Abstract
Leg length discrepancy following total hip replacement (THR) can contribute to poor hip function. Abnormal gait, pain, neurological disturbance and patient dissatisfaction have all been described as a result of leg length inequality after THR. The purpose of this study was to determine whether the use of computer navigation in THR can improve limb length restoration and early clinical outcomes. We performed a matched-pair study comparing 48 computer-assisted THR with 48 THRs performed using a traditional freehand alignment method. The same implant with a straight non-modular femoral stem was used in all cases. The navigation system used allowed the surgeon to monitor both acetabular cup placement and all the phases of femoral stem implantation including rasping. Patients were matched for age, sex, arthritis level, pre-operative diagnosis and pre-operative leg length discrepancy. At a minimum follow-up of six months, limb length discrepancy was measured using digital radiographs and a standardised protocol. The number of patients with a residual discrepancy of 10 mm or more and/or a post-operative over-lengthening were measured. The clinical outcome was evaluated using both the Harris Hip Score and the normalised Western Ontario and McMaster Universities (WOMAC) Arthritis Index. Restoration of limb length was significantly better in the computer-assisted THR group. The number of patients with a residual limb length discrepancy greater than 10 mm and/or a post-operative over-lengthening was significantly lower. No significant difference in the Harris Hip Score or normalised WOMAC Arthritis Index was seen between the two groups. The surgical time was significantly longer in the computer-assisted THR group. No post-operative dislocations were seen.
Introduction
Currently, uncemented total hip replacement (THR) represents one of the most successful orthopaedic procedures. A survival rate of the implant after THR of approximately 93% at 20 years has been documented [10, 29]. However, leg length discrepancy following THR can be a significant problem and has been shown to contribute to patient dissatisfaction. Leg length inequality following THR can result in abnormal force transmission across the hip joint and may contribute to implant loosening [8, 24]. Gofton reported increased stress in the superolateral portion of the socket in patients with unilateral lengthening [8]. Pain, instability, stiffness, neuropathy and heterotopic ossification have all been linked either directly or indirectly to leg length discrepancy. In the USA and more recently in Europe, these problems have resulted in increasing litigation [4, 14, 27, 33].
Avoiding a post-operative limb length discrepancy remains an important focus for all surgeons performing THR. To this end, a number of techniques have been proposed to assess limb length intra-operatively with varying results [27, 30, 31]. Surgeons are always looking for any new technical improvements that will help achieve a more ‘normalised’ new hip with equal leg lengths and optimal joint function [1, 19, 22].
The use of computer navigation in arthroplasty has been increasing over the past several years. These navigation techniques use sophisticated computer algorithms and tracking systems to allow the surgeon to determine the three-dimensional placement of instruments and prosthetic components during surgery [23, 33]. Studies in the literature demonstrate substantial statistical improvement in the accuracy of acetabular cup placement using navigation compared to freehand alignment methods [9, 10, 16, 21]. In 2009, Gandhi et al. presented a meta-analysis showing that navigation in hip arthroplasty improves the precision of acetabular cup placement with a lower number of outliers from the desired alignment [7]. Few studies have been published on the clinical results of femoral stem placement using computer navigation [3, 5, 17]. Only one retrospective non-matched study has been published in the literature evaluating the effect of navigation on leg length discrepancy using a straight monoblock femoral stem [18].
We performed a matched-pair study between two groups of THR using the same implant. One group of 48 patients underwent computer-assisted surgery and a second matched group underwent surgery without navigation support. The aim of the study was to determine whether using navigation in THR (Ca-THR) could achieve better results in terms of limb length discrepancy and early clinical outcomes.
Patients and methods
Patients who underwent a cementless THR using a CT-free computer-assisted alignment system (Vector Vision, version 1.52, BrainLAB, Munich, Germany) in our department between February 2003 and January 2009 were considered for this study. The criterion for inclusion was a body mass index (BMI) lower than 40. Patients with a significant hip dysplasia (≥Crowe III), limb length discrepancy greater than 3 cm or a major femoral head deformity were excluded [6]. Forty-eight patients (group B) who underwent a Ca-THR using a CT-free computer-assisted alignment system met the criteria and were included in the study.
Each patient in this group was matched with a patient who had undergone conventional freehand THR (group A) using the same implant in the same period. Patients were matched for age (maximum difference ± 3 years), sex, arthritis level according to the Kellgren and Lawrence classification [13], pre-operative diagnosis and pre-operative discrepancy (shorter to shorter, longer to longer and with a maximum difference of ±10 mm).
