Abstract
Our goal was to evaluate the objective and subjective midterm outcome after revision of a failed shoulder arthroplasty with a reverse design prosthesis. Twenty consecutive patients with 21 revisions of a primary shoulder arthroplasty using reverse shoulder prosthesis Delta III® were followed up postoperatively for a mean of 46 months including clinical and radiological examination. Complications were recorded and Constant score, DASH and SF36 were assessed. With the numbers given a significant reduction of pain was achieved from 8.7 to 3.0 (p < 0.001). There was a significant improvement of active flexion from 43° to 97° (p < 0.001) and active abduction from 44° to 90° (p < 0.001). However, at the same time, active external rotation with an adducted humerus decreased significantly from 26° to 12° (p = 0.012). The constant score improved significantly from 16.7 to 55.9 (p < 0.001). Sixteen patients (84%) rated their shoulder better or much better than before. In 43% an intraoperative and in 38% a postoperative complication occurred including two late stage infections which required prosthesis removal. Our results support the use of the reverse prosthesis as revision prosthesis. The reverse design helps to compensate functional deficits due to severe soft-tissue damage except active external rotation. Nevertheless, the revision is a technically demanding procedure reflected in a high rate of intraoperative complications. The rate of secondary infections of 10% remains a special concern.
Introduction
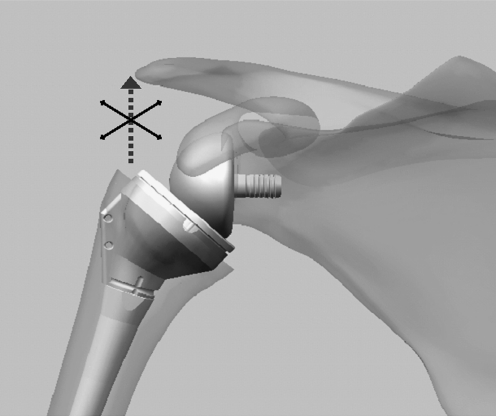
The surgical treatment of shoulder joint destruction by means of total shoulder arthroplasty has led to satisfactory results in the past and the present. Primary and secondary shoulder joint destruction, can both be reconstructed successfully with promising good mid- and long-term results [8, 13, 17, 19, 20]. However, potential complications and failures cannot be overlooked [1]. One of the most common long-term complications after conventional shoulder joint replacement is the secondary rupture of the rotator cuff. The loss of the depressor function of the cuff may lead to anterocranial migration of the humeral head [11, 21], usually associated with very severe pain in combination with a distinct loss of function. These problems are often disabling for the patient and therefore require revision. However, results of revision surgery using anatomical prosthesis designs are often disappointing [3, 18, 22, 27]. The reverse shoulder prosthesis design has demonstrated its capability in the treatment of a similar biomechanical problem, the rotator cuff arthropathy, both in short- and midterm results [2, 5, 10, 30]. The humerus is stabilised by the reverse semi-constrained design of the prosthesis against the cranial pull of the deltoid musculature (Fig. 1) [6].
Fig. 1.
Delta III prosthesis (DePuy). The semi-constrained design stabilises the humeral head against the anterocranial directed force of the deltoid muscle
Therefore, this prosthesis design offers potential as a revision prosthesis for antero-cranially unstable humeral head prostheses because the reduced cranial stability and/or migration are counteracted biomechanically. For this reason reverse shoulder arthroplasty has been regularly used as a salvage procedure for these cases in our institution since the year 2000. However, the revision situation differs substantially in several respects from the primary situation. Many factors including scarring, previous operations and malpositioning may influence the final result, in particular conditions of pain and subsequent quality of life.
There is only a small amount of evidence that solving the mechanical problem leads automatically to improved patient satisfaction [5, 28]. Therefore, a midterm analysis of the first cohort of our revision operations by means of reverse prosthesis from our institute was undertaken, with a special focus on factors such as mitigation of pain, daily activities and quality of life, in order to quantify success of the operation.
