Abstract
Study Objectives:
To assess the utility of Mallampati class, a simple grade of oropharyngeal appearance used to assess difficulty of intubation, to predict severe obstructive sleep apnea and absence of OSA (rule in severe OSA and rule out OSA).
Method:
Retrospective review of consecutive patients undergoing diagnostic polysomnography in a tertiary referral sleep disorders center. Modified Mallampati class and other simple patient characteristics (age, gender, body mass index) were compared to apnea-hypopnea index (AHI). The sensitivity, specificity, and the positive and negative likelihood ratios (LR+ and LR−) were calculated for Mallampati class IV to detect an AHI > 30 (rule in severe OSA) and Mallampati class I to detect an AHI < 5 (rule out OSA).
Results:
A total of 953 consecutive patients (619 male) undergoing diagnostic polysomnography were included. The age of the cohort was 50.0 ± 6.4 years, with a BMI of 33.8 ± 8.6 kg/m2 and AHI of 26.1 ± 25.1 /h (95% CI 1.4-78.8). Mallampati class was significantly associated with AHI (r = 0.13, p < 0.001), but there were no differences in AHI between Mallampati classes. A Mallampati class IV had a sensitivity of 40%, specificity of 67%, LR+ of 1.21, and LR− of 0.90 for an AHI > 30. A Mallampati class I was only 13% sensitive but 92% specific for an AHI < 5, with LR+ of 1.63 and LR− 0.90.
Conclusions:
Mallampati class is associated with AHI but does not significantly modify likelihood of severe OSA or absence of OSA. As such, it is of limited use to “rule in” severe OSA or “rule out OSA” in the sleep clinic population.
Citation:
Hukins C. Mallampati class is not useful in the clinical assessment of sleep clinic patients. J Clin Sleep Med 2010;6(6):545-549.
Keywords: Mallampati class, sleep apnea, prediction, polysomnography
The burden of obstructive sleep apnea (OSA) greatly exceeds the current capacity for diagnosis with polysomnography. It is estimated that more than 80% of patients with OSA remain untreated.1,2 This has resulted in significant delays for polysomnography in many centers.3 The notion of simple clinical characteristics that may predict subjects with significant OSA and allow for expedited assessment therefore is very attractive. Similarly, the ability to rule out OSA and avoid the need for polysomnography based on a simple clinical feature is highly desirable. Symptoms alone are non-discriminatory either in detecting OSA (ruling in OSA) or ruling out this condition. This is particularly true for the sleep clinic population which is an already selected cohort. Rodsutti et al4 reported the cardinal symptoms of OSA were also frequent in the non-apneic patients, with snoring occurring in 56%, choking in 67%, witnessed apneas in 35%, and waking unrefreshed in 68%. The combination of clinical features into clinical prediction models fare little better, achieving specificities of only 13% to 54% in the detecting an apnea-hypopnea index (AHI) of ≥ 10.5
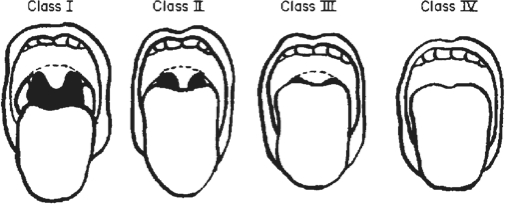
Patients with OSA have reduced upper airway cross-sectional dimensions compared to non-snorers based on complex imaging not available at the bedside.6,7 These anatomical deficits in the upper airway are likely to be involved in the pathogenesis of OSA.8 Mallampati class, an anesthetic assessment of intubation risk based on the morphology of the oropharynx, has been suggested as a possible simple assessment tool for OSA. This simple assessment was first described by Mallampati et al9 in 1985 with 3 grades, but was later modified to 4 classes (modified Mallampati class).10 The assessment is made with the patient sitting with the head in a neutral position, the mouth opened, and the tongue protruded maximally without phonation. The class is then graded based on the visibility of the airway structures (Figure 1): Grade I – tonsils, pillars and soft palate are all clearly visible; Grade II – the uvula, pillars and upper pole are visible; Grade III – only part of the soft palate is visible but the uvula is partly obscured, and Grade IV – only the hard palate is visible. There is good inter-observer agreement with the use of this classification, especially in more senior clinicians.11
Figure 1.
