Abstract
The Arenaviridae are a diverse and globally distributed collection of viruses that are maintained primarily by rodent reservoirs. Junin virus (JUNV) and Lassa virus (LASV) can both cause significant outbreaks of severe and often fatal human disease throughout their respective areas of endemicity. In an effort to improve upon the existing live attenuated JUNV Candid1 vaccine, we generated a genetically homogenous stock of this virus from cDNA copies of the virus S and L segments by using a reverse genetics system. Further, these cDNAs were used in combination with LASV cDNAs to successfully generate two recombinant Candid1 JUNV/LASV chimeric viruses (via envelope glycoprotein [GPC] exchange). It was found that while the GPC extravirion domains were readily exchangeable, homologous stable signal peptide (SSP) and G2 transmembrane and cytoplasmic tail domains were essential for correct GPC maturation and production of infectious chimeric viruses. The switching of the JUNV and LASV G1/G2 ectodomains within the Candid1 vaccine background did not alter the attenuated phenotype of the vaccine strain in a lethal mouse model. These recombinant chimeric viruses shed light on the fundamental requirements of arenavirus GPC maturation and may serve as a strategy for the development of bivalent JUNV and LASV vaccine candidates.
Divided broadly into New World and Old World serogroups, the arenaviruses (family Arenaviridae, genus Arenavirus) are rodent-borne viruses with a global distribution (12). Among this diverse family of viruses, Junin virus (JUNV) and Lassa virus (LASV) are the two medically most important and cause significant outbreaks of human disease annually. In light of their significant public health impact, these viruses have been designated category A select agents.
The New World JUNV was first isolated in the late 1950s (36, 37) and causes seasonal outbreaks involving as many as 1,000 cases of Argentine hemorrhagic fever (AHF) within the areas of endemicity of the Pampas grasslands in central Argentina (18, 30). JUNV is maintained primarily by animal-to-animal transmission in Calomys musculinus and to a lesser extent in other rodent species (33). The geographic distribution of the Old World LASV is more extensive, with the virus being present throughout western Africa. LASV was first identified in 1969 during a hemorrhagic fever outbreak among missionaries in Nigeria and is today a major health threat to humans, with an estimated 100,000 cases occurring per year (23, 35). Human infections most often result from close contact with or aerosol exposure to infected excreta from the natural reservoir, the rodent Mastomys nataliensis (34). In severe cases, both JUNV and LASV infections can exhibit a profound hemorrhagic syndrome and high case-fatality rates (up to 10 to 30% among hospitalized patients).
Although no vaccine for either pathogen has been approved by the Food and Drug Administration (FDA) for use in the United States, a live attenuated vaccine for JUNV (5, 32) was developed by the U.S. Army Medical Research Institute (USAMRIID) in the early 1980s. The generation and passage history of the original live attenuated vaccine are detailed in Fig. 1A. This vaccine strain has been administered to more than 200,000 persons throughout the area of endemicity of central Argentina (17), and it appears to be safe and efficacious. However, concerns about the documented genetic heterogeneity of the vaccine and lack of knowledge of the genetic basis of attenuation have prevented its broader approval and incorporation into medical countermeasure stockpiles (13). Additionally, the antiviral drug ribavirin has been shown to be effective against LASV but only when used early in the course of infection (31). Despite these potentially effective countermeasures, there is a critical need for improved antiviral tools and increased understanding of the basic molecular mechanisms underlying the virulence of these significant health threats.
FIG. 1.
Development of JUNV Candid1 live attenuated vaccine. (A) Vaccine history. The original vaccine virus was developed by successive passages in guinea pigs (GP) and mouse brains (MB), followed by a clonal selection in FRhl cells (5, 32). (B) Genetic characterization of the recombinant vaccine. The recombinant vaccine virus was developed by reverse genetics as described before (3). Minor changes in the sequences of S and L RNA segments were maintained as selective markers to differentiate the recombinant from the wild-type vaccine viruses.
The arenaviruses are enveloped particles containing bisegmented, single-stranded negative-sense RNA genomes encoding a total of four proteins in an ambisense fashion (9). The L genome segment (∼7.2 kb) contains the viral RNA-dependent RNA polymerase (L, RdRp) and the multifunctional Z protein, which has been demonstrated to be important as a matrix protein and is responsible for virus budding (11, 14, 17, 38, 47). The S genome segment (3.4 kb) encodes the virus nucleoprotein (N) (9) and the glycoprotein precursor (GPC), which is posttranslationally processed (28).
Both Old and New World arenavirus glycoproteins traffic to the cellular plasma membrane, where viral assembly and budding take place in coordination with the Z protein (9). Pathogenic New World arenaviruses, such as JUNV, have recently been shown to utilize the cellular surface protein transferrin receptor 1 (TfR1) for entry into the host cell (40). In contrast, Old World arenaviruses (LASV and lymphocytic choriomeningitis virus [LCMV]) and certain nonpathogenic clade C New World arenaviruses utilize the cellular protein α-dystroglycan to mediate virus attachment and entry into the cell (10, 46). The importance of this difference in cellular receptor usage among pathogenic and nonpathogenic and New World and Old World arenaviruses remains unclear.
The arenavirus GPC polyprotein is proteolytically processed into three mature proteins: the relatively long, myristoylated 58-amino-acid (aa) stable signal peptide (SSP) and two structural glycoproteins, G1 and G2 (9, 16, 50). The SSP has been demonstrated to be essential for proper trafficking of the nascent polyprotein through the endoplasmic reticulum (ER) into the Golgi compartment for further processing via interactions with the C-terminal cytoplasmic tail (CT) of G2 (2, 50). Unlike most other negative-stranded RNA viruses, which use furin-like proprotein convertases (PC), the arenaviruses utilize the SKI-I/S1P PC to cleave the nascent G1/G2 polyprotein in the Golgi compartment into mature G1 and G2 (7, 28, 42). The mature G1 protein contains the major receptor binding motif, mediates cell attachment, and binds the transmembrane-bound G2 protein by stable noncovalent linkages, including noncovalent interactions (9). The G2 protein, which functions as a transmembrane fusion protein, is comprised of three major subdomains: the (surface-exposed) N-terminal portion containing the fusion peptide motif, a transmembrane domain (TD) anchor of approximately 24 aa, and a C-terminal CT of approximately 40 aa that is embedded within the virion particle (9).
We previously developed a highly efficient reverse genetics system for the generation of infectious JUNV entirely from cDNA plasmids (3). In this study, we extended our previous findings toward the development of a reverse genetics-derived JUNV Candid1 vaccine strain, and we have generated recombinant vaccine stocks composed of a single, precisely defined genotype. Using this reverse genetics platform, we have also successfully developed two JUNV-Candid1/LASV chimeric viruses that may serve as potential vaccine candidates as well as useful tools to further characterize arenavirus glycoprotein processing and maturation. Importantly, these chimeric viruses also demonstrate that the attenuated phenotype of JUNV-Candid1 was not changed by expression of the LASV GPC, providing preliminary evidence supporting their potential use as bivalent arenavirus vaccines.
MATERIALS AND METHODS
Cell culture and biosafety.
All activities involving live JUNV and LASV were conducted in biosafety level 3 (BSL-3) and BSL-4 facilities, respectively. All animal infections were carried out in a BSL-4 laboratory following standard CDC BSL-4 safety practices. BSR-T7/5 cells were a generous gift from K. Conzelmann (Max-von-Pettenkofer-Institut, Munich, Germany). BSR-T7/5 and VeroE6 cells were propagated in Dulbecco's modified Eagle's medium (DMEM) supplemented with 5% fetal bovine serum (FBS) and penicillin-streptomycin as recommended by the manufacturer (Invitrogen). BSR-T7/5 cells were maintained under G-418 (1 mg/ml) Geneticin; Invitrogen) selection pressure every other passage.
Plasmid construction.