Patients and methods
Twenty patients with 21 implants (one bilateral) who underwent replacement of a primary shoulder arthroplasty using reverse shoulder prosthesis Delta III (DePuy France, Saint Priest CEDEX, France) were included in the study. Of these, ten were performed by the author and 11 by two co-authors (HKS and BRS). The inclusion period was from November 2000 until December 2005. The reason for the prosthesis change was, in all but one case, painful loss of function due to a rotator cuff insufficiency of the unrevised shoulder prosthesis. The exception was a patient who received a Delta III prosthesis following infection with proprioni bacterium acnes leading to the removal of the shoulder prosthesis and a three-month course of antibiotic therapy. The reduced function of the rotator cuff presented the same biomechanical problem as the other patients and so this patient was also included in the study.
Surgical technique
Within the Shoulder Department of our institution, between 150 and 200 shoulders replacements are performed annually (50% anatomical and 50% reverse prostheses) and 40 revision arthroplasties. The revision operation was performed in each case by means of the deltopectoral groove approach. The pronounced sub-deltoidal scar tissue was removed as well as the scarring surrounding the conjoined tendon. The axillary nerve was palpated. If present, remains of the subscapular tendon were detached from the lesser tuberosity of the humerus and mobilised. After sectioning the entire inferior scar the humeral head was luxated. All the prostheses except for one were cemented components. These could all be extracted from the humerus using axial blows. The cement was removed by means of chisels and high frequency cutters. In one case a humeral fenestration was performed for cement removal. Firmly set cement, which did not obstruct reimplantation, was left in situ except for the infected prosthesis. Subsequently, the glenoid was exposed followed by a complete circular capsulotomy. If present, the cemented glenoid component was removed. The glenoid preparation and implantation of the glenoid component—the glenosphere—was completed in the standard manner. If present, a shaft fissure of the humerus was fixed by means of cerclage wires, and fixation threads were pulled through the lesser tuberosity. Subsequently, the humerus components were cemented and the prosthesis was repositioned in the joint. If present, the subscapular tendon was refixed transosseously using the threads pulled through the lesser tuberosity followed by a layer-by-layer wound closure. Postoperative treatment included a sling over four weeks, with active assisted movement up to the horizontal and up to 0° external rotation. Subsequently, this was followed by four weeks of free mobilisation and the build-up of strength after eight weeks.
The initial diagnosis for shoulder arthroplasty had been a humeral head fracture in ten patients; these were treated with humeral head prostheses. A rotator cuff arthropathy was found in five patients; these were treated with a total prosthesis. The infected prosthesis was one of these two total arthroplasties. From the patient sample, three patients suffered from an arthritic joint destruction due to rheumatoid arthritis, two had osteoarthritis and one had avascular humeral head necrosis. The baseline data can be seen in Table 1.
Table 1.
Baseline data
| Characteristic | Value |
|---|---|
| Patients/shoulders | 20/21 |
| Gender (female/male) | 17/3 |
| Side (right/left) | 10/11 |
| Dominant/non-dominant | 15/6 |
| Follow-up, mean (range) | 46 months, (12–78) |
| Number of previous operations, mean (range) | 2 (1–4) |
| Implant exchanged | 21 (16 hemi-APL, 5 total APL) |
| Initial diagnosis | |
| Fracture | 10 (10 hemi) |
| Cuff tear arthropathy | 5 (2 hemi / 3 total) |
| Rheumatoid arthritis | 3 (2 hemi / 1 total) |
| Osteoarthritis | 2 (1 hemi / 1 total) |
| Avascular necrosis | 1 (1 hemi) |
| Reason for revision | |
| Anterocranial migration | 18 |
| Unstable arthroplasty | 2 |
| Infected arthroplasty | 1 |
Operation time, intraoperative blood loss as well as intra- and postoperative complications were recorded. Pain was recorded on a visual analogue scale pre- and postoperatively with a value of 10 noted for maximum pain and 0 for no pain.
The patients were examined after a mean mid-term follow-up of 46 months (range 12–78). Apart from the objective clinical parameters, pain, mobility and strength (measured with a spring balance), as well as Constant score (CS) [7] (maximum 100, minimum 0); disability of arm, shoulder and hand score (DASH) [12] (minimum 0, maximum 100); and Short Form 36 (SF 36) [29] were used as outcome parameters. This was done using the preoperative data from the clinical histories of the patients allowing calculation of the preoperative Constant score. At the time of re-examination the scores were collected using a standard questionnaire [23].
