Abstract
Intramedullary interlocking nailing for diaphyseal fractures is a standard treatment option in affluent societies. These procedures are often performed under image intensifier guidance. The cost of these gadgets precludes their common use in resource poor regions. External jig-aided intramedullary interlocking nailing is relatively cheap and offers the chance for performing these procedures in resource poor regions. The aim of this study was to document the advantages, challenges and outcome of this form of treatment in a resource poor setting. The Surgical Implant Generation Network (SIGN) implants and instrumentation were used for this study. Thirty-seven limbs in 35 patients were included. There were 30 males and five females giving a ratio of 6:1. The mean age was 35 ± 11.9 years with a range of 15–61 years. The femur and tibia were the bones studied with a total of 23 and 14 fractures, respectively (ratio 1.6:1). There were 14 comminuted fractures, two segmented fractures, six mal-unions, eight non-unions and seven simple fractures. Road traffic accidents were the most common cause of injuries with motorcycle accidents accounting for 19 (57.4%) cases. The mean follow-up period was 22 ± 5.32 months, mean time to union was 16.9 ± 5.4 weeks and the major complication was osteomyelitis (10.8%). We conclude that this is a viable treatment option for musculoskeletal injuries in resource poor regions. Education to encourage early acceptance of surgical intervention and reduced patronage of traditional bone setting for injudicious interventions can reduce the infective complication rates.
Introduction
Intramedullary interlocking nailing has revolutionised the treatment of long bone diaphyseal fractures and is considered the treatment of choice for these injuries [1, 2]. Interlocked intramedullary nailing is often performed with image intensifiers to guide placement of locking screws and is used as a minimal access procedure in many affluent societies. Intramedullary nails act as load-sharing internal splints, and locked intramedullary nails offer greater rotational stability while counteracting axial and bending forces [3].
In resource-poor societies, intramedullary interlocking nailing is rarely performed and literature from these sources is scarce [4]. This is because image intensifiers are expensive and not readily available in these areas. Modifications of standard interlocking techniques have been described from less affluent societies [4, 5]. These modifications involve either the use of external jigs to aid screw placement [4], or the use of regular screws with appropriately modified Küntscher nails [5]. A distal cortical window and an externally placed guide nail are useful in guaging slot position and screw placement in the latter [5].
The use of image intensifiers allows a minimal access approach with closed reduction of fractures. When an image intensifier is not used, fracture reduction has to be open, although the incision is smaller than that used in the application of a plate and screw assembly [5, 6]. Image intensifiers however pose the risk of radiation exposure to the patient and operating team [5, 7]. The combination of costs and risks of unnecessary radiation exposure may therefore be factors that popularise the use of an external jig-aided interlocking system, especially in resource-poor settings.
In some centres in Nigeria, Surgical Implant Generation Network (SIGN) interlocking nails and instrumentation have allowed the use of interlocking nails for humeral, femoral and tibial diaphyseal fractures [4]. This has reduced the burden of provision of care on society because the instruments and implants are offered free of charge to the patients. Standard interlocked intramedullary diaphyseal fracture care with the documented advantages of early post-operative weight bearing, high rates of fracture union and low complication rates are some of the benefits to these patients if the technique becomes readily acceptable. The aim of this report was to document our experiences with interlocking nailing without image intensifiers. Since this may be the means to achieving improved outcomes in fracture care in resource-poor settings, the challenges posed by the technique and the advantages derived should be well understood.
Patients and methods
This was a prospective descriptive study lasting 17 months involving 37 consecutive long bone fractures, non-unions or mal-unions involving the femur and tibia which presented in our hospital and accepted the described technique. Patients had the procedure explained to them, signed an informed hospital consent form and were offered interlocking intramedullary nailing using SIGN implants, instruments and technique protocols.
Specific inclusion guidelines were generally agreed. Patients with simple diaphyseal fractures, comminuted fractures, non-unions and mal-unions who consented to the treatment option were recruited. Open fractures were only included if they were Gustilo and Anderson Type I and II fractures with wounds adjudged clean after irrigation and debridement. Medullary reaming was done in all cases except comminuted and open fractures. Each patient received prophylactic Ceftriaxone or Cefuroxime and Metronidazole. Spinal or epidural anaesthesia was used in all cases.
