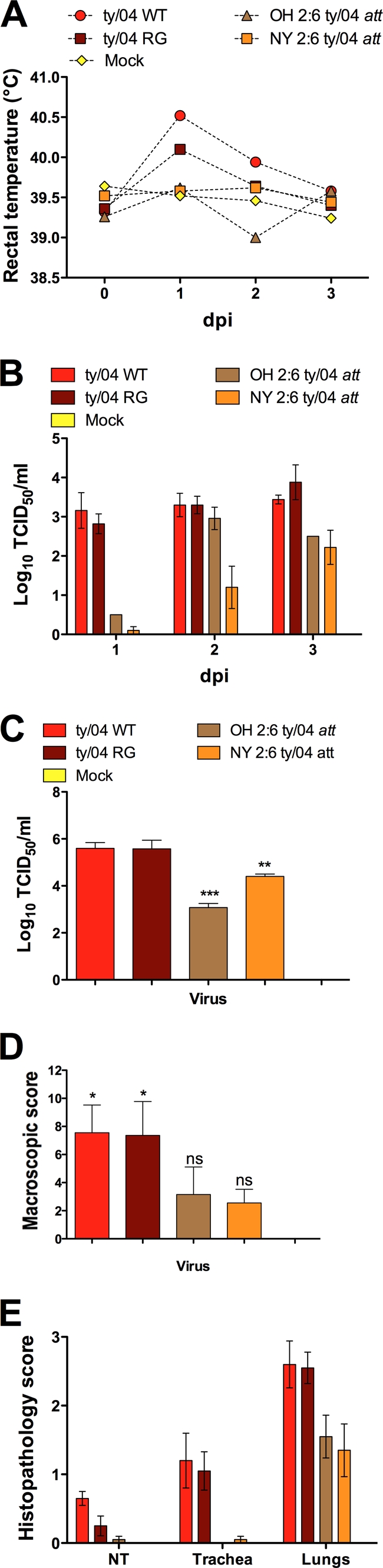
Attenuation phenotypes of H1N1 and H3N2 ty/04 att viruses in swine. Groups of pigs (n = 5) were randomly divided into five treatment groups and were inoculated intranasally with 105 TCID50s/animal of either the OH 2:6 ty/04 att (H3N2) or the NY 2:6 ty/04 att vaccine diluted in 2 ml of MEM. Two other groups were similarly inoculated either with ty/04 WT or with a WT virus generated from plasmid DNA (ty/04 RG) for comparison with the attenuation phenotype of the modified ty/04 att backbone. A fifth group was mock vaccinated with PBS alone (Mock). Nasal swabs and rectal temperature readings were taken daily. At 3 dpi, all animals were euthanized in order to measure viral replication and lung pathology. (A) Daily mean rectal temperatures of pigs following inoculation with a ty/04 WT or ty/04 att virus. (B and C) Viral titers determined by TCID50 on MDCK cells. Values are means ± standard errors of the means. Asterisks indicate values significantly different from those for the ty/04 WT control by Dunnett's test: *, P < 0.05; **, P < 0.01; ***, P < 0.001. (B) Viral shedding in nasal secretions of pigs. (C) Viral titers in bronchoalveolar lavage fluid collected at necropsy. (D and E) Macroscopic lung lesion scores (percentage of total lung area displaying macroscopic lesions) (D) and histopathological scores of nasal turbinates (NT), tracheae, and lungs (E) of swine inoculated with WT or ty/04 att viruses at 3 dpi. Lesions were compared to those of the sham-inoculated group by Dunnett's test. *, P < 0.05; ns, not significant.
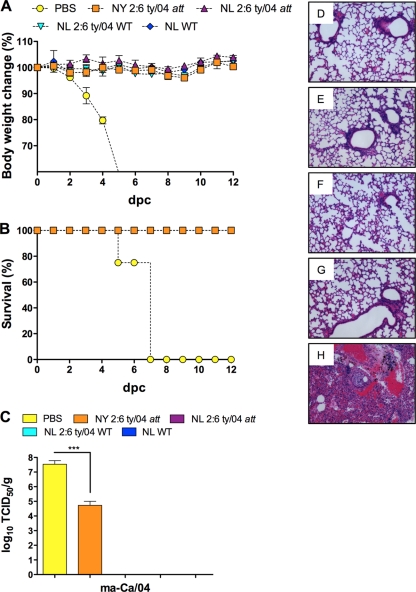
Vaccination with H1N1 ty/04 att-based vaccines confers complete protection against a lethal H1N1pdm virus challenge on mice.
Recent pathology studies have shown that H1N1pdm viral infections can lead to fatal viral pneumonia in a small percentage of cases (21, 54, 64). Thus, we have developed a lethal mouse model of H1N1pdm viral infection (77) that recapitulates the severe pneumonia induced by the novel H1N1 virus in human patients. Hence, we used this lethal model of severe H1N1 pneumonia to test whether the ty/04 att vaccines can induce protective immunity against lethal H1N1pdm virus infection.
To determine the robustness of protection induced by the two H1N1 ty/04 att vaccines, mice were intranasally challenged with 20 MLD50 of the lethal mouse-adapted Ca/04 virus at 21 dpv. Groups of mice immunized with WT H1N1 viruses (NL WT or NL 2:6 ty/04 WT) were also included as positive controls for the vaccine. Again, body weights were measured prior to the challenge infection and daily after challenge. At 5 dpc, the lungs from three animals of each group were collected for histopathology and virus titration. All the H1N1 ty/04 att-vaccinated animals were completely protected against the lethal ma-Ca/04 infection, as demonstrated by the absence of clinical signs of disease and the lack of change in body weight after challenge (Fig. 4A and B). More importantly, mice vaccinated with NL 2:6 ty/04 att had neither lung pathology nor detectable replication of the challenge virus (Fig. 4A, B, C, and D). The group that received the NY 2:6 ty/04 att vaccine showed a significantly lower level of challenge virus isolated from lungs by 5 dpc than the mock-vaccinated mice (Fig. 4C). Additionally, pulmonary histopathology was detected only in one individual in this group, which agreed with the clinical findings (Fig. 4E). As expected, the groups that were immunized with the WT H1N1 viruses were completely protected from challenge (Fig. 4A, B, and C) and had neither viral replication nor pathological alterations in the lungs (Fig. 4F and G). In contrast, all unvaccinated control mice developed severe signs of disease, such as lethargy, rough coat, dehydration, and loss of as much as 25% of body weight. The control mice died within 5 to 6 dpc (Fig. 4A and B). Examination of the lungs of the mock-immunized group revealed severe pneumonia characterized by extensive hemorrhagic lesions, necrotizing bronchitis and bronchiolitis, interstitial edema, and the presence of cell debris and inflammatory infiltrates in the alveoli (Fig. 4H). Infection by the ma-Ca/04 virus caused much more severe bronchopneumonia than the lesions induced by NL WT or NL 2:6 ty/04 WT upon immunization (compare Fig. 4H with 2G).
