Abstract
The delivery of health care is a capital intensive industry and thus hospital investment strategy continues to be an important area of interest for both health policy and research. Much attention has been given to hospitals’ capital investment policies with relatively little attention to investments in financial assets, which serve an important role in NFP hospitals. This study describes and analyzes trends in aggregate asset structure between NFP and IO hospitals during the post-capital based PPS implementation period, providing the first documentation of long-term trends in hospital investment. We find hospitals’ aggregate asset structure differs significantly based on ownership, size, and profitability. For both NFP and IO hospitals, financial securities have remained consistent over time, while fixed asset representation has declined in IO hospitals.
Introduction
The delivery of health care is a capital intensive industry and thus hospital investment strategy continues to be an important area of interest for both health policy and research. Capital investment is important for hospitals to keep pace with new medical technologies and maintain facilities for patient care needs. Accordingly, much attention has been given to hospitals’ capital investment practices. More recently, investment in financial assets (e.g. stocks and bonds) has emerged as a focus bringing attention to the role of financial assets in hospitals’ aggregate asset structure.
The role of financial assets varies by hospital ownership. While for-profit, or investor-owned (IO) hospitals, are motivated to maximize profits, not-for-profit (NFP) hospitals are motivated to maximize cash holdings (Robinson 2002; Song, et al. 2008). NFP hospitals’ motivation to maximize cash is largely driven by their inability to access external capital outside of the tax-exempt debt market. Cash and investments in financial assets allow hospitals to achieve favorable bond ratings, resulting in a lower cost of debt. This, in turn, supports investments in fixed assets (e.g., buildings and equipment) (McCue, 2001; McCue, Thompson, & Dodd-McCue, 2000/2001; Wheeler, Smith, Rivenson, & Reiter, 2000). Investments in financial assets also provide precautionary savings for NFP hospitals, and serve as a source of untaxed interest income.1
In contrast, IO hospitals utilize cash to maximize profit and shareholder wealth. Without access to the tax-exempt debt market, IO hospitals are more likely to use cash over debt to finance capital investments. More importantly, in the absence of profitable investment opportunities, IO hospitals return excess cash to shareholders in the form of dividends or share repurchases.
To date, there is neither consensus on the appropriate level of financial assets in NFP hospitals, nor evidence of the effect on hospitals of eliminating investment earnings as a source of financing (Congressional Budget Office, 2006). However, in tough economic times such as those of the present, access to debt financing is critical to prevent constraints on capital investment that could ultimately threaten quality (Reiter, Wheeler and Smith, 2008). While we do not seek to answer the question of the right balance of fixed, financial and other assets in NFP and IO hospitals in this study, we hope to lay the foundation for future studies by providing the first descriptive data on long-term investment trends in both NFP and investor-owned hospitals during the post-capital based prospective payment system (PPS) implementation period.
New Contribution
This study contributes to the existing hospital investment literature in several ways. First, prior studies generally focus either on investments in fixed assets or investments in financial assets (e.g., Calem & Rizzo, 1995; Reiter, Smith, Wheeler & Rivenson 2000; Reiter, Wheeler & Smith, 2008; Wedig, Hassan & Sloan 1989; Song, Smith & Wheeler, 2008). That approach considers only one dimension of the overall investment strategy and fails to acknowledge the role of financial investments in supporting operations and capital investment. To our knowledge, this is the first study to analyze aggregate asset structures of both fixed and financial assets. Second, earlier studies on hospital investment in financial assets focus exclusively on investment practices in NFP hospitals (Song et al. 2008). In contrast, we compare trends in asset structures between NFP and IO hospitals. We also examine the composition of asset structures over time, offering more insight than cross sectional analysis given the sensitivity of financial investments to market fluctuations. Finally, we extend prior work examining the importance of financial investment income to hospitals’ overall profitability by exploring the relationships between hospital size and profitability and asset structure (McKay and Gapenski, 2009).
