Abstract
Background:
Breastfeeding is known to have beneficial effects, but there is concern that breastfeeding during antiepileptic drug (AED) therapy may be harmful to cognitive development. Animal and human studies have demonstrated that some AEDs can adversely affect the immature brain. However, no investigation has examined effects of breastfeeding during AED therapy on subsequent cognitive abilities in children.
Methods:
The Neurodevelopmental Effects of Antiepileptic Drugs Study is an ongoing prospective multicenter observational investigation of long-term effects of in utero AED exposure on cognition. Between 1999 and 2004, we enrolled pregnant women with epilepsy who were taking a single AED (carbamazepine, lamotrigine, phenytoin, or valproate). We recently reported on differential AED effects on age 3 year cognitive outcomes. In this report, we focus on the effects of breastfeeding during AED therapy on age 3 cognitive outcomes in 199 children.
Results:
A total of 42% of children were breastfed. IQs for breastfed children did not differ from nonbreastfed children for all AEDs combined and for each of the 4 individual AED groups. Mean adjusted IQ scores (95% confidence intervals) across all AEDs were breastfed = 99 (96–103) and nonbreastfed = 98 (95–101). Power was 95% to detect a half SD IQ effect in the combined AED analysis, but was inadequate within groups.
Conclusions:
This preliminary analysis fails to demonstrate deleterious effects of breastfeeding during AED therapy on cognitive outcomes in children previously exposed in utero. However, caution is advised due to study limitations. Additional research is needed to confirm this observation and extend investigations to other AEDs and polytherapy.
GLOSSARY
- AED
= antiepileptic drug;
- NART
= National Adult Reading Test;
- NEAD
= Neurodevelopmental Effects of Antiepileptic Drugs;
- TONI
= Test of Nonverbal Intelligence;
- WASI
= Wechsler Abbreviated Scale of Intelligence.
Breastfeeding is known to be beneficial for the infant and mother.1 Breastfeeding is associated with reduced risk of severe lower respiratory tract infections, atopic dermatitis, asthma, acute otitis media, nonspecific gastroenteritis, obesity, type 1 and 2 diabetes, childhood leukemia, sudden infant death syndrome, and necrotizing enterocolitis. Several studies have suggested that breastfeeding may have positive effects on subsequent cognitive development, but this remains controversial.1 In mothers, breastfeeding is associated with a reduced risk for type 2 diabetes, breast cancer, ovarian cancer, and maternal postpartum depression.
Animal studies have demonstrated that some AEDs can produce widespread neuronal apoptosis in the neonatal brain, which is dose-dependent, occurs at therapeutically relevant blood levels, and requires only brief exposure.2–8 The effect may be due to reduced expression of neurotrophins and levels of protein kinases that promote neuronal growth and survival. Thus, AEDs might produce similar adverse effects in children exposed in utero or in the neonatal period. In fact, some AEDs have been associated with reduced cognitive abilities in children exposed in utero.9–11 Thus, concern exists that breastfeeding during AED therapy might be harmful to the child. However, no investigation has examined the effects of breastfeeding during AED therapy on subsequent cognitive abilities in children. Since neonatal exposure to AEDs via breast milk is voluntary, data are needed for mothers to make informed decisions. Here, we examine the effects of breastfeeding during AED therapy in an ongoing prospective investigation of neurodevelopmental effects of AEDs on cognitive outcomes in children of mothers with epilepsy.
METHODS
Design.
The Neurodevelopmental Effects of Antiepileptic Drugs (NEAD) study is a prospective observational study examining possible behavioral teratogenesis of AEDs. We enrolled pregnant women with epilepsy, who were on 1 of the 4 AED monotherapies (i.e., carbamazepine, lamotrigine, phenytoin, or valproate) from October 1999 through February 2004, across 25 epilepsy centers in the United States and United Kingdom. We recently reported on preliminary findings of cognitive outcomes in the children at 3 years of age.11 Here we test the hypothesis that breastfeeding during AED therapy is detrimental to the child's cognitive development.
Standard protocol approvals and patient consents.
Institutional review boards at each center approved the study, and written informed consent was obtained prior to enrollment.
Participants.
Pregnant women with epilepsy on carbamazepine, lamotrigine, phenytoin, or valproate monotherapy were enrolled. These 4 AED monotherapies were the most frequently employed during the enrollment time period. Other AEDs were not included because of insufficient numbers. Polytherapy was not included because of its association with poorer outcomes.12 A nonexposed control group was not included at the direction of an NIH review panel. Mothers with IQ below 70 were excluded to avoid floor effects and because maternal IQ is the major predictor of child IQ in population studies.13 Other exclusion criteria included positive syphilis or HIV serology, progressive cerebral disease, other major disease (e.g., diabetes), exposure to teratogenic agents other than AEDs, poor AED compliance, drug abuse in the prior year, or drug abuse sequelae.
Procedures.