FIG. 4.
Protective efficacy of ty/04 att H1N1 vaccines against lethal H1N1pdm virus challenge in mice. Groups of mice (n = 7) were vaccinated with H1N1 recombinant viruses containing either att or WT backbones. A control group was mock vaccinated with PBS. All animals were challenged 21 days later with 20 MLD50 of the lethal mouse-adapted Ca/04 virus by the intranasal route. At 5 dpc, lungs from three animals were collected and processed for virus titration and histopathology. (A) Percentages of body weight change for naïve and vaccinated mice after lethal challenge. (B) Survival rates of naïve and vaccinated mice after lethal challenge. (C) Pulmonary replication of the challenge virus in mice. Values are means ± standard errors of the means. Triple asterisks indicate a significant difference (P < 0.001) between PBS and NY 2:6 ty/04 att. (D, E, F, G, and H) Lung pathology following a lethal ma-Ca/04 challenge. Immunized animals showed no significant histopathological changes. Lungs of mice immunized with NL 2:6 ty/04 att (D), NY 2:6 ty/04 att (E), NL 2:6 ty/04 WT (F), or NL WT (G) are shown. (H) Mock-vaccinated mice had severe bronchopneumonia after lethal challenge that was characterized by extensive hemorrhagic lesions, necrotizing bronchitis and bronchiolitis, interstitial edema, and the presence of cell debris and inflammatory infiltrates in the alveoli and airways.
In order to evaluate the immune responses induced by the ty/04 att vaccines that protected mice against lethal H1N1pdm challenge, we measured the levels of anti-Ca/04 antibodies in the sera of immunized mice using an HI assay (Table 3). In general, the protection rate correlated with the HI antibody titer measured on the day of challenge (21 dpv). At 0 dpc, the GMT of antibodies against Ca/04 was slightly lower for the NY 2:6 ty/04 att vaccine group than for the NL 2:6 ty/04 att group, though the difference was not statistically significant. As expected, the highest GMT were induced by the nonattenuated viruses NL 2:6 ty/04 WT and NL WT. Mock-vaccinated animals had undetectable HI antibodies. We also found a positive correlation (Pearson's correlation coefficient [r2], 0.82; P < 0.05) between the invasiveness of the vaccines/viruses, i.e., the abilities of the H1N1 ty/04 att or WT viruses to replicate in the respiratory tract, and the levels of circulating HI antibodies. The least invasive vaccine, NY 2:6 ty/04 att, induced lower HI antibodies than the more invasive NL 2:6 ty/04 att vaccine. The highest HI titer was elicited by NL WT. Based on this correlation analysis, 82% of the variance in HI titers at 21 dpv could be explained by the differences in the abilities of the viruses to replicate in the lungs. Collectively, these results suggested that a single low-dose inoculation of the ty/04 att LAIV could prevent histopathological alterations in the lungs and provide complete protection against lethal pandemic H1N1 virus-induced pneumonia.
TABLE 3.
Immunogenicities of ty/04 att H1N1 vaccines in mice
| Group | HI titera at: |
||
|---|---|---|---|
| 0 dpv | 21 dpv | 21 dpc | |
| PBS | <10 | <10 | N/A |
| NY 2:6 ty/04 att | <10 | 25 | 1,076 |
| NL 2:6 ty/04 att | <10 | 89 | 1,810 |
| NL 2:6 ty/04 WT | <10 | 718 | 2,560 |
| NL WT | <10 | 1,016 | 2,560 |
Hemagglutination inhibition titer, given as the reciprocal of the highest dilution of serum that showed activity against the A/CA/04/09 (H1N1) virus. Values are GMT. N/A, not applicable (animals were dead at this time point).
Vaccination with H1N1 ty/04 att-based vaccines provides sterilizing immunity against an aggressive H1N1pdm virus challenge in pigs.
NY 2:6 ty/04 att was selected for a vaccination/challenge trial in swine because it was the most attenuated vaccine in mice and had limited shedding in pigs after vaccination. Because only inactivated influenza vaccines are currently licensed for use in the U.S. swine industry, we also compared side by side the efficacy of NY 2:6 ty/04 att with that of an experimental adjuvanted inactivated Ca/04 vaccine (UVAdj-Ca/04). Thus, at 2 weeks after boost immunization, pigs were challenged with 105 TCID50 of the virulent Ca/04 strain by intratracheal inoculation and were followed for 5 days. The clinical performance of the H1N1 vaccines in pigs is summarized in Table 4. Nonvaccinated and challenged (NV + Ca/04) animals developed clinical signs of disease after challenge and macroscopic lung lesions typical of influenza infection by 5 dpc. In addition, all 10 pigs from this group shed virus in the nose at both 3 and 5 dpc and had virus replicating in BALF at 5 dpc. Two doses of the UVAdj-Ca/04 vaccine provided satisfactory protection, as determined by reduced lung pathology and limited challenge virus replication in both the upper and lower respiratory tracts. However, 2 pigs in this group did shed virus in the nose at day 5, and 1 animal had detectable virus in BALF. Remarkably, none of the animals vaccinated with NY 2:6 ty/04 att had detectable infectious virus in nasal secretions or in the lungs, suggesting that replication of the challenge virus was abolished at the site of infection. Macroscopically, discrete lung lesions were detected in 50% of the animals immunized with the NY 2:6 ty/04 att vaccine; however, the percentage was lower than that for the group immunized with the inactivated vaccine, in which 90% of the animals developed limited gross pulmonary pathology upon challenge. Nevertheless, both vaccine groups had significantly lower (P < 0.001) percentages of macroscopic lung pathology than the NV + Ca/04 group. Microscopic changes associated with influenza infection in the lungs were reflective of the macroscopic pneumonia. As expected, nonvaccinated, mock-challenged (NV + Mock) controls remained healthy throughout the study and had neither significant macroscopic nor microscopic lesions in the lungs. No significant differences in rectal temperatures were detected between vaccinated groups and control groups on any day.
TABLE 4.
Clinical performance of the H1N1 ty/04 att-based vaccine in swine after challenge with pandemic H1N1 viruse
| Groupa | HI titerb | Mean score ± SEMc |
Avg log10 viral titerd in: |
Temp (°C) at 3 dpc | |||
|---|---|---|---|---|---|---|---|
| Macroscopic pneumonia | Microscopic pneumonia | Nasal swabs |
BALF (5 dpc) | ||||
| 3 dpc | 5 dpc | ||||||
| NY 2:6 ty/04 att | 16.2 (7/10) | 0.3 ± 0.1* | 0.5 ± 0.1* | 0 ± 0* | 0 ± 0* | 0 ± 0* | 39.4 ± 0.3 |
| UVAdj-Ca/04 | 20.0 (8/10) | 1.2 ± 0.6* | 0.3 ± 0.2* | 0 ± 0* | 0.4 ± 0* | 0.3 ± 0.3* | 39.5 ± 0.2 |
| NV + Ca/04 | <10 (0/10) | 5.5 ± 1.3 | 1.5 ± 0.4 | 2.2 ± 0.4 | 2.8 ± 0.2 | 3.9 ± 0.2 | 39.4 ± 0.2 |
| NV + Mock | <10 (0/10) | 0.2 ± 0.1* | 0 ± 0* | 0 ± 0* | 0 ± 0* | 0 ± 0* | 38.4 ± 0.3* |
NV + Ca/04, nonvaccinated, challenged positive-control group; NV + Mock, nonvaccinated, nonchallenged negative-control group.