Full-length cDNA copies from the JUNV Candid1 vaccine strain S and L genome segments were constructed as described previously (3). The final plasmids contained the viral antigenome flanked by the T7 RNA polymerase promoter (5′ end) and followed by hepatitis delta virus ribozyme and T7 polymerase terminator motifs (3′ end). To differentiate the recombinant virus from the wild-type (wt) virus, the following changes were inserted in the final genomic constructs: in the L segment (pJCd1L) nucleotides (nt) 5407 (C to T, Iso to Val) and 6425 (T to C noncoding) and in the S segment (pJCd1S) nt 802 (A to G, noncoding), 1006 (C to T, noncoding), and 3135 (G to A, noncoding) (Fig. 1B).
For this study, functional GPC domains and subdomains were defined as detailed in previous studies (2, 50) and numbered according to the JUNV Candid1 reference sequence (GenBank accession no. HQ126698 and HQ126699). The signal peptide fragment is “domain A” (aa 1 to 58), the G1 and G2 extravirion fragments are “domains B and C” (aa 59 to 421), and the envelope embedded transmembrane domain (aa 422 to 444) together with the intravirion cytoplasmic tail (445 to 485) is “subdomain D” (Fig. 2A). LASV glycoprotein was amplified by reverse transcription-PCR (RT-PCR) using the Josiah strain as input RNA and cloned in the pCAGGS expression plasmid. The generation of all JUNV and LASV chimeric plasmids was accomplished using standard cloning techniques. Full-length parental GPC (ABCD) or the individual structural domains A, B, C, and subdomain D were amplified as cassettes that could be inserted into the recipient cDNA plasmid. Sequences of specific primers for each fragment exchange are available upon request. The resulting plasmids were transformed into highly competent bacterial cells (XL-10 Gold; Stratagene). Transformed bacteria were selectively grown overnight, and plasmids were purified following standard molecular biology protocols and the manufacturer's instructions (Mini or Maxi Prep kit; Qiagen). Using standard cloning strategies, we constructed two plasmids, pJCd1S-ΔGPC:GFP and pJCd1S-ΔGPC:LUC, that contained a complete replacement of the GPC open reading frame by enhanced green fluorescent protein (EGFP) or Gaussia luciferase (GLUC) (NEB) (Fig. 2A). Therefore, by design these constructs required genomic replication and transcription of the carried genes to enable the detection of EGFP or LUC. In combination, the various pCAG-derived plasmids allowed for expression of GPC (either native or chimeric) and complementation of the missing gene in pJCd1S-ΔGPC:GFP or pJCd1S-ΔGPC:LUC. Prior to use in any virus rescue or other manipulation, all plasmids were sequenced to completion, and full-length plasmid sequences were compared with wt virus sequences. Details of all plasmid constructions and any associated technical details can be obtained upon request.
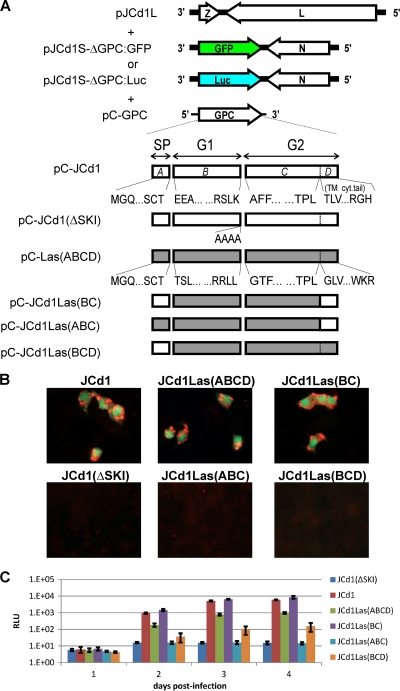
FIG. 2.
(A) Schematics of plasmids used to generate nonspreading virus replicon particles (VRPs). Antigenomic S segments contain a perfect replacement of GPC by either GFP or LUC, and the GPC-expressing plasmids correspond to either authentic JUNV or the JUNV/LASV chimeric variants. (B) VeroE6 cells were infected with GFP-expressing VRPs. Infected cells were fixed at 4 dpi, and JUNV proteins were detected with anti-JUNV rabbit serum and anti-rabbit Alexa fluor 594. Fluorescent photomicrographs were taken using specific wavelength filters (green channel, GFP; red channel, JUNV proteins) and merged digitally. (C) VeroE6 cells were infected with LUC-expressing VRPs. Supernatants of infected cells were collected at 1, 2, 3, and 4 dpi, and the luciferase activity was measured with a Renilla luciferase assay system.
JUNV-LASV GPC chimeric VRPs.
The plasmids pJCd1S-ΔGPC:GFP or pJCd1S-ΔGPC:LUC, pC-GPC (and related chimeric plasmids) and pJCd1L were used to generate infectious virus replicon particles (VRPs) that contained the fluorescent marker EGFP or Gaussia luciferase (NEB) but were incapable of cell-to-cell spread. To accomplish this, BSR-T7/5 cells seeded to approximately 75% confluence in 6- or 12-well plates were transfected with 1 μg of each plasmid using LT-1 (Mirus) transfection reagent at a volume ratio of 1:3 to 1:5 (DNA to reagent) following the manufacturer's recommended protocols. To rescue virus particles, all three plasmids must have been present in a single cell and must each have expressed their encoded proteins. Supernatants from BSR-T7/5 cells were harvested, clarified by low-speed centrifugation to remove cellular debris, and placed onto approximately 70% to 80% subconfluent monolayers of VeroE6 cells seeded in four-well chamber slides (Nunc). Chimeric VRPs were capable of infection and replication but could no longer generate infectious virus particles for subsequent rounds of infection and spread. Successful infection of VeroE6 cells was determined by the fluorescent and chemiluminescent detection assays detailed in the following paragraphs.
VRP luciferase analyses.
At 1, 2, 3, and 4 days posttransfection (dpt), 50-μl aliquots of supernatant were taken from transfected BSR-T7/5 cultures and stored at −20°C for subsequent measurement of GLUC activity (Renilla luciferase assay system; Promega) according to the manufacturer's recommended protocol. Luminescent signals from a total of 1 μl of supernatant from transfected cells were detected with a Synergy 4 multimode microplate reader (Biotek). At 1 to 4 days posttransfection, 0.5-ml aliquots of supernatant of transfected cells were passaged onto VeroE6 cells (DMEM, 5% FBS). After 1.5 h of adsorption, the VRP inocula were removed, the monolayer was washed three times with PBS, and fresh medium was replaced. Similarly, 50 μl of supernatant was taken at days 1, 2, 3, and 4 days postinfection (dpi) and stored at −20°C for subsequent analysis of GLUC activity as described above.
VRP GFP analyses.
The protocol for generation and observation of chimeric VRP-GFP particles was similar to that described above. BSR-T7/5 or VeroE6 cells were fixed (4% formaldehyde, PBS) at 4 days postinfection. Direct UV microscopy to detect GFP was combined with an indirect fluorescent-antibody assay (IFA) to detect JUNV NP using an anti-JUNV rabbit antibody and an anti-rabbit-specific secondary total IgG antibody (Alexa fluor 594; Molecular Probes). Fluorescent photomicrographs were taken using a Zeiss Axioimager microscope and fluorophore-specific-wavelength filters (green channel, GFP red channel, = JUNV NP) and were merged digitally (Photoshop CS2; Adobe).
Western blot analyses.
BSR-T7/5 cells were transfected with pC-LAS-(ABCD), pC-LAS(SKI-Imut), pC-JCd1-Las(BC), pC-JCd1-Las(ABC), or pC-JCd1-Las(BCD). Two days later, transfected cells were harvested by addition of lysis buffer containing Tris-HCl (50 mM, pH 7.4), NaCl (150 mM), EDTA (5 mM), and NP-40 (1%) supplemented with protease inhibitor cocktail (Sigma). Proteins were electrophoretically separated on 4% to 12% NuPAGE (Invitrogen) gels and transferred to a nitrocellulose membrane. The membranes were blocked with buffer containing Tris-buffered saline and 0.1% Tween 20 with 5% nonfat dry milk for 1 h and then probed overnight at 4°C with anti-G2 monoclonal antibodies (MAbs) (43). Membranes were developed using horseradish peroxidase-conjugated secondary antibodies and enhanced chemiluminescence. After detection of glycoprotein, the membrane was stripped and reprobed with actin antibody for detection of total protein.
