Abstract
Metabotropic glutamate receptors (mGluRs) are involved in the modulation of synaptic transmission and plasticity. Group II mGluRs in the spinal cord regulate glutamatergic input, but their functional changes in neuropathic pain are not clear. In this study, we determined the plasticity of spinal group II mGluRs in controlling excitatory and inhibitory synaptic transmission and nociception in neuropathic pain. Neuropathic pain was induced by spinal nerve ligation in rats, and whole-cell voltage-clamp recordings of glutamatergic excitatory postsynaptic currents (EPSCs) and spontaneous and miniature GABAergic and glycinergic inhibitory postsynaptic currents (sIPSCs and mIPSCs, respectively) were performed in spinal cord slices. The specific group II mGluR agonist (2S,2′R,3′R)-2-(2′,3′-dicarboxycyclopropyl)glycine (DCG-IV) had a similar inhibitory effect on monosynaptic EPSCs evoked from the dorsal root in sham and nerve-injured rats. However, DCG-IV produced a greater inhibitory effect on evoked polysynaptic EPSCs and the frequency of spontaneous EPSCs in nerve-injured rats than in control rats. Although DCG-IV similarly reduced the frequency of GABAergic sIPSCs and mIPSCs in both groups, it distinctly inhibited the frequency of glycinergic sIPSCs and mIPSCs only in nerve-injured rats. The DCG-IV effect was blocked by the group II mGluR antagonist but not by the N-methyl-d-aspartate receptor antagonist. Strikingly, intrathecal injection of DCG-IV dose-dependently attenuated allodynia and hyperalgesia in nerve-injured rats but produced hyperalgesia in control rats. Our study provides new information that nerve injury up-regulates group II mGluRs present on glutamatergic and glycinergic interneurons in the spinal cord. Activation of group II mGluRs reduces neuropathic pain probably by attenuating glutamatergic and glycinergic input to spinal dorsal horn neurons.
Introduction
Chronic neuropathic pain remains an unmet clinical problem because available treatments have limited efficacy in many patients. Neuropathic pain is typically caused by a lesion or dysfunction of the peripheral or central nervous system. The proposed mechanisms of neuropathic pain include increased primary afferent excitability (Gracely et al., 1992; Matzner and Devor, 1994), increased glutamatergic input to dorsal horn neurons (Kohno et al., 2003; Wang et al., 2007), and diminished GABAergic inhibition caused by a depolarizing shift in the anion gradient of dorsal horn neurons (Coull et al., 2003, 2005). The dorsal horn of the spinal cord is a crucial site for pain transmission and modulation (Cervero and Iggo, 1980). A better understanding of the cellular and molecular mechanisms that regulate the synaptic transmission in the spinal dorsal horn is critical for developing more effective treatments for neuropathic pain.
Increased glutamatergic synaptic inputs to spinal dorsal horn neurons play a pivotal role in the development and maintenance of central sensitization and neuropathic pain conditions (Kohno et al., 2003; Wang et al., 2007; Zhang et al., 2009). Glutamate is a major excitatory neurotransmitter released from primary afferents and interneurons in the spinal cord. Glutamate acts on both ionotropic receptors and metabotropic glutamate receptors (mGluRs). mGluRs are involved in synaptic plasticity at various levels of the nervous system (Anwyl, 1999). Eight mGluRs have been cloned and classified into group I (mGluR1 and mGluR5), group II (mGluR2 and mGluR3), and group III (mGluR4, mGluR6, mGluR7, and mGluR8) (Anwyl, 1999; Schoepp et al., 1999). Group I mGluRs are coupled to Gq/11 proteins, leading to activation of phospholipase C and increased neuronal firing and synaptic transmission. Group II and III mGluRs, however, are typically coupled to inhibitory Gi/o proteins, thereby inhibiting cAMP formation and voltage-gated Ca2+ channels to reduce neuronal excitability and synaptic transmission (Conn and Pin, 1997; Anwyl, 1999). Group II mGluRs (mGluR2/3) are very difficult to separate from each other by using pharmacological approaches, because their proteins share so much sequence similarity. Group II mGluRs are present in the dorsal root ganglion and spinal superficial dorsal horn (Jia et al., 1999; Carlton et al., 2001), and stimulation of these mGluRs in the spinal cord generally depresses synaptic transmission (Gerber et al., 2000; Zhou et al., 2007). We have demonstrated that activation of group I and group III mGluRs has distinct effects on synaptic transmission in the spinal dorsal horn in neuropathic pain (Chen and Pan, 2005; Zhang et al., 2009; Li et al., 2010). In contrast, the nerve injury-induced changes in group II mGluR function in the spinal dorsal horn and their functional significance in neuropathic pain is still not clear.
We, therefore, conducted the present study to determine the functional plasticity of group II mGluRs in the control of excitatory and inhibitory synaptic transmission in the spinal dorsal horn in a rat model of neuropathic pain. Our findings provide new information that nerve injury increases the function of group II mGluRs located on glutamatergic and glycinergic interneurons in the spinal dorsal horn. Furthermore, we found that stimulation of spinal group II mGluRs attenuates neuropathic pain, probably by preferential inhibition of synaptic glutamate and glycine release to dorsal horn neurons.
Materials and Methods
Animal Model of Neuropathic Pain and Intrathecal Cannulation.
Male Sprague-Dawley rats (180–200 g; Harlan, Indianapolis, IN) were used in this study. All surgical preparation and experimental protocols were approved by the Animal Care and Use Committee of the University of Texas MD Anderson Cancer Center and conformed to the National Institutes of Health guidelines for the ethical use of animals. L5 and L6 spinal nerve ligation was used as an experimental model of neuropathic pain in our study (Kim and Chung, 1992). We induced anesthesia with 2 to 3% isoflurane and then isolated the left L5 and L6 spinal nerves and ligated them tightly with 5-0 silk suture. Sham animals used as controls underwent similar surgical procedures except for nerve ligation. In animals used for behavioral studies, intrathecal catheters (PE-10 polyethylene tubing) were implanted 1 week after sham or nerve ligation surgery. The catheters were advanced 8 cm caudally through an incision in the cisternal membrane and secured to the musculature at the incision site. Only animals with no evidence of neurological deficits after catheter insertion were studied. (2S,2′R,3′R)-2-(2′,3′-dicarboxycyclopropyl)glycine (DCG-IV) was administered in a volume of 5 μl followed by a 10-μl flush with normal saline. Final behavioral tests and electrophysiological recordings were performed 3 to 4 weeks after surgery.
Behavioral Assessment of Nociception in Rats.
To quantify tactile allodynia, rats were placed in individual plastic boxes on a mesh floor and allowed to acclimate for 30 to 45 min. A series of calibrated von Frey filaments was applied perpendicularly to the plantar surface of the hindpaw with sufficient force to bend the filaments for 6 s. Brisk paw withdrawal or flinching was considered a positive response. In the absence of a response, the filament of next greater force was applied. If a response occurred, the filament of next lower force was applied. The tactile stimulus producing a 50% likelihood of withdrawal was determined by using the “up-down” calculating method (Chaplan et al., 1997; Chen et al., 2000). Tactile allodynia was confirmed in all rats subjected to spinal nerve ligation.
The paw pressure test was used to quantify the mechanical nociceptive threshold of the hindpaw (mechanical hyperalgesia) (Chen and Pan, 2006; Chen et al., 2009b). Nociceptive thresholds, expressed in grams, were measured with an analgesimeter (Ugo Basile, Varese, Italy). The test was performed by applying a pressure stimulus to the hindpaw. When a pedal that activates a motor was pressed, the force increased on a linear scale at a constant rate. When the animal showed pain by withdrawal of the paw or vocalization, the pedal was released and the nociceptive pain threshold was read on a scale.
