Abstract
The modified extended trochanteric osteotomy (ETO) preserves the posterior capsule and short external rotators through a lateral approach to the hip. The purpose of this study was to assess the performance of long ETOs, measuring 18 cm and above. Fifty three long ETOs were reviewed. The mean length of the osteotomy was 20.0 cm (range, 18–26). Mean scratch-fit length was 6.5 cm. Average follow-up was 57 months (range, 14–114 months). The Harris hip score improved from 37 preoperatively to 73 at last follow-up. Subsidence occurred in 12 (22.6%) cases. Eleven stems stabilised over the first year. One stem (1.9%) was revised for subsidence and loosening, one for a periprosthetic fracture and one for a fractured stem. Two (3.8%) cups had postoperative dislocations. Fifty two (98.1%) osteotomies united well. This series shows a low failure rate, with revision and union rates comparable to those reported for shorter ETOs. Performing the osteotomy through a lateral approach to the hip will enhance posterior stability.
Introduction
Extraction of a well fixed cementless femoral stem or a cemented stem may pose a major challenge to the surgeon performing a revision total hip arthroplasty. The extended trochanteric osteotomy (ETO) facilitates removal of such stems and additionally provides excellent acetabular exposure [1, 2]. Another indication for the use of an ETO in total hip arthroplasty is the correction of angular deformities of the proximal femur [1–3]. Published union rates of the ETO in revision hip arthroplasty were between 98% and 100% [1, 2, 4–10]. Several different methods of performing an extended trochanteric osteotomy have been described, using either a posterior or a lateral approach to the hip [1, 2, 6, 8, 9, 11]. The modified extended sliding trochanteric osteotomy preserves the posterior capsule and short external rotators in order to enhance posterior stability, through a lateral approach to the hip.
In order to allow simple and safe extraction of the stem and/or cement mantle, the trochanteric osteotomy is preferably extended to the distal extent of the porous coating or to the level of the cement plug. However, in order to allow reconstruction of the femur using a distal fixation stem, an extensive porous coated cylindrical stem [1, 2, 4, 8] or a tapered stem [7, 8], sufficient diaphyseal bone should be left intact [12–15]. Osteotomy lengths in previous reported series were between 5.8 and 19 cm (mean lengths, 12.5–13.4 cm) [1, 4, 6, 8, 11]. It was suggested in previous papers that in order for the stem to have primary stability, at least 4–7 cm of intact cortical tube is required [12–16].
The purpose of this retrospective study was to assess the performance of long extended trochanteric osteotomies, measuring 18 cm and above, with respect to femoral stem subsidence and loosening, together with union rates, functional outcomes and complications.
Patients and methods
Six hundred and six hip revision operations, performed in 544 patients, between January 2000 and March 2008 were reviewed. Data was retrospectively collected from our prospective clinical database. Of these patients, ETO was performed in 108 patients (114 hips). Four patients for whom a proximal femoral allograft was used and five extended trochanteric osteotomies performed as part of a first stage revision of infected THA were excluded from this study. Two patients died and three patients were lost to follow-up before one year of follow-up was completed. Osteotomy length was measured on the standard six weeks, postoperative anterior-posterior radiograph, from the tip of the GT to the end of the osteotomy. Radiographs were digitally calibrated according to the femoral head diameter, as recorded in the operative report. The mean length of the osteotomy was 17.4 cm (range, 9–26 cm). Of these 100 osteotomies, 53 osteotomies measured 18 cm or more in length (mean 20.0 cm; range, 18–26 cm) and were included in this study.