Mallampati class
Reproduced with permission10
BRIEF SUMMARY
Current Knowledge/Study Rationale: Upper airway anatomy is involved in the pathogenesis of OSA. Mallampati Class, a simple descriptor of upper airway morphology used in anesthetics, has been shown to be significantly related to severity of OSA based on AHI and has been suggested to be a useful sign in the clinical assessment of OSA.
Study Impact: Mallampati Class does not significantly influence pre-test probability for presence of severe OSA or absence of OSA in a sleep clinic population. Mallampati Class is not useful in the screening of sleep clinic patients for severe OSA or to rule out OSA.
There is some validation of the use of Mallampati class in clinical assessment for sleep apnea. Hiremath et al12 reported that a higher Mallampati class (more oropharyngeal crowding) was associated with increased prevalence of both OSA and difficult intubation in a cohort of patients undergoing anesthesia. Liistro13 reported a significant correlation between AHI and Mallampati class in 202 subjects undergoing polysomnography, but this association was only significant in those with nasal obstruction (62% of the cohort). The odds ratio (OR) of an AHI > 15 was 2.45 (95% CI 1.23-4.84) in subjects with nasal obstruction and a Mallampati class III-IV relative to class I-II. There was no increased OR seen in those without nasal obstruction. Yagi et al14 similarly reported a statistically significant correlation between Modified Mallampati class and AHI in 141 patients. Morinaga et al15 from the same institution also reported on the clinical utility of the Modified Mallampati class, but this time assessed the changes in AHI following nasal surgery. This group reported that improvements in AHI were negatively correlated with the Mallampati class, that is, higher degrees of oropharyngeal crowding were associated with lesser changes in AHI after nasal surgery. However, significant correlations do not confer usefulness of this measure in predicting the presence of OSA.
Nuckton et al16 prospectively assessed 137 patients attending a sleep clinic and reported an OR for OSA (defined as an AHI ≥ 5) of 2.5 (95% confidence interval [CI] 1.2-3.2) for each point increase in Mallampati class. The OR for Mallampati class was higher even than for the frequency of witnessed apneas and neck circumference. The authors concluded that the Mallampati class was a useful component of the clinical examination that had clinical value in predicting the presence severity of OSA.
Ramachandran et al17 recently reported on Mallampati class as a component of a multi-variate prediction score derived from a large retrospective cohort of patients undergoing surgery and validated prospectively in a sleep clinic population. Although the primary variable was a multi-variate prediction score, this group reported that Mallampati class III or IV was an independent predictor of an AHI > 5 with a hazard ratio of 2.7 (95% CI 2.5-3.0), which is quite similar to the data of Nuckton.16
The aim of this study was to evaluate the usefulness of Mallampati class in predicting patients with severe OSA (ruling-in severe OSA) and detecting patients without OSA (ruling-out OSA) in a sleep clinic population by assessment of likelihood ratios (LRs). A positive LR (LR+) is the ratio of the likelihood of a positive test result in those with the condition compared to the likelihood of a positive result in those without the condition and is calculated as sensitivity/(1-specificity). Similarly, a negative LR (LR−) is the ratio of the likelihood of a negative result in those with the condition to the likelihood of a negative result in those without the condition and is calculated as (1-sensitivity)/specificity. The value of the LR calculation is expressed in the formulation of Bayes' theorem: Pre-test Probability of Condition x LR = Post-test Probability of Condition.18 LR are therefore useful in assessing the impact of clinical features or test results in clinical decision making. The hypothesis is that higher Mallampati Classes (oropharyngeal crowding) would increase the likelihood of severe OSA and lower classes (less oropharyngeal crowding) would increase the likelihood of excluding OSA.