Spinal Cord Slice Preparation.
Under 2 to 3% isoflurane anesthesia, the lumbar segment of the spinal cord was removed through laminectomy. The spinal tissue was immediately placed in ice-cold sucrose artificial cerebrospinal fluid (aCSF) presaturated with 95% O2 and 5% CO2. The sucrose aCSF contained 234 mM sucrose, 3.6 mM KCl, 1.2 mM MgCl2, 2.5 mM CaCl2, 1.2 mM NaH2PO4, 12 mM glucose, and 25 mM NaHCO3. The tissue was then placed in a shallow groove formed in a gelatin block and glued onto the stage of a vibratome (Technical Products International, St. Louis, MO). Transverse spinal cord slices (400 μm) were cut in the ice-cold sucrose aCSF and preincubated in Krebs' solution oxygenated with 95% O2 and 5% CO2 at 34°C for at least 1 h before they were transferred to the recording chamber. The Krebs' solution contained 117 mM NaCl, 3.6 mM KCl, 1.2 mM MgCl2, 2.5 mM CaCl2, 1.2 mM NaH2PO4, 11 mM glucose, and 25 mM NaHCO3 gassed with 95% O2/5% CO2.
Electrophysiological Recordings.
Recordings of postsynaptic currents were performed by using the whole-cell voltage-clamp method, as described previously (Zhou et al., 2008a, 2009; Zhang et al., 2009). Each slice was placed in a glass-bottomed chamber and continuously perfused with Krebs' solution at 5.0 ml/min at 34°C maintained by an inline solution heater and a temperature controller. The neurons in lamina II were identified under a fixed-stage microscope (BX50WI; Olympus, Tokyo, Japan) with differential interference contrast/infrared illumination. The electrode for the whole-cell recordings was pulled from borosilicate glass capillaries with a puller (Sutter Instrument Company, Novato, CA). The impedance of the pipette was 5 to 10 MΩ when filled with internal solution for recording excitatory postsynaptic currents (EPSCs) containing 135 mM K-gluconate, 5 mM KCl, 2 mM MgCl2, 0.5 mM CaCl2, 5 mM HEPES, 5 mM EGTA, 5 mM ATP-Mg, 0.5. mM Na-GTP, 1 mM guanosine 5-O-(2-thiodiphosphate) (GDP-β-S), and 10 mM lidocaine N-ethyl bromide (QX314) adjusted to pH 7.2 to 7.4 with 1 M KOH (290–300 mOsm). The impedance of the pipette was 3 to 5 MΩ when filled with internal solution for recording inhibitory postsynaptic currents (IPSCs) containing 110 mM Cs2SO4, 5 mM KCl, 2 mM MgCl2, 0.5 mM CaCl2, 5 mM HEPES, 5 mM EGTA, 5 mM ATP-Mg, 0.5 mM Na-GTP, 1 mM GDP-β-S, and 10 mM QX314 adjusted to pH 7.2 to 7.4 with 1 M CsOH (290–300 mOsm). GDP-β-S was added to the internal solution to block the possible postsynaptic effect of the group II mGluR agonists. QX-314 was added into the internal solution to suppress the action potential generation from the recorded cell.
All recordings were performed on lamina II neurons at the L5 spinal level ipsilateral to the surgery side. The glutamatergic EPSCs were recorded at a holding potential of −60 mV in the presence of 2 μM strychnine and 10 μM bicuculline. Signals were recorded with an amplifier (MultiClamp 700B; Molecular Devices, Sunnyvale, CA), filtered at 1 to 2 kHz, digitized at 10 kHz, and stored into a computer with pCLAMP 9.2 (Molecular Devices). The evoked EPSCs (eEPSCs) of lamina II neurons were induced by electrical stimulation (0.8 mA, 0.2 ms, 0.2 Hz) of the dorsal root (Zhou et al., 2008a; Zhang et al., 2009). Because the retained dorsal root was very short, we did not measure the conduction velocity of afferent fibers stimulated. At the stimulation intensity used, both A- and C-afferent fibers that were in close contact with the electrode tip were stimulated (Wang et al., 2007; Zhou et al., 2010). The eEPSCs were considered monosynaptic if the latency was constant after electrical stimulation (0.2 Hz) and if no conduction failure or increased latency occurred when stimulation frequency was increased to 20 Hz. In contrast, the latency of polysynaptic eEPSCs varied and conduction failure occurred when the stimulation frequency was increased to 20 Hz (Li et al., 2010; Zhou et al., 2010).
GABAergic inhibitory postsynaptic currents (IPSCs) were recorded at a holding potential of 0 mV in the presence of 20 μM 6-cyano-7-nitroquinoxaline-2,3-dione (CNQX) and 2 μM strychnine. Glycinergic sIPSCs were recorded in the presence of 20 μM CNQX and 10 μM bicuculline (Zhou et al., 2007, 2008b). To record the miniature EPSCs (mEPSCs) and miniature IPSCs (mIPSCs), 1 μM tetrodotoxin was added to the perfusion solution.
DCG-IV and (2S)-α-ethylglutamic acid (EGLU) were purchased from Tocris Bioscience (Ellisville, MO). GDP-β-S, strychnine, CNQX, 2-amino-5-phosphonopentanoic acid (AP-5), and bicuculline were obtained from Sigma-Aldrich (St. Louis, MO). Tetrodotoxin and QX314 were obtained from Alomone Labs (Jerusalem, Israel). Drugs were dissolved in Krebs' solution and perfused into the slice chamber by using syringe pumps.
Data Analysis.
Data are presented as the means ± S.E.M. The effects of DCG-IV and EGLU on the paw withdrawal thresholds were compared by using repeated measures analysis of variance followed by Tukey's post hoc test. The sEPSCs, mEPSCs, sIPSCs, and mIPSCs were analyzed off-line with a peak detection program (MiniAnalysis; Synaptosoft, Decatur, GA). Measurements of the amplitude and frequency of sEPSCs, mEPSCs, sIPSCs, and mIPSCs were performed during control, drug application, and recovery. The cumulative probability of the amplitude and interevent interval of sEPSCs, mEPSCs, sIPSCs, and mIPSCs was compared by using the Komogorov-Smirnov test, which estimates the probability that two cumulative distributions are similar. Analyses of the effect of DCG-IV on the amplitude of eEPSCs were performed by using Clampfit 9.2 (Molecular Devices). Neurons were considered to be inhibited by DCG-IV if the amplitude of eEPSCs was reduced >15%. Differences were determined by repeated measures analysis of variance or two-way analysis of variance. P < 0.05 was considered to be statistically significant.
Results
Effect of DCG-IV on Glutamatergic Monosynaptic and Polysynaptic EPSCs in Nerve-Injured Rats.