In both groups a posterolateral approach to the hip joint was made. The same prosthesis used in both groups was a Synergy titanium tapered stem and a Reflection cup (Smith & Nephew, Memphis, TN, USA). A standard 28-mm oxinium femoral head was used with a 20° polyethylene acetabular insert in all patients. The duration of surgery was documented. Post-operative early weight-bearing as tolerated was encouraged in all patients. All episodes of hip dislocation were documented.
Intra-operatively in the navigated group the anterior pelvic plane was identified with a tracker fixed on the same fside to the anterior superior iliac spine with two 4.0 threaded pins to determine the correct socket position. The second part of the acquiring process was performed with the patient in the lateral position with a second tracker fixed to the distal femur with two other 4.0 threaded pins to determine the leg length.
In the freehand group intra-operatively the residual leg length discrepancy was assessed comparing both the level of the feet in the lateral position and the distance between the great trochanter and a pin fixed in the ilium just over the acetabulum.
Pre-operative and six month post-operative measurements of limb length discrepancy were made using a standard protocol and digital radiographs with IMPAX digital radiography software (Agfa-Gevaert N.V., Wilmington, DE, USA) as described by Takigami et al. in 2008 [31]. This technique uses a horizontal line drawn through the bottom of the ischial tuberosities. The limb discrepancy was then measured using the distance between this line and the most prominent point of the lesser trochanter on the digital radiographs. All radiographs were performed with both hips in a neutral position using a standardised protocol to ensure the same magnification. This protocol was rigidly adhered to during the study and radiographs were repeated if an error was detected. All radiographs were assessed twice by an independent radiologist blinded to the original procedure. The interval between the assessments was two weeks and the final leg length was taken as the mean value of the two assessments.
Comparisons were made between the two groups on the basis of the number of patients with a post-operative leg length discrepancy of 10 mm or more. The number of patients in each group with a post-operative limb lengthening was also compared. At a minimum follow-up of six months the clinical outcome of the THR was evaluated using both the Harris Hip Score and the normalised Western Ontario and McMaster Universities (WOMAC) Arthritis Index. The normalised WOMAC Arthritis Index uses a total score out of 100 as described in the WOMAC user’s handbook [2]. Statistical analysis of the results was performed and the two groups compared. Non-parametric testing (Kruskal-Wallis test) was adopted using Statistica 7.0 software (StatSoft Inc., Tulsa, OK, USA) for analysis because of an abnormal data distribution. Statistical significance was set at P ≤ 0.05.
Results
No statistically significant differences in patient demographics were seen. The pre-operative diagnosis in both groups was primary osteoarthritis in 21 patients, developmental dysplasia (Crowe grade I–II) in 12 patients, post-traumatic arthritis in eight patients, avascular necrosis in four patients, sequelae of septic arthritis in two patients and sequelae of Perthes disease in one patient. According to the arthritis grading system of Kellgren and Lawrence, two patients had grade 2, 12 patients grade 3 and 34 patients grade 4 disease in each group. There were no significant differences in the mean pre-operative limb length discrepancy and Harris Hip Score between the two groups. The mean pre-operative leg length discrepancy was 11.94 mm (range: 5–28 mm) in group A and 12.17 mm (range: 5–28 mm) in group B. The mean pre-operative Harris Hip Score was 40.04 (range: 30–46) in group A and 39.83 (range: 32–48) in group B. The mean follow-up was 41.19 months (range: 7–76) and 39.6 months (range: 8–77) for groups A and B, respectively (Table 1).
Table 1.