Rescue of infectious viruses.
Rescue was accomplished following previously described protocols (3). Briefly, BSRT7/5 cells were transfected with 1 μg of each of the two plasmids encoding full-length cDNA copies of the viral S (pJCd1S) and L antigenomic segments (pJCd1L). Alternatively, pJCd1L was transfected in combination with pJCd1S plasmids containing precise substitutions of the domains of the JUNV GPC with that of LASV [pJCd1-Las(ABCD), pJCd1-Las(BC), pJCd1-Las(ABC), and pJCd1-Las(BCD)]. No protein expression support plasmids were required for generation of these fully infectious chimeric viruses. Supernatants from the transfected BSRT7/5 cells were harvested and clarified by low-speed centrifugation. All rescued viruses [rJCd1V(wt), rJCd1-LASV(ABCD), rJCd1-LASV(BC), rJCd1-LASV(ABC), and rJCd1- LASV(BCD)] were propagated after a 1:5 dilution in DMEM by infecting (70% to 80%) confluent monolayers of VeroE6 cells seeded in T 25-cm2 flasks. Clarified virus supernatants were then diluted as described above and passed once more to generate a working stock of virus for subsequent experiments. The passage history of all viruses used in these studies was once in BSR-T7/5 cells and twice in VeroE6 cells. After the second passage, virus supernatants were inactivated (Roche Tripure reagent; Qiagen RNeasy) and transferred to a BSL-2 laboratory, where RNA was extracted. The exact molecular identity of each recombinant virus was confirmed by full-genome sequencing (ABI, Big Dye 3.1) following the manufacturer's recommended protocols.
Virus titration and growth curves.
All viruses were titrated by standard agarose overlay plaque assay techniques using protocols previously described (8). Growth curves were obtained on VeroE6 cells seeded in T 25-cm2 flasks that were infected at a multiplicity of infection (MOI) of 0.02 with either rJCd1V, rJCd1V-LASV(ABCD), rJCd1V-LASV(BC), or wt LASV. After a 1.5-h adsorption, the inoculum was removed, and the monolayers were washed three times with sterile PBS. Following washing, DMEM containing 2% FBS was added, and a sample was taken immediately to represent the 0-h time point (t = 0). Subsequent samples were taken from day 1 to 7 postinfection and stored at −70°C for subsequent titration using a standard 50% tissue culture infective dose (TCID50) protocol. For visualization of infected cells, monolayers were fixed (4% formaldehyde-PBS) at 5 days postinfection and were subsequently labeled with an anti-JUNV NP rabbit antibody and species-specific fluorescent secondary antibodies (Alexafluor 594 nm, anti-rabbit; Molecular Probes).
JUNV and LASV IFA.
To assess the production of JUNV NP or LASV GP by each recombinant plasmid and rescued virus, we employed a standard protocol for indirect fluorescent-antibody assay (IFA) using a polyclonal rabbit anti-JUNV NP antibody (rab-JunNP), a monoclonal mouse anti-JUNV G1 antibody, and a monoclonal mouse anti-LASV-G1 antibody. Briefly, VeroE6 cells were seeded onto four-chamber slides (Nunc) either transfected with 1 μg of pC- LAS-(ABCD), pC-LAS(SKI-Imut), pC-JCd1-Las(BC), pC-JCd1-Las(ABC), or pC-JCd1-Las(BCD) or infected at an MOI of approximately 0.1 with either rJCd1V, rJCd1/LasV(ABCD), or rJCd1/LasV(BC) virus. Transfected cells were incubated at 37°C for 1 day, at which time the supernatants were removed and the monolayers washed in PBS and fixed in 4% formaldehyde in PBS. Mock- and virus-infected cells were incubated at 37°C for 5 days, at which time the supernatants were removed and the monolayers washed in PBS and fixed in 4% formaldehyde in PBS. Cells were permeabilized or not in 0.1% Triton X-100 for 15 min and then thoroughly rinsed with PBS. Primary antibodies (1:250 in 1% bovine serum albumin [BSA]-PBS) were adsorbed at room temperature for 1 h and then washed thoroughly. Species-specific secondary antibodies (1:300) containing fluorescent conjugates (anti-mouse Alexa fluor 488 nm and anti-rabbit Alexa fluor 594 nm; Molecular Probes) were adsorbed for 1 h at room temperature and washed. Coverslips were mounted with DAPI (4′,6′-diamidino-2-phenylindole) nuclear stain (ProLong Gold; Molecular Probes).
Animals and virus infection.
Timed pregnant females (CD-1 strain; Charles River) were housed individually in microisolator pans kept within a HEPA filtration rack inside CDC's BSL-4 laboratory in Atlanta, GA. All animals were observed daily for signs of distress or illness by a licensed veterinarian or veterinary technician. Any animal observed to be in distress (with ruffled fur, paralyzed, or with moribund behavior) were humanely euthanatized under general anesthesia. All animals had access to cotton nestlet bedding materials and to food (rodent lab animal diet; Purina) and water ad libitum. For these experiments, virus infections were carried out with suckling mice that were either 2 or 14 days old. At no time, except during the brief inoculation procedure, were pups separated from mothers. A total of 20 litters of animals (1 litter = 10 animals) were used to assess the virulence and in vivo phenotypes of the wt and recombinant viruses. Initial 50% lethal dose (LD50) experiments were carried out with groups of 10 animals at 2.0 × 103, 1.0 × 103, 1.0 × 102, 1.0 × 101, and 1.0 × 100 PFU in a total volume of 25 μl; each dose was administered intracranially (i.c.) to one group of 2 day old mice and another group of 14 day-old mice. Later, each virus [rJCd1V, rJCd1-LASV(ABCD), rJCD1-LASV(BC), or wtLASV] was inoculated i.c. at a dose of 500 PFU (corresponding to approximately 500 times the LD50) in a total volume of 20 μl into one litter each of 2- and 14 day-old suckling mice. A sham-inoculated control group (n = 10) for each age group of suckling mice was inoculated with 25 μl of sterile physiological saline. Following inoculation, animals were closely observed for 28 days for signs of illness. At the completion of the study, all surviving weanling animals were humanely euthanatized, and serum samples were taken to confirm the presence of specific antibodies. All experimental procedures and husbandry of animals described in this paper were approved by the CDC Institutional Animal Care and Use Committee (IACUC) and was conducted in accordance with the Guide for the Care and Use of Laboratory Animals (34a).
RESULTS
Reverse genetics generation of a recombinant JUNV Candid1 vaccine virus.
To generate a precisely defined genetically homogeneous JUNV Candid1 virus and to provide the foundation for future studies examining the molecular basis of its attenuation, we modified our previously reported JUNV XJ13 reverse genetics system to produce this vaccine strain (3). To construct our cDNA clones, we used RNA extracted from an original ampoule of JUNV strain Candid1 vaccine seed stock, which was kindly provided by Julio Barrera-Oro, USAMRIID. Using this modified reverse genetics system, we have generated a JUNV Candid1 vaccine stock of high purity and precisely defined molecular identity from a known cDNA genomic template. Three silent changes and one conservative amino acid change were maintained as markers in the sequence of the recombinant virus that allowed for differentiation from the wild-type JUN Candid1 virus (Fig. 1B). Wild-type and recombinant viruses exhibited no significant differences in their growth kinetics in cell culture or in their attenuated phenotype in the mouse model (see Fig. 4B and data not shown).
Consistent with our previous report (3), the generation of JUNV Candid1 was found to be highly efficient and reproducible after transfection with only two plasmids encoding full-length cDNA copies of the viral S and L antigenomic segments. Based on a total of at least six independent replicates, the efficiency of virus rescue was determined to be 100% (data not shown). The high efficiency of this system likely reflects the need for only two plasmids and the lack of dependence on additional protein-expressing support plasmids as required by other arenavirus systems (15).
Generation of nonspreading virus replicon particles expressing chimeric arenavirus glycoproteins.