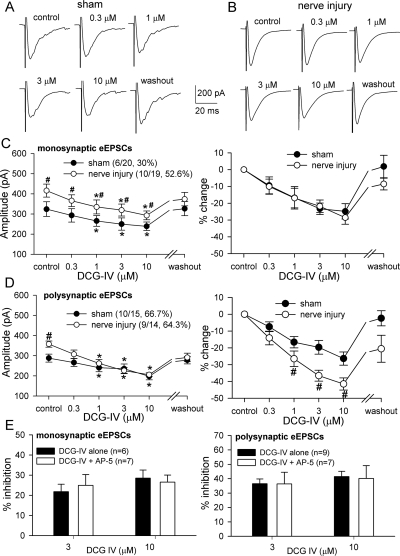
To determine the role of group II mGluRs in the control of glutamatergic input from primary afferents to dorsal horn neurons in sham and nerve-injured rats, we tested the effect of the group II mGluR agonist DCG-IV on monosynaptic eEPSCs elicited from the dorsal root. DCG-IV is a highly specific agonist of mGluR2/3 (Ishida et al., 1993a; Hayashi et al., 1994; Gerber et al., 2000). LY354740 has an affinity in the nanomolar range for group II mGluRs (Schoppa and Westbrook, 1997; Monn et al., 1999; Schoepp et al., 1999). However, we did not choose LY354740 for our study because it has a weak agonist effect on mGluR6 and mGluR8 (Wu et al., 1998; Monn et al., 1999). In nerve-injured rats, the baseline amplitude of monosynaptic eEPSCs of lamina II neurons elicited from the dorsal root (i.e., glutamatergic input from primary afferents) was significantly larger than that in sham rats (415.80 ± 32.58 versus 324.00 ± 36.48 pA; Fig. 1, A–C). Bath application of DCG-IV (1–10 μM, applied for 3 min) significantly reduced the peak amplitude of monosynaptic eEPSCs in a concentration-dependent manner in both sham rats (6 of 20 cells, 30%) and nerve-injured rats (10 of 19 cells, 52.6%; P > 0.05, Fisher's exact test) (Fig. 1, A-C). When the effect of DCG-IV on eEPSCs was normalized to baseline, the degree of inhibition of the amplitude of monosynaptic eEPSCs by DCG-IV was similar in both groups (Fig. 1C). DCG-IV (0.3–10 μM) had no significant effect on monosynaptic eEPSCs in the rest of the neurons tested in either the control group (14 of 20 neurons) or nerve-injured rats (9 of 19 neurons).
Fig. 1.
Effects of DCG-IV on the amplitude of monosynaptic and polysynaptic EPSCs of lamina II neurons evoked from primary afferents in sham and nerve-injured rats. A and B, original traces of monosynaptic eEPSCs of lamina II neurons during control and application of different concentrations of DCG-IV in one sham and one nerve-injured rat. C, summary data showing the inhibitory effect of DCG-IV on the peak amplitude of monosynaptic eEPSCs in sham and nerve-injured rats. D, summary data showing the inhibitory effect of DCG-IV on the peak amplitude of polysynaptic eEPSCs in sham and nerve-injured rats. *, P < 0.05 compared with the baseline control. #, P < 0.05 compared with the corresponding value in the control group. E, comparison of the effects of DCG-IV on monosynaptic and polysynaptic eEPSCs with and without AP-5 (50 μM) in nerve-injured rats. Data are presented as means ± S.E.M.
The baseline amplitude of polysynaptic eEPSCs from the dorsal root (i.e., mixed glutamatergic input from primary afferents and interneurons) was also significantly larger in the nerve-injured group than in the sham group (275.08 ± 22.73 versus 251.03 ± 13.63 pA; Fig. 1D). DCG-IV (1–10 μM) inhibited the amplitude of polysynaptic eEPSCs in a concentration-dependent fashion in both the sham and nerve-ligated rats (Fig. 1D). Although the incidence of inhibition of polysynaptic eEPSCs of lamina II neurons by DCG-IV was similar in the sham (10 of 15 neurons, 66.7%) and nerve-injured (9 of 14 neurons, 64.3%) groups, the magnitude of inhibition of the amplitude of polysynaptic eEPSCs by DCG-IV was significantly greater in nerve-injured rats than in sham control rats (Fig. 1D). At 3 μM, DCG-IV inhibited 36.6 ± 3.3 and 19.7 ± 4.1% of the amplitude of polysynaptic eEPSCs in nerve-injured and control rats, respectively.
Some studies have reported that DCG-IV, at a high concentration, might produce its effect via activation of NMDA receptors (Ishida et al., 1993b; Breakwell et al., 1997). To determine whether NMDA receptors are involved in the inhibitory effect of DCG-IV on synaptic transmission in the spinal cord, we tested the effect of DCG-IV in the presence of AP-5, the specific NMDA receptor antagonist in a separate group of lamina II neurons showing responses to 3 and 10 μM DCG-IV. In the presence of 50 μM AP-5, bath application of DCG-IV inhibited the amplitude of monosynaptic and polysynaptic eEPSCs to a degree that was similar to DCG-IV alone in nerve-injured rats (Fig. 1E). These results suggest that glutamatergic input from primary afferents to spinal dorsal horn neurons is augmented after nerve injury. Furthermore, our data suggest that nerve injury increases the activity of group II mGluRs expressed on glutamatergic interneurons in the spinal dorsal horn.
Effect of DCG-IV on Glutamatergic sEPSCs and mEPSCs in Control and Nerve-Injured Rats.
To further determine the role of group II mGluRs in the control of glutamatergic transmission in the spinal dorsal horn, we examined the effect of DCG-IV on glutamatergic sEPSCs and mEPSCs in lamina II neurons of sham and nerve-injured rats. There were no significant differences in the baseline amplitude (18.81 ± 1.39 versus 19.91 ± 1.45 pA) or frequency (7.54 ± 0.83 versus 7.92 ± 0.34 Hz) of sEPSCs between the sham and nerve-injured groups (Fig. 2, A–E). Bath application of 3 μM DCG-IV for 3 min significantly inhibited the frequency, but not the amplitude, of sEPSCs in all 13 neurons from sham rats and all 16 neurons from nerve-injured rats (Fig. 2, A-F). The cumulative probability analysis of sEPSCs revealed that the distribution pattern of the interevent interval of sEPSCs was shifted toward the right in response to DCG-IV (Fig. 2, C and D). When the effect of DCG-IV on sEPSCs was normalized to baseline, the magnitude of inhibition of the sEPSC frequency by DCG-IV was significantly greater in nerve-injured rats than in sham control rats (Fig. 2F). In sham and nerve-injured groups, bath application of EGLU (200 μM), a highly specific group II mGluR antagonist (Jane et al., 1996; Schoepp et al., 1999), for 3 min alone had no significant effect on sEPSCs. EGLU completely blocked the inhibitory effect of DCG-IV on the frequency of sEPSCs in both groups (n = 5 cells in each group; Fig. 2, A and B). These data provide further evidence that nerve injury increases the activity of group II mGluRs expressed on glutamatergic interneurons in the spinal dorsal horn.
Fig. 2.
Effects of DCG-IV on glutamatergic sEPSCs and mEPSCs of lamina II neurons in sham and nerve-injured rats. A and B, original traces of sEPSCs during control and application of 3 μM DCG-IV, 200 μM EGLU, and EGLU plus DCG-IV in one sham and one nerve-injured rat. C and D, cumulative probability plots of sEPSCs of the same neurons in A and B showing the distribution of the amplitude and interevent interval during control, application of 3 μM DCG-IV, and washout. E and G, summary data showing that 3 μM DCG-IV inhibited the frequency of sEPSCs and mEPSCs in sham and nerve-injured rats. F and H, summary data comparing the percentage inhibition of the frequency of sEPSCs and mEPSCs by DCG-IV in sham and nerve-injured rats. Data are presented as means ± S.E.M. *, P < 0.05 compared with the baseline control or the value in the control group.
There were no significant differences in the baseline amplitude (19.64 ± 1.98 versus 17.47 ± 1.59 pA) or frequency (5.86 ± 0.60 versus 6.09 ± 0.49 Hz) of glutamatergic mEPSCs between the sham and nerve-injured groups (Fig. 2G). Bath application of 3 μM DCG-IV also significantly inhibited the frequency, but not the amplitude, of mEPSCs in all 10 neurons from sham rats and all 10 neurons from nerve-injured rats. The inhibitory effect of DCG-IV on the frequency of mEPSCs was similar in both groups (Fig. 2, G and H).
