Abstract
The aim of this study was to identify and characterise learning curves in hip fracture surgery. Operating times were collected and related to the number of procedures done by residents performing closed reduction and internal fixation using cannulated screws for intracapsular fractures of the hip and cephalomedullary nailing for trochanteric fractures, as well as hemiarthroplasty for displaced intracapsular fractures. The mean operating times decreased significantly for all four procedures studied, though at different rates. For cannulated screws, the mean duration of surgery decreased from 47.8 minutes to 30.1 minutes for procedures 21–25. For cephalomedullary nailing without distal locking, the mean operating time decreased from 73.3 minutes to 36.3 minutes. For cephalomedullary nailing with distal locking, the mean operating time decreased from 81.7 minutes to 56.9 minutes. The mean operating time for hemiarthroplasty decreased from 97.3 minutes to 66.0 minutes. Mean operating times decreased significantly for all procedures studied, though at different rates, indicating a unique learning curve for each procedure.
Introduction
The existence of a learning curve in acquiring technical skills in orthopaedic surgery is established in the literature, but has not been studied in detail as it relates to an individual resident acquiring basic orthopaedic skills without prior experience. Learning curves have been studied in a number of fields including arthroplasty surgery [1–6]. It has been used as an argument for subspecialisation [7], implying that certain procedures are technically challenging and have poor outcomes for physicians without enough experience to master the skills needed to perform them [8].
A learning curve can be defined as an improvement in performance over time [9] or with increasing experience or training. The starting point of the curve in surgery indicates the starting level of the surgeon and the end point shows an assumed expertise level [9, 10]. The slope of the curve indicates the speed of learning, which may be influenced by surgeon-related factors as well as institutional factors such as operating team experience, institutional volume, and financial resources [9, 10].
Outcome measures in depicting the learning curve are mostly proxy measures and have included time to completion of a task [4, 6], number of X-rays necessary [4], rate of complications [11], radiological parameters [12], as well as measurements of screw placement [5, 13] and the proportion of satisfactory results [7]. Time–action analysis is a video-based quantitative method that can be used to evaluate surgical technique and learning more objectively [14], but is not practical in a clinical setting.
Obtaining knowledge about learning curves is important for several reasons. With the introduction of new orthopaedic techniques, an analysis of a learning curve is pertinent [15]. New techniques might be regarded as technically more challenging, such as mini-invasive procedures or procedures that require a high level of precision [2, 3]. However, new techniques might also be introduced to reduce the degree of difficulty or increase precision, such as novel aiming devices and computer navigation [4, 6, 16]. In clinical trials, the effect of the learning curve might be profound when an established technique is compared to novel methods [10, 17]. In organising clinical trials, it is imperative that the surgeons have equal expertise in carrying out the procedures being studied [17] to avoid expertise-based bias against implants or techniques. Cognisance of learning curves could facilitate setting a limit on the number of procedures a surgeon must have completed before being allowed to take part in a study. In addition, the mandated 80-hour work week for orthopaedic residents in the United States has reduced the number of operations performed by second and third year residents by 20% over the last several years [18]. In Europe, work weeks are generally even shorter, which raises the question of how much training is required to master various procedures.
While comparative studies between the Gamma nail and hip compression screw have shown that the Gamma nail was associated with significant learning curves [19], details of the learning curves have not previously been examined. The aim of this study was to delineate the learning curves of residents learning hip fracture surgery using the cephalomedullary nail, cannulated screw fixation and hemiarthroplasty.
Materials and methods
The data for this study was extracted from a larger prospective study on hip fractures in a community hospital serving a population of 150,000 people. Data on all hip fracture procedures (1,780) between 1998 and 2003 were recorded.
Residents were selected for this study if they had performed at least 15 hemiarthroplasties (Exeter, Universal Head, Stryker), 20 internal fixations with cannulated screws (Olmed, Uppsala, Sweden) or at least ten osteosyntheses with short cephalomedullary nail (Gamma, Stryker/Howmedica). Twelve residents fulfilled the inclusion criteria (Fig. 1). Two of them, residents 11 and 12, had some experience in fracture surgery prior to being employed at our hospital. The remaining ten residents received their first training during the study period and were thus studied from the start of their learning curve.