Information was collected on potentially confounding variables, including maternal IQ, age, education, employment, race, seizure/epilepsy types and frequency, AED dosages, compliance, socioeconomic status,14 UK/US site, preconception folate use, use of alcohol, tobacco, or other drugs during pregnancy, unwanted pregnancy, abnormalities/complications in the present pregnancy or prior pregnancies, enrollment and birth gestational age, birthweight, breastfeeding, and childhood medical diseases. Children were classified as breastfed if they were currently breastfeeding at the time of the 3-month follow-up phone call after delivery. Cognitive outcomes were evaluated by assessors (blinded to AED) using the Differential Ability Scales15 (conducted at 36–45 months/old); standardized scores were calculated. Separate investigations with very similar designs in the United States and United Kingdom were merged after initiation. Maternal IQs were determined by different measures due to the later merger; these measures included the Test of Nonverbal Intelligence (TONI)16 in 267 mothers, Wechsler Abbreviated Scale of Intelligence (WASI)17 in 18, and National Adult Reading Test (NART)18 in 18. Training and monitoring of neuropsychological evaluations were conducted to assure quality and consistency. Face-to-face training on all neuropsychological test batteries was performed annually. Each assessor was required to identify errors in a videotaped test session and provide appropriate correction for errors in administration and scoring. In addition, assessors submitted their own videotape and record forms using each test instrument to the Neuropsychology Core Director for review, feedback, and approval. If assessors failed, they submitted additional video assessment for approval prior to testing children in the study.
Statistical analysis.
The primary analysis in this substudy included 199 children, for whom there were both cognitive assessment at age 3 and data on breastfeeding. Two children with complete data were excluded from this sample because their mothers either switched AED or stopped using AEDs while breastfeeding. In the primary analysis, the breastfed and nonbreastfed groups were compared across all AEDs with respect to child cognitive outcomes at age 3. Secondary analyses examined the following: 1) effects of breastfeeding within each AED group; 2) sensitivity of results to baseline differences in covariates; and 3) sensitivity of results to missing data. Analyses were performed at the NEAD Data and Statistical Center using SAS 9.2.
Linear regression models were used to examine breastfed/nonbreastfed group differences in IQ adjusting for AED group, maternal IQ, standardized AED dose, maternal and gestational age at delivery, and preconception folate. These covariates were found to be significantly related to the age 3 outcomes in our prior analysis.11 A nonparametric Kruskal-Wallis test was used to compare duration of breastfeeding across AED groups.
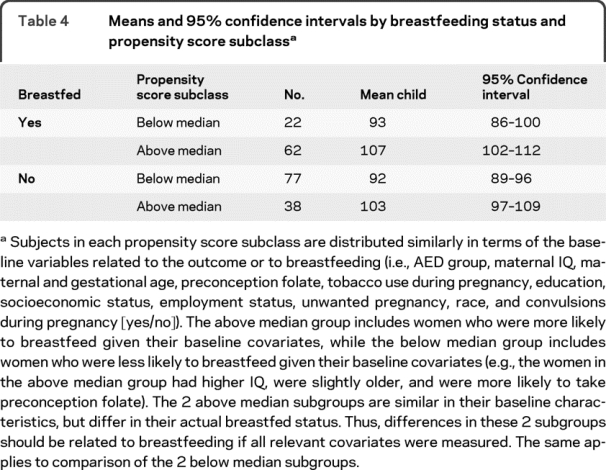
Since the women were not randomized to AED in this observational study, baseline differences between AED groups might obscure a negative effect of an AED taken during breastfeeding. Propensity scores methods are well-accepted tools to examine this possibility. Thus, subgroup analyses were conducted in which subgroups were defined by propensity scores.19,20 Propensity scores are predicted probabilities of receiving a treatment (or in this case, being breastfed) based on baseline covariates. Covariates are approximately equally distributed within subgroups defined by propensity scores. Propensity scores were estimated using predicted probabilities from a logistic regression model with breastfeeding status (yes/no) as outcome. Variables related to breastfeeding were predictors in the propensity score model along with variables significantly related to age 3 IQ.21 The predictors in the propensity score model included AED group, maternal IQ, maternal and gestational age, preconception folate, tobacco use during pregnancy, education, socioeconomic status, employment status, unwanted pregnancy, race, and convulsions during pregnancy (yes/no). Given the resulting distributions of estimated propensity scores in the 2 groups (breastfed and nonbreastfed), subjects were partitioned into 2 subgroups depending on whether their estimated propensity score was above or below the median estimated propensity score. Within each of the 2 resulting subgroups, covariates were balanced between the breastfed and nonbreastfed groups (p > 0.05, t test for continuous variables or χ2 test for categorical variables), permitting us to compare mean IQ outcomes between the breastfed group and the nonbreastfed group.
To investigate sensitivity of primary results to missing data (missing age 3 outcome or missing breastfeeding data), analyses were also conducted using the intent-to-treat sample (n = 309 live births including 6 twin pairs). To account for missing data, a third breastfeeding category was created for “breastfeeding data missing” to compare to the breastfed and nonbreastfed groups. Data were available for breastfeeding in 249 (81%). Age 3 outcomes were missing in 77 (25%). Two were excluded from the analysis because the mother stopped AED or switched AED while breastfeeding, resulting in an analysis sample size of n = 307. Monotone data Markov Chain Monte Carlo methods were used in secondary analyses to impute missing age 3 outcomes.22–24 Missing age 3 outcomes were imputed from available age 2 outcomes (n = 26 of 77) and from baseline variables related to outcome or likelihood of missing outcome data (n = 51 of 77). Baseline variables in the imputation model included AED, dose, maternal IQ and age, gestational age at delivery, preconception folate, socioeconomic status, and US/UK site. Least squares mean IQs were estimated for the breastfed and nonbreastfed groups adjusting for maternal IQ, AED group, maternal age, dose, gestational age, and folate. Standard errors and confidence intervals of all estimates incorporated imputation uncertainty.