Effect of DCG-IV on GABAergic sIPSCs and mIPSCs of Lamina II Neurons in Control and Nerve-Injured Rats.
The basal frequency (1.13 ± 0.15 versus 1.25 ± 0.14 Hz) of GABAergic sIPSCs of lamina II neurons in nerve-injured rats was similar to that in sham rats (Fig. 3). However, the amplitude of GABAergic sIPSCs in the nerve-injured group (13.29 ± 0.81 pA) was significantly smaller than that in the sham group (15.86 ± 1.21 pA; Fig. 3F). DCG-IV (0.3–10 μM) decreased the frequency, but not the amplitude, of GABAergic sIPSCs in a concentration-dependent manner in all 10 neurons from the sham control group and all 12 neurons from the nerve-ligated group (Fig. 3E). The cumulative probability analysis of GABAergic sIPSCs revealed that the distribution pattern of the interevent interval of sIPSCs was shifted toward the right in response to DCG-IV. However, the inhibitory effect of DCG-IV on the frequency of GABAergic sIPSCs did not differ significantly between the two groups.
Fig. 3.
Effects of DCG-IV on GABAergic sIPSCs of lamina II neurons in sham and nerve-injured rats. A and B, original traces of GABAergic sIPSCs during control, application of 3 μM DCG-IV, and washout in one sham and one nerve-injured rat. C and D, cumulative probability plots of GABAergic sIPSCs of the same neuron in A and B showing the distribution of the amplitude and interevent interval during control, application of DCG-IV, and washout. E, summary data comparing the baseline frequency and the effect of DCG-IV on the frequency of GABAergic sIPSCs in sham and nerve-injured rats. *, P < 0.05 compared with the baseline control. F, summary data comparing the baseline amplitude and the effect of DCG-IV on the amplitude of GABAergic sIPSCs in sham and nerve-injured rats. #, P < 0.05 compared with the corresponding value in the control group. Data presented are the means ± S.E.M.
The baseline frequency (0.92 ± 0.06 versus 0.96 ± 0.09 Hz) of GABAergic mIPSCs was also similar in sham and nerve-injured rats (Fig. 4). However, the amplitude of GABAergic mIPSCs was significantly reduced in the nerve-injured group (10.59 ± 0.42 pA) compared with that in the sham control group (14.15 ± 1.76 pA) (Fig. 4F). Bath application of 3 μM DCG-IV significantly decreased the frequency, but not the amplitude, of mIPSCs in all nine cells from the sham control group and all 12 cells from the nerve-ligated group (Fig. 4E). The inhibitory effect of DCG-IV on the frequency of GABAergic mIPSCs did not differ significantly between the two groups. It is noteworthy that 3 μM DCG-IV inhibited the frequency of sIPSCs more than that of mIPSCs in both groups. These data suggest that, although nerve injury attenuates GABAergic inhibitory input to spinal dorsal horn neurons, the activity of group II mGluRs expressed on GABAergic interneurons is not altered in this animal model of neuropathic pain.
Fig. 4.
Effects of DCG-IV on GABAergic mIPSCs of lamina II neurons in sham and nerve-injured rats. A and B, original traces of GABAergic mIPSCs during control, application of 3 μM DCG-IV, and washout in one sham and one nerve-injured rat. C and D, cumulative probability plots of GABAergic mIPSCs of the same neuron in A and B showing the distribution of the amplitude and interevent interval during control, application of DCG-IV, and washout. E, summary data comparing the baseline frequency of GABAergic mIPSCs and the effect of 3 μM DCG-IV on the frequency of GABAergic mIPSCs in sham and nerve-injured rats. *, P < 0.05 compared with the baseline control. F, summary data comparing the baseline amplitude and the effect of 3 μM DCG-IV on the amplitude of GABAergic mIPSCs in sham and nerve-injured rats. #, P < 0.05 compared with the corresponding value in the control group. Data are presented as means ± S.E.M.
Effect of DCG-IV on Glycinergic sIPSCs and mIPSCs of Lamina II Neurons in Control and Nerve-Injured Rats.
The baseline frequency of glycinergic sIPSCs of lamina II neurons did not differ significantly between the sham control and nerve-injured groups (Fig. 5). However, the baseline amplitude of glycinergic sIPSCs was significantly reduced in nerve-injured rats compared with that in sham rats (Fig. 5F). DCG-IV (0.3–10 μM) profoundly decreased the frequency, but not the amplitude, of glycinergic sIPSCs in a concentration-dependent manner in all eight cells from the nerve-ligated group (Fig. 5E). In contrast, DCG-IV had no significant effect on glycinergic sIPSCs in all 10 neurons from the sham control group (Fig. 5E). In another group of lamina II neurons in nerve-ligated rats, bath application of 50 μM AP-5 did not affect the inhibitory effect of DCG-IV (3 or 10 μM) on the frequency of glycinergic sIPSCs (Fig. 5F).
Fig. 5.
Effects of DCG-IV on glycinergic sIPSCs of lamina II neurons in sham and nerve-injured rats. A and B, original traces of glycinergic sIPSCs during control, application of 3 μM DCG-IV, and washout in one sham and one nerve-injured rat. C and D, cumulative probability plots of glycinergic sIPSCs of the same neuron in A and B showing the distribution of the amplitude and interevent interval during control, application of DCG-IV, and washout. E, summary data comparing the baseline frequency and amplitude of glycinergic sIPSCs and the effect of DCG-IV on glycinergic sIPSCs in sham and nerve-injured rats. F, summary data comparing the effects of DCG-IV on the frequency of glycinergic sIPSCs with and without 50 μM AP-5 in nerve-injured rats. *, P < 0.05 compared with the baseline control. #, P < 0.05 compared with the corresponding value in the control group. Data are presented as means ± S.E.M.
Furthermore, the frequency of glycinergic mIPSCs of lamina II neurons did not differ significantly between the sham control and nerve-injured groups (Fig. 6). However, the baseline amplitude of glycinergic mIPSCs was significantly reduced in nerve-injured rats compared with that in sham rats (Fig. 6F). Bath application of 3 μM DCG-IV significantly decreased the frequency, but not the amplitude, of mIPSCs in all 11 cells from the nerve-ligated group (Fig. 6E). In contrast, DCG-IV had no significant effect on the frequency or amplitude of glycinergic mIPSCs in all 11 neurons from the sham control group (Fig. 6E). It is noteworthy that DCG-IV (3 μM) reduced the sIPSC frequency more than the frequency of glycinergic mIPSCs in nerve-injured rats (Fig. 5E). These findings suggest that nerve injury reduces glycinergic input to spinal dorsal horn neurons and induces the expression of group II mGluRs on glycinergic interneurons and their terminals in the spinal dorsal horn.
Fig. 6.
Effect of DCG-IV on glycinergic mIPSCs of lamina II neurons in sham rats and nerve-injured rats. A and B, original traces of glycinergic mIPSCs during control, application of DCG-IV, and washout in sham and nerve-injured rats. C and D, cumulative probability plots of glycinergic mIPSCs of the same neuron in A and B showing the distribution of the amplitude and interevent interval during control, application of 3 μM DCG-IV, and washout. E, summary data comparing the baseline frequency of glycinergic mIPSCs and the effect of DCG-IV on the frequency of glycinergic mIPSCs in sham and nerve-injured rats. *, P < 0.05 compared with the baseline control. F, summary data comparing the baseline amplitude and the effect of 3 μM DCG-IV on the amplitude of glycinergic mIPSCs in sham and nerve-injured rats. #, P < 0.05 compared with the corresponding value in the control group. Data presented are the means ± S.E.M.