METHODS
The design of the study was a retrospective cross-sectional review of data from a database of consecutive patients undergoing polysomnography at a tertiary referral sleep disorders center between January 2005 and July 2007. The protocol was approved by the institution's Human Research Ethics Committee. Patients undergoing diagnostic polysomnography had the modified Mallampati class assessed by 1 of 3 sleep physicians at the time of clinical assessment; however, the decision regarding need for polysomnography was not influenced by Mallampati class. Patients who had previously undergone diagnostic polysomnography were not included. Mallampati class was assessed using the technique described by Samsoon and Young (the modified Mallampati class).10 The patient was instructed to maximally open the mouth and extend the tongue without phonation. The oropharynx was inspected with the open mouth at eye level, and the class was assigned according to the closest similarity to a standard chart (Figure 1). Clinical parameters of height, weight, BMI, and gender were recorded. Polysomnography was performed using the Compumedics e-series system (Melbourne, Australia) recording EEG, EOG, nasal pressure, oronasal flow by thermistor, chest and abdominal movement by inductance plethysmography, ECG, submental EMG, pre-tibial EMG, position, and digital video. Sleep staging was performed according to Rechtschaffen and Kales criteria19 and EEG arousals were scored according to published criteria.20 Apneas were defined as a 10-sec absence of flow, and hypopneas as a reduction in any 2 measures of respiration ≥ 10 sec duration associated with EEG arousal or ≥ 3% desaturation.
Statistical Analysis
Data are presented as mean ± standard deviation and as 95% CI. Statistical analysis was performed with SigmaStat Version 3.00 statistical software (SPSS Inc). The relationships between parameters were assessed by linear regression analysis. Multivariate analysis was performed with forward stepwise linear regression. Differences between nonparametric parameters were assessed by Kruskal-Wallis ANOVA on Ranks. The difference in Mallampati class between genders was assessed by χ2 analysis. Sensitivity, specificity, positive and negative predicted values positive and negative likelihood ratios were calculated for the association between Mallampati class IV and an AHI > 30 (the ability to rule in severe OSA) and Mallampati class I and an AHI < 5 (the ability to rule out OSA). The odds ratio (OR) was calculated for each Mallampati class for an AHI ≥ 5 and > 30, using Mallampati class I as the reference. P < 0.05 was considered significant.
RESULTS
Subjects
A total of 1140 patients were eligible for the study, but Mallampati class was not recorded on 187 patients. Therefore 953 (619 male) subjects were included in the study. The age of the cohort was 50.0 ± 6.4 years, and BMI was 33.8 ± 8.6 kg/m2. Average AHI was 26.1 ± 25.1 /h (95% CI: 1.4-78.7 /h). Average Mallampati class was 2.97 ± 0.97. Eighty-five subjects were Mallampati class I, 200 were class II, 328 were class III, and 340 were class IV in appearance.
Relationships with Mallampati Class
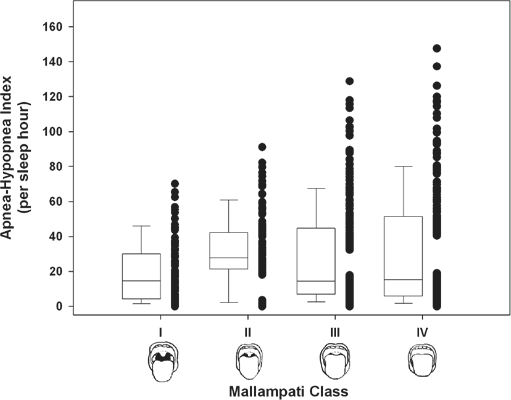
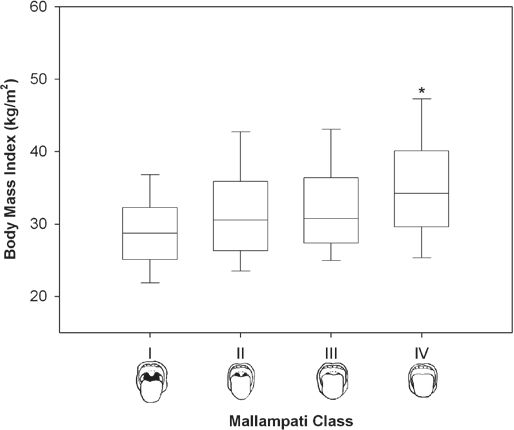
There was no difference in AHI between Mallampati classes (Figure 2). There was a statistically significant relationship between the independent variable of Mallampati class and the dependent variable of AHI (r = 0.13, p < 0.001), but Mallampati class explained only 1.7% of the variability in AHI (r2 = 0.017). Mallampati class was higher in men (3.03 ± 0.96 compared to 2.81 ± 1.01, p < 0.001). Subjects with Mallampati class IV had a higher BMI (Figure 3). Mallampati classes II and III were associated with a significantly increased OR for the presence of OSA (defined as AHI ≥ 5; Table 1), using Mallampati class I as the reference. However, the OR for severe OSA (AHI > 30) was significant only for Mallampati class IV (Table 1).