Technique
Preoperatively, nail sizes were determined by clinical and radiological parameters. In femoral fractures and when the antegrade approach was the technique of choice, nail length was determined by measuring from the tip of the greater trochanter to the superior pole of the patellar of the contralateral femur (x mm). The final nail length was determined by subtracting 50 mm from the distance obtained (x−50 mm) and correcting to the nearest whole number. The use of an X-ray on the contralateral femur for length determination was precluded by lack of resources. This also limits radiation exposure. In the tibia, nail length was determined by measuring from the tibial tubercle to the tip of the medial malleolus and subtracting 30–50 mm from the obtained length. Nail diameters were determined by measuring the diameter of the medullary canal and correcting to the nearest whole number after subtracting a magnification factor of 10%.
Intraoperatively, all fractures were approached and reduced directly using small incisions. The external jig and nails were assembled with instructions as contained in the SIGN instrumentation guide manual and instructional CD. Once the holes/slot in the nail have been aligned with the holes in the target arm using the alignment pins, the apparatus is disassembled, leaving the nail attached to the T-handle and the proximal and distal target arms coupled together. In the antegrade approach to the femur, the greater trochanter is approached and broached via a small incision over the trochanter. We routinely access the medullary cavity through the postero-lateral aspect of the greater trochanter. The cavity can also be accessed through the pirifomis fossa.
In the retrograde approach to the femur and the approach to the tibia, we access the knee joint through a straight incision over the anterior knee with splitting of the patellar ligament in the line of it’s fibres. With the knee flexed 60–90° (we prefer 90°), adequate retraction and minimal excision the fat pad, the entry points on the femur (the middle of the intercondylar groove) and tibia (about 2 cm proximal to the tibial tubercle at the anterior edge of the tibial plateau) are identified and broached. Manual reaming is then performed to 3–4 mm above the pre-determined nail diameter. The medullary cavity is then lavaged with normal saline and the nails introduced. A soft tissue protector used during nail insertion prevents soft tissue devitalisation and nail contamination by skin organisms. The fractures are reduced and held before the nail traverses the fracture site.
We usually aim to allow the T-handle–nail junction to lie about 4 mm from the superior bone margin at the entry site. The target arm is then re-coupled to the T-handle and the alignment pins used to determine the sites of skin incision for interlocking screw insertion. Cannulae guide in drilling the interlocking holes, which are appropriately expanded using the step-drill. Correct screw hole–nail hole/slot alignment is determined by obtaining the “SIGN feel” using slot finders. Interlocking is then performed and the T-handle and target arms uncoupled from the nail. Wound closure and dressings follow standard techniques.
All patients were encouraged to do early range of motion (ROM) exercises for all joints. X-rays were done in the immediate postoperative period, at ten weeks postoperatively and subsequently at 16–18 weeks [8]. Crutch-aided full weight bearing was delayed until an average of 12 weeks postoperatively. Fracture union, non-union and chronic osteomyelitis were defined by radiological and clinical criteria. The mean period of follow-up was 22 ± 5.32 months, and results were analysed using EPI-INFO 2002 (revision 2).
Results
Thirty-seven fractures in 35 patients who accepted the procedure were included in the study. The ages of patients ranged from 15 to 61 years with a mean of 35 ± 11.9 years. Thirty patients (83.8%) were males, 18 (48.6%) were civil servants, ten (27.0%) were students, eight (21.6%) were businessmen and one (2.7%) was a clergy man. Two patients had bilateral lower limb fractures involving one femur and tibia each. Table 1 shows the causes of injury while Table 2 shows the type of fracture pathologies. Twenty-three (62.2%) fractures were femoral and 14 (37.8%) were tibial. Table 3 shows screw deployment.
Table 1.
Causes of injury
| Causes of injury | Frequency | Percentage (%) |
|---|---|---|
| Road traffic accident (car) | 11 | 29.7 |
| Road traffic accident (motorcycle) | 19 | 51.4 |
| Fall | 4 | 10.8 |
| Assault | 3 | 8.1 |
| Total | 37 | 100 |
Table 2.
Fracture pathology
| Fracture pathology | Frequency | Percentage (%) |
|---|---|---|
| Communited | 14 | 37.8 |
| Malunion | 6 | 16.2 |
| Non-union | 8 | 21.6 |
| Segmental | 2 | 5.4 |
| Simple | 7 | 18.9 |
| Total | 37 | 100 |
Table 3.