General satisfaction with the operation was ascertained with the standard questions “How is my situation now compared with the situation before surgery” (possible answers: much worse, worse, better or much better), “are you satisfied with the operation?” (0 = not at all, 10 = completely) and “would you undergo the same operation under the same circumstances again?” (possible answers: yes, no, I don’t know).
A true anteroposterior (AP) radiograph, parallel to the glenoid, was taken at follow-up. The shoulder joint was adjusted under image intensifier control to ensure that the paths of the X-rays were exactly parallel to the glenoid. Signs for lysis, as well as changes of position of the components, were recorded for all components. Notching of the inferior glenoid was also investigated using the true AP radiographs and graded as described by Sirveaux et al. [25]. The statistical analysis was performed using a paired t-test for normal distributed samples as well as Wilcoxon-and Mann-Whitney U-Test for non-normal distributed data. The level of significance was set at p = 0.05.
Results
Two (9.5%) of the 21 reverse shoulder arthroplasties had to be removed again because of late stage low grade infection, in one case with Streptococcus mitis/oralis after nine months and in the other with Staphylococcus epidermidis after 32 months. Due to progression of the infectious disease after explantation into a chronic osteomyelitis, no reimplantation was performed. In the following sections, these two cases are excluded from the results but are described separately.
A significant improvement in the pain level following operation was achieved, from 8.7 (range 2–10) preoperatively to 3.0 (range 0–9) (p < 0.001) postoperatively.
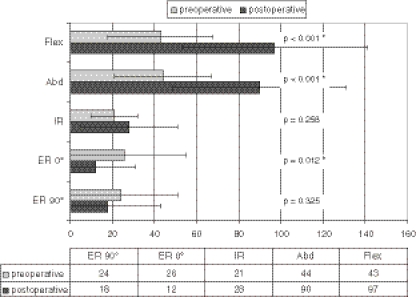
There was a significant improvement of active flexion and active abduction. Active internal rotation increased, although not significantly. Active external rotation in adduction decreased significantly and active external rotation at 90° of abduction decreased insignificantly. This corresponds to an increase of positive external rotation lag signs from 13 patients (68%) preoperatively to 18 patients (95%) postoperatively.
The detailed values and the changes in the ROM after operation can be seen in Fig. 2.
Fig. 2.
Range of motion (ROM) pre- and postoperatively. Flex flexion, Abd abduction, IR internal rotation, ER external rotation, * indicates significant value
The preoperative abduction strength increased significantly from 0.1 kg (range 0–2) preoperatively to 3.9 kg (range 0–10) (p = 0.001) postoperatively.
One glenoid component loosened 39 months after surgery without dislocation of the humeral component in a patient with rheumatoid arthritis. A radiolucent line around the metaphyseal part of the humeral component was found in one case (5%), but there were no radiolucencies around the humeral stem. Of the 18 cases with a stable glenoid component, a notching of the inferior glenoid occurred in 13 cases (72%). Of these, five showed grade I (28%), four grade II (22%), three grade III (17%) and one grade IV (6%). No correlation was found between the presence or grade of notching and the clinical result of pain (subscore of the Constant score, p = 0.467) and active flexion (p = 0.409).
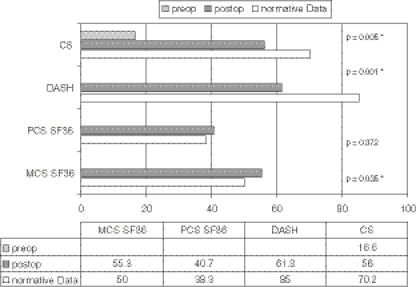
As a result of the operation, the Constant score showed a significant improvement but still considerably below age related norms. This was also true for the postoperative DASH score. The postoperative physical component summary (PCS) and of the SF36 showed no significant difference to the normal value. The mental component summary (MCS) of the SF36 was significantly better than the norm value. The detailed values are shown in Fig. 3. No significant correlation was found between the outcome in the CS (p = 0.295) and the initial diagnosis or the time between the first prosthesis and the revision surgery.