RESULTS
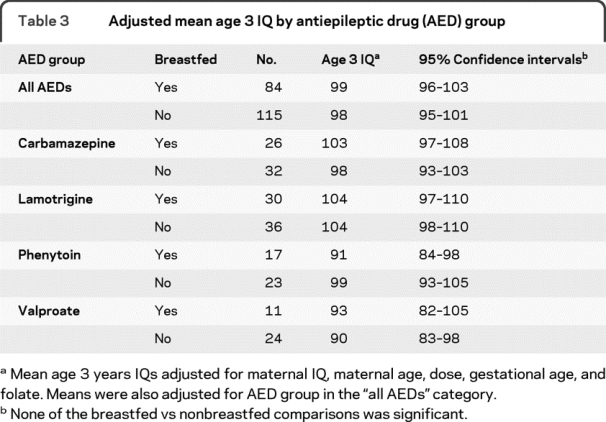
The primary analysis included 194 mothers and 199 children (5 sets of twins). Baseline characteristics of the breastfed and nonbreastfed groups and differences between groups are depicted in table 1. The statistical results for the primary analysis of all AEDs combined are presented in table 2. No effect of breastfeeding was seen on IQ outcomes at age 3. Follow-up analyses for each AED group individually also found no effect of breastfeeding on IQ. Table 3 summarizes the sample sizes, adjusted mean IQs, 95% confidence intervals, and statistical comparisons for all AEDs combined and for each AED group. Overall, 42% of children were breastfed; median time breastfeeding across all AEDs was 6 months (range 3–24 months). The percent breastfed for each AED group were as follows: CBZ = 44%, LTG = 46%, PHT = 42%, and VPA = 32%, which did not differ statistically across AEDs (p = 0.61). AED groups also did not differ in breastfeeding duration (p = 0.70). Mean adjusted IQ scores (95% confidence intervals) across all AEDs were as follows: breastfed = 99 (96:103) and nonbreastfed = 98 (95:101). Power was 95% to detect a half SD IQ effect in the combined AED analysis, but was inadequate within groups. Note that the mean IQ scores in table 3 differ from those presented in our prior publication11 because the primary analyses differed. The present IQ results are divided by breastfed/nonbreastfed and are based on a subset of 199 children for whom there were both cognitive assessment at age 3 and data on breastfeeding. The prior publication presented IQs based on an intent-to-treat analysis of the full 307 live births. Nevertheless, the differential pattern across AEDs is the same with the lowest IQs associated with in utero valproate exposure.
Table 1 Baseline characteristics of 194 mothers according to breastfed category for the 199 children
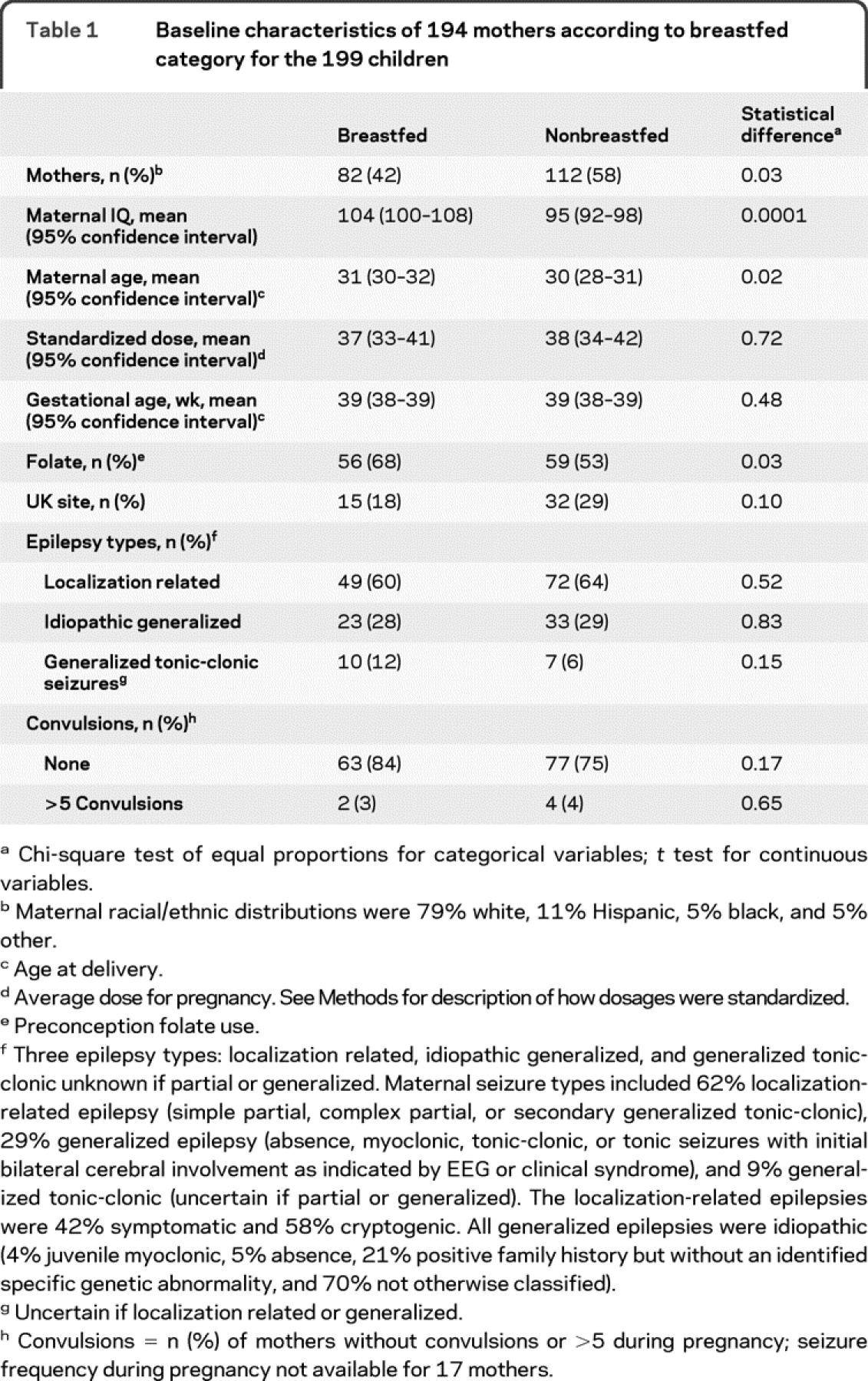
Table 2 Statistical results for effects of breastfeeding and other factors on age 3 child IQ based on regression models for the age 3 completer population with data on breastfeeding (n = 199)
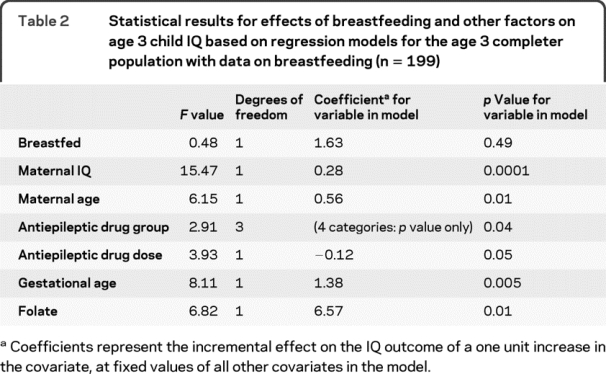
Table 3 Adjusted mean age 3 IQ by antiepileptic drug (AED) group
The propensity score analysis suggests that the results are not due to differences in baseline variables related to either the child IQ outcome or breastfeeding status (table 4). The analysis examining sensitivity of results to missing data demonstrates that the results cannot be explained by incomplete data. A summary of missing data for age 3 IQ and for breastfeeding for each AED group is given in table e-1 (on the Neurology® Web site at www.neurology.org). In the intent-to-treat sample, which included 307 of the originally enrolled children, missing outcomes were imputed and a third breastfeeding category was created for missing breastfeeding data. The adjusted mean IQs (95% confidence intervals) are as follows: breastfed = 100 (96–103); nonbreastfed = 97 (94–100); missing breastfeeding data = 97 (92–102).
Table 4 Means and 95% confidence intervals by breastfeeding status and propensity score subclass
DISCUSSION