Screw deployment
| Screws | Frequency | Percentage (%) |
|---|---|---|
| 1D1P | 16 | 43.2 |
| 1PnoD | 3 | 8.1 |
| 2D1P | 17 | 45.9 |
| 2D2P | 1 | 2.7 |
| Total | 37 | 100 |
D distal, P proximal
The antegrade approach was used in 17 patients (45.9%) with femoral fractures; the retrograde approach was used in six (16.2%) patients. Fifteen patients (40.5%) had bone grafts. Complications included osteomyelitis (n = 4, 10.8%), superficial surgical site infection (n = 3, 8.1%) which settled, and implant failure with non-union (n = 1, 2.7%). Two (33%) of the six patients who had a retrograde approach to the femur had varying degrees of knee stiffness. The majority (n = 27, 73%) had no complications during the period. The most common intra-operative difficulty was distal locking which was encountered in ten patients (27%).
Overall mean union time for all fractures was 16.9 ± 5.4 weeks while the average healing time for femoral fractures (17.2 ± 5.9 weeks) was longer than the average healing time (16.4 ± 4.8 weeks) for tibial fractures. There was, however, no statistically significant difference between the mean healing time for femoral and tibial fractures (t = 0.37, df = 21, p > 0.05). One patient (2.7%) required dynamisation.
Discussion
The burden of musculoskeletal disease is at the forefront of healthcare worldwide and the estimated lifetime cost of injuries is enormous [9]. Resource poor regions are not immune to the challenges these injuries pose. The biological and financial advantages of interlocked intra-medullary nailing of diaphyseal fractures include early postoperative weight bearing, high rates of fracture union, early range of motion (ROM), low complication rates and reduced costs [2, 9–11]. The addition of interlocking screws allows control of rotational forces at the fracture site and represents a significant advantage over non-locked nails. Union rates between 95 and 99% have been reported with the use of interlocked intramedullary nails [2]. Many interlocked nails are performed under image intensifier guidance and this poses the risk of undue radiation exposure to the patient and operating team [7]. Image intensifiers are also expensive.
The Surgical Implant Generation Network (SIGN) interlocking nail is particularly suited for resource-poor regions [10]. The implants and instrumentation are offered free of charge and the system does nor require a fracture table, power reaming or image intensification. The solid nails used in the tibia, femur and humerus are the same. The challenge in resource poor regions is the increased burden of care occasioned by traumatic incidents and the attendant effects on their fragile economies. Poor roads, improperly maintained vehicles, illiteracy concerning road signs and lack of good emergency systems combine to cause a large number of road accidents and poor treatment outcomes [12]. These factors are aggravated by the increased patronage of traditional bonesetters whose interventions usually result in such complications as non union, mal-union and gangrene [13].
Thirty-five patients with 37 fractures accepted the procedure over a period of 17 months. Out of these, road traffic accidents accounted for 81% of the injuries. The mean age of our patients (35 ± 11.9 years) compared well with that of the other published Nigerian study on interlocking intramedullary nails [4]. Malunions and non-unions accounted for a combined 37.8% of our patients. This is much higher than figures reported in a previous Nigerian study with a combined rate of 8% [4]. These were patients who had earlier refused surgery and opted for traditional bone setting. These results underscore the influence of poverty and illiteracy on decision making in many resource poor regions. All fractures in this series were approached and reduced by open techniques. The absence of an image intensifier precluded minimal access techniques. However, the smaller incision lengths required compared to those used for plate and screw osteosynthesis confers the advantage of less contamination, less soft tissue manipulation and less risk for infection [14]. These factors may have resulted in our comparable infection rates (10.8% osteomyelitis), considering the number treated after traditional bone setting interventions, and high rates of union (97.3%).
The management of postoperative chronic osteomyelitis was dependent on the stage of healing of the fractures. All patients who presented with chronic osteomyelitis and healed fractures had the nails removed, the medullary cavity reamed and lavaged. Marrow samples were obtained for microscopy, culture and sensitivity (MCS). The reamed marrow was then washed with an antibiotic solution and the patient placed on an MCS directed six to eight week course of antibiotics using the sequential intravenous–oral protocol. Serial Erythrocyte sedimentation rates and complete blood counts were used for follow-up. We have no access to C-reactive protein estimation. During the immediate six to eight weeks post implant removal and debridement, the limb was protected and weight bearing forbidden.