Figure 2.
Relationship between Mallampati class and AHI
Drawings of Mallamapti class used with permission.10
Figure 3.
Relationship between body mass index and Mallampati class
Drawings of Mallampati class reproduced with permission.10 *p < 0.001 compared to Mallampati class I, II, and III.
Table 1.
Distribution of Mallampati class at Different AHI thresholds (≥ 5 and > 30)
| Mallampati Class | AHI ≥ 5 |
AHI > 30 |
||||||
|---|---|---|---|---|---|---|---|---|
| Proportion with AHI ≥ 5 | OR | (95% CI) | p | Proportion with AHI > 30 | OR | (95% CI) | p | |
| I | 0.73 | 1.00 | - | - | 0.24 | 1.00 | ||
| II | 0.85 | 2.04 | (1.07-3.90) | 0.03 | 0.28 | 1.25 | (0.68-2.31) | 0.54 |
| III | 0.84 | 1.95 | (1.09-3.48) | 0.02 | 0.31 | 1.44 | (0.82-2.54) | 0.23 |
| IV | 0.81 | 1.57 | (0.89-2.77) | 0.13 | 0.35 | 1.75 | (1.01-3.08) | < 0.05 |
Proportion of subjects in each Mallampati class with AHI ≥ 5 and > 30. OR = odds ratio for AHI ≥ 5 and > 30 in each class, with Mallampati class I as the reference (OR = 1).
Other Associations with AHI
AHI was significantly related to BMI (r = 0.25, p < 0.001) but not to age (r = 0.05, p = 0.11). AHI was significantly higher in males (median of 20.2/h compared to 15.8 /h; p < 0.001). AHI was most closely associated with the linear combination of BMI, gender, and age (r = 0.32, p < 0.001); however, the addition of Mallampati class did not improve the association.
Use of Mallampati Class IV to Predict AHI > 30
A total of 297 subjects had severe OSA (AHI > 30). Mallampati class IV was only 40% (95% CI: 36% to 45%) sensitive and 67% (64% to 69%) specific for an AHI > 30. PPV and NPV were 35% (31% to 39%) and 71% (69% to 73%), respectively. The LR+ was 1.21 (1.01-1.44) and LR− 0.90 (0.80-1.00).
Use of Mallampati Class I to Rule Out OSA
There were 178 subjects without OSA (AHI < 5). Mallampati class I was only 13% (8% to 18%) sensitive but 92% (90% to 94%) specific for AHI < 5. PPV and NPV were 27% (18% to 37%) and 82% (80% to 85%), respectively. LR+ was 1.63 (1.03-2.53), and LR− was 0.90 (0.89-1.01).
DISCUSSION
There is evidence that the upper airway size and shape is involved in the pathogenesis of OSA.6–8 The Mallampati class is a simple9,10,13 and reproducible11 technique to assess tongue size and pharyngeal dimensions and has been validated as a tool for assessing risk of difficult intubation.
This study does confirm that Mallampati class is significantly associated with AHI, with the severity of OSA positively correlated with more oropharyngeal “crowding.” However, the Mallampati class only explains 1.7% of the variability in AHI. There was no difference in average AHI between Mallampati classes, but higher Mallampati classes (II and III but not IV) were associated with an increased odds ratio for the presence of OSA (defined as AHI ≥ 5). A Mallampati class of IV was also associated with an increased OR for severe OSA (AHI > 30). However, in multivariate analysis, AHI was best predicted by the linear combination of BMI, gender, and age; the addition of Mallampati class did not improve the closeness of this relationship.
The purpose of the study was to evaluate the utility of the Mallampati class to triage patients referred to a sleep center, either by indicating increased likelihood of severe OSA (ruling in severe OSA) or reducing the likelihood of any OSA (ruling out OSA). Mallampati class IV was associated with an increased OR for AHI > 30 relative to class I. However, the utility of this clinical sign is best represented by the likelihood ratios. A Mallampati class IV had a LR+ of 1.21 (that is, the effect of the presence of Mallampati class IV) and LR− of 0.9 (the effect of the absence of Mallampati class IV). LR has a direct effect on the likelihood of disease as expressed in Bayes' theorem Pre-test Probability of Condition × LR = Post-test Probability of Condition.18 Nomograms are available to demonstrate this relationship.18 An LR+ between 1 and 2 or LR− between 0.5 and 1 have negligible effect on pre-test likelihood of disease, whereas LR+ > 10 and LR− < 0.1 have large effects. Therefore, the presence of Mallampati class IV has limited effect on likelihood of severe OSA. Similarly, a Mallampati class I has a LR+ of 1.63 and LR− of 0.96 for AHI < 5 and has limited use in ruling out OSA in the sleep clinic population.