Effect of Intrathecal Injection of DCG-IV on Tactile Allodynia and Hyperalgesia in Nerve-Injured Rats.
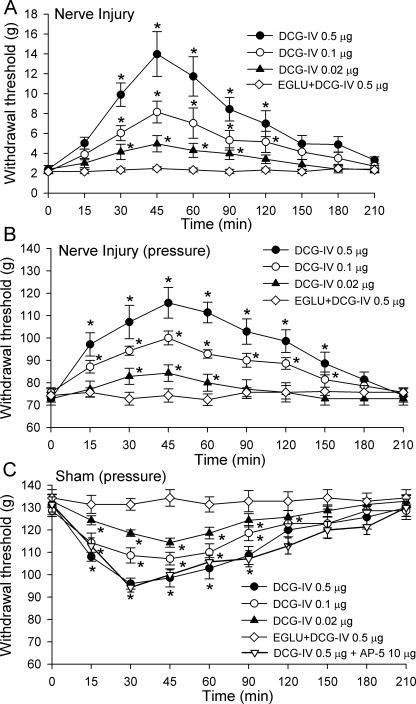
To determine how group II mGluR stimulation affects nociceptive transmission at the spinal level, we compared the potential antinociceptive effects of intrathecal injection of DCG-IV in control and nerve-injured rats. Intrathecal injection of 0.02 to 0.5 μg of DCG-IV significantly increased the paw withdrawal threshold in response to application of von Frey filaments in nerve-ligated rats in a dose-dependent manner (n = 7 rats in each dose group; Fig. 7A). These doses of DCG-IV were selected in our preliminary experiments. The maximal effect of DCG-IV appeared within 30 min and gradually subsided within 150 min after intrathecal administration. To ensure the specific effect of DCG-IV on group II mGluRs, EGLU (10 μg), a specific antagonist for group II mGluRs, was given intrathecally 15 min before 0.5 μg of DCG-IV was injected in another seven rats. Intrathecal injection of 10 μg of EGLU did not significantly change the baseline withdrawal threshold (data not shown). EGLU abolished the effect of DCG-IV on tactile allodynia in nerve-injured rats (Fig. 7A).
Fig. 7.
Time course of the effect of intrathecal injection of DCG-IV on the paw withdrawal thresholds in sham and nerve-injured rats. A, effect of intrathecal injection of DCG-IV on tactile allodynia measured with von Frey filaments in nerve-injured rats. B, effect of intrathecal injection of DCG-IV on hyperalgesia tested with a noxious pressure stimulus in nerve-injured rats. C, effect of intrathecal injection of DCG-IV on the nociceptive withdrawal threshold in response to a noxious pressure stimulus in sham control rats. Intrathecal pretreatment with 10 μg of EGLU abolished the effect of DCG-IV on the paw withdrawal thresholds in both sham and nerve-injured rats. Note that intrathecal pretreatment with 10 μg of AP-5 did not alter the effect of DCG-IV (0.5 μg) on the withdrawal threshold in sham control rats. Data presented as mean ± S.E.M. (n = 7 rats in each dose group). *, P < 0.05 compared with the respective baseline control (time 0).
Intrathecal administration of DCG-IV also dose-dependently increased the paw withdrawal threshold in response to the noxious pressure stimulus in nerve-injured rats (Fig. 7B). We were surprised to find that intrathecal injection of DCG-IV significantly reduced the pressure withdrawal threshold in sham rats in a dose-dependent manner (Fig. 7C). In both groups, the peak effect of DCG-IV appeared within 30 min after intrathecal injection, and the effect lasted for approximately 150 min. Intrathecal pretreatment with 10 μg of EGLU completely blocked the effect of 0.5 μg of DCG-IV on the pressure withdrawal threshold in both sham and nerve-injured rats (Fig. 7, B and C). In addition, to determine whether the pronociceptive effect of DCG-IV resulted from NMDA receptor activation in sham control rats, we examined the effect of DCG-IV in the presence of the NMDA receptor antagonist AP-5 in another seven sham rats. In this protocol, we injected 10 μg of AP-5 intrathecally 15 min before administration of 0.5 μg of DCG-IV. Intrathecal injection of 0.5 μg of DCG-IV similarly reduced the pressure withdrawal threshold in the presence of AP-5 (Fig. 7C).
Discussion
In this study, we determined the functional plasticity of spinal group II mGluRs in the regulation of excitatory and inhibitory synaptic transmission in neuropathic pain. We found that the amplitude of monosynaptic and polysynaptic eEPSCs evoked from primary afferents was significantly larger in spinal nerve-injured rats than in control rats. This finding suggests that nerve injury increases the glutamatergic input from primary afferents to spinal dorsal horn neurons. Our results are consistent with previous studies showing augmented glutamatergic input from primary afferents in neuropathic pain induced by nerve ligation and diabetic neuropathy in rats (Kohno et al., 2003; Wang et al., 2007; Zhang et al., 2009). The study by Moore et al. (2002) did not find any difference in the amplitude of primary afferent-evoked EPSCs of lamina II neurons in their nerve injury models. However, there are some major technical differences between their studies and ours (e.g., suction versus bipolar electrode, long versus short dorsal root, blind versus visualized recording, and recording at L4 versus L5/L6 levels). Increased excitability of primary afferent nerves and ectopic discharges from injured afferent nerves (Gracely et al., 1992; Matzner and Devor, 1994) can result in enhanced glutamatergic input from primary afferents. In addition, nerve injury reduces the expression and activity of voltage-activated and Ca2+-activated K+ channels in primary sensory neurons (Everill and Kocsis, 1999; Kim et al., 2002; Sarantopoulos et al., 2007; Chen et al., 2009a).
GABA and glycine are the two major inhibitory neurotransmitters in the normal spinal cord. Reduced GABA- and glycine-mediated inhibition (disinhibition) may also contribute to the hyperexcitability of spinal dorsal horn neurons and pain sensitivity. For instance, blocking spinal GABAA receptors produces tactile allodynia in rats (Sorkin et al., 1998). In addition, blockade of glycine receptors in the spinal cord leads to hypersensitivity of spinal dorsal horn neurons and allodynia in rats (Yaksh, 1989). We found that the baseline amplitude, but not the frequency, of GABAergic and glycinergic sIPSCs and mIPSCs was significantly smaller in nerve-injured rats than in control rats. In addition, the reduction in the amplitude of glycinergic IPSCs seemed to be greater than that of GABAergic IPSCs in the spinal cord of nerve-injured rats. Some studies reported that the number of GABA-immunoreactive neurons in the spinal dorsal horn is reduced after nerve injury (Castro-Lopes et al., 1993; Ibuki et al., 1997; Moore et al., 2002). However, other studies have shown that nerve injury does not cause any significant loss of GABAergic and glycinergic neurons in the spinal dorsal horn (Polgár et al., 2003, 2005; Hermanns et al., 2009).