Patient demographic data, 48 cases in each group. Data reported as mean value (M), standard deviation (SD), range (R) and P value (P)
| Group A (THR) | Group B (Ca-THR) | P | |
|---|---|---|---|
| Age | M: 71.98 | M: 72.23 | 0.99 |
| SD: ±9.39 | SD: ±8.41 | ||
| R: 45–88 | R: 48–86 | ||
| Sex | Male: 22 | ||
| Female: 26 | |||
| Pre-operative Harris Hip Score | M: 40.04 | M: 39.83 | 0.85 |
| SD: ±4.63 | SD: ±5.13 | ||
| R: 30–46 | R: 32–48 | ||
| Pre-operative limb length discrepancy (mm) | M: 11.94 | M: 12.17 | 0.48 |
| SD: ±6.80 | SD: ±5.93 | ||
| R: 5–28 | R: 5–28 | ||
| Follow-up | M: 41.19 | M: 39.60 | 0.7195 |
| SD: ±21.39 | SD: ±21.26 | ||
| R: 7–76 | R: 8–77 | ||
| Pre-operative diagnosis (cases) | 21 primary arthritis | ||
| 12 developmental dysplasia (Crowe I–II) | |||
| 8 post-traumatic arthritis | |||
| 4 avascular necrosis | |||
| 2 sequelae of septic arthritis | |||
| 1 sequelae of Perthes disease | |||
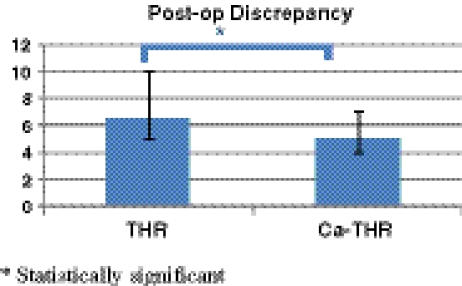
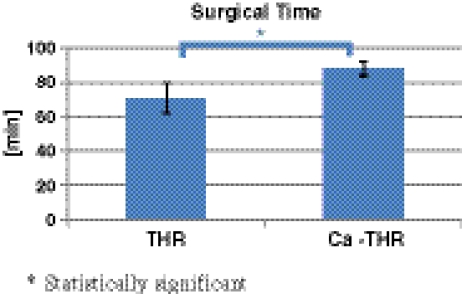
Surgical time was statistically longer in the computer-assisted group with a mean of 89.39 (range: 77–122) compared to 73.17 min (range: 48–116) in the freehand group. In the computer-assisted group, the mean post-operative leg length discrepancy was reduced to 5.06 mm (range: 0–12) compared to 7.64 mm (range: 0–20) in the freehand group. This difference was statistically significant. In neither group did the post-operative leg length discrepancy exceed 2 cm (Fig. 1). A statistically significant increase in the number of patients with a post-operative over-lengthening was seen in the freehand group (eight cases in group A and one case in group B). Only five patients had a post-operative leg length discrepancy of 10 mm or greater in the computer-assisted group compared with 13 patients in the freehand group. This difference was statistically significant. At latest follow-up, no sign of major subsidence was seen in any of the implants.
Fig. 1.
Post-operative leg length discrepancy
There were no complications attributable to the navigation with no pin tract infections or fractures.
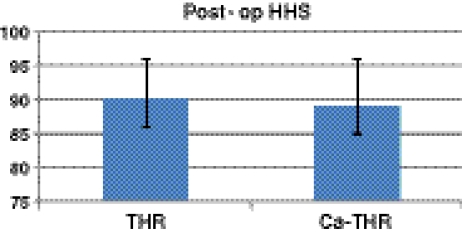
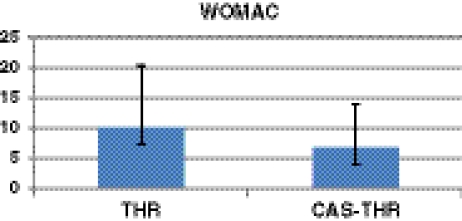
There were no statistically significant differences in the Harris Hip Score between the two groups and all the patients were satisfied with the outcome at follow-up (Fig. 2). The mean Harris Hip Score was 89.73 (range: 72–100) and 88.87 (range: 74–100) in groups A and B, respectively. The normalised WOMAC Arthritis Index was 13.21 (range: 0–40) in group A and 9.33 (range: 0–30) in group B (Fig. 3). This difference was not statistically significant. No prosthetic dislocations were seen during the study and to date, no patient has required a revision procedure (Table 2).
Fig. 2.
Post-operative Harris Hip Score
Fig. 3.
Post-operative normalised WOMAC Arthritis Index
Table 2.
Post-operative results for the two groups. Data reported as mean value (M), standard deviation (SD) and range (R)
| Group A (THR) | Group B (Ca-THR) | P | |
|---|---|---|---|
| Post-operative Harris Hip Score | M: 89.73 | M: 88.87 | 0.5791 |
| SD: ±7.10 | SD: ±7.51 | ||
| R: 72–100 | R: 74–100 | ||
| Post-operative limb length discrepancy (mm) | M: 7.65 | M: 5.06 | 0.0043 |
| SD: ±4.36 | SD: ±2.99 | ||
| R: 0–20 | R: 0–12 | ||
| # post-op. length.: 8 | # post-op. length.: 1 | 0.0148 | |
| # ≥ 10: 13 | # ≥ 10: 5 | 0.0374 | |
| WOMAC | M: 13.21 | M: 9.33 | 0.0503 |
| SD: ±9.82 | SD: ±7.04 | ||
| R: 0–40 | R: 0–30 | ||
| Surgical time (min) | M: 73.17 | M: 89.39 | 0.0000 |
| SD: ±15.26 | SD: ±9.68 | ||
| R: 48–116 | R: 77–122 |
Discussion
Leg length discrepancy following THR can result in poor hip function. Limp, abnormal gait, pain, neurological disturbance and patient dissatisfaction have all been described as a result of leg length inequality after THR. These problems can lead to revision surgery and may even be a source of litigation. Despite new implant designs, instrumentation and surgical techniques, limb length discrepancy still remains a concern for patients and surgeons [4, 14, 28, 34].