The high efficiency of the JUNV Candid1 reverse genetics procedure prompted us to investigate the possibility of using this platform to potentially produce chimeric viruses utilizing the JUNV Candid1 backbone to express the surface antigens of other arenavirus threat agents. As JUNV and LASV are the greatest public health threats that would benefit most from vaccine developments, we chose to examine the possibility of expressing LASV glycoproteins within the context of the JUNV Candid1 backbone. We anticipated that it may be challenging to combine disparate Old World and New World arenavirus components in this manner. Earlier studies had shown interaction of the JUNV SSP and G2 cytoplasmic tail (48, 49) and interaction of LCMV glycoprotein with the Z protein (11). These findings suggested that there may be limitations with regard to reverse genetics generation of infectious chimeric arenaviruses expressing heterologous glycoprotein domains or entire glycoproteins.
To initiate this project, we designed virus replicon particles (VRPs) which lacked the ability to spread beyond the initial infected cell (see Materials and Methods). These VRPs have the advantage that they can be easily manipulated in a BSL-3 laboratory to assess the basic requirements and optimal experimental conditions for the generation of chimeric viruses. VRPs containing chimeric JUNV/LASV glycoproteins were generated from rational combinations of four structural domains (A to D) of the GPCs from the parent viruses. Domain A corresponds to the N-terminal SSP, domains B and C include the surface-exposed ectodomains of G1/G2, and domain D includes the C-terminal transmembrane domain (TD) and cytoplasmic tail (CT) region of G2. Briefly, parental and chimeric VRPs were generated by transfecting a mix of three plasmids. The first (pJCd1L) encoded the complete JUNV L segment, the second encoded the JUNV S segment with a perfect replacement of the GPC open reading frame (ORF) with either eGFP (pJCd1S-ΔGPC:GFP) or Gaussia luciferase (pJCd1S-ΔGPC:Luc), and the third encoded the parental or chimeric GPCs (pC plasmids [Fig. 2A]). Successful VRP generation was achieved using the native JUNV GPC, the entire LASV GPC [pC-Las(ABCD)], or the chimeric GPC where the exposed extravirion G1/G2 of JUNV were replaced with those of LASV [pC-JCd1-Las(BC)] (Fig. 2B). Despite this success, we were unable to detect infectious VRPs utilizing cDNA constructs containing nonhomologous replacements of either the signal peptide [pC-JCd1-Las(ABC)] or transmembrane domain/cytoplasmic tail (TD-CT) of G2 [pC-JCd1-Las(BCD)] (Fig. 2B).
Similar findings were obtained using the luciferase-expressing VRPs. As a negative control to account for passive transfer of luciferase signal in subsequent VeroE6 passages, a plasmid (pJCd1-ΔSKI) containing a mutation in the SKI-1/S1P subtilase cleavage recognition site that prevents cleavage and generation of infectious VRPs was utilized. Although primary replication activity in BSR-T7/5 cells was equivalent among all chimeras tested (data not shown), substantial differences in luciferase signal upon passage in VeroE6 cells were detected among the various GPC chimeric VRPs compared with the wt JUNV GPC controls (Fig. 2C).
As observed in the previous experiment with EGFP constructs, both the complete GPC exchange [pC-JCd1- Las(ABCD)] and the G1/G2 domain exchange [pC-JCd1-Las(BC)] VRPs generated luciferase signals equivalent to those with the pC-GPC-JCd1(wt) controls, whereas the nonhomologous end constructs [pC-JCd1-Las(ABC)] and [pC-JCd1-Las(BCD)] showed a significant deficit in the observed luciferase signal compared with the wt controls. Interestingly, a low level of luciferase activity was observed when VRPs were made in the presence of pC-JCd1-Las(BCD). Taken together, these results indicate that homologous signal peptide and TD-CT of G2 are essential to the proper maturation of nascent GPC and production of infectious VRP particles.
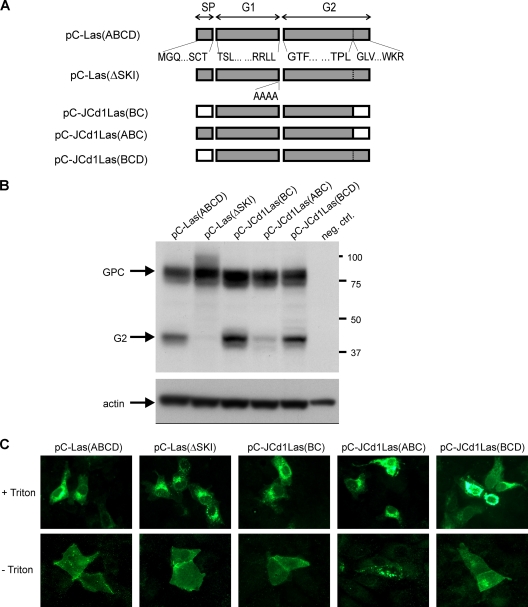
The failure to generate infectious VRPs with mismatched SSP and G2 TM-CT is not limited to lack of GPC S1P/SKI-1 cleavage.
As shown in Fig. 2B and C, there was a substantial deficit in VRP generation when pC-JCd1-LAS(ABC) or pC-JCd1-Las(BCD) plasmid was used to complement either pJCd1S-ΔGPC:GFP or pJCd1S-ΔGPC:LUC. To determine if the lack of VRP generation was due to inefficient GPC cleavage, BSR-T7/5 cells were transfected as previously described with either pC-LAS-(ABCD), pC-LAS(ΔSKI), pC-JCd1-Las(BC), pC-JCd1-Las(ABC), or pC-JCd1-Las(BCD). As expected, Western blot analyses revealed that the wild-type pC-LAS(ABCD) and the chimeric pC-JCd1Las(BC) were cleaved into SSP, GP1, and GP2 efficiently and equivalently (Fig. 3). No cleavage was observed in our negative-control plasmid containing a disrupted SKI-I cleavage site [pC-LAS(ΔSKI)]. Very small amounts of mature G2 were observed with pC-JCd1-LAS(ABC), presumably due to inefficient SlP/SKI-I processing. Strikingly, the chimeric pC-JCd1-Las(BCD), which also exhibited decreased generation of infectious VRPs, was processed at levels equivalent to those for wt LASV. This indicates that while lack of GPC processing can be an explanation for the failure to generate infectious VRPs with the JUN-LAS(ABC) mismatched SSP and G2 TD-CT, some additional step must be blocked in the case of the JUN-LAS(BCD) mismatch.
FIG. 3.
(A) Schematics of plasmids used to express authentic LASV GPC and the JUNV/LASV chimeric variants. (B) BSRT7/5 cells were transfected with the GPC expression plasmids and harvested at 2 dpt. Protein lysates were analyzed by Western blotting using anti-LASV G2 MAb. The membrane was stripped and reprobed with anti-actin MAb as a loading control. Uncleaved GPC, the G2 cleavage product, and actin are indicated with arrows. (C) Monolayers of VeroE6 cells were transfected with the GPC expression plasmids and fixed at 1 dpt. The intracellular (upper row) and surface (lower row) distributions of LASV glycoprotein were examined by IFA using an anti-LASV G2 MAb.
Moreover, we examined the intracellular and surface distributions of these LASV glycoproteins expressed in transfected VeroE6 cells by IFA. As shown in Fig. 3C, the intracellular (upper row) and the extracellular (lower row) distribution patterns of LASV glycoproteins containing homologous SSP and TD-CT were indistinguishable in cells transfected with either pC-LAS-(ABCD), pC-LAS(ΔSKI), or pC-JCd1-Las(BC). Interestingly, the two glycoproteins with mismatched SSP and TD-CT showed two distinct patterns of surface distribution. The poorly cleaved chimeric glycoprotein, pC-LAS(ABC), showed an abnormal and punctuated distribution on the cell surface, while the well-cleaved chimeric glycoprotein, pC- LAS-(BCD), showed a pattern similar to that of the wild-type glycoprotein. These results clearly indicated that efficient glycoprotein processing and normal cell surface distribution are necessary but not sufficient for the generation of infectious VRPs.
Rescue of JUNV and LASV chimeric viruses containing exchanges of the full-length GPC or G1/G2 ectodomains only.