Whereas ionotropic glutamate receptors are responsible for fast excitatory synaptic transmission, mGluRs have an important role in synaptic modulation throughout the central nervous system. Activation of group II mGluRs generally depresses glutamatergic and GABAergic transmission in the normal spinal cord (Gerber et al., 2000; Zhou et al., 2007), but the functional plasticity of spinal group II mGluRs in the regulation of synaptic transmission in neuropathic pain remains unclear. It has been shown that systemic administration of the group II mGluR agonist (2R,4R)-aminopyrrolidine-2,4-dicarboxylate attenuates tactile allodynia induced by nerve injury in rats (Fisher et al., 2002). Others have reported that although intraperitoneal injection of the group II mGluR agonist (1S,2R,5R,6R)-2-amino-4-oxabicyclo[3.1.0]hexane-2,6-dicarboxylic acid (LY379268) reduces allodynia, it has no significant effect on heat and mechanical hyperalgesia induced by spinal nerve ligation in rats (Simmons et al., 2002). However, the direct spinal effects of the group II mGluR agonists on neuropathic pain and the associated underlying synaptic mechanisms remain to be investigated. We found that spinally administered DCG-IV dose-dependently attenuated allodynia and hyperalgesia in nerve-injured rats. Unexpectedly, we found that DCG-IV dose-dependently decreased the paw withdrawal threshold in response to noxious mechanical stimulus (i.e., hyperalgesia) in control rats. In addition to their presence on primary afferent terminals (Gerber et al., 2000; Carlton et al., 2001), group II mGluRs exist on GABAergic interneurons in the spinal cord (Zhou et al., 2007). The inhibitory effect of the group II mGluR agonist on GABAergic inhibitory input to spinal dorsal horn neurons may explain the pronociceptive effect of DCG-IV in control animals. DCG-IV produced a similar degree of inhibition of the monosynaptic eEPSCs evoked from the dorsal root in nerve-injured and control rats, suggesting that peripheral nerve injury had no significant effect on the function of group II mGluRs expressed on primary afferent terminals. However, DCG-IV had a significantly greater inhibitory effect on polysynaptic eEPSCs and sEPSCs in nerve-injured rats than in control rats. Our results are consistent with a study showing that the group II mGluR agonist reduces noxious stimulus-evoked glutamate release, measured using microdialysis and high-performance liquid chromatography techniques, in the spinal cord of rats with neuropathic pain (Kumar et al., 2010). It should be noted that potential changes in postsynaptic group II mGluRs in neuropathic pain cannot be ruled out because of the use of GDP-β-S in the internal recording solution in our experiments. Our study suggests that activation of group II mGluRs inhibits nociceptive transmission by reducing glutamatergic input to spinal dorsal horn neurons in a neuropathic pain state.
Another salient finding of our study is that stimulation of group II mGluRs with DCG-IV decreased the frequency of glycinergic sIPSCs and mIPSCs of dorsal horn neurons only in nerve-injured rats. We also found that DCG-IV produced much larger inhibition of glycinergic sIPSCs than glycinergic mIPSCs in nerve-injured rats. Thus, it seems that nerve injury up-regulates group II mGluRs on both somatodentritic sites and presynaptic terminals of glycinergic interneurons in the spinal dorsal horn. The mechanisms underlying the distinct effect of the group II mGluRs on glycinergic input in nerve-injured rats are not clear. It is possible that nerve injury may selectively up-regulate group II mGluRs on a subpopulation of GABAergic-glycinergic interneurons in the spinal cord through increased excitability of a particular group of primary afferents (Lu and Perl, 2003). Immunocytochemical results suggest that GABA- and glycine-like immunoreactivities are often colocalized in the spinal dorsal horn (Todd and Sullivan, 1990; Todd, 1996). However, corelease of GABA and glycine from the same synaptic terminal in the superficial dorsal horn seems rare because direct paired recordings of dorsal horn neurons show that the IPSCs evoked from a single presynaptic terminal are mediated by either GABAA or glycine receptors but not by both (Lu and Perl, 2003; Santos et al., 2007). In addition, our previous studies have shown that muscarinic receptor subtypes and group II and III mGluRs are differentially involved in the control of GABAergic and glycinergic input in the spinal dorsal horn (Zhang et al., 2005; Wang et al., 2006; Zhou et al., 2007, 2008b). It has been shown that down-regulation of the K+/Cl− cotransporter-2 and an increase in intracellular chloride concentrations of dorsal horn neurons after sciatic nerve injury can lead to paradoxical excitation and increased firing activity of dorsal horn neurons in response to GABA (Coull et al., 2003). Hence, inhibition of abnormal GABAergic and glycinergic input by activation of group II mGluRs may reduce paradoxical excitation of spinal dorsal horn neurons by GABA and glycine to reduce neuropathic pain. Nevertheless, it is not certain whether the inhibitory effect of DCG-IV on GABAergic and glycinergic input to dorsal horn neurons contributes to the antinociceptive effect of spinally administered DCG-IV on neuropathic pain. In addition, because glycine is a coagonist of NMDA receptors, reduced synaptic glycine release by activation of group II mGluRs may attenuate neuropathic pain by inhibiting the activity of NMDA receptors in the spinal cord induced by nerve injury.
It has been reported that higher concentrations of DCG-IV could stimulate NMDA receptors (Ishida et al., 1993b; Breakwell et al., 1997). Because activation of presynaptic NMDA receptors increases neurotransmitter release in the spinal cord (Liu et al., 1997; Zhou et al., 2010), the inhibitory effects of DCG-IV on synaptic transmission observed in our study cannot be explained by its effect on NMDA receptors. In addition, it has been shown that 5 μM DCG-IV does not produce any significant change in intracellular Ca2+ in all superficial dorsal horn neurons in rats (Heinke and Sandkuhler, 2007), suggesting that this concentration of DCG-IV does not activate NMDA receptors in the spinal dorsal horn. Nevertheless, it could be argued that the observed pronociceptive effect of DCG-IV in sham control rats may result from stimulation of NMDA receptors. However, we found that blocking the NMDA receptors with AP-5 did not affect the spinal effect of DCG-IV on the pressure withdrawal threshold in sham control rats. Furthermore, we found that AP-5 failed to alter the inhibitory effects of DCG-IV on monosynaptic and polysynaptic eEPSCs and glycinergic sIPSCs in nerve-injured rats. Therefore, the spinal effects of DCG-IV on synaptic transmission and nociception observed in our study are unlikely to be caused by the activation of NMDA receptors.
In summary, we demonstrated in this study that activation of group II mGluRs at the spinal level produces a distinct effect on nociception in control and nerve-injured rats. Our findings suggest that nerve injury up-regulates group II mGluRs present on glutamatergic and glycinergic interneurons in the spinal dorsal horn in neuropathic pain. Therefore, activation of group II mGluRs could reduce neuropathic pain by selectively attenuating glutamatergic input and synaptic glycine release to spinal dorsal horn neurons. Our findings provide new information about the plasticity of group II mGluRs in the spinal dorsal horn in neuropathic pain. These functional changes in group II mGluRs provide a rationale for the use of spinally administered group II mGluR agonists to treat neuropathic pain.
This study was supported by the National Institutes of Health National Institute of General Medical Sciences [Grant GM64830], the National Institutes of Health National Institute of Neurological Disorders and Stroke [Grant NS45602], and the N.G. and Helen T. Hawkins Endowment (to H.L.P.).
Article, publication date, and citation information can be found at http://jpet.aspetjournals.org.
doi:11.1124/jpet.110.173112.
- mGluR
- metabotropic glutamate receptor
- EPSC
- excitatory postsynaptic current
- eEPSC
- evoked EPSC
- mEPSC
- miniature EPSC
- IPSC
- inhibitory postsynaptic current
- sIPSC
- spontaneous IPSC
- mIPSC
- miniature IPSC
- DCG-IV
- (2S,2′R,3′R)-2-(2′,3′-dicarboxycyclopropyl)glycine
- EGLU
- (2S)-α-ethylglutamic acid
- GDP-β-S
- guanosine 5′-O-(2-thiodiphosphate)
- CNQX
- 6-cyano-7-nitroquinoxaline-2,3-dione
- AP-5
- 2-amino-5-phosphonopentanoic acid
- NMDA
- N-methyl-d-aspartate
- LY379268
- (1S,2R,5R,6R)-2-amino-4-oxabicyclo[3.1.0]hexane-2,6-dicarboxylic acid
- QX314
- lidocaine N-ethyl bromide
- aCSF
- artificial cerebrospinal fluid.