In the literature only one study in 2002 questioned any correlation between leg discrepancy after hip arthroplasty and functional outcome and patient satisfaction [32].
In 2007, Rubash and Parvataneni advocated specific perioperative steps to reduce the impact of limb discrepancy including provision of adequate patient information, accurate pre-operative templating and fixed reference points to measure intra-operative leg length [27]. Some authors recommend intra-operative use of Kirschner wires, Steinman pins or dedicated tools such as callipers to help measure intra-operative leg length [20, 30, 31].
Several studies have shown better placement of the acetabular cup and femoral stem can be achieved in THR using either a CT-based or image-free computer navigation system. The authors of many of these studies suggest that the technological advances now available could result in more accurate implant alignment and that this in turn may translate into better implant stability, performance and survivorship [9, 11, 12, 15, 16, 21]. In 2008, Renkawitz et al. in a saw-bone model study, postulated that imageless navigation could help the surgeon to restore both leg length and femoral offset [25]. A cadaver study in 2009 by the same authors using CT measurements showed that intra-operative assessments of leg length and femoral offset are reliable and accurate with an imageless calculation algorithm [26]. However, a retrospective non-matched study by Mainard et al. showed no clear advantage in restoration of limb length when using a computer-assisted technique in hip arthroplasty compared with a freehand technique [18]. However, up to now no study has reported any relevant clinical advantage in using navigation compared to a freehand technique.
In 2008, we published a retrospective matched-pair study comparing restoration of both limb length and femoral offset using either a computer navigated THR or a freehand alignment system [5]. Computer navigation resulted in significantly better results for both these parameters. However, this study had only 22 patients in each treatment group and a short modular femoral stem was used. Strict exclusion criteria were used and only patients with no hip deformity were included in the study. In addition, the navigation software used only evaluated the modular neck on the final implant and was not able to guide femoral canal rasping or final stem position.
In this study we did not consider the femoral offset and focused on limb discrepancy. A traditional non-modular femoral stem was used. The computer navigation system used allowed all phases of femoral stem implantation and femoral canal rasping to be assessed. In this study 48 matched-pair patients undergoing computer-assisted THR were compared with the same number undergoing traditional freehand THRs using the same implant. At a minimum of six months of follow-up our results demonstrated that in THR computer navigation significantly improves the restoration of limb length. In the computer-assisted group we had significantly fewer cases with a residual discrepancy greater than 10 mm and a significantly lower number of cases with post-operative over-lengthening. No statistically significant difference was seen in the Harris Hip Score or normalised WOMAC Arthritis Index between the two groups. No incidence of prosthetic dislocation was seen during the study in both groups. No significant intra-operative complications occurred. However, the surgical time was statistically longer in the computer-assisted group (Figs. 4 and 5).
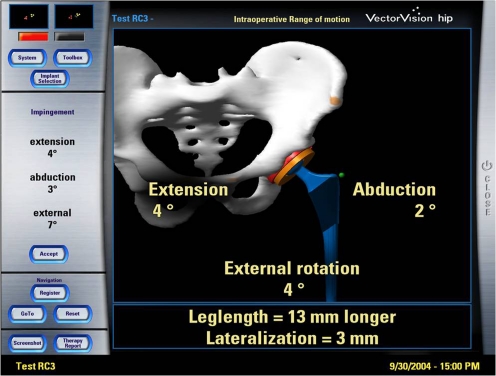
Fig. 4.
Surgical time
Fig. 5.
Final screen shot with the data achieved
We recognise that our study has some limitations. It was a retrospective analysis, the patients were not randomised and the follow-up was too short to detect any difference in the clinical outcome. Strict inclusion criteria including diagnosis, age and sex, BMI and pre-operative discrepancy were adopted to match the two groups.