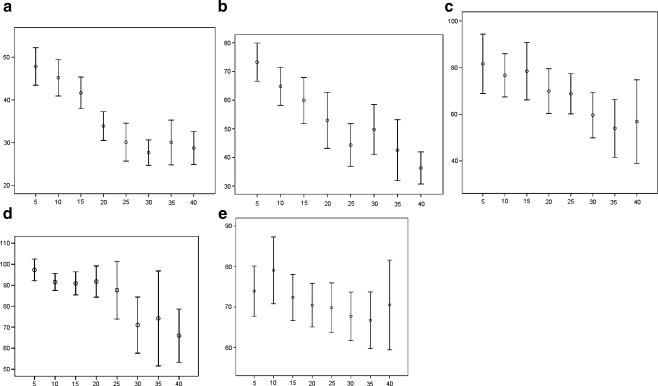
Fig. 1.
Mean operating times for all residents for each procedure. The procedures are grouped into clusters of five procedures according to the order in which they were undertaken, with the values on the x-axes corresponding to five procedures. Operating times are on the y-axis. Vertical bars represent 95% confidence intervals of mean. Non-overlapping bars indicate statistically significant differences between groups. a Internal fixation with cannulated screws. b Closed reduction and intramedullary nailing without distal locking. c Closed reduction and intramedullary nailing with distal locking. d Hemiarthroplasty performed by residents. e Hemiarthroplasty performed by orthopaedic surgeons
In order to increase the robustness of the study, seven orthopaedic surgeons employed at the hospital were included in the study to serve as controls. It was assumed that they had reached a plateau in their learning curves. These surgeons performed very few operations other than hemiarthroplasties and, for that reason, only the hemiarthroplasties were included in the statistical analysis. The undisplaced and moderately displaced femoral neck fractures were treated with two cannulated screws inserted percutaneously under fluoroscopic control, whereas the severely displaced intracapsular fractures were treated by bipolar hemiarthroplasty using a direct lateral Hardinge approach [20]. Trochanteric fractures were treated by closed reduction and cephalomedullary nailing with or without distal locking screws depending on the stability of the fracture.
A number of perioperative variables were recorded. The anaesthetic nurse registered operating times and bleeding; radiation time was automatically registered by the fluoroscopy device. For this study we elected to examine duration of surgery as representing the progress of acquiring surgical proficiency most accurately. The time spent reducing fractures was included in the times used for the analysis.
Statistical analysis
Each surgeon performed a series of operations and the procedures in each group of operations were assigned ascending numbers. In order to visualise the actual learning curve for each procedure, we grouped the procedures in groups of five according to the order undertaken. We then calculated the mean and the 95% confidence interval for the mean for each group of five procedures.
For analysis of the individual surgeon’s performance, we used ranked correlation in the SPSS statistical software package (SPSS Inc., Chicago, IL, USA) to obtain a Spearman’s correlation coefficient. The duration of each operation was recorded with the longest times receiving the highest number. Correlation coefficients will therefore be negative if the operating times decrease with increasing volume.
Results
Twelve residents performed 996 procedures and seven orthopedic surgeons performed 245 procedures (Table 1). Table 2 shows the number and operating times for all operations performed by residents. The mean operating time for cannulated screws was 37.2 minutes, decreasing from a high of 47.8 minutes for the first five procedures to a plateau of 30.1 minutes for procedures 21–25 (Fig. 1a). Operating times for procedures 15–20 and above were significantly shorter than operating times for the first 15 procedures as evidenced by non-overlapping confidence intervals. Operating times for procedures 26–30 were shorter than procedures 16–20, but this was not statistically significant.
Table 1.