Fig. 3.
Score results with normative data (* significant value)
Patient satisfaction For the question “How is my situation now compared with the situation before surgery?”, one patient answered much worse (5%), two with worse (11%), four with better (21%) and 12 with much better (63%). Mean value of satisfaction with the surgery was 7.6 (range 0–10). From the sample, 16 patients stated that they would have the surgery again (84%), one patient would not do it again (5%) and one patient could not make a decision about this question (5%).
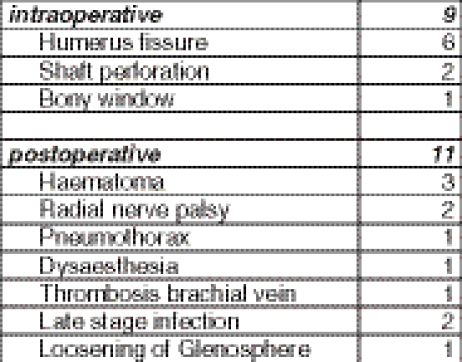
Procedure and complications The average duration of the procedure was 236 min (range 140–337) and the intra-operative blood loss was 641 ml (range 250–2000).From the initial 21 procedures, 12 (57%) were uneventful while in nine cases (43%) an intraoperative complication occurred. Details are shown in Fig. 4. The fissures were fixed with cerclage wires with an uneventful bone healing. Postoperatively, eight patients (38%) of the initial cohort of 21 patients, including the patients with the late stage infections, had a total of 11 complications. Details are shown in Fig. 4.One glenosphere (5%) was loosened 39 months after revision surgery in a patient with rheumatoid arthritis Fig. 5. As mentioned before, two arthroplasties (9.5%) had to be removed because of late stage low grade infection. The re-operation rate overall was 9.5%.Both patients with late stage infection had the same treatment after implant removal [14]. After an initial period of 12 weeks with antibiotics according to the bacterial resistance, they showed a relapse of the infection. Despite a revision with debridement of both the soft tissue and the bone and a further 12-week period with antibiotics, there were still signs of infection including signs of a chronic osteomyelitis in the MRI. Therefore it was decided that reimplantation would not occur. One year after explantation, despite an almost complete loss of function, both patients described a fair satisfaction score of 4 (range 0–10) Fig. 6.
Fig. 4.
Intra- and postoperative complications of the initial cohort of 21 patients including the patients with late stage infections
Fig. 5.
Fifty nine year old female patient with a long standing rheumatoid arthritis. Intraoperative fracture of the major tubercle, fixation with transosseous sutures. Six months after surgery with good integration of the major tubercle (left). Loosening of the Glenosphere 39 months after surgery (right)
Fig. 6.
A 62-year-old female patient. Left One year after revision arthroplasty with clinical signs of late stage infection (Streptococcus mitis/oralis). Center i.v.-gadolinium enhanced MRI with signs of a persisting chronic osteomyelitis after implant removal. Right Definitive resection situation after debridement
Discussion
Both patient satisfaction and objective parameters indicated that reverse shoulder arthroplasty is a viable option to rescue shoulder function after failed primary shoulder arthroplasty.
Patient satisfaction with the revision surgery can also be clinically confirmed and mirrors the psychological well-being of the SF-36. With the numbers given, a significant pain reduction is accompanied by a clear improvement in mobility. These interpretations are supported by a significant improvement in the Constant score. These results correspond to those previously reported in the literature [5, 10]. A result was achieved which allows the patient to carry out day-to-day activities up to chest height with little pain. However, at shoulder level and higher, no powerful use of the arm can be expected, a result that is typically worse than with the primary use of the reverse prosthesis [5, 10, 30]. Not surprisingly, the scores (Constant and DASH) showed significant deficits postoperatively compared to normative data.
Although the indications for the primary implantation of the prostheses were different, the biomechanical problem before the revision operation was initially the same in each case: anterocranial migration of the humeral component. Therefore, in the authors’ opinion this justifies a common approach. This procedure showed itself to be appropriate in that there was no correlation between the results and the initial diagnosis. It can be concluded that the migration not only biomechanically represents the main problem and leads to functional loss, but that it is also the main cause of pain in cases of very different aetiology.
