Abstract
Noninvasive ventilation is widely used for chronic respiratory failure in children with neuromuscular disorders, thus avoiding the need for tracheostomy. However, the pressures required to support ventilation in these children may be considerably higher than those necessary to treat obstructive sleep apnea. The complications of nasal positive airway pressure are numerous, including skin breakdown, conjunctivitis, nasal congestion, airway dryness, pneumothorax, and bowel obstruction. Ophthalmologic complaints are particularly common, largely attributed to an air leak in the mask. In the present case, we demonstrate, through two modalities—video and CT scan—retrograde airflow through the nasolacrimal duct causing sleep disruption and eye irritation in a profoundly hypotonic 14-month-old boy with chronic respiratory failure on bilevel ventilation during sleep.
Citation:
Zandieh S; Katz ES. Retrograde lacrimal duct airflow during nasal positive pressure ventilation. J Clin Sleep Med 2010;6(6):603-604.
Keywords: Neuromuscular disorder, continuous positive airway pressure, bilevel positive pressure, pediatrics
Noninvasive ventilation (NIV) is an effective and well-tolerated modality, currently used in approximately 50% of children requiring chronic mechanical respiratory support.1,2 However, compliance may be limited in some patients due to side effects. Ocular complaints with NIV are particularly common, including conjunctivitis, choroidal effusion, corneal erosion, increased ocular pressure, and have been largely attributed to mask leaks or eye compression due to a poorly fitting mask.3 We report a well-documented case of retrograde airflow through the nasolacrimal duct in a profoundly hypotonic child using NIV for chronic respiratory failure. This mechanism may contribute to the high incidence of ocular complaints associated with NIV, even with well fitting nasal interfaces.
REPORT OF CASE
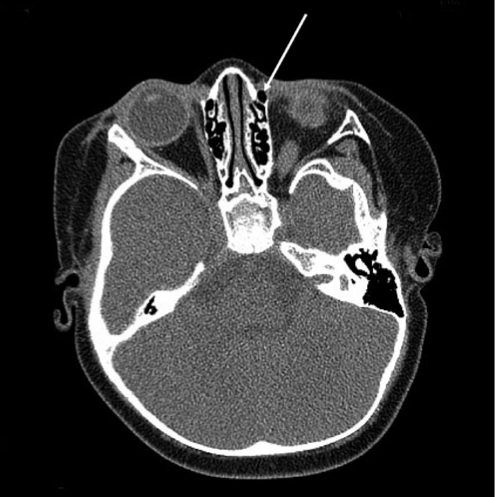
A 14-month-old boy with profound hypotonia of unknown etiology despite an extensive work-up, has been managed since 4 months of age with nasal bilevel positive airway pressure during sleep. The initial polysomnogram, at 4 months, demonstrated excessive periodic breathing, central apneas, and hypercapnia (70 torr). The original bilevel ventilation settings of 10/4, rate 28/minute, in the spontaneous/timed mode were well tolerated for 10 months, with adequate gas exchange. A follow-up bilevel ventilation titration at 14 months of age indicated the need to increase pressures to 15/6. He tolerated these new settings well for approximately 1 month, until his parents began noticing his left eye bulging outward simultaneously with the inspiratory cycle of the bilevel device (see supplemental video online at www.aasmnet.org/jcsm). Sleep disruption was evident during these periods of retrograde airflow through the lacrimal duct. He appeared to rub his eyes frequently during this time and demonstrated photophobia. Flexible nasopharyngoscopy revealed patent choanae bilaterally and a normal nasal pharynx. An orbital and facial computerized tomography (CT) scan showed no skeletal abnormalities, though air was visualized in the nasolacrimal duct (Figure 1). An ophthalmology evaluation found a V-pattern exotropia and amblyopia of the left eye. Subsequently, his bilevel pressures were returned to 10/4 initially, but were gradually increased to 14/4, and his back-up rate was increased to 30/minute. There has been no recurrence of the retrograde airflow or ophthalmologic symptoms after a one year follow-up.
Figure 1.
Axial CT scan image, off bilevel ventilation, at the orbital level in a child, with retrograde airflow through the nasolacrimal duct during nasal positive pressure therapy
The arrow indicates air in the nasolacrimal duct.