Overview of 1,241 procedures performed in the study
| Type of surgery | Number of procedures | Mean operating time (minutes) | Minimum operating time (minutes) | Maximum operating time (minutes) |
|---|---|---|---|---|
| Cannulated screws | 412 | 37 | 10 | 120 |
| IM nail, no locking screw | 235 | 54 | 15 | 145 |
| IM nail with locking screw | 200 | 70 | 27 | 190 |
| Hemiarthroplasty residents | 215 | 92 | 40 | 155 |
| Hemiarthroplasty orthopaedic surgeons | 245 | 72 | 40 | 150 |
IM intramedullary
Table 2.
Number of procedures (count) and durations (time) for each procedure performed by the 12 residents
| Resident number | Osteosynthesis with cannulated screws | Cephalomedullary nailing, no distal locking | Cephalomedullary nailing with distal locking | Hemiarthroplasty | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | Time (min) | Minimum (min) | Maximum (min) | Count | Time (min) | Minimum (min) | Maximum (min) | Count | Time (min) | Minimum (min) | Maximum (min) | Count | Time (min) | Minimum (min) | Maximum (min) | |
| 1 | 45 | 34 | 18 | 67 | 14 | 55 | 35 | 90 | 19 | 63 | 33 | 105 | 20 | 82 | 62 | 100 |
| 2 | 22 | 44 | 20 | 120 | 11 | 70 | 30 | 145 | 14 | 70 | 45 | 110 | 11 | 89 | 65 | 112 |
| 3 | 30 | 49 | 25 | 100 | 17 | 72 | 50 | 105 | 10 | 93 | 35 | 139 | 25 | 99 | 73 | 140 |
| 4 | 45 | 31 | 13 | 90 | 21 | 48 | 17 | 79 | 18 | 61 | 27 | 190 | 23 | 86 | 60 | 115 |
| 5 | 14 | 45 | 20 | 60 | 5 | 62 | 47 | 110 | 7 | 83 | 50 | 155 | 15 | 109 | 90 | 135 |
| 6 | 21 | 41 | 22 | 57 | 18 | 64 | 40 | 120 | 7 | 85 | 40 | 138 | 12 | 97 | 83 | 120 |
| 7 | 22 | 40 | 20 | 65 | 21 | 66 | 32 | 108 | 5 | 94 | 65 | 123 | 3 | 97 | 85 | 105 |
| 8 | 35 | 33 | 11 | 81 | 29 | 50 | 15 | 115 | 30 | 58 | 37 | 105 | 21 | 92 | 69 | 120 |
| 9 | 37 | 32 | 12 | 53 | 12 | 46 | 27 | 77 | 20 | 71 | 50 | 115 | 16 | 102 | 47 | 135 |
| 10 | 32 | 39 | 12 | 70 | 32 | 48 | 25 | 85 | 15 | 67 | 30 | 135 | 19 | 94 | 65 | 155 |
| 11 | 40 | 27 | 10 | 60 | 21 | 41 | 20 | 95 | 10 | 61 | 38 | 85 | 37 | 83 | 60 | 130 |
| 12 | 40 | 46 | 20 | 85 | 16 | 63 | 31 | 120 | 27 | 77 | 48 | 135 | 13 | 84 | 40 | 108 |
| Mean | 32 | 38 | 10 | 120 | 18 | 57 | 15 | 145 | 15 | 74 | 27 | 190 | 18 | 93 | 40 | 155 |
For cephalomedullary nailing without distal locking, the mean operating time was 55.2 minutes, which declined from 73.3 minutes for the first five procedures to 36.3 minutes for the procedures 36 and beyond (Fig. 1b). The residents performed procedures 16–20 significantly faster than procedures 1–5. Procedures 36 and beyond were executed significantly faster than procedures 16–20.
For cephalomedullary nailing with distal locking, the mean operating time was 69.8 minutes, which decreased from 81.7 minutes for the first five procedures to 56.9 minutes for procedures 36 and beyond. The residents did procedures 31–35 significantly faster than procedures 1–10, but there were no further significant reductions in mean operating time later in this series (Fig. 1c).