The mean age at time of surgery was 73 years (range, 27–91 years). Included were 30 (57%) women and 23 (43%) men. Mean BMI (body mass index) was 24.1 (range, 21–29). Mean ASA (American Society of Anaesthesiologists) score was 1.89. Ten (19%) patients had an ASA score of 1.39 (74%) patients had a score of 2 and four (8%) had a score of 3. The mean preoperative Harris hip score (HHS) was 37 (range, 10–84). The indication for 45 revisions (85%) was aseptic loosening. Five (9%) revisions were performed for periprosthetic fractures, two (4%) for fractured stems and one (2%) for instability. The femoral stem that was extracted during revision was a cemented stem in 44 (83%) cases and a cementless stem in nine (17%) cases. The study operation was a first hip arthroplasty revision for 40 (75%) patients, a second revision for nine (17%), and a third or fourth revision for four (8%). Twenty nine (55%) osteotomies were performed for femoral revision alone, and 24 (45%) osteotomies for femoral and acetabular revision. All femurs were reconstructed with a modular, titanium stem (ZMR, Zimmer, Warsaw, Indiana, USA). Extensively porous coated components were used in 24 (45%) hips. Assembled modular stem lengths were between 250 and 320 mm (mean, 294 cm). Tapered components were used in 29 (55%) hips. Assembled modular stem lengths were between 265 and 335 mm (mean, 302 mm). Thirty six cases (68%) had cortical strut augmentation of the osteotomy. Average follow-up was 57 months (range, 14–114 months).
Our surgical preoperative planning included the radiographic assessment of femoral bone loss and stem fixation. In situ, stem type and fixation dictate surgical exposure. For cemented stems and well fixed cementless stems with extensive coating, our practice is to perform an ETO. The end of the osteotomy is extended to the level of the cement plug or the distal end of the porous coating. If that planned length of osteotomy precludes distal fixation with at least 4–5 cm of diaphyseal bone, we plan a shorter osteotomy and drill through the more distal cement in order to extract it.
All operations were performed by the two senior authors (AEG, DB). The osteotomy is performed from proximal to distal, starting at the tip of the GT and extending distally as planned and measured from the tip of the GT. The osteotomy is made from posterior to anterior. In the proximal femur it is performed between the posterior border of the gluteus medius anteriorly and the piriformis and short external rotators posteriorly. The posterior capsule and short external rotators remain intact. At the diaphyseal part, approximately one third of the femur circumference is included in the osteotomy. The osteotomised fragment is retracted anteriorly, with the abductors and vastus lateralis muscles attached. The anterior pseudo-capsule is removed, and the hip is dislocated anteriorly. Following acetabular and femoral reconstruction, the osteotomy is reduced and held with double-looped 16-gauge stainless steel wires, the number of wires used is determined by the length of the osteotomy. Cortical struts are used to augment the osteotomy if the bone is of poor quality. Morselised bone graft is placed at the osteotomy junction to facilitate union. A mixture of morselised allograft and autograft from the acetabular and femoral reamings is used. During postoperative rehabilitation, patients are restricted from active abduction for at least six weeks.
Follow-up evaluation took place at six weeks, 12 weeks, six months and one year after the procedure and then once yearly. Clinical evaluation included the Harris hip score (HHS) preoperatively, at six weeks after the revision and at annual follow-up visits. Patient medical records were reviewed to record complications and further revision surgery. Radiological evaluation included routine hip radiographs (anterior-posterior view of the pelvis as well as anterior-posterior and lateral view of the affected hip) performed preoperatively, immediately postoperatively and at six weeks, six months and annually post surgery (Fig. 1). All radiographs were reviewed by one observer not involved in patient care. Radiographs were digitally calibrated according to femoral head diameter, as recorded in the operative note. Immediate postoperative radiographs were reviewed to ascertain the length of the osteotomy and the amount of “scratch-fit” and distal fit (Fig. 2). Scratch-fit was defined as the length of stem in contact with both medial and lateral cortical bone on the anterior-posterior radiograph or with both the anterior and posterior cortices on the lateral radiograph, the longer of which was considered as the scratch-fit. Distal fit was defined as the length of stem extending beyond the osteotomy. The latest follow-up radiographs were reviewed to assess union of the osteotomy and femoral stem loosening. The osteotomy was deemed united when bridging callus was present on both the anteroposterior and lateral radiographs [2]. Femoral stem loosening was assessed according to the criteria described by Engh et al. [17] and was considered to be definitely present when stem subsidence of more than 2 mm, a pedestal or interface deterioration were noted. The length of osteotomy and the extent of scratch-fit fixation and distal fit were correlated against femoral stem loosening.