Background on Hospital Investment
Medicare reimbursement policies have historically influenced hospitals’ investment practices. Prior to 1992, hospital investment decisions focused primarily on fixed assets, consistent with the incentives present under a cost-based reimbursement system for capital (Trigeorgis & Brindamour, 1993; Wedig, Sloan, Hassan & Morrisey, 1988). Relatively little attention was paid to investments in financial assets as interest income generated from financial investments offset the interest expense reimbursable under a cost based system. The introduction of PPS in 1992 for capital expenditures increased hospitals’ attention to financial assets as evidenced by a decrease in capital expenditures and steady increase in cash balances, particularly among NFP hospitals (Barniv, Danvers, & Healy, 2000; Lynch 2003).
As a result of this growth in cash holdings, income from unrestricted financial investments grew in importance as a contributor to hospitals’ profitability. From 2003–2005, unrestricted investment income comprised approximately 1.3 percent of total revenues in Florida hospitals, and combined with income from other non-operating activities, raised total margins by approximately 1.7 percentage points (McKay and Gapenski 2009).
Using data from California, we compare asset structures between NFP and IO hospitals over a 10-year period, focusing on the relative representation of fixed and financial assets both across hospital characteristics and over time.
Study Data and Methods
Data and Study Sample
Data for this analysis come from the California Office of Statewide Health Planning and Development (OSHPD) Annual Hospital Financial Data for years 1997–2006. California is the largest state that requires hospitals to report financial data and provides the most comprehensive publicly available source of hospital financial data.2 Comprehensive and accurate hospital financial data on a national scale are not available(Magnus and Smith, 2000). We include annual financial reports for all nonfederal, general acute care hospitals. Several hospitals submitted duplicate reports in the same reporting period. In those instances, we kept the report that reflected the greatest number of reporting days. We excluded hospitals with annual reporting periods of fewer than 360 days or greater than 365 days.3 We also excluded reports that were either clearly erroneous or represented extreme outliers.4 Over the 10 year study period, we identified 34 hospitals in the sample that closed according to a report published by the California Hospital Association (California Hospital Association 2008). Mergers were most often reflected by one hospital taking over another (personal communication, OSHPD). Hospitals that merged during the study period are reflected as individual observations in the pre-merger period. In the post-merger period, financial data from these hospitals are reflected in the reports of the acquiring hospitals. The resulting sample includes 3,099 pooled hospital observations representing 382 general acute care hospitals in California from 1997–2006.5
Hospital characteristics for the pooled sample are presented in Table 1. Hospitals are classified as NFP or IO based on hospital reported ownership status on the annual hospital disclosure report. NFP hospitals include nonfederal government, church, or non-profit corporation owned hospitals. Of the 3,099 hospital observations, 74 percent are NFP hospitals. In the aggregate sample, small hospitals (< than 100 beds) represent 26 percent of the pooled observations while medium (100–300 beds) and large (> 300 beds) hospitals represent 47 percent and 27 percent, respectively. NFP hospitals in the sample are larger than IO hospitals with an average of 244 beds versus 163 beds in IO hospitals. NFP and IO hospitals are similar in terms of total asset size, with hospitals averaging $10,968 in total assets per adjusted admission. IO hospitals are more profitable than NFP hospitals with a weighted average operating margin of 7.5 percent versus 2.9 percent in NFP hospitals.
Table 1.
Hospital Descriptive Characteristics 1997–2006
| IO | NFP | Total | |
|---|---|---|---|
| Hospitals Years | (n=792) | (n=2,307) | (n=3,099) |
| 1997 | 90 | 245 | 335 |
| 1998 | 77 | 238 | 315 |
| 1999 | 80 | 237 | 317 |
| 2000 | 82 | 234 | 316 |
| 2001 | 83 | 232 | 315 |
| 2002 | 89 | 224 | 313 |
| 2003 | 83 | 230 | 313 |
| 2004 | 68 | 228 | 296 |
| 2005 | 65 | 218 | 283 |
| 2006 | 75 | 221 | 296 |
| Number of Unique Hospitals | 111 | 271 | 382 |
| Percent of hospitals with 9 or more report years | 61.4% | 84.0% | 78.3% |
| Percent of hospitals with 5 or more report years | 93.2% | 97.0% | 96.0% |
| Hospital Size | |||
| Small (<100 beds) | 218 (27.5%) | 599 (26.0%) | 817 (26.4%) |
| Medium (100–300 beds) | 491 (62.0%) | 957 (41.5%) | 1,448 (46.7%) |
| Large (>300 beds) | 83 (10.5%) | 751 (32.6%) | 834 (26.9%) |
| Asset Size ($) per Adjusted Admission** | Mean (SD) | Mean (SD) | Mean (SD) |
| Financial Assets | 414.5 (1,686) | 2,651 (3,644) | 2,080 (3,401) |
| Real Assets | 4,013 (3,977) | 5,001 (4,309) | 4,749 (4,248) |
| Other Assets | 6,491 (8,373) | 3,331 (2,798) | 4,138 (5,061) |
| Total Assets | 10,919 (10,937) | 10,984 (7,491) | 10,968 (8,503) |
| Operating Margin*** | 7.5% (14.0) | 2.9% (10.1) | 3.6% (10.8) |
| Total Margin*** | 7.6% (13.7) | 7.2% (10.2) | 7.3% (108) |
Source: California Office of Statewide Planning and Development Annual Financial Data for General Acute Care Hospitals 1997–2006, 382 individual hospitals
Hospital Closure data by fiscal year as reported by the California Hospital Association as of 10/30/2008
Admissions adjusted to reflect outpatient activity.