These data on the surface appear to contradict the findings of Nuckton et al16 who reported an independent association of Mallampati class with the odds of having OSA and with the AHI. The authors felt that Mallampati class had practical value in clinical settings. There were some differences between our cohort and that of Nuckton. Our cohort had a slightly lower male predominance (65% vs 72%), was slightly older (50.0 ± 6.4 vs 46.0 ± 12 years), slightly more obese (BMI 33.8 ± 8.6 vs 31.3 ± 6.9 kg/m2), and had more severe OSA (AHI 26.1 ± 25.1 vs 18.1 ± 24.6). Our cohort also had a higher proportion with OSA in each Mallampati class with OSA as defined by an AHI ≥ 5 (class I 73% vs 33%, class II 85% vs 48%, class III 84% vs 69%, and class IV 81% vs 70%). These differences probably occur as a result of differences in selection bias between the cohorts. Despite the differences, Nuckton reported an LR+ for the presence of OSA (AHI ≥ 5) for class I of 0.4, class II of 0.7, class III of 1.6, and class IV of 1.7, which is very similar to our data. LR+ in these ranges offer negligible effect on pre-test probability for OSA and agree with our data that Mallampati class has little utility in predicting the presence of OSA.
The main weakness of our data is the potential for selection bias. Our data cannot be generalized to populations outside the sleep clinic as the cohort was heavily selected for a high pre-test probability for OSA leading to referral to a sleep center. The need for polysomnography was not affected by Mallampati class. At this institution, 85% to 90% of referrals proceed to polysomnography, illustrating the selected nature of the cohort before inclusion into the study. The purpose of the study was to evaluate the utility of Mallampati class in a selected population of subjects already screened for high likelihood of disease to determine whether this simple clinical sign was useful in screening or triaging subjects for polysomnography. The findings of this study may not be applicable to general population screening where the cohort is less heavily selected than that of the sleep clinic population.
Another weakness of this cohort is the inability to adjust for nasal symptoms which has been suggested as a possible cofactor in the association with sleep apnea.13 Other studies have also suggested that Mallampati class may have a role as part of a broader multivariate prediction score 17 but the retrospective data from this study was limited to inclusion of a small number of clinical variables only.
In summary, Mallampati class IV is not useful in ruling in patients with severe OSA, and Mallampati class I is not useful in ruling out OSA in the sleep clinic population. As such, Mallampati class has no use in triaging patients for urgency for polysomnography based on likelihood of the severity of OSA in those centers where there are delays for polysomnography as a result of the increasing demand on a limited resource.
DISCLOSURE STATEMENT
This was not an industry supported study. The author has indicated no financial conflicts of interest.