Patients who presented with chronic osteomyelitis without fracture union were managed with a suppressive protocol while waiting for union to occur. All the fractures eventually united and the implants were removed. We did not perform either an immediate or delayed exchange nailing in any of the patients who presented with postoperative osteomyelitis. We also did not use antibiotic impregnated beads or the modified Lautenbach procedure [15] for the treatment of any of these cases.
The overall mean union time of 16.9 ± 5.4 weeks compares with those of other studies [9, 16]. Reaming for most fractures and bone graft augmentation for non-unions may have contributed to our union rates. There was no mechanical failure in our study. The implant failure recorded was a loose screw. Mechanical failure in interlocked intramedullary nails occurs at the distal end, through the middle screw hole/slot, in instances where the “fracture-locking hole” distance is less than 5 cm and is due to increased stress concentration at the locking holes [11]. Mechanical failure is also common with non-standardised locally produced implants [11].
Though statistically insignificant, femoral fractures took a longer time to heal in our study than tibial fractures (femoral, 17.2 ± 5.9 weeks; tibial, 16.4 ± 4.8 weeks). This may have been because there were more femoral malunions and non-unions who presented after intervention by traditional bonesetters. Crutch aided weight bearing was commenced at an average 12 weeks postoperatively. This was after X-rays showed signs of progressive union. Though early weight-bearing is one of the documented advantages of interlocked intra-medullary nailing, we delayed weight-bearing to reduce the cyclical loading stresses imposed by walking. This is necessary in our environment where the procedure is not readily accepted, a revision procedure would be more difficult to accept and where patients would likely disobey medical instructions concerning crutch aided touch down weight bearing. However, during the interval, active range of motion (ROM) exercises to the hips, knees and ankles were encouraged.
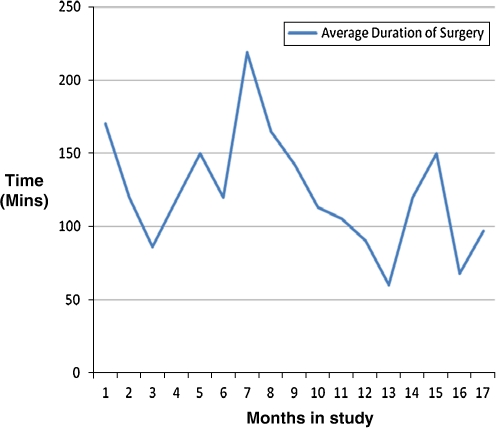
Our results do not show any significant influences on union rates and osteomyelitis by the number of distal and proximal screws used. Distal interlocking screw insertion presented intraoperative difficulties in 27% of our patients. This is where image intensifiers provide an advantage. Duration of surgery over time (Fig. 1) shows a learning process is necessary for surgeons beginning to use the technique. Each major upward spike occurred when more surgeons began using the technique and difficulties with distal interlocking was the major cause of intraoperative delays. Mild nail deformation and rotation as the nail passes down the medullary canal are likely causes of “external jig-nail slot” mismatches. The mean operating times however compare with those of other published studies [14].
Fig. 1.
Learning process
Retrograde interlocked intramedullary nailing is useful in obese patients, patients with floating knees, and in older and osteoporotic patients [14]. Retrograde nail insertion for distal femoral fractures requires less soft tissue dissection compared to plate and screw osteosynthesis. There is therefore less blood loss, shorter operating times and reduced risk for infection. Postoperative knee stiffness can be a major complication, especially in patients who do not commence early knee-mobilisation and in situations as in resource-poor regions, where continuous passive motion machines are not available. This complication was seen in two out of six patients (33%) in our study who had retrograde nailing.
Conclusion
Overall, external jig aided interlocking intramedullary nailing yielded high union rates and minimal complication rates in our experience. This is significant when the number of patients who had been exposed to injudicious traditional bone setting interventions before enrolment is considered. Patients in resource-poor regions can thus have the documented benefits of this treatment modality combined with the advantage of reduced costs. Medullary reaming whenever feasible and bonegraft augmentation for all non-unions with this technique contribute to high union rates [16]. This is important in resource-poor regions with scarce finances and settings where surgical interventions are not readily accepted. Public education to reduce patronage and hence the complications of traditional bone setting and encouragement of early acceptance of appropriate surgical interventions will popularise the technique in the developing world with consistent results. Where local implant production is feasible, standardisation of production materials must be stressed to reduce the incidence of mechanical failure.