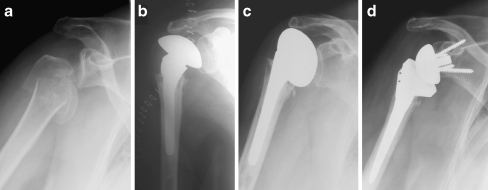
However, in comparison to conventional, primary implanted total shoulder prostheses, the expected functional results were clearly worse [8, 17, 19, 20]. This can be explained by the severe structural damage of the rotator cuff and the postoperative scarring (Fig. 7).
Fig. 7.
Four-part fracture of the humeral head treated elsewhere with a humeral head prosthesis (a). Missing greater tuberosity in the postoperative X-ray (b). Six-month postop cranialisation of the prosthesis (c). After revision with a reverse prosthesis Delta III (d)
Complete improvement of shoulder function cannot be expected despite significant improvements in all domains. Patients reported a massive reduction in pain but most did not become pain-free. Additionally, although mobility significantly improved, it was not restored to normal movement. The restoration of active external rotation presents a special challenge. The active external rotation after surgery was significantly worse than before the intervention, associated with an increase in the rate of positive external rotation lag signs. Only one patient was able to hold the arm actively in a neutral rotation position after the revision. The increasing loss of the external rotators (infraspinatus and teres minor) reflects the intraoperative bone loss of the proximal humerus—especially on the greater tuberosity—due to the technical difficulties of cement removal. This leads to a considerable handicap in daily life as even light objects, such as a glass or spoon, cannot be held by the externally rotated arm. A possible solution to this problem is the combination of the reverse prosthesis with a latissimus dorsi transfer [15]. This combined procedure was proven effective in the primary implantation of a reverse prosthesis [4, 9]. However, data about the revision situation has not yet been published. In the future, modular prostheses in which the humeral stem can be left in place while only revising the head to a reverse design might improve these results [24].
Despite the promising results, intra- and postoperative complications remain a matter of concern, with an intraoperative complication rate of 43% and postoperative of 38%. These complication rates are higher than after primary implantation of the prosthesis [5, 25, 28, 30].
The main intraoperative complication of this operation is the shaft fissure. This again reflects the difficulties of cement removal combined with often very atrophic bone resulting in a long operation with significant blood loss. The fissures were fixed with cerclage wires, and in all cases sufficiently stable conditions were obtained for stable cementation. However, the process of putting cerclages around the humerus is accompanied by significant stretching of the soft tissues and the authors consider that the three transient nerve problems were due to nerve stretching during fixation of the shaft fissures. Therefore, in cases of cement removal difficulty, a primary shaft osteotomy or humeral bone fenestration [26] should at least be considered as the less traumatic procedure. This method was successfully used in one patient.
The most serious complication remains infection. While there were no acute infections, two cases of late stage infections occurred (9.5%). Both cases developed a chronic osteomyelitis despite removal of the prosthesis with adequate antibiotic treatment. Therefore both shoulders remained in the status of a definitive resection arthroplasty.
While there is no comparable data in literature about intra-operative complications, the postoperative complication rates published are comparable with ours. Boileau et al. reported a complication rate of 47% and an infection rate of 16% after 40 months [5], and Wall et al. reported 37% complications after 40 months [28]; both studies were performed with the same prosthesis. Levy et al. reported 48% of complications with a different reverse prosthesis design [16].