REFERENCES
- 1.Young T, Evans L, Finn L, Palta M. Estimation of the clinically diagnosed proportion of sleep apnea syndrome in middle-aged men and women. Sleep. 1997;20:705–6. doi: 10.1093/sleep/20.9.705. [DOI] [PubMed] [Google Scholar]
- 2.Kapur V, Strohl KP, Redline S, Iber C, O'Connor G, Nieto J. Underdiagnosis of sleep apnea syndrome in U.S. communities. Sleep Breath. 2002;6:49–54. doi: 10.1007/s11325-002-0049-5. [DOI] [PubMed] [Google Scholar]
- 3.Flemons WW, Douglas NJ, Kuna ST, Rodenstein DO, Wheatley J. Access to diagnosis and treatment of patients with suspected sleep apnea. Am J Respir Crit Care Med. 2004;169:668–72. doi: 10.1164/rccm.200308-1124PP. [DOI] [PubMed] [Google Scholar]
- 4.Rodsutti J, Hensley M, Thakkinstian A, D'Este C, Attia J. A clinical decision rule to prioritize polysomnography in patients with suspected sleep apnea. Sleep. 2004;27:694–9. doi: 10.1093/sleep/27.4.694. [DOI] [PubMed] [Google Scholar]
- 5.Rowley JA, Aboussouan LS, Badr MS. The use of clinical prediction formulas in the evaluation of obstructive sleep apnea. Sleep. 2000;23:929–38. doi: 10.1093/sleep/23.7.929. [DOI] [PubMed] [Google Scholar]
- 6.Bradley TD, Brown IG, Grossman RF, et al. Pharyngeal size in snorers, nonsnorers, and patients with obstructive sleep apnea. N Engl J Med. 1986;315:1327–31. doi: 10.1056/NEJM198611203152105. [DOI] [PubMed] [Google Scholar]
- 7.Isono S, Remmers JE, Tanaka A, Sho Y, Sato J, Nishino T. Anatomy of pharynx in patients with obstructive sleep apnea and in normal subjects. J Appl Physiol. 1997;82:1319–26. doi: 10.1152/jappl.1997.82.4.1319. [DOI] [PubMed] [Google Scholar]
- 8.White DP. Pathogenesis of obstructive and central sleep apnea. Am J Respir Crit Care Med. 2005;172:1363–70. doi: 10.1164/rccm.200412-1631SO. [DOI] [PubMed] [Google Scholar]
- 9.Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32:429–34. doi: 10.1007/BF03011357. [DOI] [PubMed] [Google Scholar]
- 10.Samsoon GL, Young JR. Difficult tracheal intubation: a retrospective study. Anaesthesia. 1987;42:487–90. doi: 10.1111/j.1365-2044.1987.tb04039.x. [DOI] [PubMed] [Google Scholar]
- 11.Rosenstock C, Gillesberg I, Gatke MR, Levin D, Kristensen MS, Rasmussen LS. Inter-observer agreement of tests used for prediction of difficult laryngoscopy/tracheal intubation. Acta Anaesthesiol Scand. 2005;49:1057–62. doi: 10.1111/j.1399-6576.2005.00792.x. [DOI] [PubMed] [Google Scholar]
- 12.Hiremath AS, Hillman DR, James AL, Noffsinger WJ, Platt PR, Singer SL. Relationship between difficult tracheal intubation and obstructive sleep apnoea. Br J Anaesth. 1998;80:606–11. doi: 10.1093/bja/80.5.606. [DOI] [PubMed] [Google Scholar]
- 13.Liistro G, Rombaux P, Belge C, Dury M, Aubert G, Rodenstein DO. High Mallampati score and nasal obstruction are associated risk factors for obstructive sleep apnoea. Eur Respir J. 2003;21:248–52. doi: 10.1183/09031936.03.00292403. [DOI] [PubMed] [Google Scholar]
- 14.Yagi H, Nakata S, Tsuge H, et al. Morphological examination of upper airway in obstructive sleep apnea. Auris Nasus Larynx. 2009;36:444–9. doi: 10.1016/j.anl.2008.11.003. [DOI] [PubMed] [Google Scholar]
- 15.Morinaga M, Nakata S, Yasuma F, et al. Pharyngeal morphology: a determinant of successful nasal surgery for sleep apnea. Laryngoscope. 2009;119:1011–6. doi: 10.1002/lary.20175. [DOI] [PubMed] [Google Scholar]
- 16.Nuckton TJ, Glidden DV, Browner WS, Claman DM. Physical examination: Mallampati score as an independent predictor of obstructive sleep apnea. Sleep. 2006;29:903–8. doi: 10.1093/sleep/29.7.903. [DOI] [PubMed] [Google Scholar]
- 17.Ramachandran SK, Kheterpal S, Consens F, et al. Derivation and validation of a simple perioperative sleep apnea prediction score. Anesth Analg. 2010;110:1007–15. doi: 10.1213/ANE.0b013e3181d489b0. [DOI] [PubMed] [Google Scholar]
- 18.Gallagher EJ. Clinical utility of likelihood ratios. Ann Emerg Med. 1998;31:391–7. doi: 10.1016/s0196-0644(98)70352-x. [DOI] [PubMed] [Google Scholar]
- 19.Rechtschaffen A, Kales A. Los Angeles: Brain Information Service/Brain Research Institute, UCLA; 1968. A manual of standardized terminology, techniques and scoring system for sleep stages in human subjects. [Google Scholar]
- 20.EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep. 1992;15:173–84. [PubMed] [Google Scholar]