Adjusted to 2006 dollar values.
Mean values for operating and total margins are weighted by total assets
Methods
The focus of this study is on hospitals’ asset allocation in the presence of choice. Therefore, asset structure of the hospital is defined, to the extent possible, based on unrestricted assets, or assets without external agency or donor-imposed restrictions. Consistent with this definition, “assets whose use is limited” are included in the asset structure as restrictions on these funds are typically determined internally by the board versus by an external agency. Assets are categorized into three classes: fixed assets, financial assets, and other assets. Fixed assets include unrestricted property, plant, and equipment (PPE) less accumulated depreciation, construction in progress, and investments in PPE. Financial assets include unrestricted cash, marketable securities, all assets whose use is limited, and investment in other assets. The balance is categorized as “other assets” and primarily includes items such as receivables and intangible assets. All asset values are adjusted for inflation using the consumer price index to reflect 2006 dollar values.
Descriptive statistics are calculated to compare investment practices of IO and NFP hospitals, and to identify differences in investment practices over time. We first present aggregate asset structures of IO and NFP hospitals by comparing the proportion of fixed, financial and other assets to total assets averaged over the 10-year study period. We also compare average proportion of assets by hospital ownership and size where hospital size is defined by the number of licensed beds. We test for significance of the differences in the proportion of asset type to total assets using two-sample independent t-tests at p < 0.05. Second, we measure significance of trends in investments in fixed and financial assets using ordinary least squares regression. The dependent variable is defined as the proportion of asset type. Explanatory variables include ownership, dummy variables reflecting each year in the study period and the interaction of ownership and year. Post-estimation tests (joint F-tests) are used to assess overall significance of the trend at p< 0.05. Compounded annual growth rates are calculated to measure the change in proportion of investment assets over the ten year time period. Finally, for NFP hospitals, we compare average proportion of each asset type by hospital profitability. We classify hospitals into three groups: low profit, medium profit, and high profit. Low profit hospitals are those with an average operating margin of zero or less, medium profit hospitals have operating margins between 0 and 5 percent, and high profit hospitals have average operating margins above 5 percent over the study period.6
Results
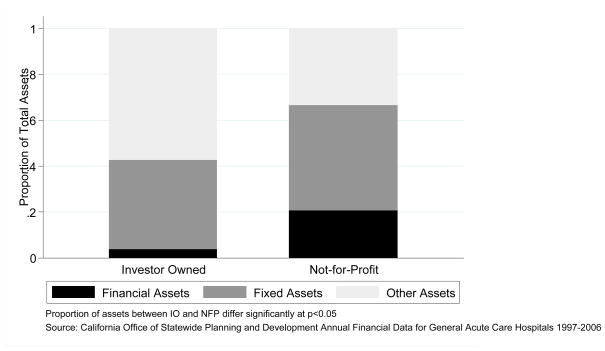
Aggregate asset structure
Hospitals’ aggregate asset structures, exclusive of most restricted assets, averaged over the 10-year study period are presented in Figure 1. Among all hospitals, financial investments represent 17 percent and fixed investments 44 percent of total assets. However, the aggregate asset structures held by NFP hospitals and IO hospitals differ significantly. NFP hospitals hold over five times as many financial assets compared to IO hospitals, with financial assets representing 21 percent of total assets in NFP hospitals compared to 4 percent in IO hospitals. NFP hospitals also hold a greater proportion of fixed assets in their overall asset structures, with 46 percent of total assets dedicated to property, plant and equipment versus 39 percent in IO hospitals. Other assets comprise 33 percent of the aggregate asset structures in NFP hospitals and 57 percent in IO hospitals.