The mean operating time for hemiarthroplasty was 91.6 minutes, decreasing from 97.3 minutes for the first five procedures to 66.0 minutes for the 36th and later. Procedures 26–30 were carried out significantly faster than procedures 1–15, and there was a drop from procedures 21–25 to procedures 26–30. Wide confidence intervals noted are probably due to fewer surgeons doing this many procedures (Fig. 1d).
For hemiarthroplasty performed by the orthopaedic surgeons, the mean operating time was 72 minutes (40–150). The mean difference between the surgeons and the residents was 20 minutes (95% CI 16.7–23.4). The residents reached the mean operating time of the orthopedic surgeons performing their procedures 26–30. For the orthopaedic surgeons, there was also a trend toward shorter operating times for procedures performed later in their series, with operating times decreasing from 73.9 to 70.5 minutes (Fig. 1e).
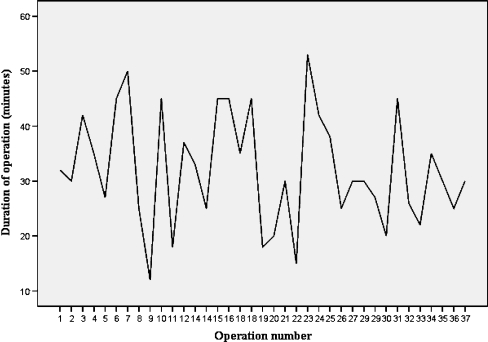
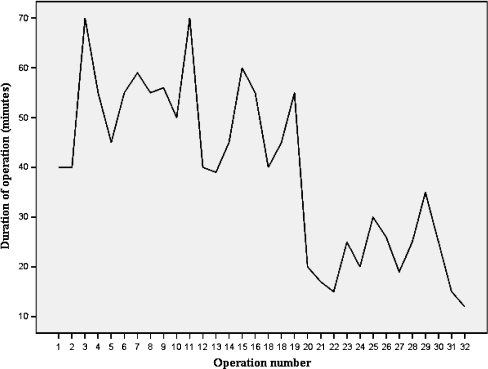
There was a significant correlation between large volume and decreasing operating times for eight of 12 residents doing cannulated screws (Table 3). Only one of the eight residents that did more than 30 operations failed to improve their operating time. All 12 residents performed 14 or more procedures, and the residents who did not decrease their time performed 14, 21, 22 and 37 procedures. The individual curves of resident 9, who did not improve, and resident 10, who decreased time significantly, are shown in Figs. 2 and 3. Resident 9 had large fluctuations in operating times, that did not seem to decrease with time, whereas resident 10 had a marked reduction in operating time after 20 cases.
Table 3.
Number of cases for each resident for each procedure including Spearman’s correlation coefficient and p-value
| Resident | Cannulated screws | Intramedullary nail, no distal locking screw | Intramedullary nail with distal locking screw | Hemiarthroplasty | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number | Spearman | p-value | Number | Spearman | p-value | Number | Spearman | p-value | Number | Spearman | p-value | |
| 1 | 45 | −0.42 | 0.005 | 14 | −0.66 | 0.010 | 19 | −0.56 | 0.013 | 20 | −0.09 | 0.694 |
| 2 | 22 | −0.66 | 0.001 | 11 | −0.43 | 0.190 | 14 | −0.44 | 0.117 | 11 | −0.05 | 0.883 |
| 3 | 30 | −0.56 | 0.001 | 17 | −0.05 | 0.859 | 10 | −0.20 | 0.578 | 25 | 0.31 | 0.136 |
| 4 | 45 | −0.52 | 0.000 | 21 | −0.56 | 0.009 | 18 | −0.50 | 0.036 | 23 | −0.71 | 0.000 |
| 5 | 14 | −0.06 | 0.850 | 5 | 0.05 | 0.935 | 7 | −0.49 | 0.268 | 15 | −0.11 | 0.703 |
| 6 | 21 | −0.01 | 0.962 | 18 | −0.57 | 0.013 | 7 | 0.36 | 0.432 | 12 | −0.53 | 0.077 |
| 7 | 22 | −0.29 | 0.189 | 21 | −0.79 | 0.000 | 5 | −0.50 | 0.391 | 0 | ||
| 8 | 35 | −0.42 | 0.011 | 29 | −0.61 | 0.000 | 30 | −0.46 | 0.011 | 21 | 0.12 | 0.610 |
| 9 | 37 | −0.20 | 0.246 | 12 | −0.39 | 0.208 | 20 | −0.02 | 0.925 | 16 | 0.40 | 0.124 |
| 10 | 32 | −0.74 | 0.000 | 32 | −0.75 | 0.000 | 15 | −0.56 | 0.032 | 19 | −0.46 | 0.047 |
| 11 | 40 | −0.49 | 0.001 | 21 | −0.39 | 0.079 | 10 | −0.43 | 0.214 | 37 | −0.61 | 0.000 |
| 12 | 40 | −0.41 | 0.010 | 16 | −0.52 | 0.039 | 27 | −0.30 | 0.123 | 13 | 0.39 | 0.193 |
p-values shown in italics are significant
Fig. 2.
Duration of surgery for one resident (resident 9) performing cannulated screws who did not improve mean operating times during the series of procedures
Fig. 3.
Duration of surgery for one resident (resident 10) performing cannulated screws who improved mean operating times during the series of procedures