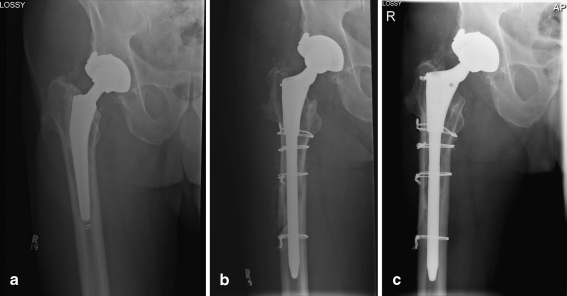
Fig. 1.
a An 83-year-old man with a loose cemented stem. b The stem was revised through an 18-cm extended trochanteric osteotomy. Five centimetres of scratch-fit were available for distal stem fixation. c Five years after revision, the stem is well fixed and the extended trochanteric osteotomy has healed
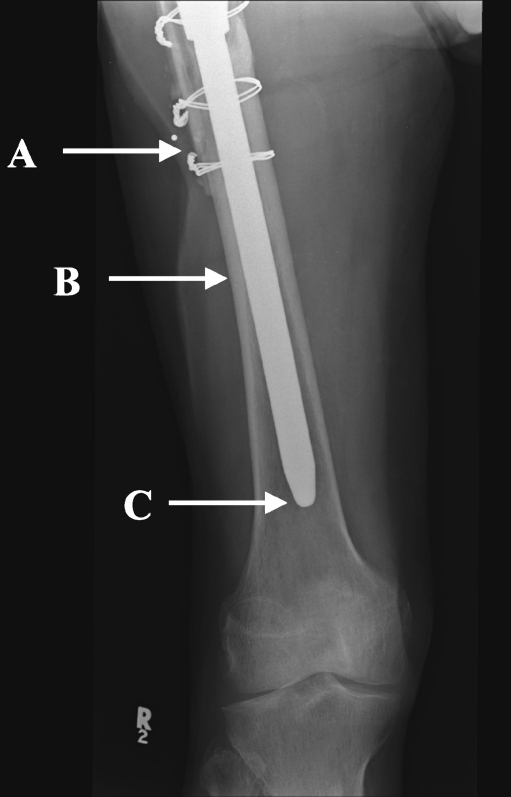
Fig. 2.
Scratch-fit was measured as the length of stem between the tip of the ETO (a) and the most distal level in which the stem is in close contact with two cortices (b). Distal fit was defined as the length of stem extending beyond the osteotomy (between A and C)
Continuous variables were compared using the t-test for independent samples. Post-hoc power analysis was performed when differences between groups were not statistically significant at P ≤ 0.05.
Results
The mean length of the osteotomy was 20.0 cm (range, 18–26 cm). Mean scratch-fit was 6.4 cm (range, 4–11 cm) and the distal fit was over a mean distance of 11.5 cm (range, 6–18.5 cm) (Table 1). Scratch-fit length in hips in which porous coated cylindrical stems were implanted was 7.7 cm (range, 5–11). In hips in which tapered stems were used the mean scratch-fit length was 5.5 cm (range, 4–10).
Table 1.
ETO, scratch-fit and distal-fit lengths
| Measurement | Taper stems (n = 29) | Porous stems (n = 24) | Total (n = 53) |
|---|---|---|---|
| ETO lengtha | 20.5 (18–26) | 19.5 (18–23) | 20.0 (18–26) |
| Scratch-fit lengthb | 5.5 (4–10) | 7.7 (5–11) | 6.3 (2–11) |
| Distal-fit lengthc | 10.9 (6–15) | 12.2 (6.5–18.5) | 11.5 (6–18.5) |
| Number of subsided stems | 8 | 4 | 12 |
ETO extended trochanteric osteotomy
a From the tip of the GT to the distal end of the osteotomy
b The length of stem in contact with cortical bone
c The length of the stem extending beyond the osteotomy
Three stems (5.7%) were re-revised. One stem (1.9%) was revised for subsidence and loosening. This porous stem had 5 cm of scratch-fit and 14 cm of distal-fit. A proximal femoral allograft was used for revision. One (1.9%) stem was revised due to a periprosthetic fracture and one (1.9%) stem due to a fracture of the stem at the modular junction one year postoperatively.