Figure 1.
Hospitals Portfolio of Unrestricted Assets: Average Proportion by Asset Type and Ownership 1997–2006
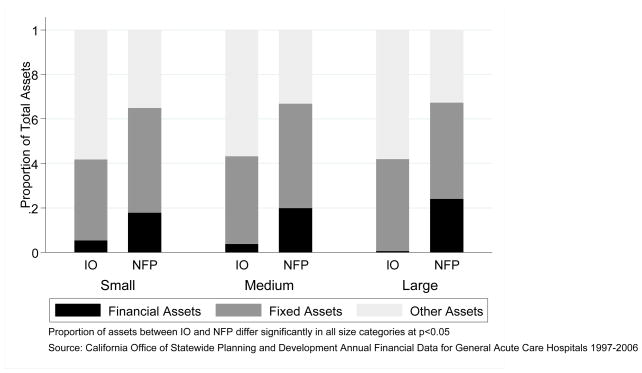
Asset Structure by Hospital Size and Ownership
A similar pattern emerges when analyzing aggregate asset structures by hospital size and ownership (Figure 2). Regardless of hospital size, NFP hospitals hold a significantly greater proportion of financial assets compared to IO hospitals. For NFP hospitals, the proportion of financial assets is positively associated with hospital size. Small NFP hospitals hold 18 percent of total assets in financial assets while large NFP hospitals on average hold over 24 percent in financial assets. In contrast, the proportion of financial assets in IO hospitals is inversely related to hospital size. Small IO hospitals hold approximately 5.5 percent of total assets in financial investments while large IO hospitals hold less than 1 percent in financial investments. The proportion of fixed assets increases with hospital size in IO hospitals from 36 percent in small IO hospitals to 41 percent in large IO hospitals. In NFP hospitals, however, fixed assets are comparable in small and medium sized hospitals (47 percent) but have smaller representation in large hospitals (44 percent).
Figure 2.
Average Proportion by Assets By Hospital Size and Ownership 1997–2006
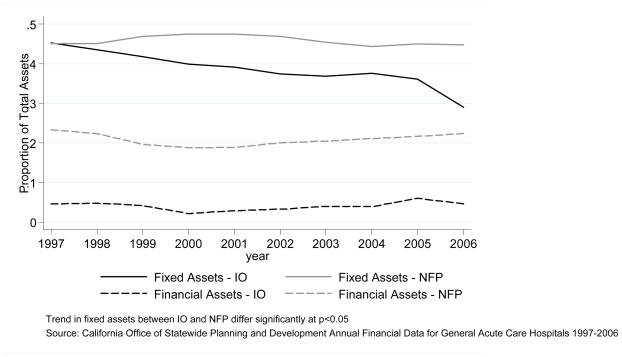
Trends over time
Over the 10 year study period, the trend in proportion of financial investments remained constant for both NFP and IO hospitals (Figure 3). Over the same period, however, significantly different trends emerged between NFP and IO hospitals with regard to fixed assets. NFP hospitals’ proportion of fixed assets to total assets remained unchanged over the 10 years, while the IO hospitals’ proportion of fixed assets decreased 36 percent from 1997 to 2006. This decrease in the proportion of real assets among IO hospitals translates to a compound annual growth rate of − 4.8 percent.
Figure 3.