Following the promising results with the envelope protein exchanges of either the full-length GPC or the ectodomains of G1/G2, we generated infectious chimeric viruses using a similar cloning and reverse genetics strategy. After creation of the relevant full-length chimeric GPC cDNA plasmids, chimeric viruses containing precise exchanges of JUNV and LASV GPC ABCD and BC subdomains were rescued with 100% efficiency in several experimental replicates.
We failed to rescue infectious chimeric viruses containing nonhomologous stable signal peptide and TD-CT of G2, rJCd1/LASV(ABC), and rJCd1/LASV(BCD) (Fig. 4A), showing that in agreement with our previous VRP experiments, rescue of fully infectious recombinant virus was found to be dependent on the presence of homologous SSP (domain A) and the C terminus (domain D) of the G2 glycoprotein.
FIG. 4.
(A) Left, schematics of plasmids used to generate fully infectious viruses expressing authentic or chimeric GPC. Recombinant viruses were generated in BSRT7/5 cells and passaged twice onto VeroE6 cells. Right, viral titers were determined by standard plaque assay. (B) One-step growth curves were examined by infecting VeroE6 cells, collecting infectious supernatants at 24-h intervals, and determining viral titers in a TCID50 assay.
All rescued viruses were passaged twice on VeroE6 cells, subjected to full-length complete genome sequencing, and titrated. Final endpoint titers of the chimeric viruses, rJCd1-LASV(ABCD) and rJCd1-LASV(BC), were similar to that of the parental virus, rJCd1V (Fig. 4B). In all cases, the recombinant virus S and L segment sequences were identical to the template plasmids. Growth curves were determined for all rescued recombinant viruses to examine the possible impact of the GPC exchanges on their in vitro growth characteristics. The two recombinant chimeric viruses, rJCd1/LASV(ABCD) and rJCd1/LASV(BC), exhibited growth characteristics similar to those of nonchimeric control viruses, wtJCd1V and rJCd1V. All viruses reached peak titers of approximately 4.0 × 106 TCID50/ml by 4 days postinfection; only negligible differences in the growth rate kinetics were observed during days 1 to 4 postinfection (Fig. 4B.).
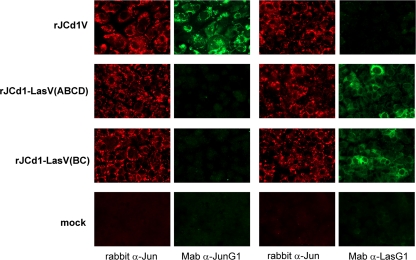
Additional confirmation of the antigenic identity of each recombinant virus was obtained by differential IFA staining of VeroE6 cells infected at an MOI of 1.0 with each recombinant virus. Using JUNV- and LASV-specific anti-NP (red channel) and anti-G1 (green channel) antibodies, we could discriminate each chimeric virus on the basis of the staining pattern (Fig. 5). For example, cells infected with the recombinant chimeric virus rJCd1V/LASV(ABCD) were found to be double positive with the JUNV anti-NP antibody and the LASV anti-G1 antibody but were negative when a JUNV anti-G1 antibody was utilized (Fig. 5, second row).
FIG. 5.
Expression of viral proteins in infected cell monolayers. VeroE6 cells were infected (MOI = 1) with authentic JCd1V (first row) or chimeric JCd1/LASV viruses (second and third rows) or were mock infected (fourth row). Three days later, cells were fixed and stained with specific antibodies. JUNV NP was detected with anti-JUNV rabbit serum (first and third columns), JUNV GPC with anti-JUNV G1(second column), and LASV GPC with anti-LASV G1 (fourth column).
JUNV Candid1 vaccine expressing the LASV GPC retains the Candid1 attenuated phenotype in mice.
To assess the contribution of the JUNV Candid1 and LASV GPC domains to virulence, the classic suckling mouse model was utilized. JUNV strain Candid1 was shown to be highly lethal in 2-day-old suckling mice when inoculated i.c., with all mice succumbing to infection within 9 to 12 days postinfection (calculated LD50 of <1.0 PFU) (Fig. 6A). Age-related resistance to JUNV Candid1 was observed among 14-day-old mice; only a small percentage succumbed to infection after challenge with 500 PFU i.c. (Fig. 6B and C). The calculated JUNV Candid1 LD50 among suckling mice aged 14 days at the time of infection was determined to exceed 1,000 PFU (the maximum dose tested due to technical limitations of the i.c. inoculum volume) (Fig. 6A). Conversely, LASV (at 500 PFU/i.c. dose) was found to be avirulent in 2-day-old suckling mice, but it gained virulence as the mice aged, becoming nearly uniformly lethal in mice infected at 14 days of age (Fig. 6B and C). We utilized these observed differences in age-dependent lethality to determine the relative contributions of the JUNV and LASV GPCs to virulence in this animal model system. Both rescued chimeric viruses, rJCd1-LASV(ABCD) and rJCd1-LASV(BC), were found to retain the attenuated phenotype of the parental JUNV Candid1 strain; i.e., both chimeras were highly virulent in 2-day-old suckling mice, resulting in uniform 100% lethality. The viral genomes from several mice were sequenced to verify that they retained the genome sequence of the input virus (data not shown). The rJCd1-LASV(ABCD) and rJCd1-LASV(BC) viruses were completely avirulent in older, 14-day-old suckling mice (Fig. 6B and C), even at a dose of 2,000 PFU (data not shown). The minor differences in time to death observed between mice infected with rJCd1-LasV and rJCd1V were not statistically significant, as the time to death has been seen to vary from 7 to 20 dpi in different repeat experiments. These results, taken together, strongly suggest that inclusion of the LASV GPC does not enhance the virulence of the JUNV Candid1 vaccine and may provide a strategy for the development of JUNV/LASV arenavirus vaccine candidates.
FIG. 6.
Neurovirulence test in the mouse model. (A) The lethal dose for recombinant JUNVs was assayed by i.c. injection of 1 to 1,000 PFU/mouse in both 2- and 4-day-old mice. Infected mice were examined for any sign of disease, and mortality was recorded for 28 days postinfection. (B and C) To determine the survival curves, groups of 2-day-old mice (B) and 14-day-old mice (C) were infected i.c. with 500 PFU of authentic LASV, recombinant JUNV, or JUNV/LASV chimeric viruses. Infected mice were examined for any sign of disease, and mortality was recorded for 28 days postinfection.
DISCUSSION
The substantial numbers of JUNV and LASV cases reported each year among humans, along with the high case-fatality rate associated with these pathogens, render them a substantial public health threat in many areas of the world. Of additional, significant concern is the potential intentional release of these agents in acts of bioterrorism. Safe and effective vaccines to combat these health and security threats are critically needed.
In this report, we describe the successful use of reverse genetics to generate a genetically homogeneous recombinant JUNV Candid1 vaccine and attenuated JUNV/LASV chimeric viruses that may serve as potential bivalent vaccine candidates for these two diverse arenaviruses. An important advantage of this strategy is that it relies on the preexisting JUNV Candid1 vaccine strain, which was proved to be safe and effective (4, 5, 32). Since its approval for human use in Argentina in the 1980s, more than 200,000 persons throughout central Argentina have been vaccinated to date (18). However, despite this record, concerns remain regarding the well-documented genetic heterogeneity of the current Candid1 vaccine, which likely resulted from the vaccine's extensive in vivo passage history (13) (Fig. 1). The ability to efficiently generate pure stocks of recombinant JUNV Candid1 virus directly from cDNA clones provides the foundation for improvements in this vaccine and studies to precisely determine the contributions made by various mutations to the attenuated phenotype of the vaccine. In addition, this platform allowed us to investigate glycoprotein interactions involved in arenavirus maturation, propagation, and virulence by generation of JUNV Candid1 and LASV chimeric VRPs and infectious viruses.
The mechanisms and regulation of GPC maturation of arenaviruses have been the focus of much investigation over the past 20 years (9, 26). With the ultimate goal of developing vaccine candidates for JUNV and LASV in mind, we employed a general strategy of envelope exchange using precisely defined chimeric GPC domain constructs between these two significant New World and Old World arenaviruses. We generated a full complement of chimeric JUNV and LASV GPC cDNA plasmids containing various combinations of the SSP, G1/G2 ectodomains, and G2 TM-CT domains either together or individually. Using these constructs, we successfully demonstrated that efficient virus replication and propagation require the presence of homologous virus species-specific SSP and the G2 C terminus.