The main question of this study was the general suitability of the revision operation using a reverse prosthesis. This question can be adequately answered after a follow-up period of almost four years. The reverse prosthesis offers a possible solution to former, practically hopeless, situations which placed great strain on patients, and it is justified by currently available data that this operation should be pursued further. So far, 95% of the prostheses are radiologically stable and well-centred; only one glenosphere loosened 39 months after revision surgery in a patient with a long-standing rheumatoid arthritis and therefore very poor bone stock on the glenoid side. This loosening was interpreted as a complete failure of fixation in the osteoporotic bone and not a consequence of glenoid notching. However, in line with other studies [5, 28, 30], 72% of the cases showed notching on the inferior glenoid. While the notching in four patients clearly reached further cranial beyond the lowest screw (grades III & IV), this notching never led to a loosening of the prosthesis. In addition, no correlation could be found between the notching and the clinical result, a fact that is also reported in literature [5, 28, 30]. The long-term consequences of this notching remain unclear. It is assumed that the notching is progressive and can therefore eventually lead to a loosening of the prosthesis which might explain the functional deterioration after six years reported by Guery et al. [10]. This hypothesis can only be verified using long-term studies. Based on the results of primary implantation published so far, a favourable midterm, if not long-term, process can be assumed. However, since the revision situation differs greatly from the primary situation, especially with regard to the soft tissues, these results cannot be assumed. Long-term follow-ups are absolutely necessary in order to verify the suitability of the method in the long term.
Acknowledgement
The authors would like to thank Susann Drerup for the data management.
Conflict of interest statement The authors declare that they have no conflict of interest
References
- 1.Aldinger PR, Raiss P, Rickert M, Loew M (2009) Complications in shoulder arthroplasty: an analysis of 485 cases. Int Orthop. doi:10.1007/s00264-009-0780-7 [DOI] [PMC free article] [PubMed]
- 2.Baulot E, Chabernaud D, Grammont PM. Results of Grammont’s inverted prosthesis in omarthritis associated with major cuff destruction. Apropos of 16 cases. Acta Orthop Belg. 1995;61(Suppl 1):112–119. [PubMed] [Google Scholar]
- 3.Berth A, Pap G. Hemi-versus bipolar shoulder arthroplasty for chronic rotator cuff arthropathy. Int Orthop. 2008;32(6):735–740. doi: 10.1007/s00264-007-0394-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Boileau P, Chuinard C, Roussanne Y, Bicknell RT, Rochet N, Trojani C. Reverse shoulder arthroplasty combined with a modified latissimus dorsi and teres major tendon transfer for shoulder pseudoparalysis associated with dropping arm. Clin Orthop Relat Res. 2008;466(3):584–593. doi: 10.1007/s11999-008-0114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15(5):527–540. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 6.Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg. 2005;14(1 Suppl S):147S–161S. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 7.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 8.Edwards TB, Kadakia NR, Boulahia A, Kempf JF, Boileau P, Nemoz C, Walch G. A comparison of hemiarthroplasty and total shoulder arthroplasty in the treatment of primary glenohumeral osteoarthritis: results of a multicenter study. J Shoulder Elbow Surg. 2003;12(3):207–213. doi: 10.1016/S1058-2746(02)86804-5. [DOI] [PubMed] [Google Scholar]
- 9.Favre P, Loeb MD, Helmy N, Gerber C. Latissimus dorsi transfer to restore external rotation with reverse shoulder arthroplasty: a biomechanical study. J Shoulder Elbow Surg. 2008;17(4):650–658. doi: 10.1016/j.jse.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 10.Guery J, Favard L, Sirveaux F, Oudet D, Mole D, Walch G. Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am. 2006;88(8):1742–1747. doi: 10.2106/JBJS.E.00851. [DOI] [PubMed] [Google Scholar]
- 11.Hsu HC, Luo ZP, Cofield RH, An KN. Influence of rotator cuff tearing on glenohumeral stability. J Shoulder Elbow Surg. 1997;6(5):413–422. doi: 10.1016/S1058-2746(97)70047-8. [DOI] [PubMed] [Google Scholar]