Geometric mean HI titer against Ca/04 at the day of challenge. Numbers in parentheses are the number of animals that seroconverted/total animals per group.
Microscopic pneumonia scores range from zero to 3. Macroscopic pneumonia was scored as the percentage of total lung area displaying gross lesions.
Measured as TCID50 per ml of fluid.
Asterisked values are significantly different from those for the NV + Ca/04 control group (P < 0.05).
Serum samples were also collected at the day of challenge, and Ca/04-specific antibodies were examined by an HI assay. All pigs were negative for antibodies (HI titer < 10) at the start of the experiment. At the day of challenge, 8 out of 10 pigs in the inactivated-vaccine group had detectable HI antibodies against Ca/04, whereas 7 out of 10 animals in the NY 2:6 ty/04 att group were HI positive. The mean HI antibody titers measured at the day of challenge in the two vaccine groups were approximately the same (Table 4).
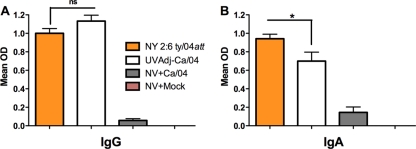
To characterize the immunoglobulins present in the lower respiratory tracts of swine, total levels of Ca/04-specific IgG or IgA isotype antibodies were measured by ELISA in BALF samples collected at necropsy (5 dpi). The data presented in Fig. 5 show the mean of the isotype response in each group. Levels of Ca/04-specific IgG were similar for the two vaccinated groups (Fig. 5A). In contrast, IgA levels in BALF from pigs in the NY 2:6 ty/04 att group were significantly higher than those in the inactivated-vaccine group (Fig. 5B). Taken together, these results suggest that the NY 2:6 ty/04 att vaccine is immunogenic in pigs and provides sterilizing immunity against pandemic H1N1 virus challenge.
FIG. 5.
Antibody isotype profiles in BALF samples of vaccinated pigs after challenge with the H1N1pdm virus. The levels of Ca/04-specific IgG (A) and IgA (B) antibodies present in BALF samples were quantified by ELISA. Groups of pigs (n = 10) were vaccinated twice either with the NY 2:6 ty/04 att vaccine or with an inactivated Ca/04 vaccine, challenged with the H1N1pdm virus at 2 weeks postboost, and necropsied at 5 dpi, when BALF was collected. Nonvaccinated pigs challenged with the Ca/04 virus (NV + Ca/04) and nonvaccinated, mock-challenged pigs (NV + Mock) were included as controls. Results are given as mean ODs ± standard errors of the means. *, P < 0.05 for comparison between the NY 2:6 ty/04 att and UVAdj-Ca/04 vaccines by the Student t test.
DISCUSSION
The 2009 H1N1 pandemic, caused by a triple-reassortant influenza virus, has spread worldwide and has had profound economic, health, and social impacts. This virus is the predominant circulating influenza virus among people in both the Northern and Southern Hemispheres (1) and has the ability to infect pigs experimentally and under natural conditions (9, 30, 39, 70, 75). Therefore, the development of alternative influenza vaccines for use in humans and animals would play an important role in mitigating the effects of the evolving H1N1 virus pandemic. Inactivated swine influenza vaccines are available for pigs; however, they do not provide either adequate immunity or cross-protection (71). This poor cross-protection associated with the use of inactivated vaccines was highlighted in a recent study, which reported only limited serologic cross-reactivity between sera from pigs vaccinated with contemporary H1 swine influenza viruses and the pandemic H1N1 2009 isolates (69). These findings are of major significance for the current scenario, given the possibility that 2009 H1N1 viruses could become established in swine. In the present study, we addressed this issue and developed temperature-sensitive LAIVs for use in pigs. Moreover, we used mouse and swine models to test the efficacy of our vaccine platform in protecting against severe H1N1pdm virus-induced pneumonia, which has been reported in some human fatalities (21, 54, 64).
In this study, we have used reverse genetics and molecular biology techniques to modify the polymerase genes of a swine-like TR influenza virus with the goal of developing alternative influenza vaccines for use in more than one animal species. We have previously shown that attenuation of an avian influenza strain required both the ts mutations found on the PB2 and PB1 genes of the A/Ann Arbor/6/60 (H2N2) human strain and incorporation of an HA tag epitope into the carboxy terminus of PB1 (63). Here we studied the effects of the ts and att (ts plus HA tag) mutations in the polymerase activity of a triple-reassortant influenza virus whose polymerase genes are of avian (PB2 and PA), human (PB1), and swine (NP) origins. We demonstrated that the introduction of ts mutations into the PB2 and PB1 subunits of a TR influenza virus severely impaired polymerase activity in human cells (293T) at nonpermissive temperatures. This effect on polymerase function was enhanced by the covalent attachment of an HA epitope in PB1. These results are in agreement with our previous studies in which incorporation of an HA tag in PB1 synergistically enhances the attenuating effects of the ts mutations in the context of an avian influenza strain (25, 63). It is not clear how the ts loci combined with the HA tag modulate polymerase activity at elevated temperatures. In addition, the mechanisms responsible for the restricted replication of the ts influenza viruses at the nonpermissive temperature have not been completely elucidated. A recently proposed mechanism to explain the ts phenotype involves multiple defects in the replication of the MDV A/Ann Arbor/6/60 harboring the ts loci. These defects include decreased vRNA synthesis, blockage of viral RNP export from the nucleus, reduced incorporation of M1, and production of virions with irregular morphology at 39°C (12).
To gain further insight into the phenotypic alterations caused by the att mutations in viruses containing the TRIG cassette, we investigated the replication of WT and att H1N1 viruses at different temperatures. In agreement with the RNP reconstitution assay and our previous reports (25, 63), the growth of the ty/04 att viruses was highly restricted at nonpermissive temperatures. Thus, introduction of the double mutations from an H9N2 avian virus into a divergent TR influenza virus strain was sufficient to transfer the ts phenotype.