The present study did not demonstrate any deleterious effects of breastfeeding during AED therapy on cognitive outcomes in children who were previously exposed to AEDs during their mother's pregnancy. Similar to our prior report,11 IQ at age 3 years in children of women with epilepsy is related to maternal IQ, maternal age, gestational age, preconception folate use, and type of AED exposure. Fetal valproate exposure was associated with lower IQ in a dose-dependent manner, consistent with other studies that indicate a special teratogenic risk for valproate.12 Children exposed in utero to valproate are at risk for both congenital malformations and cognitive impairment.9–12,25,26 The recent American Academy of Neurology guidelines recommend that if possible, valproate should be avoided during the first trimester of pregnancy to decrease the risk of major congenital malformations and avoided throughout pregnancy to prevent reduced cognitive outcomes.12
Strengths of our study include its prospective design, blinded cognitive assessments using standardized measures, and detailed monitoring of multiple potential confounding factors. However, caution is advised due to study limitations, which include a relatively small sample size, loss of enrolled subjects to analysis, lack of randomization, lack of an unexposed control group during pregnancy, lack of details to fully quantitate the amount of breastfeeding, absence of AED concentrations in breast milk or in children's serum, and relatively young age of the children at this planned interim analysis. In addition, the present study does not address any potential deleterious effects of AED exposure through breast milk in the newborn not previously exposed in utero.
Because the NEAD study is not a randomized trial, it is possible that an adverse effect of breastfeeding during AED therapy might be obscured by confounding factors related to baseline characteristics, which might affect the child's IQ. For example, maternal IQ was higher in the breastfeeding group, and preconception folate use was also higher in the breastfeeding group. Further, a larger portion of patients on valproate had generalized epilepsy. However, no adverse effects of breastfeeding were found in analyses adjusting for these and other baseline characteristics, including the propensity score subgroup analyses.
Rather than epilepsy or seizures, most AED prescriptions are written for pain or psychiatric indications. Our study did not include women who were prescribed AEDs for these other indications, but there is concern that their children are at the same risk, since one study found that incidence of malformations in these children is similar to that of children of women taking AEDs for epilepsy.27
Why would adverse cognitive outcomes be associated with in utero exposure for some AEDs (e.g., valproate), but not for exposure to breastfeeding? Susceptibility to AED exposure may be greater for the fetal than neonatal brain, but animal studies would suggest that this is not the case. The adverse effects on the immature brain seen with some AEDs are dose dependent. The blood levels achieved in the child during breastfeeding are likely to be substantially lower than those achieved during pregnancy,28 and thus, may be inadequate to produce the adverse effects. Alternatively, adverse effects produced from in utero exposure may mask any further smaller effects obtained during breastfeeding. In addition, the proposed benefits of breastfeeding on newborn cognitive development1 could offset potential deleterious effects of continued AED exposure. Although not significant, fewer mothers on valproate breastfed, but the mean IQ of children of women with epilepsy on valproate who breastfed was not less than the mean among those who did not breastfeed while taking valproate (see table 3). Other baseline differences between the breastfed and nonbreastfed groups may have obscured breastfeeding effects, but as noted previously propensity score analyses did not provide evidence for this hypothesis.