Subsidence occurred in 12 (22.6%) hips, in the range of 5 to 22 mm (mean, 13.6 mm). One patient, with a subsidence of 20 mm, was symptomatic and needed a revision. The 11 other patients who had radiographic evidence of subsidence were observed only and stabilisation occured sometime during the first postoperative year. Four of them complained of pain, which resolved with stabilisation of the stem. Mean scratch-fit lengths were 5.7 ± 1.85 (range, 4–9) for the subsided stems and 6.6 ± 2.08 (range, 4–11) for the stems that did not subside (p = 0.18, post hoc power = 37%). Mean distal-fit lengths were 10.3 ± 2.6 (range, 6–15) for the stems that subsided and 11.8 ± 2.76 (range, 6.5–18.5) for the stems that did not subside (p = 0.099, post hoc power = 49%).
The osteotomy was intraoperatively fragmented in four cases (7.5%), three of which were at the junction of the GT and the diaphyseal part, at the level of the vastus lateralis ridge. Two (3.8%) other patients had undisplaced diaphyseal cracks starting at the level of the tip of the ETO and extending distally. There was no case of femoral perforation by a reamer or stem. In all cases the fractures were wired and four of them were protected by a cortical strut. All intraoperative fractures healed uneventfully.
The mean Harris hip score improved from 37 points (range, 10–84) before the operation to 73 points (range, 36–96) at last follow-up. Of the 53 osteotomies, 52 (98.1%) united. In one case (1.9%) the diaphyseal part of the ETO united but the fragmented GT did not unite and migrated proximally. Two patients (3.8%) dislocated postoperatively. Both patients had recurrent dislocations and had the cup revised. Other complications included one haematoma requiring incision and drainage and one deep infection that required debridement.
Discussion
The extended trochanteric osteotomy in revision total hip arthroplasty is a well established technique to facilitate removal of cement from the femoral canal and extraction of well fixed cementless femoral stems. It also provides excellent exposure of the acetabulum and can be employed to correct angular deformities of the proximal femur. The ETO minimises the risk of femoral perforation and fracture, in particular in the deformed femur. Preservation of an intact musculo-osseous-muscular sleeve comprised of the gluteus medius and minimus, the GT, and the vastus lateralis, allows physiological reconstruction of the hip's soft tissue envelope [18, 19] and prevents proximal migration of the osteotomy. Union rates of the osteotomy in this and previous studies were between 98 and 100% [1, 2, 4, 7, 8, 10]. In the face of infection, union rate may be as low as 86% [11]. The union rate of ETO in our study was higher than the 86–95% reported rate of union for trochanteric slide osteotomies [19–22]. This may be accounted for by the longer bony surface available for healing, the tubular structure of the diaphysis which may better serve as a platform for wire fixation than the rounded GT, and the longer portion of vastus lateralis that remains attached to the osteotomy fragment and prevents proximal migration. Although a learning curve might be expected and more fractures of the osteotomised fragment may occur in the hands of less experienced surgeons, these fractures are generally expected to heal uneventfully.
Femoral reconstruction following an ETO can be achieved using distal fixation implants [1, 2, 4, 7, 8]. In order for the stem to have primary stability, at least 4–7 cm of intact cortical tube is required [12–16]. Previous reported series of extended trochanteric osteotomies had osteotomy lengths of between 5.8 and 19 cm (mean lengths, 12.5–13.4 cm) [1, 2, 6, 8, 11]. Published stem re-revision rates at one to eight years were between 0 and 6.8% [1, 2, 4, 6]. Miner reported a series of 166 extended trochanteric osteotomies, performed through the posterior approach [2]. A cylindrical porous coated stem was used for reconstruction. Mean osteotomy length was 14.1 cm and mean scratch-fit was 6.45 cm (range, 3.6–9.7). At mean follow-up of 3.9 years, three (1.8%) stems were re-revised. Mean osteotomy length in our series was 20 cm, with mean scratch-fit length of 6.3 cm. Re-revision rate at mean follow-up of five years was 5.7%. Although there was no significant difference between scratch-fit and distal-fit lengths of stems that subsided and those that did not, there was a trend towards significance. However, most subsided stems were asymptomatic and stabilised sometime during the first postoperative year.