DISCUSSION
Ophthalmologic problems are reported in 10% to 30% of patients using NIV. Bacterial conjunctivitis and dry eyes are the most commonly reported ailments.4–6 Other ophthalmologic complications of continuous positive airway pressure (CPAP) include keratoconjunctivitis sicca, corneal abrasion, choroidal effusion, and increased ocular pressure.3 Direct trauma from eye rubbing may give rise to surface inflammation and ischemia.4 Three mechanisms for the eye sequelae from NIV have been postulated: (1) air leak around the superior portion of the mask, resulting in air blowing into the eye; (2) compression of venous drainage from the eye due to pressure from the mask and non-supine positioning; and (3) retrograde movement of air and mucus from the nasal passage through the nasolacrimal duct and into the eye.
NIV through a nasal mask is being increasingly used as a long-term therapy for young children with chronic respiratory failure due to neuromuscular weakness.1 The pressure settings required may be quite a bit higher than those typically required to treat obstructive sleep apnea, resulting in more complications. The present well-documented case of retrograde airflow through the nasolacrimal duct into the eye during positive pressure therapy is the first reported in a child. This complication has been previously described in an adult with Duchenne Muscular Dystrophy who developed keratoconjunctivitis sicca.7 Thus, it is plausible that this complication may be more prevalent in the setting of neuromuscular weakness. Our patient was successfully ventilated through a nasal interface using a lower inspiratory pressure and increased back-up rate, with a resolution of the retrograde nasolacrimal duct airflow. The use of a one-way nasolacrimal valve was reported successful in the previously reported adult case.7
The long-term use of NIV is expanding in patients with chronic respiratory failure, who may require high levels of pressure support. Ophthalmologic complications frequently accompany NIV usage, and clinicians should be aware of the possibility of retrograde nasolacrimal flow in patients with neuromuscular weakness, even with a well fitting mask.
DISCLOSURE STATEMENT
The authors have indicated no financial conflicts of interest.
ABBREVIATIONS
- CPAP
continuous positive airway pressure
- NIV
noninvasive ventilation
- CT
computerized tomography
REFERENCES
- 1.Graham RJ, Fleegler EW, Robinson WM. Chronic ventilator need in the community: a 2005 pediatric census of Massachusetts. Pediatrics. 2007;119:e1280–7. doi: 10.1542/peds.2006-2471. [DOI] [PubMed] [Google Scholar]
- 2.Marcus CL, Rosen G, Ward SL, et al. Adherence to and effectiveness of positive airway pressure therapy in children with obstructive sleep apnea. Pediatrics. 2006;117:e442–51. doi: 10.1542/peds.2005-1634. [DOI] [PubMed] [Google Scholar]
- 3.Waller EA, Bendel RE, Kaplan J. Sleep disorders and the eye. Mayo Clin Proc. 2008;83:1251–61. doi: 10.4065/83.11.1251. [DOI] [PubMed] [Google Scholar]
- 4.Guilleminault C, Nino-Murcia G, Heldt G, Baldwin R, Hutchinson D. Alternative treatment to tracheostomy in obstructive sleep apnea syndrome: nasal continuous positive airway pressure in young children. Pediatrics. 1986;78:797–802. [PubMed] [Google Scholar]
- 5.Kakkar RK, Berry RB. Positive airway pressure treatment for obstructive sleep apnea. Chest. 2007;132:1057–72. doi: 10.1378/chest.06-2432. [DOI] [PubMed] [Google Scholar]
- 6.Nino-Murcia G, McCann CC, Bliwise DL, Guilleminault C, Dement WC. Compliance and side effects in sleep apnea patients treated with nasal continuous positive airway pressure. West J Med. 1989;150:165–9. [PMC free article] [PubMed] [Google Scholar]
- 7.Goktas O, Haberman A, Thelen A, Schrom T. [The punctum plug as an option for treating retrograde air flow from the lacrimal sac] Laryngorhinootologie. 2007;86:732–5. doi: 10.1055/s-2007-966511. [DOI] [PubMed] [Google Scholar]