Further studies are needed to confirm our preliminary analysis and to extend investigations to other AEDs and to AED polytherapy. In addition, it is critical that research be conducted to understand the underlying mechanisms of adverse AED effects on the immature brain and to define the risks associated with AEDs in the neonate for treatment of seizures where the AED blood levels are higher.
COINVESTIGATORS
The NEAD Study Group: David Labiner, MD (Arizona Health Sciences Center, Tucson, AZ, Site Investigator), Jennifer Moon, PhD (Arizona Health Sciences Center, Tucson, AZ, Site Investigator), Scott Sherman, MD (Arizona Health Sciences Center, Tucson, AZ, Site Investigator), Deborah T. Combs Cantrell, MD (Baylor Medical Center, Irving, TX, Site Investigator), Cheryl Silver, PhD (University of Texas-Southwestern, Dallas, TX, Site Investigator), Monisha Goyal, MD (Case Western Reserve University, Cleveland, OH, Site Investigator), Mike R. Schoenberg, PhD (Case Western Reserve University, Cleveland, OH, Site Investigator), Alison Pack, MD (Columbia University, New York, NY, Site Investigator), Christina Palmese, PhD (Columbia University, New York, NY, Site Investigator), Joyce Echo, PhD (Columbia University, New York, NY, Site Investigator), Kimford J. Meador, MD (Emory University, Atlanta, GA, Principal Investigator), David Loring, PhD (Emory University, Atlanta, GA, Site Investigator), Page Pennell, MD (Emory University, Atlanta, GA, Site Investigator), Daniel Drane, PhD (Emory University, Atlanta, GA, Site Investigator), Eugene Moore, BS (Emory University, Atlanta, GA, Site Investigator), Megan Denham, MAEd (Emory University, Atlanta, GA, Site Investigator), Charles Epstein, MD (Emory University, Atlanta, GA, Site Investigator), Jennifer Gess, PhD (Emory University, Atlanta, GA, Site Investigator), Sandra Helmers, MD (Emory University, Atlanta, GA, Site Investigator), Thomas Henry, MD (Emory University, Atlanta, GA, Site Investigator), Gholam Motamedi, MD (Georgetown University, WA, DC, Site Investigator), Erin Flax, BS (Georgetown University, Washington, DC, Site Investigator), Edward Bromfield, MD (Harvard–Brigham & Women's, Boston, MA, Site Investigator), Katrina Boyer, PhD (Harvard–Brigham & Women's, Boston, MA), Barbara Dworetzky, ScB, MD (Harvard-Brigham & Women's, Boston, MA, Site Investigator), Andrew Cole, MD (Harvard–Massachusetts General, Boston, MA, Site Investigator), Lucila Halperin, BA (Harvard–Massachusetts General, Boston, MA, Site Investigator), Sara Shavel-Jessop, BA (Harvard–Massachusetts General, Boston, MA, Site Investigator), Gregory Barkley, MD (Henry Ford Hospital, Detroit, MI, Site Investigator), Barbara Moir, MS (Henry Ford Hospital, Detroit, MI, Site Investigator), Cynthia Harden, MD (Medical College of Cornell University, New York, NY, Site Investigator), Tara Tamny-Young, PhD (Medical College of Cornell University, New York, NY, Site Investigator), Gregory Lee, PhD (Medical College of Georgia, Augusta, GA, Site Investigator), Morris Cohen, EdD (Medical College of Georgia, Augusta, GA), Patricia Penovich, MD (Minnesota Epilepsy Group, St. Paul, MN, Site Investigator), Donna Minter, EdD (Minnesota Epilepsy Group, St. Paul, MN, Site Investigator), Layne Moore, MD (Ohio State University, Columbus, OH, Site Investigator), Kathryn Murdock, MA (Ohio State University, Columbus, OH, Site Investigator), Joyce Liporace, MD (Riddle Health Care, Media, PA, Site Investigator), Kathryn Wilcox, BS (Riddle Health Care, Media, PA, Site Investigator), Andres Kanner, MD (Rush University Medical Center, Chicago, I, Site Investigator L), Michael N. Nelson, PhD (Rush University Medical Center, Chicago, I, Site Investigator L), William Rosenfeld, MD (The Comprehensive Epilepsy Care Center for Children and Adults, St. Louis, MO, Site Investigator), Michelle Meyer, MEd (The Comprehensive Epilepsy Care Center for Children and Adults, St. Louis, MO, Site Investigator), Jill Clayton-Smith, MD (St. Mary's Hospital, Manchester, England, Site Investigator), George Mawer, MD (St. Mary's Hospital, Manchester, England, Site Investigator), Usha Kini, MD (St. Mary's Hospital, Manchester, England, Site