Trends in Hospitals’ Asset Structure by Ownership 1997–2006
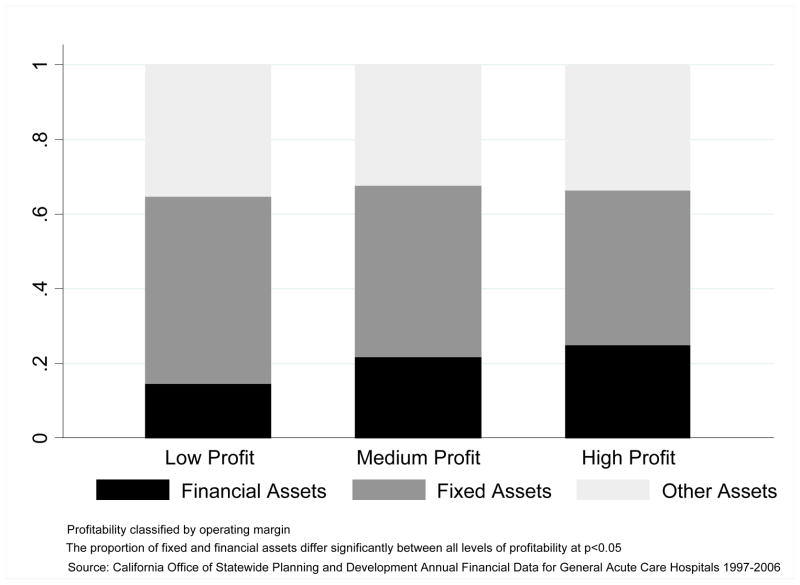
NFP Asset Structure by Hospital Profitability
Trends in asset structure by levels of profitability in NFP hospitals are presented in Figure 4. Similar to hospital size, the level of profitability is positively associated with the proportion of financial assets in NFP hospitals.7 Low profit hospitals hold approximately 15 percent of total assets in financial investments compared with 22 and 25 percent in medium and high profit NFP hospitals, respectively. Low, medium, and high profit hospitals hold statistically significantly different proportions of financial investments. The proportion of fixed assets has a significant inverse relationship with level of profitability. Low profit hospitals hold half of their total assets in property, plant and equipment while medium and high profit hospitals hold 46 and 41 percent, respectively.
Figure 4.
NFP Hospitals Average Proportion of Assets by Profitability 1997–2006
Conclusions
Our analysis demonstrates that hospitals’ aggregate asset structures differ significantly based on ownership. As expected, NFP hospitals hold far more of their total assets in financial securities than do IO hospitals. This difference suggests that financial investments play a strategic role among NFP hospitals, providing precautionary savings and securing favorable bond ratings and access to debt. Given this strategic role, financial investments are likely to be particularly important to NFP hospitals during industry or economic downturns when debt financing is not easily accessible.
In contrast, IO hospitals appear to reinvest earnings in operations and return excess capital to owners. This finding is consistent with a profit maximization objective, and suggests that IO hospitals may be less constrained when accessing external funds because of their broader access to capital markets.
For both types of hospitals, financial securities have remained a relatively consistent proportion of total assets over time, suggesting that investment strategies have not changed substantially over the ten year period. In contrast, representation of fixed assets has declined in investor-owned hospitals over the 10 year period. This result may reflect differences in mission, aging of facilities, and/or agility in adjusting to market conditions. Alternatively, the apparent decline may reflect changes in payer mix or collection strategies that have caused growth in receivables (represented by “other assets”) to outpace growth in fixed capital investment.
Consistent with previous findings showing that financial investment income contributes importantly to hospital revenue and profitability, larger and more profitable NFP hospitals hold greater proportions of their assets in financial securities than do smaller, less profitable NFPs. This difference likely reflects greater resource availability (e.g. access to professional investment managers, access to debt markets in lieu of internal cash reserves) in larger and more profitable hospitals; however, it may also be due to a heavier reliance on financial investments to support operations or a greater strategic focus on financial investment earnings.
This study has several limitations that may affect interpretation of the results. First, the study only considers hospitals in California; therefore, the trends we observe may not be fully generalizable to the rest of the U.S. Second, several significant market changes were occurring during the study period. Tenet, a large IO hospital chain with a substantial presence in California, sold several hospitals during the study period. Tenet’s departure from the California market may have contributed to the decrease in real assets among IO hospitals. For sensitivity, we ran our analysis excluding Tenet hospitals. Excluding Tenet hospitals, IO hospitals decreased their proportion of real assets by 26 percent, or 3.4 percent annually, versus 36 percent and 4.2 percent annually including Tenet; however the difference over time relative to NFP hospitals was not statistically significant. This is not entirely surprising, as Tenet represents 41 percent of the IO hospital observations in our sample. This underscores the impact that a single hospital system with major market presence can have on capital investment behavior observed in hospitals. Tenet was also found guilty of Medicare fraud in 2003, which resulted in a settlement charge of $2 billion. We would expect this to potentially affect their financial asset position, but our results were robust when we excluded Tenet hospitals from our sample.