Likewise, we could not demonstrate any clinical relevance of a worse leg length restoration with similar clinical results in both the groups at a short follow-up. However, these results demonstrated that using computer navigation in THR could enhance the surgeon’s ability to correct limb length discrepancy. We believe that computer navigation of both the femoral stem and acetabular cup in THR represents a practical way to achieve a more ‘anatomical hip arthroplasty’. We advocate longer follow-up to detect the real influence on the outcome and patient satisfaction.
References
- 1.Barrak RL. Dislocation after total hip arthroplasty: implant design and orientation. J Am Acad Orthop Surg. 2003;11:89–99. doi: 10.5435/00124635-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Bellamy N. WOMAC: a 20-year experiential review of a patient-centered self-reported health status questionnaire. J Rheumatol. 2002;29:2473–2476. [PubMed] [Google Scholar]
- 3.Braun A, Lazovic D, Zigan R. Modular short-stem prosthesis in total hip arthroplasty: implant positioning and the influence of navigation. Orthopedics. 2007;30(10 Suppl):S148–S152. [PubMed] [Google Scholar]
- 4.Clark CR, Huddleston HD, Schoch EP, 3rd, Thomas BJ. Leg-length discrepancy after total hip arthroplasty. J Am Acad Orthop Surg. 2006;14(1):38–45. doi: 10.5435/00124635-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 5.Confalonieri N, Manzotti A, Montironi F, Pullen C (2008) Leg length discrepancy, dislocation rate, and offset in total hip replacement using a short modular stem: navigation vs conventional freehand. Orthopedics 31(10 Suppl 1):pii:orthosupersite.com/view.asp?rID=35541 [PubMed]
- 6.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61(1):15–23. [PubMed] [Google Scholar]
- 7.Gandhi R, Marchie A, Farrokhyar F, Mahomed N. Computer navigation in total hip replacement: a meta-analysis. Int Orthop. 2009;33(3):593–597. doi: 10.1007/s00264-008-0539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gofton JP. Studies in osteoarthritis of the hip. IV. Biomechanics and clinical considerations. Can Med Assoc J. 1971;104(11):1007–1011. [PMC free article] [PubMed] [Google Scholar]
- 9.Haaker RGA, Tiedjen K, Ottersbach A, Rubenthaler F, Stockheim M, Stiehl JB. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007;22(2):151–159. doi: 10.1016/j.arth.2005.10.018. [DOI] [PubMed] [Google Scholar]
- 10.Havelin LI, Engesaeter LB, Espehaug B, Furnes O, Lie SA, Vollset SE. The Norwegian Arthroplasty Register: 11 years and 73,000 arthroplasties. Acta Orthop Scand. 2000;71:337–353. doi: 10.1080/000164700317393321. [DOI] [PubMed] [Google Scholar]
- 11.Kalteis T, Handel M, Bäthis H, Perlick L, Tingart M, Grifka J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: is it as accurate as CT-based navigation? J Bone Joint Surg. 2006;88(2):163–167. doi: 10.1302/0301-620X.88B2.17163. [DOI] [PubMed] [Google Scholar]
- 12.Kalteis T, Handel M, Herold T, Perlick L, Baethis H, Grifka J. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. Int Orthop. 2005;29(5):272–276. doi: 10.1007/s00264-005-0671-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Konyves A, Bannister GC. The importance of leg length discrepancy after total hip arthroplasty. J Bone Joint Surg Br. 2005;87(2):155–157. doi: 10.1302/0301-620X.87B2.14878. [DOI] [PubMed] [Google Scholar]
- 15.Jenny JY, Boeri C, Dosch JC, Uscatu M, Ciobanu E. Navigated non-image-based positioning of the acetabulum during total hip replacement. Int Orthop. 2009;33(1):83–87. doi: 10.1007/s00264-007-0479-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lazovic D, Kaib N. Results with navigated bicontact total hip arthroplasty. Orthopedics. 2005;28(10 Suppl):S1227–S1233. doi: 10.3928/0147-7447-20051002-05. [DOI] [PubMed] [Google Scholar]