The next step for evaluating live att influenza vaccines would be to test whether the vaccines were safe for use in mice and other animal models. Consistent with our in vitro data, all the H1N1 ty/04 att-based vaccines were sufficiently attenuated in mice, unlike their WT H1N1 counterparts, which caused clinical disease and pulmonary pathology. However, there were differences in the extent of attenuation depending on the origin of the surface protein genes. Although none of the ty/04 att vaccines caused clinical disease or major histopathological changes in mice, animals inoculated with NL 2:6 ty/04 att had higher levels of replication of the vaccine virus in the lungs than the group immunized with NY 2:6 ty/04 att. These findings were not unexpected, since our group and others have reported limited replication of LAIVs (att or ts) upon intranasal inoculation of mice and ferrets (14, 15, 25, 34). The difference in attenuation between the two vaccines suggests that the surface genes from A/Netherlands/602/09 carry virulent markers that might be absent in A/New York/18/09. In fact, a recent study reported a difference in virulence between Ca/04, which is more closely related to A/New York/18/09, and A/Netherlands/602/09 (45). These authors reported that A/Netherlands/602/09 was lethal to C57B/6 mice, in contrast to Ca/04, even though their genomes differ only in eight amino acid positions. Future studies investigating the contributions of individual amino acids to the delayed clearance of NL 2:6 ty/04 att compared to that of NY 2:6 ty/04 att will help to pinpoint virulence determinants in the surface glycoproteins of the H1N1pdm viruses.
We next evaluated the safety and efficacy of the double mutant live att influenza vaccines in pigs. Although other strategies, such as truncations of NS1 (58, 62, 73) and elastase growth restriction (47, 48), have been developed for attenuating live influenza viruses for use in swine, these technologies are relatively new and are not as well characterized as the ts vaccines. In addition to the impact of influenza infection on the swine industry, the testing of influenza vaccines in pigs also offers the possibility of extrapolating the findings to humans, since there are important similarities between the two species regarding the distribution of sialic acid receptors, cytokine production, and clinical-pathological outcomes after influenza infection (4-6, 49, 68). Data from our safety studies showed that both the H3N2 and H1N1 ty/04 att vaccines were attenuated in pigs, as evidenced by the absence of clinical signs of disease upon intranasal vaccination, reduced viral replication in the respiratory tract, and minimal pathological changes in the lungs. The decreased replication of the ty/04 att vaccines in the upper respiratory tracts of pigs is consistent with previous reports showing that the cold-adapted, temperature-sensitive A/Ann Arbor/6/60 influenza vaccines replicate to moderate levels in the nasal cavities of ferrets (13-15, 34) and that NS1-truncated H3N2 influenza vaccines also show limited replication in the nasal cavities in pigs (62). Although the ty/04 att vaccines were detected in BALF samples, the level of viral replication was significantly lower than that of unmodified virus and, more importantly, caused no overt clinical signs and only minimal pathology in the lungs. A minimal amount of replication is likely beneficial for eliciting T-cell responses to internal genes, which may provide heterologous cross-protection. These findings are also consistent with safety studies of truncated NS1-based vaccines in swine, which showed limited replication and pathology in the lower respiratory tract (62). Moreover, a detailed toxicological evaluation of the trivalent seasonal human LAIV or the H5N1 LAIV in ferrets showed that the virus replicated in the lungs and caused discrete to moderate bronchointerstitial inflammation at 3 days after intranasal administration and that these adverse effects correlated with the origin of the surface genes and with the dose and volume of the vaccine (33). Since we used a large volume (2 ml) in our vaccination experiments, the present study confirms and extends the safety studies of Jin and colleagues with ferrets (33). It has been shown that intranasal administration of volumes larger than 0.2 ml results in replication of the A/Ann Arbor/6/60 LAIV in the lower respiratory tracts of ferrets (33), but the authors also emphasized that the ferret studies did not accurately reflect the administration of this vaccine to humans, where intranasal delivery of a 0.5-ml inoculum containing radiolabeled albumin failed to reach the lower respiratory tract (10). Thus, our safety studies in swine could be more relevant than the ferret model for evaluating the adverse effects of live att influenza vaccines for use in humans.
One of the most challenging tasks in producing effective live attenuated vaccines is to achieve an adequate balance between safety and efficacy. By introducing the att modifications into the polymerase genes of a swine-like TR strain, this desirable balance was achieved. The vaccines were attenuated in both mice and pigs and, more importantly, elicited protective immunity in both species. In mice, the ty/04 att-based H1N1 vaccine proved to be efficacious against a lethal infection with the H1N1pdm virus. The mouse challenge model used in our vaccine trials attempted to recapitulate the severe pneumonia induced by the pandemic H1N1 virus in certain human patients. All vaccinated animals survived the lethal challenge and had no signs of morbidity following challenge, even though one vaccinated group had limited viral replication in the lungs. The incomplete clearance of challenge virus from the lungs of the immunized mice was not unexpected. Previously, we reported that mice vaccinated with the avian att backbone and challenged with a lethal dose of an H5N1 virus had viral replication in the lungs, although the animals were completely protected from disease (25). Our results are in agreement with this report, and it is noteworthy that the limited pulmonary replication of the challenge virus did not cause significant pathological changes, correlating with the clinical findings. The ty/04 att-based H1N1 vaccine was also immunogenic in swine and provided sterilizing immunity upon an aggressive challenge with the pandemic H1N1 virus, in contrast to an experimental inactivated-Ca/04 vaccine, which elicited protective but not sterilizing immunity in all animals. Although serum HI antibody titers were modest in the att H1N1 virus-vaccinated group at the day of challenge, high levels of Ca/04-specific IgA and IgG were detected in the lungs of all pigs in the group. The local antibody response is likely correlated with the protection from challenge with Ca/04. Cell-mediated immunity (CMI) in response to vaccination with the live att H1N1 virus is also likely involved in stimulating the strong mucosal antibody response, either through interaction with B cells, through helper T cells, or through cytotoxic T cells. Further studies are needed to address the role of CMI in the protective response induced by the live att H1N1 vaccine in swine.
In the face of influenza pandemics that have the ability to overcome the species barriers, such as the 2009 H1N1 pandemic, the supply of vaccines for use in agriculture could be jeopardized. Our cell culture-based live att H1N1 vaccines could be an attractive alternative for this possible pandemic vaccine shortage. Because the live ty/04 att vaccines developed here are efficacious in multiple species, are easier to manufacture than inactivated vaccines, and do not require adjuvants, our study represents a major advance in vaccine development for the 2009 H1N1 influenza pandemic.
In conclusion, we have demonstrated that the double attenuating mutations first implemented for an H9N2 avian influenza strain could be successfully transferred to a heterologous nonattenuated swine-like triple-reassortant influenza virus. Thus, our second generation of live att influenza vaccines based on modifications of the PB2 and PB1 genes of ty/04 expresses desirable biological traits in vitro, retains its safety properties in vivo, and can induce excellent protection against aggressive H1N1 virus challenges in more than one animal species. Our studies highlight the attenuation of the ty/04 att vaccine platform and its potential as a master donor strain for the generation of live attenuated vaccines with applications in both human and veterinary medicine.