Extended trochanteric osteotomies may be associated with several different approaches to the hip joint. Most reported series included a posterolateral approach to the hip joint with posterior surgical dislocation of the hip. Reported postoperative dislocation rates after this approach were between 7% and 30% [1, 2, 8, 9, 11]. ETO through a transgluteal approach, with anterior surgical dislocation of the hip, was also reported [6, 7, 10], and had 0–5% of postoperative dislocations, comparable to the dislocation rate of the current series, which was 3.8%. We find the transgluteal technique to result in an unnecessary damage to the abductor muscles. Our technique includes a lateral approach to the hip and an anterior surgical dislocation, with preservation of the posterior capsule and external rotator attachments, and the abductor muscles mass and tendons. The decision to perform an ETO using the described technique should be made preoperatively.
In conclusion, our series of long ETOs shows a low failure rate, with re-revision and union rates comparable to those reported for shorter ETOs. Used in combination with modular distal fixation stems, the osteotomy may be extended as far distal as needed, as long as it does not preclude distal fixation with at least 4 cm of diaphyseal bone. Performing the osteotomy through a lateral approach to the hip, while preserving the attachment of the external rotators and posterior capsule, will enhance posterior stability and prevent postoperative dislocations.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Chen WM, McAuley JP, Engh CA, Jr, Hopper RH, Jr, Engh CA. Extended slide trochanteric osteotomy for revision total hip arthroplasty. J Bone Joint Surg Am. 2000;82:1215–1219. doi: 10.2106/00004623-200009000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Miner TM, Momberger NG, Chong D, Paprosky WL. The extended trochanteric osteotomy in revision hip arthroplasty: a critical review of 166 cases at mean 3-year, 9-month follow-up. J Arthroplasty. 2001;16:S188–S194. doi: 10.1054/arth.2001.29385. [DOI] [PubMed] [Google Scholar]
- 3.Della Valle CJ, Berger RA, Rosenberg AG, Jacobs JJ, Sheinkop MB, Paprosky WG. Extended trochanteric osteotomy in complex primary total hip arthroplasty. A brief note. J Bone Joint Surg Am. 2003;85-A(12):2385–2390. doi: 10.2106/00004623-200312000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Mardones R, Gonzalez C, Cabanela ME, Trousdale RT, Berry DJ. Extended femoral osteotomy for revision of hip arthroplasty: results and complications. J Arthroplasty. 2005;20:79–83. doi: 10.1016/j.arth.2004.10.014. [DOI] [PubMed] [Google Scholar]
- 5.Paprosky WG, Sporer SM. Controlled femoral fracture: easy in. J Arthroplasty. 2003;18:S91–S93. doi: 10.1054/arth.2003.50074. [DOI] [PubMed] [Google Scholar]
- 6.MacDonald SJ, Cole C, Guerin J, Rorabeck CH, Bourne RB, McCalden RW. Extended trochanteric osteotomy via the direct lateral approach in revision hip arthroplasty. Clin Orthop Relat Res. 2003;417:210–216. doi: 10.1097/01.blo.0000096818.67494.7b. [DOI] [PubMed] [Google Scholar]
- 7.Lerch M, Lewinski G, Windhagen H, Thorey F. Revision of total hip arthroplasty: clinical outcome of extended trochanteric osteotomy and intraoperative femoral fracture. Technol Health Care. 2008;16(4):293–300. [PubMed] [Google Scholar]