The proportion of residents who significantly decreased their operating time was not statistically different (Fisher’s exact test) between the procedures. The proportion of residents improving their operating times for cannulated screws was 8/12, for unlocked cephalomedullary nailing 7/12, for locked cephalomedullary nailing 4/12, and for hemiarthroplasty 3/12, indicating that learning curves are different for each operation.
For the orthopaedic surgeons, we found a significant correlation between operation time and volume for one surgeon, who was the slightly less experienced surgeon of the group.
Discussion
This study examined operating times to determine whether a learning curve or learning effect could be measured for hip fracture surgery. However, it is important to emphasise that this does not imply that fast is always better than slow. It is perfectly conceivable that a resident can move along the learning curve by performing the procedure at a constant speed, but with increasing precision and improved technical quality. Nevertheless, the speed at which a certain procedure is executed is an important aspect of the technical learning process. In addition, duration of operation has economic implications due to the price of running an operating facility, as well as physiological implications to the patient. In this study we used operating time as a proxy measure for evidence of learning, which is supported by other studies using time to complete a task as a measurement of outcome [4, 6].
The main finding in this study is a significant correlation between the number of cases completed and decrease in operating time. The mean number of operations with cannulated screws for each surgeon was larger than the other groups (32), but even though the number of cephalomedullary nails and hemiarthroplasties was practically the same, the proportion of residents improving was strikingly different. Only 3/12 residents improved after performing a mean of 18 hemiarthroplasties, while 7/12 resident improved doing the same number of unlocked nails. The difference is not statistically different, but the trend suggests that the number of procedures necessary might be different for different procedures.
Based on these results, it is evident that more complex operations are those where a decreasing proportion of residents show improvement by performing practically the same number of procedures. This finding is supported by differences in the learning curves depicted in Fig. 1a–e. The curves suggest that for the cannulated screws, operating times were significantly lower at a lower volume than for the other procedures. For cannulated screws, a volume of 15 procedures was required to perform faster than the five first procedures, whereas the residents needed 20 unlocked and 30 locked nailing procedures, respectively, to perform faster than the first five procedures. For hemiarthroplasties, 25 procedures were needed to perform faster than the initial five procedures.
For hemiarthroplasty, the surgeons served as a control, and the mean operating times of the surgeons may indicate a level of expertise. The residents reached this level after having performed 25 procedures. For the other procedures, we do not have a control group, but the shape of the curves seem to indicate a plateau for the cannulated screws. For the nailing procedures, it is harder to see a definite plateau.