Acknowledgments
We thank Yonas Araya, Erin Sorrell, and Danielle Hickman for assistance with mouse studies. We are indebted to Andrea Ferrero and Theresa Wolter for excellent laboratory managerial skills. Michelle Harland, Brian Pottebaum, and Jason Huegel are thanked for technical assistance and assistance with the swine study. We thank Ron A. Fouchier for providing the reverse genetics plasmids for A/Netherlands/602/09 (H1N1) and Ruben Donis at the Centers for Disease Control and Prevention, Atlanta, GA, for supplying the wild-type viruses and the NY HA plasmid used in this study. We also thank Troy Sutton for critical reading of the manuscript.
Mention of trade names or commercial products in this article is solely for the purpose of providing specific information and does not imply recommendation or endorsement by the U.S. Department of Agriculture. The opinions expressed in this article are those of the authors and do not necessarily represent the views of the granting agencies.
This research was made possible through funding by a CDC-HHS grant (1U01CI000355), an NIAID-NIH grant (R01AI052155), a CSREES-USDA grant (2005-05523), an NIAID-NIH contract (HHSN266200700010C), and USDA-ARS. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Footnotes
Published ahead of print on 20 October 2010.
The authors have paid a fee to allow immediate free access to this article.
REFERENCES
- 1.Al Hajjar, S., and K. McIntosh. 2010. The first influenza pandemic of the 21st century. Ann. Saudi Med. 30:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ambrose, C. S., C. Luke, and K. Coelingh. 2008. Current status of live attenuated influenza vaccine in the United States for seasonal and pandemic influenza. Influenza Other Respi. Viruses 2:193-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ambrose, C. S., T. Yi, R. E. Walker, and E. M. Connor. 2008. Duration of protection provided by live attenuated influenza vaccine in children. Pediatr. Infect. Dis. J. 27:744-748. [DOI] [PubMed] [Google Scholar]
- 4.Barbé, F., K. Atanasova, and K. Van Reeth. 22 January 2010. Cytokines and acute phase proteins associated with acute swine influenza infection in pigs. Vet. J. [Epub ahead of print.] doi: 10.1016/j.tvjl.2009.12.012. [DOI] [PMC free article] [PubMed]
- 5.Barbé, F., X. Saelens, D. Braeckmans, F. Lefevre, and K. Van Reeth. 2010. Role of IFN-α during the acute stage of a swine influenza virus infection. Res. Vet. Sci. 88:172-178. [DOI] [PubMed] [Google Scholar]
- 6.Barnard, D. L. 2009. Animal models for the study of influenza pathogenesis and therapy. Antivir. Res. 82:A110-A122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Belshe, R. B., C. S. Ambrose, and T. Yi. 2008. Safety and efficacy of live attenuated influenza vaccine in children 2-7 years of age. Vaccine 26(Suppl. 4):D10-D16. [DOI] [PubMed] [Google Scholar]
- 8.Block, S. L., R. Yogev, F. G. Hayden, C. S. Ambrose, W. Zeng, and R. E. Walker. 2008. Shedding and immunogenicity of live attenuated influenza vaccine virus in subjects 5-49 years of age. Vaccine 26:4940-4946. [DOI] [PubMed] [Google Scholar]
- 9.Brookes, S. M., R. M. Irvine, A. Nunez, D. Clifford, S. Essen, I. H. Brown, K. Van Reeth, G. Kuntz-Simon, W. Loeffen, E. Foni, L. Larsen, M. Matrosovich, M. Bublot, J. Maldonado, M. Beer, and G. Cattoli. 2009. Influenza A (H1N1) infection in pigs. Vet. Rec. 164:760-761. [DOI] [PubMed] [Google Scholar]
- 10.Bryant, M. L., P. Brown, N. Gurevich, and I. R. McDougall. 1999. Comparison of the clearance of radiolabelled nose drops and nasal spray as mucosally delivered vaccine. Nucl. Med. Commun. 20:171-174. [DOI] [PubMed] [Google Scholar]
- 11.Chambers, T. M., R. E. Holland, L. R. Tudor, H. G. Townsend, A. Cook, J. Bogdan, D. P. Lunn, S. Hussey, P. Whitaker-Dowling, J. S. Youngner, R. W. Sebring, S. J. Penner, and G. L. Stiegler. 2001. A new modified live equine influenza virus vaccine: phenotypic stability, restricted spread and efficacy against heterologous virus challenge. Equine Vet. J. 33:630-636. [DOI] [PubMed] [Google Scholar]
- 12.Chan, W., H. Zhou, G. Kemble, and H. Jin. 2008. The cold adapted and temperature sensitive influenza A/Ann Arbor/6/60 virus, the master donor virus for live attenuated influenza vaccines, has multiple defects in replication at the restrictive temperature. Virology 380:304-311. [DOI] [PubMed] [Google Scholar]
- 13.Chen, G. L., E. W. Lamirande, H. Jin, G. Kemble, and K. Subbarao. 2010. Safety, immunogenicity, and efficacy of a cold-adapted A/Ann Arbor/6/60 (H2N2) vaccine in mice and ferrets. Virology 398:109-114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen, G. L., and K. Subbarao. 2009. Live attenuated vaccines for pandemic influenza. Curr. Top. Microbiol. Immunol. 333:109-132. [DOI] [PubMed] [Google Scholar]
- 15.Chen, Z., C. Santos, A. Aspelund, L. Gillim-Ross, H. Jin, G. Kemble, and K. Subbarao. 2009. Evaluation of live attenuated influenza A virus H6 vaccines in mice and ferrets. J. Virol. 83:65-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cox, R. J., K. A. Brokstad, and P. Ogra. 2004. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand. J. Immunol. 59:1-15. [DOI] [PubMed] [Google Scholar]
- 17.Dawood, F. S., S. Jain, L. Finelli, M. W. Shaw, S. Lindstrom, R. J. Garten, L. V. Gubareva, X. Xu, C. B. Bridges, and T. M. Uyeki. 2009. Emergence of a novel swine-origin influenza A (H1N1) virus in humans. N. Engl. J. Med. 360:2605-2615. [DOI] [PubMed] [Google Scholar]
- 18.Enserink, M., and J. Cohen. 2009. Virus of the year. The novel H1N1 influenza. Science 326:1607. [DOI] [PubMed] [Google Scholar]