- 8.Levine BR, Della Valle CJ, Lewis P, Berger RA, Sporer SM, Paprosky W. Extended trochanteric osteotomy for the treatment of Vancouver B2/B3 periprosthetic fractures of the femur. J Arthroplasty. 2008;23(4):527–533. doi: 10.1016/j.arth.2007.05.046. [DOI] [PubMed] [Google Scholar]
- 9.Morshed S, Huffman GR, Ries MD. Extended trochanteric osteotomy for 2-stage revision of infected total hip arthroplasty. J Arthroplasty. 2005;20(3):294–301. doi: 10.1016/j.arth.2004.09.060. [DOI] [PubMed] [Google Scholar]
- 10.Peters PC, Jr, Head WC, Emerson RH., Jr An extended trochanteric osteotomy for revision total hip replacement. J Bone Joint Surg Br. 1993;75(1):158–159. doi: 10.1302/0301-620X.75B1.8110207. [DOI] [PubMed] [Google Scholar]
- 11.Levine BR, Della Valle CJ, Hamming M, Sporer SM, Berger RA, Paprosky WG. Use of the extended trochanteric osteotomy in treating prosthetic hip infection. J Arthroplasty. 2009;24(1):49–55. doi: 10.1016/j.arth.2008.01.306. [DOI] [PubMed] [Google Scholar]
- 12.Böhm P, Bischel O. The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res. 2004;420:148–159. doi: 10.1097/00003086-200403000-00021. [DOI] [PubMed] [Google Scholar]
- 13.Engh CA, Jr, Hopper RH, Jr, Engh CA., Sr Distal ingrowth components. Clin Orthop Relat Res. 2004;420:135–141. doi: 10.1097/00003086-200403000-00019. [DOI] [PubMed] [Google Scholar]
- 14.Krishnamurthy AB, MacDonald SJ, Paprosky WG. 5- to 13-year follow-up study on cementless femoral components in revision surgery. J Arthroplasty. 1997;12(8):839–847. doi: 10.1016/S0883-5403(97)90152-2. [DOI] [PubMed] [Google Scholar]
- 15.McAuley JP, Engh CA., Jr Femoral fixation in the face of considerable bone loss: cylindrical and extensively coated femoral components. Clin Orthop Relat Res. 2004;429:215–221. doi: 10.1097/01.blo.0000150274.21573.f4. [DOI] [PubMed] [Google Scholar]
- 16.Sporer SM, Paprosky WG. Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res. 2003;417:203–209. doi: 10.1097/01.blo.0000096803.78689.0c. [DOI] [PubMed] [Google Scholar]
- 17.Engh CA, Massin P, Suthers KE. Roentgenographic assessment of the biologic fixation of porous-surfaced femoral components. Clin Orthop Relat Res. 1990;257:107–128. [PubMed] [Google Scholar]
- 18.Goodman S, Pressman A, Saastamoinen H, Gross A. Modified sliding trochanteric osteotomy in revision total hip arthroplasty. J Arthroplasty. 2004;9:1039–1041. doi: 10.1016/j.arth.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 19.Lakstein D, Safir O, Backstein D, Kosashvili Y, Gross AE (2009) Modified trochanteric slide for complex hip arthroplasty: clinical outcomes and complication rates. J Arthroplasty (in press) [DOI] [PubMed]
- 20.Bal BS, Kazmier P, Burd T, Aleto T. Anterior trochanteric slide osteotomy for primary total hip arthroplasty. Review of nonunion and complications. J Arthroplasty. 2006;21(1):59–63. doi: 10.1016/j.arth.2005.04.020. [DOI] [PubMed] [Google Scholar]
- 21.Ebraheim NA, Patil V, Liu J, Haman SP. Sliding trochanteric osteotomy in acetabular fractures: a review of 30 cases. Injury. 2007;38(10):1177–1182. doi: 10.1016/j.injury.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 22.Baba T, Shitoto K (2009) Revision of total hip arthroplasty using the Kerboull and KT plates. Int Orthop. doi:10.1007/s00264-009-0789-y [DOI] [PMC free article] [PubMed]