Authorship Contributions
Participated in research design: Zhou, S.-R. Chen, and Pan.
Conducted experiments: Zhou, S.-R. Chen, and H. Chen.
Wrote or contributed to the writing of the manuscript: Zhou and Pan.
References
- Anwyl R. (1999) Metabotropic glutamate receptors: electrophysiological properties and role in plasticity. Brain Res Brain Res Rev 29:83–120 [DOI] [PubMed] [Google Scholar]
- Breakwell NA, Huang L, Rowan MJ, Anwyl R. (1997) DCG-IV inhibits synaptic transmission by activation of NMDA receptors in area CA1 of rat hippocampus. Eur J Pharmacol 322:173–178 [DOI] [PubMed] [Google Scholar]
- Carlton SM, Hargett GL, Coggeshall RE. (2001) Localization of metabotropic glutamate receptors 2/3 on primary afferent axons in the rat. Neuroscience 105:957–969 [DOI] [PubMed] [Google Scholar]
- Castro-Lopes JM, Tavares I, Coimbra A. (1993) GABA decreases in the spinal cord dorsal horn after peripheral neurectomy. Brain Res 620:287–291 [DOI] [PubMed] [Google Scholar]
- Cervero F, Iggo A. (1980) The substantia gelatinosa of the spinal cord: a critical review. Brain 103:717–772 [DOI] [PubMed] [Google Scholar]
- Chaplan SR, Malmberg AB, Yaksh TL. (1997) Efficacy of spinal NMDA receptor antagonism in formalin hyperalgesia and nerve injury evoked allodynia in the rat. J Pharmacol Exp Ther 280:829–838 [PubMed] [Google Scholar]
- Chen SR, Pan HL. (2005) Distinct roles of group III metabotropic glutamate receptors in control of nociception and dorsal horn neurons in normal and nerve-injured Rats. J Pharmacol Exp Ther 312:120–126 [DOI] [PubMed] [Google Scholar]
- Chen SR, Pan HL. (2006) Loss of TRPV1-expressing sensory neurons reduces spinal mu opioid receptors but paradoxically potentiates opioid analgesia. J Neurophysiol 95:3086–3096 [DOI] [PubMed] [Google Scholar]
- Chen SR, Cai YQ, Pan HL. (2009a) Plasticity and emerging role of BKCa channels in nociceptive control in neuropathic pain. J Neurochem 110:352–362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen SR, Eisenach JC, McCaslin PP, Pan HL. (2000) Synergistic effect between intrathecal non-NMDA antagonist and gabapentin on allodynia induced by spinal nerve ligation in rats. Anesthesiology 92:500–506 [DOI] [PubMed] [Google Scholar]
- Chen SR, Samoriski G, Pan HL. (2009b) Antinociceptive effects of chronic administration of uncompetitive NMDA receptor antagonists in a rat model of diabetic neuropathic pain. Neuropharmacology 57:121–126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conn PJ, Pin JP. (1997) Pharmacology and functions of metabotropic glutamate receptors. Annu Rev Pharmacol Toxicol 37:205–237 [DOI] [PubMed] [Google Scholar]
- Coull JA, Beggs S, Boudreau D, Boivin D, Tsuda M, Inoue K, Gravel C, Salter MW, De Koninck Y. (2005) BDNF from microglia causes the shift in neuronal anion gradient underlying neuropathic pain. Nature 438:1017–1021 [DOI] [PubMed] [Google Scholar]
- Coull JA, Boudreau D, Bachand K, Prescott SA, Nault F, Sík A, De Koninck P, De Koninck Y. (2003) Trans-synaptic shift in anion gradient in spinal lamina I neurons as a mechanism of neuropathic pain. Nature 424:938–942 [DOI] [PubMed] [Google Scholar]
- Everill B, Kocsis JD. (1999) Reduction in potassium currents in identified cutaneous afferent dorsal root ganglion neurons after axotomy. J Neurophysiol 82:700–708 [DOI] [PubMed] [Google Scholar]
- Fisher K, Lefebvre C, Coderre TJ. (2002) Antinociceptive effects following intrathecal pretreatment with selective metabotropic glutamate receptor compounds in a rat model of neuropathic pain. Pharmacol Biochem Behav 73:411–418 [DOI] [PubMed] [Google Scholar]
- Gerber G, Zhong J, Youn D, Randic M. (2000) Group II and group III metabotropic glutamate receptor agonists depress synaptic transmission in the rat spinal cord dorsal horn. Neuroscience 100:393–406 [DOI] [PubMed] [Google Scholar]
- Gracely RH, Lynch SA, Bennett GJ. (1992) Painful neuropathy: altered central processing maintained dynamically by peripheral input. Pain 51:175–194 [DOI] [PubMed] [Google Scholar]
- Hayashi Y, Sekiyama N, Nakanishi S, Jane DE, Sunter DC, Birse EF, Udvarhelyi PM, Watkins JC. (1994) Analysis of agonist and antagonist activities of phenylglycine derivatives for different cloned metabotropic glutamate receptor subtypes. J Neurosci 14:3370–3377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinke B, Sandkühler J. (2007) Group I metabotropic glutamate receptor-induced Ca(2+)-gradients in rat superficial spinal dorsal horn neurons. Neuropharmacology 52:1015–1023 [DOI] [PubMed] [Google Scholar]
- Hermanns H, Muth-Selbach U, Lipfert P, Braun S, Werdehausen R, Bauer I. (2009) Loss of spinal glycinergic neurons is not necessary for development of neuropathic pain in transgenic mice expressing enhanced green fluorescent protein in glycinergic neurons. Neuroscience 159:1148–1153 [DOI] [PubMed] [Google Scholar]
- Ibuki T, Hama AT, Wang XT, Pappas GD, Sagen J. (1997) Loss of GABA-immunoreactivity in the spinal dorsal horn of rats with peripheral nerve injury and promotion of recovery by adrenal medullary grafts. Neuroscience 76:845–858 [DOI] [PubMed] [Google Scholar]
- Ishida M, Saitoh T, Shinozaki H. (1993a) A new metabotropic glutamate receptor agonist: developmental change of its sensitivity to receptors in the newborn rat spinal cord. Neurosci Lett 160:156–158 [DOI] [PubMed] [Google Scholar]
- Ishida M, Saitoh T, Shimamoto K, Ohfune Y, Shinozaki H. (1993b) A novel metabotropic glutamate receptor agonist: marked depression of monosynaptic excitation in the newborn rat isolated spinal cord. Br J Pharmacol 109:1169–1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jane DE, Thomas NK, Tse HW, Watkins JC. (1996) Potent antagonists at the L-AP4- and (1S,3S)-ACPD-sensitive presynaptic metabotropic glutamate receptors in the neonatal rat spinal cord. Neuropharmacology 35:1029–1035 [DOI] [PubMed] [Google Scholar]
- Jia H, Rustioni A, Valtschanoff JG. (1999) Metabotropic glutamate receptors in superficial laminae of the rat dorsal horn. J Comp Neurol 410:627–642 [PubMed] [Google Scholar]
- Kim DS, Choi JO, Rim HD, Cho HJ. (2002) Down-regulation of voltage-gated potassium channel alpha gene expression in dorsal root ganglia following chronic constriction injury of the rat sciatic nerve. Brain Res Mol Brain Res 105:146–152 [DOI] [PubMed] [Google Scholar]
- Kim SH, Chung JM. (1992) An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain 50:355–363 [DOI] [PubMed] [Google Scholar]