- 19.Garten, R. J., C. T. Davis, C. A. Russell, B. Shu, S. Lindstrom, A. Balish, W. M. Sessions, X. Xu, E. Skepner, V. Deyde, M. Okomo-Adhiambo, L. Gubareva, J. Barnes, C. B. Smith, S. L. Emery, M. J. Hillman, P. Rivailler, J. Smagala, M. de Graaf, D. F. Burke, R. A. Fouchier, C. Pappas, C. M. Alpuche-Aranda, H. Lopez-Gatell, H. Olivera, I. Lopez, C. A. Myers, D. Faix, P. J. Blair, C. Yu, K. M. Keene, P. D. Dotson, Jr., D. Boxrud, A. R. Sambol, S. H. Abid, K. St. George, T. Bannerman, A. L. Moore, D. J. Stringer, P. Blevins, G. J. Demmler-Harrison, M. Ginsberg, P. Kriner, S. Waterman, S. Smole, H. F. Guevara, E. A. Belongia, P. A. Clark, S. T. Beatrice, R. Donis, J. Katz, L. Finelli, C. B. Bridges, M. Shaw, D. B. Jernigan, T. M. Uyeki, D. J. Smith, A. I. Klimov, and N. J. Cox. 2009. Antigenic and genetic characteristics of swine-origin 2009 A(H1N1) influenza viruses circulating in humans. Science 325:197-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gibbs, A. J., J. S. Armstrong, and J. C. Downie. 2009. From where did the 2009 ‘swine-origin’ influenza A virus (H1N1) emerge? Virol. J. 6:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gill, J. R., Z. M. Sheng, S. F. Ely, D. G. Guinee, M. B. Beasley, J. Suh, C. Deshpande, D. J. Mollura, D. M. Morens, M. Bray, W. D. Travis, and J. K. Taubenberger. 2010. Pulmonary pathologic findings of fatal 2009 pandemic influenza A/H1N1 viral infections. Arch. Pathol. Lab. Med. 134:235-243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Golde, W. T., P. Gollobin, and L. L. Rodriguez. 2005. A rapid, simple, and humane method for submandibular bleeding of mice using a lancet. Lab. Anim. (NY) 34:39-43. [DOI] [PubMed] [Google Scholar]
- 23.Halbur, P. G., P. S. Paul, M. L. Frey, J. Landgraf, K. Eernisse, X. J. Meng, M. A. Lum, J. J. Andrews, and J. A. Rathje. 1995. Comparison of the pathogenicity of two US porcine reproductive and respiratory syndrome virus isolates with that of the Lelystad virus. Vet. Pathol. 32:648-660. [DOI] [PubMed] [Google Scholar]
- 24.He, X. S., T. H. Holmes, C. Zhang, K. Mahmood, G. W. Kemble, D. B. Lewis, C. L. Dekker, H. B. Greenberg, and A. M. Arvin. 2006. Cellular immune responses in children and adults receiving inactivated or live attenuated influenza vaccines. J. Virol. 80:11756-11766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hickman, D., M. J. Hossain, H. Song, Y. Araya, A. Solorzano, and D. R. Perez. 2008. An avian live attenuated master backbone for potential use in epidemic and pandemic influenza vaccines. J. Gen. Virol. 89:2682-2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoffmann, E., G. Neumann, Y. Kawaoka, G. Hobom, and R. G. Webster. 2000. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl. Acad. Sci. U. S. A. 97:6108-6113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hoffmann, E., J. Stech, Y. Guan, R. G. Webster, and D. R. Perez. 2001. Universal primer set for the full-length amplification of all influenza A viruses. Arch. Virol. 146:2275-2289. [DOI] [PubMed] [Google Scholar]
- 28.Hofshagen, M., B. Gjerset, C. Er, A. Tarpai, E. Brun, B. Dannevig, T. Bruheim, I. G. Fostad, B. Iversen, O. Hungnes, and B. Lium. 2009. Pandemic influenza A(H1N1): human to pig transmission in Norway? Euro Surveill. 14:pii:19406. [DOI] [PubMed] [Google Scholar]
- 29.Horimoto, T., and Y. Kawaoka. 2009. Designing vaccines for pandemic influenza. Curr. Top. Microbiol. Immunol. 333:165-176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Howden, K. J., E. J. Brockhoff, F. D. Caya, L. J. McLeod, M. Lavoie, J. D. Ing, J. M. Bystrom, S. Alexandersen, J. M. Pasick, Y. Berhane, M. E. Morrison, J. M. Keenliside, S. Laurendeau, and E. B. Rohonczy. 2009. An investigation into human pandemic influenza virus (H1N1) 2009 on an Alberta swine farm. Can. Vet. J. 50:1153-1161. [PMC free article] [PubMed] [Google Scholar]
- 31.Itoh, Y., K. Shinya, M. Kiso, T. Watanabe, Y. Sakoda, M. Hatta, Y. Muramoto, D. Tamura, Y. Sakai-Tagawa, T. Noda, S. Sakabe, M. Imai, Y. Hatta, S. Watanabe, C. Li, S. Yamada, K. Fujii, S. Murakami, H. Imai, S. Kakugawa, M. Ito, R. Takano, K. Iwatsuki-Horimoto, M. Shimojima, T. Horimoto, H. Goto, K. Takahashi, A. Makino, H. Ishigaki, M. Nakayama, M. Okamatsu, D. Warshauer, P. A. Shult, R. Saito, H. Suzuki, Y. Furuta, M. Yamashita, K. Mitamura, K. Nakano, M. Nakamura, R. Brockman-Schneider, H. Mitamura, M. Yamazaki, N. Sugaya, M. Suresh, M. Ozawa, G. Neumann, J. Gern, H. Kida, K. Ogasawara, and Y. Kawaoka. 2009. In vitro and in vivo characterization of new swine-origin H1N1 influenza viruses. Nature 460:1021-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jin, H., B. Lu, H. Zhou, C. Ma, J. Zhao, C. F. Yang, G. Kemble, and H. Greenberg. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18-24. [DOI] [PubMed] [Google Scholar]
- 33.Jin, H., S. Manetz, J. Leininger, C. Luke, K. Subbarao, B. Murphy, G. Kemble, and K. L. Coelingh. 2007. Toxicological evaluation of live attenuated, cold-adapted H5N1 vaccines in ferrets. Vaccine 25:8664-8672. [DOI] [PubMed] [Google Scholar]
- 34.Joseph, T., J. McAuliffe, B. Lu, L. Vogel, D. Swayne, H. Jin, G. Kemble, and K. Subbarao. 2008. A live attenuated cold-adapted influenza A H7N3 virus vaccine provides protection against homologous and heterologous H7 viruses in mice and ferrets. Virology 378:123-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Karasin, A. I., S. Carman, and C. W. Olsen. 2006. Identification of human H1N2 and human-swine reassortant H1N2 and H1N1 influenza A viruses among pigs in Ontario, Canada (2003 to 2005). J. Clin. Microbiol. 44:1123-1126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karasin, A. I., C. W. Olsen, and G. A. Anderson. 2000. Genetic characterization of an H1N2 influenza virus isolated from a pig in Indiana. J. Clin. Microbiol. 38:2453-2456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Karasin, A. I., M. M. Schutten, L. A. Cooper, C. B. Smith, K. Subbarao, G. A. Anderson, S. Carman, and C. W. Olsen. 2000. Genetic characterization of H3N2 influenza viruses isolated from pigs in North America, 1977-1999: evidence for wholly human and reassortant virus genotypes. Virus Res. 68:71-85. [DOI] [PubMed] [Google Scholar]