Interestingly, the numbers for the orthopaedic surgeons also indicated that speed increases with increasing numbers during this study period. We found a significant correlation between speed and volume only for the surgeon known to have somewhat less experience than the others; but even for the group as a whole, there was a trend toward lower operating times with an increasing volume of procedures.
There are multiple weaknesses in this study. First, we have not adjusted for possible case mix. Patient-related factors such as obesity and difficult versus easy fractures might influence operating times. The latter may be a concern for the cannulated screws, which were the treatment of choice for undisplaced as well as moderately displaced fractures; but preliminary analysis showed no difference in operating times for cannulated screws between displaced and moderately displaced fractures. The trochanteric fractures were treated by unlocked cephalomedullary nailing when stable and locked nailing when unstable, but there might still be some variance in fracture severity within the groups. We have also not allowed for previous non-orthopaedic experience. Some residents might have done some general surgery before starting their orthopaedic residency. Furthermore, some residents may simply be more active, doing more cases outside this study. Inexperienced staff may increase operating time [21], and there might be some variations in the experience of the surgical teams that has affected some procedures. Lastly, we were not able to record any data pertaining to the supervision offered during the surgery. Teaching styles may be different, and this could account for some variation in the operating times.
In reviewing the relationship between volume and quality, Shervin et al. called for additional studies to illuminate the causal factors between volume and outcome [22]. Our study is a contribution to that end and indicates that there are differences in learning curves between procedures and between residents. This may have implications for surgical training, choice of implants, as well as for the design of surgical trials. Further studies into the relationship between operating time and quality of surgery are needed.
Footnotes
Level of evidence: Level II, prognostic study
Contributor Information
Kristian Bjorgul, Phone: +1-434-2430067, FAX: +1-434-2430242, Email: kb8kb@virginia.edu, Email: krisbjorgul@gmail.com.
Wendy M. Novicoff, Phone: +1-434-2430296, FAX: +1-434-2430242, Email: wmn2v@virginia.edu
Khaled J. Saleh, Phone: +1-217-5458865, FAX: +1-217-5457901, Email: ksaleh@siumed.edu
References
- 1.Delaunay C, Kapandji AI. 10-year survival of Zweymuller total prostheses in primary uncemented arthroplasty of the hip. Rev Chir Orthop Reparatrice Appar Mot. 1998;84:421–432. [PubMed] [Google Scholar]
- 2.Paillard P. Hip replacement by a minimal anterior approach. Int Orthop. 2007;31(Suppl 1):S13–S15. doi: 10.1007/s00264-007-0433-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Swanson TV. Posterior single-incision approach to minimally invasive total hip arthroplasty. Int Orthop. 2007;31(Suppl 1):S1–S5. doi: 10.1007/s00264-007-0436-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pardiwala D, Prabhu V, Dudhniwala G, Katre R. The AO distal locking aiming device: an evaluation of efficacy and learning curve. Injury. 2001;32:713–718. doi: 10.1016/S0020-1383(01)00100-0. [DOI] [PubMed] [Google Scholar]
- 5.De VJ, Vandenberghe D. Acute percutaneous scaphoid fixation using a non-cannulated Herbert screw. Chir Main. 2003;22:78–83. doi: 10.1016/S1297-3203(03)00026-X. [DOI] [PubMed] [Google Scholar]