Acknowledgments
Appreciation is extended to Dr. Lew Zirkle and Surgical Implant Generation Network (SIGN), Richland, WA, USA for making the implants and instrumentation available at no cost.
References
- 1.Wolinsky P, Tejwani N, Richmond JH, Koval KJ, Egol K, Stephen DJG. Controversies in intramedullary nailing of femoral shaft fractures. J Bone Joint Surg (Am) 2001;83:1404–1415. [PubMed] [Google Scholar]
- 2.Wiss DA. What’s new in orthopaedic trauma? J Bone Joint Surg (Am) 2001;83:172–1772. doi: 10.2106/00004623-200111000-00032. [DOI] [PubMed] [Google Scholar]
- 3.Müller ME, Allgöwer M, Schneider R, Willenegger H (Eds) (1995) Medullary nailing of femur and tibia. In: Manual of internal fixation (techniques recommended by the AO-ASIF Group), 3rd edn. Springer, Berlin, pp 291–365
- 4.Ikem IC, Ine HR, Ogunlusi JD. Achieving interlocking nails without using an image intensifier. Int Orthop. 2007;31(4):487–490. doi: 10.1007/s00264-006-0219-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ogbemudia AO, Enemudo R, Edomwonyi E (2007) Closed interlocked nailing of a fractured femur without X-ray guide in first trimester pregnancy: a case report. Internet J Third World Med 5(2)
- 6.Giri SK, Adhikari BR, Gurung GB, RcD BAR, Khatri K. Mini-open reduction and intramedullary interlocking nailing of fracture shaft of tibia without an image intensifier. Nepal Med Coll J. 2008;10(2):123–125. [PubMed] [Google Scholar]
- 7.Giordano BD, Ryder S, Baumhauer JF, DiGiovanni BF. Exposure to direct and scatter radiation with use of mini-c-arm fluoroscopy. J Bone Joint Surg (Am) 2007;89:948–952. doi: 10.2106/JBJS.F.00733. [DOI] [PubMed] [Google Scholar]
- 8.Robertson A, Sutherland M, Keating JF. Intramedullary nailing of tibial fractures: how often are post-operative radiographs needed? J R Coll Surg Edinb. 2000;45:220–222. [PubMed] [Google Scholar]
- 9.Buckley R, Panaro CDA (2007) General principles of fracture care. eMedicine. http://emedicine.medscape.com/article/1270717-overview. Accessed 25 January 2010
- 10.Gosselin RA, Heilto M, Zirkle L. Cost effectiveness of replacing skeletal traction by interlocked intramedullary nailing for femoral shaft fractures in a provincial trauma hospital in Cambodia. Int Orthop. 2009;33(5):1445–1448. doi: 10.1007/s00264-009-0798-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bhat AK, Rao SK, Bhaskarand K. Mechanical failure in intramedullary interlocking nails. J Ortho Surg. 2006;14(2):138–141. doi: 10.1177/230949900601400206. [DOI] [PubMed] [Google Scholar]
- 12.Kobusingye OC. Why poor countries cannot afford to ignore road safety. Afr J Trauma. 2004;2:6. [Google Scholar]
- 13.Ikpeme IA, Udosen AM, Okereke-Okpa I. Patients' perception of traditional bone setting in Calabar. Port Harcourt Med J. 2007;1:104–108. [Google Scholar]
- 14.Gurkan V, Orhun H, Doganay M, Saliogu F, Ercan T, Dursun M, Bulbul M. Retrograde intramedullary interlocking nailing in fractures of the distal femur. Acta Orthop Traumatol Turc. 2009;43(3):199–205. doi: 10.3944/AOTT.2009.199. [DOI] [PubMed] [Google Scholar]
- 15.Ikpeme IA, Udosen AM. Improvised irrigation and drainage system for the Laurenback procedure. Int J Trp Surg. 2009;3(2):84–87. [Google Scholar]
- 16.Shafi MK, Ahmed N, Khan AH, Aziz A. Results of fracture union in closed reamed interlocking nail in fractures of femur. Pak J Med Sci. 2008;24(5):698–701. [Google Scholar]