- 38.Klimov, A. I., A. Y. Egorov, M. I. Gushchina, T. E. Medvedeva, W. C. Gamble, L. G. Rudenko, G. I. Alexandrova, and N. J. Cox. 1995. Genetic stability of cold-adapted A/Leningrad/134/47/57 (H2N2) influenza virus: sequence analysis of live cold-adapted reassortant vaccine strains before and after replication in children. J. Gen. Virol. 76(Pt. 6):1521-1525. [DOI] [PubMed] [Google Scholar]
- 39.Lange, E., D. Kalthoff, U. Blohm, J. P. Teifke, A. Breithaupt, C. Maresch, E. Starick, S. Fereidouni, B. Hoffmann, T. C. Mettenleiter, M. Beer, and T. W. Vahlenkamp. 2009. Pathogenesis and transmission of the novel swine-origin influenza virus A/H1N1 after experimental infection of pigs. J. Gen. Virol. 90:2119-2123. [DOI] [PubMed] [Google Scholar]
- 40.Lekcharoensuk, P., K. M. Lager, R. Vemulapalli, M. Woodruff, A. L. Vincent, and J. A. Richt. 2006. Novel swine influenza virus subtype H3N1, United States. Emerg. Infect. Dis. 12:787-794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lunn, D. P., S. Hussey, R. Sebing, K. E. Rushlow, S. V. Radecki, P. Whitaker-Dowling, J. S. Youngner, T. M. Chambers, R. E. Holland, Jr., and D. W. Horohov. 2001. Safety, efficacy, and immunogenicity of a modified-live equine influenza virus vaccine in ponies after induction of exercise-induced immunosuppression. J. Am. Vet. Med. Assoc. 218:900-906. [DOI] [PubMed] [Google Scholar]
- 42.Ma, W., M. Gramer, K. Rossow, and K. J. Yoon. 2006. Isolation and genetic characterization of new reassortant H3N1 swine influenza virus from pigs in the midwestern United States. J. Virol. 80:5092-5096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ma, W., K. M. Lager, A. L. Vincent, B. H. Janke, M. R. Gramer, and J. A. Richt. 2009. The role of swine in the generation of novel influenza viruses. Zoonoses Public Health 56:326-337. [DOI] [PubMed]
- 44.Ma, W., A. L. Vincent, M. R. Gramer, C. B. Brockwell, K. M. Lager, B. H. Janke, P. C. Gauger, D. P. Patnayak, R. J. Webby, and J. A. Richt. 2007. Identification of H2N3 influenza A viruses from swine in the United States. Proc. Natl. Acad. Sci. U. S. A. 104:20949-20954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Manicassamy, B., R. A. Medina, R. Hai, T. Tsibane, S. Stertz, E. Nistal-Villan, P. Palese, C. F. Basler, and A. Garcia-Sastre. 2010. Protection of mice against lethal challenge with 2009 H1N1 influenza A virus by 1918-like and classical swine H1N1 based vaccines. PLoS Pathog. 6:e1000745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Marsh, G. A., J. M. Watson, W. E. White, and G. A. Tannock. 2003. An evaluation of the genetic stability and pathogenicity of the Russian cold-adapted influenza A donor strains A/Leningrad/134/17/57 and A/Leningrad/134/47/57 in ferrets. J. Virol. Methods 107:63-69. [DOI] [PubMed] [Google Scholar]
- 47.Masic, A., L. A. Babiuk, and Y. Zhou. 2009. Reverse genetics-generated elastase-dependent swine influenza viruses are attenuated in pigs. J. Gen. Virol. 90:375-385. [DOI] [PubMed] [Google Scholar]
- 48.Masic, A., J. S. Booth, G. K. Mutwiri, L. A. Babiuk, and Y. Zhou. 2009. Elastase-dependent live attenuated swine influenza A viruses are immunogenic and confer protection against swine influenza A virus infection in pigs. J. Virol. 83:10198-10210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nelli, R. K., S. V. Kuchipudi, G. A. White, B. B. Perez, S. P. Dunham, and K. C. Chang. 2010. Comparative distribution of human and avian type sialic acid influenza receptors in the pig. BMC Vet. Res. 6:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Neumann, G., T. Noda, and Y. Kawaoka. 2009. Emergence and pandemic potential of swine-origin H1N1 influenza virus. Nature 459:931-939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Olsen, C. W. 2002. The emergence of novel swine influenza viruses in North America. Virus Res. 85:199-210. [DOI] [PubMed] [Google Scholar]
- 52.Olsen, C. W., A. I. Karasin, S. Carman, Y. Li, N. Bastien, D. Ojkic, D. Alves, G. Charbonneau, B. M. Henning, D. E. Low, L. Burton, and G. Broukhanski. 2006. Triple reassortant H3N2 influenza A viruses, Canada, 2005. Emerg. Infect. Dis. 12:1132-1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Paillot, R., D. Hannant, J. H. Kydd, and J. M. Daly. 2006. Vaccination against equine influenza: quid novi? Vaccine 24:4047-4061. [DOI] [PubMed] [Google Scholar]
- 54.Perez-Padilla, R., D. de la Rosa-Zamboni, S. Ponce de Leon, M. Hernandez, F. Quinones-Falconi, E. Bautista, A. Ramirez-Venegas, J. Rojas-Serrano, C. E. Ormsby, A. Corrales, A. Higuera, E. Mondragon, and J. A. Cordova-Villalobos. 2009. Pneumonia and respiratory failure from swine-origin influenza A (H1N1) in Mexico. N. Engl. J. Med. 361:680-689. [DOI] [PubMed] [Google Scholar]
- 55.Reed, L. J., and H. Muench. 1938. A simple method for estimating fifty percent endpoints. Am. J. Hyg. 27:493-497. [Google Scholar]
- 56.Rhorer, J., C. S. Ambrose, S. Dickinson, H. Hamilton, N. A. Oleka, F. J. Malinoski, and J. Wittes. 2009. Efficacy of live attenuated influenza vaccine in children: a meta-analysis of nine randomized clinical trials. Vaccine 27:1101-1110. [DOI] [PubMed] [Google Scholar]
- 57.Richt, J. A., K. M. Lager, B. H. Janke, R. D. Woods, R. G. Webster, and R. J. Webby. 2003. Pathogenic and antigenic properties of phylogenetically distinct reassortant H3N2 swine influenza viruses cocirculating in the United States. J. Clin. Microbiol. 41:3198-3205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Richt, J. A., P. Lekcharoensuk, K. M. Lager, A. L. Vincent, C. M. Loiacono, B. H. Janke, W. H. Wu, K. J. Yoon, R. J. Webby, A. Solorzano, and A. Garcia-Sastre. 2006. Vaccination of pigs against swine influenza viruses by using an NS1-truncated modified live-virus vaccine. J. Virol. 80:11009-11018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shinde, V., C. B. Bridges, T. M. Uyeki, B. Shu, A. Balish, X. Xu, S. Lindstrom, L. V. Gubareva, V. Deyde, R. J. Garten, M. Harris, S. Gerber, S. Vagasky, F. Smith, N. Pascoe, K. Martin, D. Dufficy, K. Ritger, C. Conover, P. Quinlisk, A. Klimov, J. S. Bresee, and L. Finelli. 2009. Triple-reassortant swine influenza A (H1) in humans in the United States, 2005-2009. N. Engl. J. Med. 360:2616-2625. [DOI] [PubMed] [Google Scholar]