- 17.Lazovic D, Zigan R. Navigation of short-stem implants. Orthopedics. 2006;29(10 Suppl):S125–S129. [PubMed] [Google Scholar]
- 18.Mainard D (2008) Navigated and nonnavigated total hip arthroplasty: results of two consecutive series using a cementless straight hip stem. Orthopedics 31(10 Suppl 1): pii:orthosupersite.com/view.asp?rID=35528 [PubMed]
- 19.Malik A, Maheshwari A, Dorr LD. Impingement with total hip replacement. J Bone Joint Surg Am. 2007;89:1832–1842. doi: 10.2106/JBJS.F.01313. [DOI] [PubMed] [Google Scholar]
- 20.Matsuda K, Nakamura S, Matsushita T. A simple method to minimize limb-length discrepancy after hip arthroplasty. Acta Orthop. 2006;77(3):375–379. doi: 10.1080/17453670610046280. [DOI] [PubMed] [Google Scholar]
- 21.Nogler M, Kessler O, Prassl A, Donnely B, Streicher R, Sledge JB, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop Relat Res. 2004;426:159–163. doi: 10.1097/01.blo.0000141902.30946.6d. [DOI] [PubMed] [Google Scholar]
- 22.Lakshmanan P, Ahmed SM, Hansford RG, Woodnutt DJ. Achieving the required medial offset and limb length in total hip arthroplasty. Acta Orthop Belg. 2008;74:49–53. [PubMed] [Google Scholar]
- 23.Paratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89(3):494–499. doi: 10.2106/JBJS.F.00529. [DOI] [PubMed] [Google Scholar]
- 24.Parvizi J, Sharkey PF, Bissett GA, Rothman RH, Hozack WJ. Surgical treatment of limb-length discrepancy following total hip arthroplasty. J Bone Joint Surg Am. 2003;85-A(12):2310–2317. doi: 10.2106/00004623-200312000-00007. [DOI] [PubMed] [Google Scholar]
- 25.Renkawitz T, Sendtner E, Grifka J, Kalteis J. Accuracy of imageless stem navigation during simulated total hip arthroplasty. Acta Orthop. 2008;79(6):785–788. doi: 10.1080/17453670810016858. [DOI] [PubMed] [Google Scholar]
- 26.Renkawitz T, Schuster T, Herold T, Goessmann H, Sendtner E, Grifta J, Kalteis J. Measuring leg length and offset with an imageless navigation system during total hip arthroplasty: is it really accurate? Int J Med Robot. 2009;5(2):192–197. doi: 10.1002/rcs.250. [DOI] [PubMed] [Google Scholar]
- 27.Rubash HE, Parvataneni HK. The pants too short, the leg too long: leg length inequality after THA. Orthopedics. 2007;30:764–765. doi: 10.3928/01477447-20070901-30. [DOI] [PubMed] [Google Scholar]
- 28.Sarin VK, Pratt WR, Bradley GW. Accurate femur repositioning is critical during intraoperative total hip arthroplasty length and offset assessment. J Arthroplasty. 2005;20(7):887–891. doi: 10.1016/j.arth.2004.07.001. [DOI] [PubMed] [Google Scholar]
- 29.Sathappan SS, Teicher ML, Capeci C, Yoon M, Wasserman BR, Jaffe WL. Clinical outcome of total hip arthroplasty using the normalized and proportionalized femoral stem with a minimum 20-year follow-up. J Arthroplasty. 2007;22(3):356–362. doi: 10.1016/j.arth.2006.04.004. [DOI] [PubMed] [Google Scholar]
- 30.Shiramizu K, Naito M, Shitama T, Nakamura Y, Shitama H. L-shaped caliper for limb length measurement during total hip arthroplasty. J Bone Joint Surg Br. 2004;86:966–969. doi: 10.1302/0301-620X.86B7.14587. [DOI] [PubMed] [Google Scholar]
- 31.Takigami I, Itokazu M, Itoh Y, Mtasumoto K, Yamamoto T, Shimizu K. Limb-length measurement in total hip arthroplasty using a calipers dual pin retractor. Bull NYU Hosp Jt Dis. 2008;66(2):107–110. [PubMed] [Google Scholar]
- 32.White TO, Dougall TW. Arthroplasty of the hip. Leg length is not important. J Bone Joint Surg Br. 2002;84(3):335–338. doi: 10.1302/0301-620X.84B3.12460. [DOI] [PubMed] [Google Scholar]
- 33.Wixson RL. Computer-assisted total hip navigation. Instr Course Lect. 2008;57:707–720. [PubMed] [Google Scholar]
- 34.Wylde V, Whitehouse SL, Taylor AH, Pattison GT, Bannister GC, Blom AW. Prevalence and functional impact of patient-perceived leg length discrepancy after hip replacement. Int Orthop. 2009;33(4):905–909. doi: 10.1007/s00264-008-0563-6. [DOI] [PMC free article] [PubMed] [Google Scholar]