- 12.Hudak PL, Amadio PC, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG) Am J Ind Med. 1996;29(6):602–608. doi: 10.1002/(SICI)1097-0274(199606)29:6<602::AID-AJIM4>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 13.John M, Pap G, Angst F, Flury MP, Lieske S, Schwyzer HK, Simmen BR. Short-term results after reversed shoulder arthroplasty (Delta III) in patients with rheumatoid arthritis and irreparable rotator cuff tear. Int Orthop. 2010;34(1):71–77. doi: 10.1007/s00264-009-0733-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kirchhoff C, Braunstein V, Buhmann Kirchhoff S, Oedekoven T, Mutschler W, Biberthaler P. Stage-dependant management of septic arthritis of the shoulder in adults. Int Orthop. 2009;33(4):1015–1024. doi: 10.1007/s00264-008-0598-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lehmann LJ, Mauerman E, Strube T, Laibacher K, Scharf HP (2009) Modified minimally invasive latissimus dorsi transfer in the treatment of massive rotator cuff tears: a two-year follow-up of 26 consecutive patients. Int Orthop. doi:10.1007/s00264-009-0782-5 [DOI] [PMC free article] [PubMed]
- 16.Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007;89(2):189–195. doi: 10.2106/JBJS.E.01310. [DOI] [PubMed] [Google Scholar]
- 17.Mansat P, Mansat M, Bellumore Y, Rongieres M, Bonnevialle P. Mid-term results of shoulder arthroplasty for primary osteoarthritis. Rev Chir Orthop Reparatrice Appar Mot. 2002;88(6):544–552. [PubMed] [Google Scholar]
- 18.Neer CS, 2nd, Kirby RM. Revision of humeral head and total shoulder arthroplasties. Clin Orthop. 1982;170:189–195. [PubMed] [Google Scholar]
- 19.Norris TR, Iannotti JP. Functional outcome after shoulder arthroplasty for primary osteoarthritis: a multicenter study. J Shoulder Elbow Surg. 2002;11(2):130–135. doi: 10.1067/mse.2002.121146. [DOI] [PubMed] [Google Scholar]
- 20.Orfaly RM, Rockwood CA, Jr, Esenyel CZ, Wirth MA. A prospective functional outcome study of shoulder arthroplasty for osteoarthritis with an intact rotator cuff. J Shoulder Elbow Surg. 2003;12(3):214–221. doi: 10.1016/S1058-2746(02)86882-3. [DOI] [PubMed] [Google Scholar]
- 21.Paletta GA, Jr, Warner JJ, Warren RF, Deutsch A, Altchek DW. Shoulder kinematics with two-plane X-ray evaluation in patients with anterior instability or rotator cuff tearing. J Shoulder Elbow Surg. 1997;6(6):516–527. doi: 10.1016/S1058-2746(97)90084-7. [DOI] [PubMed] [Google Scholar]
- 22.Petersen SA, Hawkins RJ. Revision of failed total shoulder arthroplasty. Orthop Clin North Am. 1998;29(3):519–533. doi: 10.1016/S0030-5898(05)70026-2. [DOI] [PubMed] [Google Scholar]
- 23.Simmen BR, Angst F, Schwyzer HK, Herren DB, Pap G, Aeschlimann A, Goldhahn J. A concept for comprehensively measuring health, function and quality of life following orthopaedic interventions of the upper extremity. Arch Orthop Trauma Surg. 2009;129(1):113–118. doi: 10.1007/s00402-008-0718-3. [DOI] [PubMed] [Google Scholar]
- 24.Simmen BR, Schwyzer HK, Flury MP, Goldhahn J. In situ assembly of a modular noncemented total shoulder prosthesis for the reconstruction of complex joint pathology. Oper Orthop Traumatol. 2009;21(1):35–50. doi: 10.1007/s00064-009-1604-z. [DOI] [PubMed] [Google Scholar]
- 25.Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg Br. 2004;86(3):388–395. doi: 10.1302/0301-620X.86B3.14024. [DOI] [PubMed] [Google Scholar]
- 26.Sperling JW, Cofield RH. Humeral windows in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(3):258–263. doi: 10.1016/j.jse.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 27.Sperling JW, Cofield RH. Revision total shoulder arthroplasty for the treatment of glenoid arthrosis. J Bone Joint Surg Am. 1998;80(6):860–867. doi: 10.2106/00004623-199806000-00010. [DOI] [PubMed] [Google Scholar]
- 28.Wall B, Nove-Josserand L, O'Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg Am. 2007;89(7):1476–1485. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- 29.Ware JE, Jr, Gandek B. Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol. 1998;51(11):903–912. doi: 10.1016/S0895-4356(98)00081-X. [DOI] [PubMed] [Google Scholar]
- 30.Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87(7):1476–1486. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]