- 60.Shope, R. E. 1931. The etiology of swine influenza. Science 73:214-215. [DOI] [PubMed] [Google Scholar]
- 61.Smith, G. J., D. Vijaykrishna, J. Bahl, S. J. Lycett, M. Worobey, O. G. Pybus, S. K. Ma, C. L. Cheung, J. Raghwani, S. Bhatt, J. S. Peiris, Y. Guan, and A. Rambaut. 2009. Origins and evolutionary genomics of the 2009 swine-origin H1N1 influenza A epidemic. Nature 459:1122-1125. [DOI] [PubMed] [Google Scholar]
- 62.Solórzano, A., R. J. Webby, K. M. Lager, B. H. Janke, A. Garcia-Sastre, and J. A. Richt. 2005. Mutations in the NS1 protein of swine influenza virus impair anti-interferon activity and confer attenuation in pigs. J. Virol. 79:7535-7543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Song, H., G. R. Nieto, and D. R. Perez. 2007. A new generation of modified live-attenuated avian influenza viruses using a two-strategy combination as potential vaccine candidates. J. Virol. 81:9238-9248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Soto-Abraham, M. V., J. Soriano-Rosas, A. Diaz-Quinonez, J. Silva-Pereyra, P. Vazquez-Hernandez, O. Torres-Lopez, A. Roldan, A. Cruz-Gordillo, P. Alonso-Viveros, and F. Navarro-Reynoso. 2009. Pathological changes associated with the 2009 H1N1 virus. N. Engl. J. Med. 361:2001-2003. [DOI] [PubMed] [Google Scholar]
- 65.Talaat, K. R., R. A. Karron, K. A. Callahan, C. J. Luke, S. C. DiLorenzo, G. L. Chen, E. W. Lamirande, H. Jin, K. L. Coelingh, B. R. Murphy, G. Kemble, and K. Subbarao. 2009. A live attenuated H7N3 influenza virus vaccine is well tolerated and immunogenic in a Phase I trial in healthy adults. Vaccine 27:3744-3753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tang, Y., C. W. Lee, Y. Zhang, D. A. Senne, R. Dearth, B. Byrum, D. R. Perez, D. L. Suarez, and Y. M. Saif. 2005. Isolation and characterization of H3N2 influenza A virus from turkeys. Avian Dis. 49:207-213. [DOI] [PubMed] [Google Scholar]
- 67.Townsend, H. G., S. J. Penner, T. C. Watts, A. Cook, J. Bogdan, D. M. Haines, S. Griffin, T. Chambers, R. E. Holland, P. Whitaker-Dowling, J. S. Youngner, and R. W. Sebring. 2001. Efficacy of a cold-adapted, intranasal, equine influenza vaccine: challenge trials. Equine Vet. J. 33:637-643. [DOI] [PubMed] [Google Scholar]
- 68.Van Reeth, K., S. Van Gucht, and M. Pensaert. 2002. In vivo studies on cytokine involvement during acute viral respiratory disease of swine: troublesome but rewarding. Vet. Immunol. Immunopathol. 87:161-168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Vincent, A. L., J. R. Ciacci-Zanella, A. Lorusso, P. C. Gauger, E. L. Zanella, M. E. Kehrli, Jr., B. H. Janke, and K. M. Lager. 2010. Efficacy of inactivated swine influenza virus vaccines against the 2009 A/H1N1 influenza virus in pigs. Vaccine 28:2782-2787. [DOI] [PubMed] [Google Scholar]
- 70.Vincent, A. L., K. M. Lager, K. S. Faaberg, M. Harland, E. L. Zanella, J. R. Ciacci-Zanella, M. E. Kehrli, Jr., B. H. Janke, and A. Klimov. 2010. Experimental inoculation of pigs with pandemic H1N1 2009 virus and HI cross-reactivity with contemporary swine influenza virus antisera. Influenza Other Respi. Viruses 4:53-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Vincent, A. L., K. M. Lager, B. H. Janke, M. R. Gramer, and J. A. Richt. 2008. Failure of protection and enhanced pneumonia with a US H1N2 swine influenza virus in pigs vaccinated with an inactivated classical swine H1N1 vaccine. Vet. Microbiol. 126:310-323. [DOI] [PubMed] [Google Scholar]
- 72.Vincent, A. L., W. Ma, K. M. Lager, B. H. Janke, and J. A. Richt. 2008. Swine influenza viruses: a North American perspective. Adv. Virus Res. 72:127-154. [DOI] [PubMed] [Google Scholar]
- 73.Vincent, A. L., W. Ma, K. M. Lager, B. H. Janke, R. J. Webby, A. Garcia-Sastre, and J. A. Richt. 2007. Efficacy of intranasal administration of a truncated NS1 modified live influenza virus vaccine in swine. Vaccine 25:7999-8009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Webby, R. J., K. Rossow, G. Erickson, Y. Sims, and R. Webster. 2004. Multiple lineages of antigenically and genetically diverse influenza A virus co-circulate in the United States swine population. Virus Res. 103:67-73. [DOI] [PubMed] [Google Scholar]
- 75.Weingartl, H. M., R. A. Albrecht, K. M. Lager, S. Babiuk, P. Marszal, J. Neufeld, C. Embury-Hyatt, P. Lekcharoensuk, T. M. Tumpey, A. Garcia-Sastre, and J. A. Richt. 2009. Experimental infection of pigs with the human 1918 pandemic influenza virus. J. Virol. 83:4287-4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75a.World Health Organization Department of Communicable Disease Surveillance and Response. WHO manual on animal influenza diagnosis and surveillance. WHO/CDS/CSR/NCS/2002.5, rev. 1. World Health Organization, Geneva, Switzerland. http://www.who.int/vaccine_research/diseases/influenza/WHO_manual_on_animal-diagnosis_and_surveillance_2002_5.pdf.
- 76.Yassine, H. M., M. Q. Al-Natour, C. W. Lee, and Y. M. Saif. 2007. Interspecies and intraspecies transmission of triple reassortant H3N2 influenza A viruses. Virol. J. 4:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ye, J., E. M. Sorrell, Y. Cai, H. Shao, K. Xu, L. Pena, D. Hickman, H. Song, M. Angel, R. A. Medina, B. Manicassamy, A. Garcia-Sastre, and D. R. Perez. 2010. Variations in the hemagglutinin of the 2009 H1N1 pandemic virus: potential for strains with altered virulence phenotype? PLoS Pathog. 6:e1001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhou, N. N., D. A. Senne, J. S. Landgraf, S. L. Swenson, G. Erickson, K. Rossow, L. Liu, K. Yoon, S. Krauss, and R. G. Webster. 1999. Genetic reassortment of avian, swine, and human influenza A viruses in American pigs. J. Virol. 73:8851-8856. [DOI] [PMC free article] [PubMed] [Google Scholar]