Investigator), Roy Martin, PhD (University Alabama, Birmingham, AL, Site Investigator), Michael Privitera, MD (University of Cincinnati, Cincinnati, OH, Site Investigator), Jennifer Bellman, PsyD (University of Cincinnati, Cincinnati, OH), David Ficker, MD (University of Cincinnati, Cincinnati, OH, Site Investigator), Lyle Baade, PhD (University of Kansas School of Medicine–Wichita, Wichita, KS, Site Investigator), Kore Liow, MD (University of Kansas School of Medicine–Wichita, Wichita, KS, Site Investigator), David Chadwick, MD (University of Liverpool, Liverpool, England, Site Investigator), Gus Baker, PhD (University of Liverpool, Liverpool, England, Site Investigator), Alison Booth, BSc (University of Liverpool, Liverpool, England, Site Investigator), Rebecca Bromley, BSc (University of Liverpool, Liverpool, England, Site Investigator), Sara Dutton, BSc (University of Liverpool, Liverpool, England, Site Investigator), James Kelly, BSc (University of Liverpool, Liverpool, England, Site Investigator), Jenna Mallows, BSc (University of Liverpool, Liverpool, England, Site Investigator), Lauren McEwan, MSc (University of Liverpool, Liverpool, England, Site Investigator), Laura Purdy, BSC (University of Liverpool, Liverpool, England, Site Investigator), Eugene Ramsay, MD (University of Miami, Miami, FL, Site Investigator), Patricia Arena, PhD (University of Miami, Miami, FL, Site Investigator), Laura Kalayjian, MD (University of Southern California, Los Angeles, CA, Site Investigator), Christianne Heck, MD (University of Southern California, Los Angeles, CA, Site Investigator), Sonia Padilla, PsyD (University of Southern California, Los Angeles, CA, Site Investigator), John Miller, MD (University of Washington, Seattle, WA, Site Investigator), Gail Rosenbaum, BA (University of Washington, Seattle, WA, Site Investigator), Alan Wilensky, MD (University of Washington, Seattle, WA, Site Investigator), Tawnya Constantino MD (University of Utah, Salt Lake City, UT, Site Investigator), Julien Smith, PhD (University of Utah, Salt Lake City, UT, Site Investigator), Naghme Adab, MD (Walton Centre for Neurology & Neurosurgery, Liverpool, England, Site Investigator), Gisela Veling-Warnke, MD (Walton Centre for Neurology & Neurosurgery, Liverpool, England, Site Investigator), Maria Sam, MD (Wake Forest University, Winston-Salem, NC, Site Investigator), Cormac O'Donovan, MD (Wake Forest University, Winston-Salem, NC, Site Investigator), Cecile Naylor, PhD (Wake Forest University, Winston-Salem, NC, Site Investigator), Shelli Nobles, MS (Wake Forest University, Winston-Salem, NC, Site Investigator), Cesar Santos, MD (Wake Forest University, Winston-Salem, NC, Site Investigator). Executive Committee Coinvestigators: Gregory L. Holmes, MD (Dartmouth Medical School, Hanover, NH), Maurice Druzin, MD (Stanford University, Stanford, CA), Martha Morrell, MD (Stanford University, Stanford, CA), Lorene Nelson, PhD (Stanford University, Stanford, CA), Richard Finnell, PhD (Texas A & M University Health Science Center, Houston, TX), Mark Yerby, MD (University of Oregon, Portland, OR), Khosrow Adeli, PhD (University of Toronto, Toronto, Ontario, Canada), Peter Wells, PharmD (University of Toronto, Toronto, Ontario, Canada). Data and Statistical Center Coinvestigators: Temperance Blalock, AA (EMMES Corporation, Rockville, MD), Nancy Browning, PhD (EMMES Corporation, Rockville, MD), Todd Crawford, MS (EMMES Corporation, Rockville, MD), Linda Hendrickson (EMMES Corporation, Rockville, MD), Bernadette Jolles, MA (EMMES Corporation, Rockville, MD), Meghan Kelly Kunchai, MPH (EMMES Corporation, Rockville, MD), Hayley Loblein, BS (EMMES Corporation, Rockville, MD), Yinka Ogunsola, BS (EMMES Corporation, Rockville, MD), Steve Russell, BS (EMMES Corporation, Rockville, MD), Jamie Winestone, BS (EMMES Corporation, Rockville, MD), Mark Wolff, PhD (EMMES Corporation, Rockville, MD), Phyllis Zaia, BS (EMMES Corporation, Rockville, MD), Thad Zajdowicz, MD, MPH (EMMES Corporation, Rockville, MD).
ACKNOWLEDGMENT
The investigators thank the children and families who have given their time to participate in the NEAD Study.