- Kohno T, Moore KA, Baba H, Woolf CJ. (2003) Peripheral nerve injury alters excitatory synaptic transmission in lamina II of the rat dorsal horn. J Physiol 548:131–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar N, Laferriere A, Yu JS, Poon T, Coderre TJ. (2010) Metabotropic glutamate receptors (mGluRs) regulate noxious stimulus-induced glutamate release in the spinal cord dorsal horn of rats with neuropathic and inflammatory pain. J Neurochem 114:281–290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li JQ, Chen SR, Chen H, Cai YQ, Pan HL. (2010) Regulation of increased glutamatergic input to spinal dorsal horn neurons by mGluR5 in diabetic neuropathic pain. J Neurochem 112:162–172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H, Mantyh PW, Basbaum AI. (1997) NMDA-receptor regulation of substance P release from primary afferent nociceptors. Nature 386:721–724 [DOI] [PubMed] [Google Scholar]
- Lu Y, Perl ER. (2003) A specific inhibitory pathway between substantia gelatinosa neurons receiving direct C-fiber input. J Neurosci 23:8752–8758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matzner O, Devor M. (1994) Hyperexcitability at sites of nerve injury depends on voltage-sensitive Na+ channels. J Neurophysiol 72:349–359 [DOI] [PubMed] [Google Scholar]
- Monn JA, Valli MJ, Massey SM, Hansen MM, Kress TJ, Wepsiec JP, Harkness AR, Grutsch JL, Jr, Wright RA, Johnson BG, et al. (1999) Synthesis, pharmacological characterization, and molecular modeling of heterobicyclic amino acids related to (+)-2-aminobicyclo[3.1.0]hexane-2,6-dicarboxylic acid (LY354740): identification of two new potent, selective, and systemically active agonists for group II metabotropic glutamate receptors. J Med Chem 42:1027–1040 [DOI] [PubMed] [Google Scholar]
- Moore KA, Kohno T, Karchewski LA, Scholz J, Baba H, Woolf CJ. (2002) Partial peripheral nerve injury promotes a selective loss of GABAergic inhibition in the superficial dorsal horn of the spinal cord. J Neurosci 22:6724–6731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polgár E, Hughes DI, Arham AZ, Todd AJ. (2005) Loss of neurons from laminas I-III of the spinal dorsal horn is not required for development of tactile allodynia in the spared nerve injury model of neuropathic pain. J Neurosci 25:6658–6666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polgár E, Hughes DI, Riddell JS, Maxwell DJ, Puskár Z, Todd AJ. (2003) Selective loss of spinal GABAergic or glycinergic neurons is not necessary for development of thermal hyperalgesia in the chronic constriction injury model of neuropathic pain. Pain 104:229–239 [DOI] [PubMed] [Google Scholar]
- Santos SF, Rebelo S, Derkach VA, Safronov BV. (2007) Excitatory interneurons dominate sensory processing in the spinal substantia gelatinosa of rat. J Physiol 581:241–254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarantopoulos CD, McCallum JB, Rigaud M, Fuchs A, Kwok WM, Hogan QH. (2007) Opposing effects of spinal nerve ligation on calcium-activated potassium currents in axotomized and adjacent mammalian primary afferent neurons. Brain Res 1132:84–99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoepp DD, Jane DE, Monn JA. (1999) Pharmacological agents acting at subtypes of metabotropic glutamate receptors. Neuropharmacology 38:1431–1476 [DOI] [PubMed] [Google Scholar]
- Schoppa NE, Westbrook GL. (1997) Modulation of mEPSCs in olfactory bulb mitral cells by metabotropic glutamate receptors. J Neurophysiol 78:1468–1475 [DOI] [PubMed] [Google Scholar]
- Simmons RM, Webster AA, Kalra AB, Iyengar S. (2002) Group II mGluR receptor agonists are effective in persistent and neuropathic pain models in rats. Pharmacol Biochem Behav 73:419–427 [DOI] [PubMed] [Google Scholar]
- Sorkin LS, Puig S, Jones DL. (1998) Spinal bicuculline produces hypersensitivity of dorsal horn neurons: effects of excitatory amino acid antagonists. Pain 77:181–190 [DOI] [PubMed] [Google Scholar]
- Todd AJ. (1996) GABA and glycine in synaptic glomeruli of the rat spinal dorsal horn. Eur J Neurosci 8:2492–2498 [DOI] [PubMed] [Google Scholar]
- Todd AJ, Sullivan AC. (1990) Light microscope study of the coexistence of GABA-like and glycine-like immunoreactivities in the spinal cord of the rat. J Comp Neurol 296:496–505 [DOI] [PubMed] [Google Scholar]
- Wang XL, Zhang HM, Chen SR, Pan HL. (2007) Altered synaptic input and GABAB receptor function in spinal superficial dorsal horn neurons in rats with diabetic neuropathy. J Physiol 579:849–861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang XL, Zhang HM, Li DP, Chen SR, Pan HL. (2006) Dynamic regulation of glycinergic input to spinal dorsal horn neurones by muscarinic receptor subtypes in rats. J Physiol 571:403–413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S, Wright RA, Rockey PK, Burgett SG, Arnold JS, Rosteck PR, Jr, Johnson BG, Schoepp DD, Belagaje RM. (1998) Group III human metabotropic glutamate receptors 4, 7 and 8: molecular cloning, functional expression, and comparison of pharmacological properties in RGT cells. Brain Res Mol Brain Res 53:88–97 [DOI] [PubMed] [Google Scholar]
- Yaksh TL. (1989) Behavioral and autonomic correlates of the tactile evoked allodynia produced by spinal glycine inhibition: effects of modulatory receptor systems and excitatory amino acid antagonists. Pain 37:111–123 [DOI] [PubMed] [Google Scholar]
- Zhang HM, Chen SR, Pan HL. (2009) Effects of activation of group III metabotropic glutamate receptors on spinal synaptic transmission in a rat model of neuropathic pain. Neuroscience 158:875–884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang HM, Li DP, Chen SR, Pan HL. (2005) M2, M3, and M4 receptor subtypes contribute to muscarinic potentiation of GABAergic inputs to spinal dorsal horn neurons. J Pharmacol Exp Ther 313:697–704 [DOI] [PubMed] [Google Scholar]
- Zhou HY, Chen SR, Chen H, Pan HL. (2008a) Sustained inhibition of neurotransmitter release from nontransient receptor potential vanilloid type 1-expressing primary afferents by mu-opioid receptor activation-enkephalin in the spinal cord. J Pharmacol Exp Ther 327:375–382 [DOI] [PubMed] [Google Scholar]
- Zhou HY, Chen SR, Chen H, Pan HL. (2009) The glutamatergic nature of TRPV1-expressing neurons in the spinal dorsal horn. J Neurochem 108:305–318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou HY, Chen SR, Chen H, Pan HL. (2010) Opioid-induced long-term potentiation in the spinal cord is a presynaptic event. J Neurosci 30:4460–4466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou HY, Zhang HM, Chen SR, Pan HL. (2007) Increased nociceptive input rapidly modulates spinal GABAergic transmission through endogenously released glutamate. J Neurophysiol 97:871–882 [DOI] [PubMed] [Google Scholar]
- Zhou HY, Zhang HM, Chen SR, Pan HL. (2008b) Increased C-fiber nociceptive input potentiates inhibitory glycinergic transmission in the spinal dorsal horn. J Pharmacol Exp Ther 324:1000–1010 [DOI] [PubMed] [Google Scholar]