Envelope protein exchange among arenaviruses and other negative-sense RNA viruses to generate multivalent recombinant live attenuated arenavirus vaccines has been previously demonstrated (6, 21, 25). In addition, several studies have shown that the SSP of the Arenaviridae is required for GPC maturation and eventual production of infectious virions (16, 17, 25, 50). Furthermore, studies involving JUNV have demonstrated that interactions between the SSP and G2-cytoplasmic domains are critical to mask endogenous dibasic ER retention signals located within G2 (2), thus allowing for the further processing and eventual incorporation of mature SSP, G1, and G2 into nascent virion particles.
Schlie et al. (44) have recently described the relationship of LASV CT to GPC maturation. That report suggested that LASV CT was required for correct GPC oligomerization, which seemed to be a prerequisite for SKI-1/S1P processing. The correct interaction between SSP and CT apparently triggers a change in conformation of the GPC into a trimer that is selectively cleaved; thus, processing of SKI-1 appears to serve a quality control step where only trimers are incorporated in virions. Without proper oligomerization and interactions of the SSP and G2, an uncleaved form of GPC can be found on the cellular plasma membrane; however, this immature glycoprotein precursor is unable to form infectious virus particles (2, 27, 44).
During the initial stages of our research, we anticipated some challenges for the successful generation of a recombinant JUNV Candid1 expressing LASV GPC, based on two relevant reports: first, the well-defined interaction of JUNV SSP with the G2 cytoplasmic tail (48, 49), and second, the suggested interaction of LCMV GPC with the Z protein (11). In light of this information, we set out to define functionally relevant GPC domains that could be exchanged and still generate a virus that replicates efficiently while maintaining the avirulent phenotype of the parental Candid1 in animal models (and presumably in humans). Surprisingly, our studies demonstrated that recombinant VRPs containing the full-length LASV GPC [JCd1-Las(ABCD)] and nonhomologous G1/G2 ectodomains [JCd1-Las(BC)] can indeed be generated, and they were found to replicate at levels similar to those for wt JCd1 GPC VRPs in cell culture. Nonhomologous SSP and G2-cytoplamic domain exchanges led to significantly depressed production of infectious VRPs that was undetectable when measured with GFP fluorescence and only slightly above background when measured by luciferase activity.
Even more surprisingly, reverse genetics generated infectious chimeric viruses containing exchanges of the full-length LASV GPC [rJCd1V-LASV(ABCD)] or the extravirion ectodomains of G1/G2 [rJCd1V-LASV(BC)] were found to have near-equivalent cell culture growth characteristics compared with authentic JUNV. These results clearly demonstrated that the sequence mismatch of (i) the LASV G1/G2 glycoproteins with JUNV N and Z proteins or (ii) the JUNV SSP and G2 cytoplasmic domain with the G1/G2 ectodomains, did not result in significant defects in virus replication or production of infectious particles. Earlier studies with LCMV and LASV have provided evidence of interaction of the Z protein with the GP and suggested that this interaction is of importance for arenavirus maturation (11). Our results would be consistent with the sequence divergence between Old World (LASV) and New World (JUNV) arenavirus glycoproteins and Z proteins being insufficient to prevent this interaction. In addition, the earlier study (11) had demonstrated direct interaction of the SSP with Z. Interestingly, we found no difference in chimeric virus replication whether the Z protein was matched with the SSP protein [rJCd1-LASV(BC)] or not matched [rJCd1-LASV(ABCD)], suggesting a lack of a strict sequence requirement for such interactions to occur.
The main constraint we found for the generation of chimeric JUNV Candid1 infectious viruses where the JUNV glycoprotein has been replaced with the LASV glycoprotein was the requirement to match the virus species origin of the SSP and G2 cytoplasmic tail domains. Interestingly, our Western blot analysis and VRP experiments suggested different mechanisms to explain why these chimeras did not sustain production of infectious viruses. The defect where the mismatch was the G2 cytoplasmic tail [pC-JCd1-Las(ABC)] appeared to be more severe, in that in addition to lack of generation of infectious virus, the GPC was not processed efficiently by the S1P/SKI-I protease, and it presented an abnormal distribution at the cell surface (Fig. 3C). In contrast, the Las(ABC) chimeric protein processing was almost completely abrogated, while the Las(BCD) protein did not show any defect in cleavage or in cell surface expression.
In a very recent report, Schlie et al. (44) have shown that the exchange of the LASV GPC CT with that of the closely related LCMV also blocked SKI-1/S1P cleavage. The exact reason for the block remains unclear, but current data suggest that the chimeric GPC was not in the correct ternary or quaternary conformation to allow SKI-1/S1P cleavage. Strikingly, introduction of matching JUNV SSP and JUNV TM/CT into the LASV GPC promoted its cleavage and the production of infectious virus, suggesting that interaction between the matched pair of SSP and TM/CT is solely responsible for the rescue of the defect in their original unproductive GPC chimeras (the equivalent of ABC and BCD proteins discussed here).
In contrast to the defect where the mismatch was the G2 cytoplasmic tail [pC-JCd1-Las(ABC)], the defect with the mismatch in the SSP [JCd1-Las(BCD)] produced a GPC that was efficiently cleaved by S1P/SKI-I and presented a normal cell surface distribution but, surprisingly, failed to support robust generation of VRPs or infectious chimeric virus. These results further suggest that chimeric GPC folds and traffics to the cellular compartment where S1P/SKI-1 cleavage occurs but is then defective in a subsequent step prior to maturation of infectious virus particles. Further studies on the relationship of GPC maturation and budding of virus particles will be necessary to elucidate the precise basis of this additional defect. Taken together, these results indicate that homologous SSP and G2-cytoplasmic tail domains, regardless of their origin (JUNV or LASV), are essential for the efficient generation of an infectious virus.
Using a lethal model of arenavirus infection in suckling/weanling mice, we established a clear age-dependent phenotype between JUNV and LASV. In this model, suckling mice aged 2 days old at the time of infection were highly susceptible to lethal infection by JUNV. However, LASV was found to be phenotypically avirulent in these mice, even at dosages exceeding 1,000 times the JUNV LD50 (Fig. 6A). This virulence phenotype was reversed when older mice were used. In 14-day-old suckling mice, JUNV Candid1 was found to be completely attenuated, whereas LASV was shown to have near 100% lethality (Fig. 6A). Strikingly, a Candid1-like pattern of age-dependent lethality was also observed with both envelope exchange JUNV-LASV chimeras, i.e., JCd1-LASV(ABCD) and rJCd1-LASV(BC) (Fig. 6). Even though these chimeras did not cause lethality in 14-day-old suckling mice, all ani- mals infected with either rJCd1-LASV(ABCD) or rJCd1- LASV(BC) developed robust anti-NP antibody responses by 28 days postinfection, equivalent to those observed in rJUNV-Candid1 survivor animals.
The underlying pathophysiological mechanisms of this age-related phenomenon remain unknown. However, this finding may be related to the well-described observation of LASV dependence on host immune dysregulation for lethality in humans and animal models, rather than direct virus-induced cell toxicity (20, 22, 29, 39, 41, 45). Neonatal mice are known to preferentially develop type II immune responses for several days postbirth without the maturation and robust action of type I responses (reviewed in references 1, 19, and 24) that are thought to be responsible for the observed immunopathology of fatal Lassa fever. Further study of these JUNV-LASV chimeras may shed light on the complex interplay of the neonatal murine immune system and the molecular mechanisms by which arenaviruses establish persistent infection in rodent hosts. Regardless of the physiological mechanism, it is clear that the LASV GPC alone is not sufficient to alter the attenuated phenotype of the JUNV-Candid1 vaccine strain in 14-day-old weanling mice.