- 6.Rosenkranz J, Babst R. A special instrument: the LISS tractor. Oper Orthop Traumatol. 2006;18:88–99. doi: 10.1007/s00064-006-1164-4. [DOI] [PubMed] [Google Scholar]
- 7.Jain NP, Jowett AJ, Clarke NM. Learning curves in orthopaedic surgery: a case for super-specialisation? Ann R Coll Surg Engl. 2007;89:143–146. doi: 10.1308/003588407X155798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hansen TB, Snerum L. Elektra trapeziometacarpal prosthesis for treatment of osteoarthrosis of the basal joint of the thumb. Scand J Plast Reconstr Surg Hand Surg. 2008;42:316–319. doi: 10.1080/02844310802393974. [DOI] [PubMed] [Google Scholar]
- 9.Cook JA, Ramsay CR, Fayers P. Statistical evaluation of learning curve effects in surgical trials. Clin Trials. 2004;1:421–427. doi: 10.1191/1740774504cn042oa. [DOI] [PubMed] [Google Scholar]
- 10.Ramsay CR, Grant AM, Wallace SA, Garthwaite PH, Monk AF, Russell IT. Statistical assessment of the learning curves of health technologies. Health Technol Assess. 2001;5:1–79. doi: 10.3310/hta5120. [DOI] [PubMed] [Google Scholar]
- 11.Wiese M, Kramer J, Bernsmann K, Ernst WR. The related outcome and complication rate in primary lumbar microscopic disc surgery depending on the surgeon’s experience: comparative studies. Spine J. 2004;4:550–556. doi: 10.1016/j.spinee.2004.02.007. [DOI] [PubMed] [Google Scholar]
- 12.Callaghan JJ, Heekin RD, Savory CG, Dysart SH, Hopkinson WJ (1992) Evaluation of the learning curve associated with uncemented primary porous-coated anatomic total hip arthroplasty. Clin Orthop Relat Res 132–144 [PubMed]
- 13.Heller JG, Carlson GD, Abitbol JJ, Garfin SR. Anatomic comparison of the Roy-Camille and Magerl techniques for screw placement in the lower cervical spine. Spine. 1991;16:S552–S557. doi: 10.1097/00007632-199110001-00020. [DOI] [PubMed] [Google Scholar]
- 14.Minekus JP, Rozing PM, Valstar ER, Dankelman J. Evaluation of humeral head replacements using time-action analysis. J Shoulder Elbow Surg. 2003;12:152–157. doi: 10.1067/mse.2003.14. [DOI] [PubMed] [Google Scholar]
- 15.Gross M. Innovations in surgery. A proposal for phased clinical trials. J Bone Joint Surg Br. 1993;75:351–354. doi: 10.1302/0301-620X.75B3.8496198. [DOI] [PubMed] [Google Scholar]
- 16.Cobb JP, Kannan V, Brust K, Thevendran G. Navigation reduces the learning curve in resurfacing total hip arthroplasty. Clin Orthop Relat Res. 2007;463:90–97. doi: 10.1097/BLO.0b013e318126c0a5. [DOI] [PubMed] [Google Scholar]
- 17.Devereaux PJ, Bhandari M, Clarke M, Montori VM, Cook DJ, Yusuf S, Sackett DL, Cinà CS, Walter SD, Haynes B, Schünemann HJ, Norman GR, Guyatt GH. Need for expertise based randomised trials. Br Med J. 2005;330:88–93. doi: 10.1136/bmj.330.7482.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weatherby BA, Rudd JN, Ervin TB, Stafford PR, Norris BL. The effect of resident work hour regulations on orthopaedic surgical education. J Surg Orthop Adv. 2007;16:19–22. [PubMed] [Google Scholar]
- 19.Goldhagen PR, O’Connor DR, Schwarze D, Schwartz E. A prospective comparative study of the compression hip screw and the gamma nail. J Orthop Trauma. 1994;8:367–372. doi: 10.1097/00005131-199410000-00001. [DOI] [PubMed] [Google Scholar]
- 20.Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg Br. 1982;64:17–19. doi: 10.1302/0301-620X.64B1.7068713. [DOI] [PubMed] [Google Scholar]
- 21.Minekus JP, Rozing PM, Nelissen R, Dankelman J (2005) Identifying error pathways during elbow and knee replacements. Clin Orthop Relat Res 121–127 [DOI] [PubMed]
- 22.Shervin N, Rubash HE, Katz JN. Orthopaedic procedure volume and patient outcomes: a systematic literature review. Clin Orthop Relat Res. 2007;457:35–41. doi: 10.1097/BLO.0b013e3180375514. [DOI] [PubMed] [Google Scholar]