Third is the influence of system affiliation on reported asset structure. The major concern with system affiliation is the transfer of financial assets to the corporate level that would not be reflected in individual hospital reports. While ideally system affiliated hospitals should allocate assets to individual hospitals, OSHPD does not have clear reporting guidelines for system affiliated hospitals. It is possible that system affiliated hospitals manage financial assets at the corporate level to take advantage of centralized investment management services, which may skew our results. Analysis of asset structure by system status revealed that IO hospitals that were system-affiliated appeared to hold lower proportions of financial assets than independent IO hospitals, suggesting that transfers to the corporate level may occur. However, there were no differences by system status among NFP hospitals.
Fourth, because our analysis focused on unrestricted assets, there was concern that some assets classified as “assets whose use is limited” may be externally restricted. To validate the data, we cross checked several individual hospital reports with their audited financial statements found on recent bond prospectus’. We concluded that “assets whose use is limited” included a limited percentage of restricted accounts which is unlikely to affect our results.
Finally, we focused on fixed and financial assets as a proportion of total assets, and therefore the change in relative proportion of assets does not necessarily reflect the change in absolute dollars.
Despite the limitations, this study provides a first look at hospital asset structure over time, and including both fixed and financial assets. As such, it lays an important foundation for future research looking at hospital investment strategy, and its relationship to hospital performance across a spectrum of outcomes. Future studies should explore management decision-making, particularly with respect to the way hospital managers balance investment in fixed versus financial assets. Research is also needed to quantify the reliance on financial investment income in NFP hospitals nationally, and to understand the consequences for hospital performance if financial investment were to be limited. Lastly, future studies should address the effect of the credit market collapse on fixed capital investment in both IO and NFP hospitals across the U.S.
Footnotes
Not-for-profit hospitals are able to earn arbitrage profits by using their access to tax-exempt debt financing to free up internally generated cash for investment in higher yielding securities. Specifically, hospitals are able to use tax exempt debt in lieu of cash and other financial securities to support expenditures on property and equipment. In turn, hospitals’ cash balances can be invested in taxable debt and other securities that provide returns that are greater than the cost of tax-exempt financing.
Washington, Texas, and Florida also require hospital financial reporting.
In 2003, the majority of the Tenet owned hospitals had abbreviated reporting periods of 214 days (or six months), which subsequently adjusted their fiscal calendar dates going forward. During this time, Tenet announced intentions to sell many of its hospitals in California. For this reporting year only, we kept observations with 214 reporting days as balance sheet items used in this analysis should not be affected by the abbreviated reporting period.
Specifically, 28 reports that reported zero real assets were excluded as erroneous. We also identified outliers based on the mean operating margin plus/minus 3 standard deviations, resulting in the exclusion of 45 reports.
Of the 382 hospitals, 96% have 5 or more annual reports and 78% have 9 or more annual reports over the 10 year period.
Low profit hospitals are the bottom quartile, medium profit hospitals are in the 2nd and 3rd quartile, and high profit hospitals are in the top quartile of operating margins for NFP hospitals.
The correlation between hospital size and profitability is 0.18.
Contributor Information
Paula H. Song, Email: psong@cph.osu.edu, Division of Health Services Management and Policy, The Ohio State University.
Kristin L. Reiter, Email: reiter@email.unc.edu, Department of Health Policy and Management, The University of North Carolina at Chapel Hill.
References
- Barniv R, Danvers K, Healy J. The impact of Medicare capital prospective payment regulation on hospital capital expenditures. Journal of Accounting and Public Policy. 2000;19(1):9–40. [Google Scholar]
- Calem PS, Rizzo JA. Financing Constraints and Investment: New Evidence from Hospital Industry Data. Journal of Money, Credit, and Banking. 1995;27(4):1002–14. [Google Scholar]
- California Hospital Association. Report on Hospital Closures in California. 2008 (Updated 10/30/2008. http://www.calhospital.org.