Given how divergent JUNV and LASV are, it was surprising that the infectious JUNV-Candid1-LASV chimeric viruses generated here retained infectivity in tissue culture and in vivo, comparable to that of authentic JUNV-Candid1 virus. This is particularly so in light of the well-demonstrated major impact that minor sequence changes can have on viral virulence. For example, the virulent JUNV-XJ13 and the vaccine JUNV-Candid1 strains differ in only nine and six amino acids (nine in the L polymerase, five in the glycoproteins, and one in NP), but clearly exhibit very different virulence phenotypes in a variety of animal models (e.g., mice, guinea pigs, and rhesus macaques) (5, 18, 30, 32).
The attenuated phenotype of these JUNV-LASV chimeras may allow for their use in the rational development of bivalent JUNV and LASV live attenuated vaccine platforms that employ an envelope protein exchange strategy. While i.c. inoculation of mice has proved to be a convenient and useful model for study of arenaviruses, the precise relevance of such studies to viral pathogenesis and virus attenuation in humans is questionable. Further characterization of these constructs in a vaccination-challenge animal model (such as guinea pigs or nonhuman primates) will be essential and required before more definitive statements on the immunogenicity and efficacy of these JUNV-LASV chimeras as vaccine candidates can be made. The results presented here represent a first step toward the production of rationally designed, safe, and effective live attenuated bivalent arenavirus vaccines that can be used to combat these significant health threats.
Acknowledgments
We thank K. Conzelmann for providing BSRT7/5 cells and J. Barrera-Oro for providing the original stock of Junin virus Candid1.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
Footnotes
Published ahead of print on 27 October 2010.
REFERENCES
- 1.Adkins, B. 2000. Development of neonatal Th1/Th2 function. Int. Rev. Immunol. 19:157-171. [DOI] [PubMed] [Google Scholar]
- 2.Agnihothram, S. S., J. York, and J. H. Nunberg. 2006. Role of the stable signal peptide and cytoplasmic domain of G2 in regulating intracellular transport of the Junin virus envelope glycoprotein complex. J. Virol. 80:5189-5198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albarino, C. G., E. Bergeron, B. R. Erickson, M. L. Khristova, P. E. Rollin, and S. T. Nichol. 2009. Efficient reverse genetics generation of infectious Junin viruses differing in glycoprotein processing. J. Virol. 83:5606-5614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ambrosio, A. M., L. M. Riera, C. Saavedra Mdel, and M. S. Sabattini. 2006. Immune response to vaccination against Argentine hemorrhagic fever in an area where different arenaviruses coexist. Viral Immunol. 19:196-201. [DOI] [PubMed] [Google Scholar]
- 5.Barrera Oro, J. G., and K. T. McKee, Jr. 1991. Toward a vaccine against Argentine hemorrhagic fever. Bull. Pan Am. Health Organ. 25:118-126. [PubMed] [Google Scholar]
- 6.Bergthaler, A., N. U. Gerber, D. Merkler, E. Horvath, J. C. de la Torre, and D. D. Pinschewer. 2006. Envelope exchange for the generation of live-attenuated arenavirus vaccines. PLoS Pathog. 2:e51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beyer, W. R., D. Popplau, W. Garten, D. von Laer, and O. Lenz. 2003. Endoproteolytic processing of the lymphocytic choriomeningitis virus glycoprotein by the subtilase SKI-1/S1P. J. Virol. 77:2866-2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bird, B. H., C. G. Albarino, A. L. Hartman, B. R. Erickson, T. G. Ksiazek, and S. T. Nichol. 2008. Rift valley fever virus lacking the NSs and NSm genes is highly attenuated, confers protective immunity from virulent virus challenge, and allows for differential identification of infected and vaccinated animals. J. Virol. 82:2681-2691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Buchmeier, M. J., C. J. Peters, and J. C. de la Torre. 2007. Arenaviridae: the viruses and their replication, p. 1792-1827. In D. M. Knipe and P. M. Howley (ed.), Fields virology, 5th ed., vol. 2. Lippincott, Williams and Wilkins, Philadelphia, PA. [Google Scholar]
- 10.Cao, W., M. D. Henry, P. Borrow, H. Yamada, J. H. Elder, E. V. Ravkov, S. T. Nichol, R. W. Compans, K. P. Campbell, and M. B. Oldstone. 1998. Identification of alpha-dystroglycan as a receptor for lymphocytic choriomeningitis virus and Lassa fever virus. Science 282:2079-2081. [DOI] [PubMed] [Google Scholar]
- 11.Capul, A. A., M. Perez, E. Burke, S. Kunz, M. J. Buchmeier, and J. C. de la Torre. 2007. Arenavirus Z-glycoprotein association requires Z myristoylation but not functional RING or late domains. J. Virol. 81:9451-9460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Casals, J. 1975. Arenaviruses. Yale J. Biol. Med. 48:115-140. [PMC free article] [PubMed] [Google Scholar]
- 13.Contigiani, M., S. Medeot, and G. Diaz. 1993. Heterogeneity and stability characteristics of Candid 1 attenuated strain of Junin virus. Acta Virol. 37:41-46. [PubMed] [Google Scholar]
- 14.Cornu, T. I., and J. C. de la Torre. 2002. Characterization of the arenavirus RING finger Z protein regions required for Z-mediated inhibition of viral RNA synthesis. J. Virol. 76:6678-6688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de la Torre, J. C. 2008. Reverse genetics approaches to combat pathogenic arenaviruses. Antiviral Res. 80:239-250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eichler, R., O. Lenz, T. Strecker, and W. Garten. 2003. Signal peptide of Lassa virus glycoprotein GP-C exhibits an unusual length. FEBS Lett. 538:203-206. [DOI] [PubMed] [Google Scholar]
- 17.Eichler, R., T. Strecker, L. Kolesnikova, J. ter Meulen, W. Weissenhorn, S. Becker, H. D. Klenk, W. Garten, and O. Lenz. 2004. Characterization of the Lassa virus matrix protein Z: electron microscopic study of virus-like particles and interaction with the nucleoprotein (NP). Virus Res. 100:249-255. [DOI] [PubMed] [Google Scholar]
- 18.Enria, D. A., and J. G. Barrera Oro. 2002. Junin virus vaccines. Curr. Top. Microbiol. Immunol. 263:239-261. [DOI] [PubMed] [Google Scholar]
- 19.Fadel, S., and M. Sarzotti. 2000. Cellular immune responses in neonates. Int. Rev. Immunol. 19:173-193. [DOI] [PubMed] [Google Scholar]
- 20.Fisher-Hoch, S., J. B. McCormick, D. Sasso, and R. B. Craven. 1988. Hematologic dysfunction in Lassa fever. J. Med. Virol. 26:127-135. [DOI] [PubMed] [Google Scholar]
- 21.Fisher-Hoch, S. P., L. Hutwagner, B. Brown, and J. B. McCormick. 2000. Effective vaccine for Lassa fever. J. Virol. 74:6777-6783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fisher-Hoch, S. P., S. W. Mitchell, D. R. Sasso, J. V. Lange, R. Ramsey, and J. B. McCormick. 1987. Physiological and immunologic disturbances associated with shock in a primate model of Lassa fever. J. Infect. Dis. 155:465-474. [DOI] [PubMed] [Google Scholar]
- 23.Frame, J. D., J. M. Baldwin, Jr., D. J. Gocke, and J. M. Troup. 1970. Lassa fever, a new virus disease of man from West Africa. I. Clinical description and pathological findings. Am. J. Trop. Med. Hyg. 19:670-676. [DOI] [PubMed] [Google Scholar]