DISCLOSURE
Dr. Meador serves on the editorial boards of Neurology®, Behavior & Neurology, Epilepsy and Behavior, Epilepsy Currents, Epilepsy.com, and the Journal of Clinical Neurophysiology and on the Professional Advisory Board for the Epilepsy Foundation; received travel support from Sanofi-Aventis; and received research support from GlaxoSmithKline, Eisai Inc., Marinus Pharmaceuticals, Inc., Myriad Genetics, Inc., NeuroPace, Inc., Pfizer, SAM Technology Inc., SCHWARZ PHARMA (UCB), the NIH (NINDS 2RO1-NS38455 Meador [PI], NINDS R01-NSO31966-11A2 [consultant], NINDS N01-NS-5-2364 [consultant], NINDS R01-NSO39466 [coinvestigator], and 1RC1MD004563 [coinvestigator]), and the Epilepsy Foundation. Dr. Baker serves on a scientific advisory board for Sanofi-Aventis; serves on the editorial board of Epilepsy and Behavior; has received speaker honoraria from Eisai Inc., UCB, and Janssen; receives research support from UCB, Sanofi-Aventis, Pfizer Inc., Epilepsy Research UK, Medical Research Council, and Epilepsy Action UK; and has served as an expert witness in litigation related to neurodevelopment effects of antiepileptic drugs. Dr. Browning receives research support from the NIH (NINDS R01 NS050659 [Statistician, Data Center PI]) and holds stock in Human Genome Sciences, Inc. Dr. Clayton-Smith is journal editor for Clinical Dysmorphology and has served as an expert witness in litigation related to neurodevelopment effects of antiepileptic drugs. Dr. Combs-Cantrell has received speaker honoraria from GlaxoSmithKline. Dr. Cohen serves on the editorial board of Developmental Neuropsychology and receives royalties from the publication of Children's Memory Scale (The Psychological Corp., 1997). Dr. Kalayjian has received speaker honoraria from GlaxoSmithKline and Ortho-McNeil-Janssen Pharmaceuticals, Inc. and receives research support from Marinus Pharmaceuticals, Inc. Dr. Kanner has served on scientific advisory boards for GlaxoSmithKline, Ortho-McNeil-Janssen Pharmaceuticals, Inc., UCB, Valeant Pharmaceuticals International, and Pfizer Inc.; has received speaker honoraria from GlaxoSmithKline, Ortho-McNeil-Janssen Pharmaceuticals, Inc., UCB, and Pfizer Inc.; serves on the editorial boards of Epilepsy & Behavior, Epilepsia, and CNS Spectrums; receives royalties from the publication of Psychiatric Issues in Epilepsy, Second Edition: A Practical Guide to Diagnosis and Treatment (Lippincott Williams & Wilkins, 2006) and Controversial Issues in Psychiatric Aspects of Epilepsy (Elsevier, 2008); has served on speakers' bureaus for GlaxoSmithKline, UCB, and Pfizer Inc.; and receives research support from GlaxoSmithKline and Novartis. Dr. Liporace receives royalties from the publication of Crash Course Neurology (Elsevier, 2006) and has served on speakers' bureaus for and received speaker honoraria from UCB and GlaxoSmithKline. Dr. Pennell has served on a scientific advisory board for and received funding for travel from UCB and the Epifellows Foundation; serves as a contributing editor for Epilepsy Currents and on the editorial board of Epilepsia; and has received research support from UCB, GlaxoSmithKline, Marinus Pharmaceuticals, Inc., the NIH (1P50 MH68036-01 [Project 1 PI], NINDS RO3 NS063233 [PI], NINDS RO1 NS 39466 [Site PI], and NINDS RO1NS38455 [PI, Codirector of Administrative Core]), the Centers for Disease Control and Prevention, and the Emory University Research Council. Dr. Privitera has served on scientific advisory boards or as a consult for Ortho-McNeil-Janssen Pharmaceuticals, Inc., UCB, Johnson & Johnson, and the Epifellows Foundation; has received funding for travel and speaker honoraria from Ortho-McNeil-Janssen Pharmaceuticals, Inc., Pfizer Inc., GlaxoSmithKline, Janssen, and UCB; has served on speakers' bureaus for UCB, Pfizer Inc., GlaxoSmithKline, and Ortho-McNeil-Janssen Pharmaceuticals, Inc.; and has received research support from UCB, Ortho-McNeil-Janssen Pharmaceuticals, Inc., the NIH (K01-DA020485 [co-I], K23 NS052468 [co-Mentor], 1K23NS02170-01 [co-I], 2R01-NS38455 [site PI]), the American Epilepsy Society, and the Shor Foundation for Epilepsy Research. Dr. Loring serves on scientific advisory boards for the Epilepsy Foundation and Sanofi-Aventis; serves as a consulting editor for the Journal of Clinical and Experimental Neuropsychology, as contributing editor for Epilepsy Currents, and on the editorial board of Neuropsychology Review; serves as a consultant for NeuroPace, Inc., Sanofi-Aventis, and UCB; receives royalties from the publication of Neuropsychological Assessment, 4th ed. (Oxford University Press, 2004) and INS Dictionary of Neuropsychology (Oxford University Press, 1999); estimates that 50% of his clinical effort involves neuropsychological testing; and receives research support from NeuroPace, Inc., SAM Technology Inc., Myriad Pharmaceuticals, Inc., Novartis, the NIH (NINDS R01038455 [co-I] and NINDS R01NS031966 [consultant)], and the Epilepsy Foundation.
Address correspondence and reprint requests to Dr. Kimford J. Meador, Department of Neurology, Emory University, Woodruff Memorial Research Building, 101 Woodruff Circle, Suite 6000, Atlanta, GA 30322 kimford.meador@emory.edu
Editorial, page 1948
Supplemental data at www.neurology.org
e-Pub ahead of print on November 24, 2010, at www.neurology.org.
Study funding: Supported by the NIH/NINDS (2 RO1 NS038455 and R01NS050659) and the UK Epilepsy Research Foundation (RB219738).
Disclosure: Author disclosures are provided at the end of the article.
Received February 1, 2010. Accepted in final form May 7, 2010.