- Congressional Budget Office. Nonprofit Hospitals and Tax Arbitrage. Washington, D.C.: The Congress of the United States; 2006. [Google Scholar]
- Gentry WM. Debt, Investment, and Endowment Accumulation: The case of Not-For-Profit Hospitals. Journal of Health Economics. 2002;21(5):845–72. doi: 10.1016/s0167-6296(02)00056-5. [DOI] [PubMed] [Google Scholar]
- Kauer RT, Silvers JB. Hospital Free Cash Flow. Health Care Management Review. 1991;16(4):67–78. [PubMed] [Google Scholar]
- Lynch LJ. The effect of Medicare capital prospective payment regulation: additional evidence from hospital financing decisions. Journal of Accounting and Public Policy. 2003;22:151–173. [Google Scholar]
- Magnus SA, Smith DG. Better Medicare cost report data are needed to help hospitals benchmark costs. Health Care Management Review. 2000;25(4):65–76. doi: 10.1097/00004010-200010000-00006. [DOI] [PubMed] [Google Scholar]
- McCue MJ. A Trend Analysis of Hospitals with High Cash and Security Investments. Hospital Topics. 2001;79(1):23–27. doi: 10.1080/00185860109597896. [DOI] [PubMed] [Google Scholar]
- McCue MJ, Thompson JM, Dodd-McCue D. Association of Market, Mission, Operational, and Financial Factors with Hospitals’ Level of Cash and Security Investments. Inquiry. 2000/2001;37(4):411–22. [PubMed] [Google Scholar]
- McKay NL, Gapenski LC. Nonpatient revenues in hospitals. Health Care Management Review. 2009;34(3):234–241. doi: 10.1097/HMR.0b013e3181a16bbc. [DOI] [PubMed] [Google Scholar]
- Reiter KL, Smith DG, Wheeler JRC, Rivenson HL. Capital investment strategies in health care systems. Journal of Health Care Finance. 2000;26(4):31–41. [PubMed] [Google Scholar]
- Reiter KL, Wheeler JRC, Smith DG. Liquidity Constraints on Hospital Investment When Credit Markets are Tight. Journal of Health Care Finance. 2008;35(1):24–33. [Google Scholar]
- Rivenson HL, Wheeler JRC, Smith DG, Reiter KL. Cash Management in Health Care Systems. Journal of Health Care Finance. 2000;26(4):59–69. [PubMed] [Google Scholar]
- Robinson JC. Bond-Market Skepticism and Stock-Market Exuberance in the Hospital Industry. Health Affairs. 2002;21(1):101–117. doi: 10.1377/hlthaff.21.1.104. [DOI] [PubMed] [Google Scholar]
- Song PH, Smith DG, Wheeler JRC. It was the Best of Times, It was the Worst of Times: A Tale of Two Years in Not-for-Profit Hospital Financial Investment. Health Care Management Review. 2008 July/September;33(4):234–242. doi: 10.1097/01.HMR.0000324905.96401.f3. [DOI] [PubMed] [Google Scholar]
- Trigeorgis L, Brindamour P. Distortions in Capital Asset Acquisition and Financing under Cost-Based Reimbursement. The Financial Review. 1993;28(3):417–429. [Google Scholar]
- Wedig GJ, Hassan M, Morrisey MA. Tax-Exempt Debt and the Capital Structure of Nonprofit Organizations: An Application to Hospitals. Journal of Finance. 1996;21(4):1247–1283. [Google Scholar]
- Wedig GJ, Hassan M, Sloan FA. Hospital investment decisions and the cost of capital. The Journal of Business. 1989;4(62):517–537. [Google Scholar]
- Wedig GJ, Sloan F, Hassan M, Morrisey MA. Capital structure, ownership, and capital payment policy: the case of hospitals. Journal of Finance. 1988;43(1):21–40. [Google Scholar]
- Wheeler JRC, Smith DG, Rivenson HL, Reiter KL. Capital Structure Strategy in Health Care Systems. Journal of Health Care Finance. 2000;26(4):42–52. [PubMed] [Google Scholar]