- 24.Garcia, A. M., S. A. Fadel, S. Cao, and M. Sarzotti. 2000. T cell immunity in neonates. Immunol. Res. 22:177-190. [DOI] [PubMed] [Google Scholar]
- 25.Geisbert, T. W., S. Jones, E. A. Fritz, A. C. Shurtleff, J. B. Geisbert, R. Liebscher, A. Grolla, U. Stroher, L. Fernando, K. M. Daddario, M. C. Guttieri, B. R. Mothe, T. Larsen, L. E. Hensley, P. B. Jahrling, and H. Feldmann. 2005. Development of a new vaccine for the prevention of Lassa fever. PLoS Med. 2:e183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gunther, S., and O. Lenz. 2004. Lassa virus. Crit. Rev. Clin. Lab. Sci. 41:339-390. [DOI] [PubMed] [Google Scholar]
- 27.Kunz, S., K. H. Edelmann, J. C. de la Torre, R. Gorney, and M. B. Oldstone. 2003. Mechanisms for lymphocytic choriomeningitis virus glycoprotein cleavage, transport, and incorporation into virions. Virology 314:168-178. [DOI] [PubMed] [Google Scholar]
- 28.Lenz, O., J. ter Meulen, H. D. Klenk, N. G. Seidah, and W. Garten. 2001. The Lassa virus glycoprotein precursor GP-C is proteolytically processed by subtilase SKI-1/S1P. Proc. Natl. Acad. Sci. U. S. A. 98:12701-12705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mahanty, S., K. Hutchinson, S. Agarwal, M. McRae, P. E. Rollin, and B. Pulendran. 2003. Impairment of dendritic cells and adaptive immunity by Ebola and Lassa viruses. J. Immunol. 170:2797-2801. [DOI] [PubMed] [Google Scholar]
- 30.Maiztegui, J. I., K. T. McKee, Jr., J. G. Barrera Oro, L. H. Harrison, P. H. Gibbs, M. R. Feuillade, D. A. Enria, A. M. Briggiler, S. C. Levis, A. M. Ambrosio, N. A. Halsey, and C. J. Peters. 1998. Protective efficacy of a live attenuated vaccine against Argentine hemorrhagic fever. AHF Study Group. J. Infect. Dis. 177:277-283. [DOI] [PubMed] [Google Scholar]
- 31.McCormick, J. B., I. J. King, P. A. Webb, C. L. Scribner, R. B. Craven, K. M. Johnson, L. H. Elliott, and R. Belmont-Williams. 1986. Lassa fever. Effective therapy with ribavirin. N. Engl. J. Med. 314:20-26. [DOI] [PubMed] [Google Scholar]
- 32.McKee, K. T., Jr., J. G. Oro, A. I. Kuehne, J. A. Spisso, and B. G. Mahlandt. 1992. Candid no. 1 Argentine hemorrhagic fever vaccine protects against lethal Junin virus challenge in rhesus macaques. Intervirology 34:154-163. [DOI] [PubMed] [Google Scholar]
- 33.Mills, J. N., B. A. Ellis, J. E. Childs, K. T. McKee, Jr., J. I. Maiztegui, C. J. Peters, T. G. Ksiazek, and P. B. Jahrling. 1994. Prevalence of infection with Junin virus in rodent populations in the epidemic area of Argentine hemorrhagic fever. Am. J. Trop. Med. Hyg. 51:554-562. [PubMed] [Google Scholar]
- 34.Monath, T. P., V. F. Newhouse, G. E. Kemp, H. W. Setzer, and A. Cacciapuoti. 1974. Lassa virus isolation from Mastomys natalensis rodents during an epidemic in Sierra Leone. Science 185:263-265. [DOI] [PubMed] [Google Scholar]
- 34a.National Research Council. 1996. Guide for the care and use of laboratory animals. National Academy Press, Washington, DC.
- 35.Omilabu, S. A., S. O. Badaru, P. Okokhere, D. Asogun, C. Drosten, P. Emmerich, B. Becker-Ziaja, H. Schmitz, and S. Gunther. 2005. Lassa fever, Nigeria, 2003 and 2004. Emerg. Infect. Dis. 11:1642-1644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Parodi, A. S., D. J. Greenway, H. R. Rugiero, M. Frigerio, J. M. De La Barrera, N. Mettler, F. Garzon, M. Boxaca, L. Guerrero, and N. Nota. 1958. Concerning the epidemic outbreak in Junin. Dia Med. 30:2300-2301. [PubMed] [Google Scholar]
- 37.Parodi, A. S., H. R. Rugiero, D. J. Greenway, N. Mettler, and M. Boxaca. 1961. Isolation of the Junin virus from rodents of non-epidemic areas. Prensa Med. Argentina 48:2321-2322. [PubMed] [Google Scholar]
- 38.Perez, M., R. C. Craven, and J. C. de la Torre. 2003. The small RING finger protein Z drives arenavirus budding: implications for antiviral strategies. Proc. Natl. Acad. Sci. U. S. A. 100:12978-12983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Peters, C. J., C. T. Liu, G. W. Anderson, Jr., J. C. Morrill, and P. B. Jahrling. 1989. Pathogenesis of viral hemorrhagic fevers: Rift Valley fever and Lassa fever contrasted. Rev. Infect. Dis. 11(Suppl. 4):S743-S749. [DOI] [PubMed] [Google Scholar]
- 40.Radoshitzky, S. R., J. Abraham, C. F. Spiropoulou, J. H. Kuhn, D. Nguyen, W. Li, J. Nagel, P. J. Schmidt, J. H. Nunberg, N. C. Andrews, M. Farzan, and H. Choe. 2007. Transferrin receptor 1 is a cellular receptor for New World haemorrhagic fever arenaviruses. Nature 446:92-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roberts, P. J., D. Cummins, A. L. Bainton, K. J. Walshe, S. P. Fisher-Hoch, J. B. McCormick, J. G. Gribben, S. J. Machin, and D. C. Linch. 1989. Plasma from patients with severe Lassa fever profoundly modulates f-met-leu-phe induced superoxide generation in neutrophils. Br. J. Haematol. 73:152-157. [DOI] [PubMed] [Google Scholar]
- 42.Rojek, J. M., A. M. Lee, N. Nguyen, C. F. Spiropoulou, and S. Kunz. 2008. Site 1 protease is required for proteolytic processing of the glycoproteins of the South American hemorrhagic fever viruses Junin, Machupo, and Guanarito. J. Virol. 82:6045-6051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ruo, S. L., S. W. Mitchell, M. P. Kiley, L. F. Roumillat, S. P. Fisher-Hoch, and J. B. McCormick. 1991. Antigenic relatedness between arenaviruses defined at the epitope level by monoclonal antibodies. J. Gen. Virol. 72:549-555. [DOI] [PubMed] [Google Scholar]
- 44.Schlie, K., T. Strecker, and W. Garten. 2010. Maturation cleavage within the ectodomain of Lassa virus glycoprotein relies on stabilization by the cytoplasmic tail. FEBS Lett. 584:4379-4382. [DOI] [PubMed] [Google Scholar]
- 45.Schmitz, H., B. Kohler, T. Laue, C. Drosten, P. J. Veldkamp, S. Gunther, P. Emmerich, H. P. Geisen, K. Fleischer, M. F. Beersma, and A. Hoerauf. 2002. Monitoring of clinical and laboratory data in two cases of imported Lassa fever. Microbes Infect. 4:43-50. [DOI] [PubMed] [Google Scholar]
- 46.Spiropoulou, C. F., S. Kunz, P. E. Rollin, K. P. Campbell, and M. B. Oldstone. 2002. New World arenavirus clade C, but not clade A and B viruses, utilizes alpha-dystroglycan as its major receptor. J. Virol. 76:5140-5146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Strecker, T., R. Eichler, J. Meulen, W. Weissenhorn, H. Dieter Klenk, W. Garten, and O. Lenz. 2003. Lassa virus Z protein is a matrix protein and sufficient for the release of virus-like particles. J. Virol. 77:10700-10705. (Erratum, 77:12927.) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.York, J., D. Dai, S. M. Amberg, and J. H. Nunberg. 2008. pH-induced activation of arenavirus membrane fusion is antagonized by small-molecule inhibitors. J. Virol. 82:10932-10939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.York, J., and J. H. Nunberg. 2007. A novel zinc-binding domain is essential for formation of the functional Junin virus envelope glycoprotein complex. J. Virol. 81:13385-13391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.York, J., V. Romanowski, M. Lu, and J. H. Nunberg. 2004. The signal peptide of the Junin arenavirus envelope glycoprotein is myristoylated and forms an essential subunit of the mature G1-G2 complex. J. Virol. 78:10783-10792. [DOI] [PMC free article] [PubMed] [Google Scholar]