REFERENCES
- 1.Ip S, Chung M, Raman G, et al. A summary of the Agency for Healthcare Research and Quality's evidence report on breastfeeding in developed countries. Breastfeed Med 2009;4(suppl 1):S17–S30. [DOI] [PubMed] [Google Scholar]
- 2.Bittigau P, Sifringer M, Genz K, et al. Antiepileptic drugs and apoptotic neurodegeneration in the developing brain. Proc Natl Acad Sci USA 2002;99:15089–15094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bittigau P, Sifringer M, Ikonomidou C. Antiepileptic drugs and apoptosis in the developing brain. Ann NY Acad Sci 2003;993:103–114. [DOI] [PubMed] [Google Scholar]
- 4.Glier C, Dzietko M, Bittigau P, et al. Therapeutic doses of topiramate are not toxic to the developing rat brain. Exp Neurol 2004;187:403–409. [DOI] [PubMed] [Google Scholar]
- 5.Katz I, Kim J, Gale K, Kondratyev A. Effects of lamotrigine alone and in combination with MK-801, phenobarbital, or phenytoin on cell death in the neonatal rat brain. J Pharmacol Exp Ther 2007;322:494–500. [DOI] [PubMed] [Google Scholar]
- 6.Kim JS, Kondratyev A, Tomita Y, Gale K. Neurodevelopmental impact of antiepileptic drugs and seizures in the immature brain. Epilepsia 2007;48(suppl 5):19–26. [DOI] [PubMed] [Google Scholar]
- 7.Manthey D, Asimiadou S, Stefovska V, et al. Sulthiame but not levetiracetam exerts neurotoxic effect in the developing rat brain. Exp Neurol 2005;193:497–503. [DOI] [PubMed] [Google Scholar]
- 8.Stefovska VG, Uckermann O, Czuczwar M, et al. Sedative and anticonvulsant drugs suppress postnatal neurogenesis. Ann Neurol 2008;64:434–445. [DOI] [PubMed] [Google Scholar]
- 9.Adab N, Kini U, Vinten J, et al. The longer term outcome of children born to mothers with epilepsy. J Neurol Neurosurg Psychiatry 2004;75:1575–1583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gaily E, Kantola-Sorsa E, Hiilesmaa V, et al. Normal intelligence in children with prenatal exposure to carbamazepine. Neurology 2004;62:28–32. [DOI] [PubMed] [Google Scholar]
- 11.Meador KJ, Baker GA, Browning N, et al. Cognitive function at 3 years of age after fetal exposure to antiepileptic drugs. N Engl J Med 2009;360:1597–1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harden CL, Meador KJ, Pennell PB, et al. Practice Parameter update: management issues for women with epilepsy: focus on pregnancy (an evidence-based review): teratogenesis and perinatal outcomes: Report of the Quality Standards Subcommittee and Therapeutics and Technology Subcommittee of the American Academy of Neurology and American Epilepsy Society. Neurology 2009;50:1237–46. [DOI] [PubMed] [Google Scholar]
- 13.Sattler JM. Assessment of Children, 3rd ed. San Diego: Jerome M. Sattler Pub., Inc.; 1992. [Google Scholar]
- 14.Hollingshead AB. Four Factor Index of Social Status. New Haven, CT: Yale University; 1975. [Google Scholar]
- 15.Elliot CD. Differential abilities scales. San Antonio, TX: The Psychological Corporation; 1990. [Google Scholar]
- 16.Brown L, Sherbenou RJ, Johnsen SK. Test of Non-verbal Intelligence (TONI-3), 3rd ed. Austin, TX: Pro-Ed; 1996. [Google Scholar]
- 17.Wechsler D. Wechsler Abbreviated Scale of Intelligence (WASI). San Antonio, TX: Psychological Corporation; 1999. [Google Scholar]
- 18.Nelson H, Willison J. National adult reading test (NART). Oxford, England: NFER-Nelson Publishing; 1991. [Google Scholar]
- 19.Rosenbaum P, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika 1983;70:41–55. [Google Scholar]
- 20.D'Agostino RB. Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med 1998;17:2265–2281. [DOI] [PubMed] [Google Scholar]
- 21.Brookhart MA, Schneeweiss S, Rothman KJ, et al. Variable selection for propensity score models. Am J Epidemiol 2006;163:1149–1156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Little RJA, Rubin DB. Statistical Analysis with Missing Data, 2nd ed. New York: John Wiley & Sons, Inc.; 2002. [Google Scholar]
- 23.Schafer JL. Analysis of Incomplete Multivariate Data. New York: Chapman and Hall; 1997. [Google Scholar]
- 24.Li KH. Imputation using Markov chains. J Stat Comput Simul 1988;30:57–79. [Google Scholar]
- 25.Meador K, Reynolds MW, Crean S, et al. Pregnancy outcomes in women with epilepsy: a systematic review and meta-analysis of published pregnancy registries and cohorts. Epilepsy Res 2008;81:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Meador KJ, Baker G, Cohen MJ, et al. Cognitive/behavioral teratogenetic effects of antiepileptic drugs. Epilepsy Behav 2007;11:292–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Holmes LB, Harvey EA, Coull BA, et al. The teratogenicity of anticonvulsant drugs. N Engl J Med 2001;344:1132–1138. [DOI] [PubMed] [Google Scholar]
- 28.Hovinga CA, Pennell PB. Antiepileptic drug therapy in pregnancy II: fetal and neonatal exposure. Int Rev Neurobiol 2008;83:241–258. [DOI] [PubMed] [Google Scholar]




