This study examines the value of the Edmonton Symptom Assessment System (ESAS), a measure of symptom burden adopted by Ontario's cancer centers, among clinical teams and barriers to its use in the enhancement of multidisciplinary care.
Abstract
Purpose:
Despite growing implementation of electronic symptom assessment in oncology settings, few studies have described how standardized symptom assessment can enhance multidisciplinary care. The Edmonton Symptom Assessment System (ESAS) is a validated measure of symptom burden that has been adopted by Ontario's cancer centers to assess symptoms for patients with cancer. This study examines the perceived value of the ESAS among clinical teams and barriers to its use in enhancing multidisciplinary care.
Methods:
Self-completed surveys were administered online to clinical teams at various disease-site clinics at a cancer center in Ontario, Canada.
Results:
One hundred twenty-eight nurses, oncology physicians, and allied health professions completed the survey. The majority of nurses (89%), physicians (55%), and other providers (57%) reported referring to ESAS in clinic either “always” or “most of the time.” Many of those who either “never” or “rarely” looked at ESAS scores reported finding it more efficient to talk to the patient or do their own assessment to determine symptom issues. Although most of the nurses and allied health professions found the ESAS to enhance patient care, help patients to articulate their symptom issues, and facilitate follow-up with patients with past symptom issues, only approximately half of the physicians agreed with these statements.
Conclusion:
Variable adoption of the ESAS by physicians may limit its potential to improve both interprofessional communication and comprehensive symptom control. To encourage consistent use, a symptom assessment system needs to be complementary to the perceived roles of all multidisciplinary team members, including physicians.
Introduction
Adequately addressing symptom needs of patients with cancer often requires the involvement of multidisciplinary providers.1,2 Nurses and doctors may screen and manage physical symptoms, such as pain and nausea, while other health care providers, such as social workers, focus on psychological and emotional supportive care issues. Evidence shows, however, that providers often under-recognize symptom burden in patients,3,4 with studies demonstrating that patients with cancer have significant symptom issues such as distress, fatigue, nausea, anxiety, and depression.5–7
Standardized symptom assessment in cancer care is purported to help providers better identify symptom needs, improve symptom management, and facilitate multidisciplinary care. Multiple validated tools exist to measure cancer symptoms.1 Moreover, electronic symptom assessment systems have been successfully implemented in oncology settings.8–10 Yet few studies have investigated providers' perceptions of how a symptom assessment system can improve multidisciplinary care for patients with cancer.
In 2007, all cancer centers in Ontario, Canada, began implementing the use of an electronic version of the Edmonton Symptom Assessment Scale (ESAS) at every patient visit, thus effectively standardizing cancer symptom screening across the province.11 The ESAS is a patient-reported, validated tool developed for quick assessment of symptom needs in routine practice.12–15 This instrument measures the severity (scale of 0 to 10) of nine common cancer physical and psychological symptoms, specifically pain, shortness of breath, nausea, anxiety, depression, tiredness, drowsiness, appetite, and well-being. In addition to Canada, the United Kingdom, the United States, and other countries have used the ESAS in oncology settings.16–18
The screening of symptoms occurs at each patient's visit to a cancer center, including first consultation and follow-up visits. Upon arrival at the center, patients have the option of electronically completing the ESAS at a touch-screen kiosk. A printed summary of the symptom scores, including those from previous visits, is then given to the patient to use for discussion with the clinical primary care team, which is composed of the nurse and oncology physician, during the visit. If the patient has high ESAS scores, ideally the clinical team will discuss a care plan with the patient that addresses the symptoms and will make a referral to other multidisciplinary providers as appropriate.
The patient-reported ESAS scores are meant to facilitate dialogue about symptom needs between the patient and health care providers, while encouraging multidisciplinary care and treatment through referrals to other members of the team as required. This study specifically explores how the electronic, standardized ESAS symptom assessment system implemented in Ontario is being used by providers in multidisciplinary teams, its perceived utility, and barriers to its use at a regional cancer center.
Methods
Design, Setting, and Participants
An online survey was administered to all clinical teams at the Juravinski Cancer Centre (JCC) in Hamilton, Ontario. The JCC is a regional cancer center in southern Ontario, serving approximately 23,000 individual patients annually, including more than 5,000 new patients, resulting in more than 200,000 patient encounters per year. Since March 2009, approximately 3,500 to 4,000 ESAS reports have been completed each month at the JCC, with the ESAS completed at approximately 50% of visits. All providers in clinical primary teams at the JCC were invited to participate in the survey. The team members included physicians (ie, general practitioner in oncology, medical oncologist, radiation oncologist, and surgical oncologist), nurses (ie, advanced practice nurse, registered nurse, and specialized oncology nurse), and allied health professionals (eg, social worker, dietician, chaplain, etc).
Survey
The research team developed the unique survey on the basis of the relevant literature, expert opinion from multidisciplinary perspectives, and previously used questions.19 The final 13 questions selected were pilot tested for clarity and relevance by nurses and physicians from another regional cancer center. The main questions focused on (1) the demographics of the providers; (2) the extent to which the providers use the ESAS and reasons why they might not use it; (3) the process of how they use the ESAS, if they do; (4) perceptions of the ESAS's usefulness to their clinical practice, rated on a four-point Likert scale ranging from “strongly agree” to “strongly disagree”; and (5) suggestions for improving the utility of ESAS in the clinical setting.
The research team conducted the survey in March 2010. The Web link to the online survey was e-mailed to all clinical staff at the JCC. Subsequent weekly reminder e-mails and a letter from the JCC president were sent to encourage participation over the 3 weeks that followed. Analysis of survey responses was descriptive, examining the results of the questions by provider type. We dichotomized the four-point scales for ease of reporting. Open-ended responses were coded, and themes were extracted. Ethics approval was obtained from the McMaster University Ethics Review Board (Hamilton, Ontario, Canada).
Results
Of a sample of 239 providers, 128 completed the survey, yielding a response rate of 53.6%. The pilot testing did not result in any revision of the survey instrument, therefore these responses (n = 33) were included. Respondents consisted of 51.6% nurses (n = 66), 36.7% oncology physicians (n = 47), and 11.7% allied health professions (n = 15). Women comprised 72% of respondents, reflective of the gender imbalance among nurses, who represent more than half the sample. Table 1 reports the characteristics of the respondent providers, constituting a variety of disease-site teams.
Table 1.
Characteristics of Clinician Respondents (N = 128)
| Sample Characteristic | No. | % |
|---|---|---|
| Sex | ||
| Female | 92 | 71.9 |
| Male | 36 | 28.1 |
| Profession | ||
| Nurse total | 66 | 51.6 |
| Advanced practice nurse | 5 | 11.7 |
| Registered nurse | 37 | 28.9 |
| Registered nurse CON(c) | 24 | 18.8 |
| Oncology physician total | 47 | 36.7 |
| General practitioner in oncology* | 6 | 4.7 |
| Medical oncologist | 14 | 10.9 |
| Radiation oncologist | 21 | 16.4 |
| Surgical oncologist | 6 | 4.7 |
| Other provider | 15 | 11.7 |
| Affiliated disease site(s)† | ||
| Breast | 72 | 56.3 |
| Gastrointestinal | 51 | 39.8 |
| Genitourinary | 51 | 39.8 |
| Lung | 46 | 35.9 |
| Gynecologic | 37 | 28.9 |
| Head and neck | 25 | 19.5 |
| Other | 64 | 50.0 |
| Time in clinical practice, years | ||
| 0-5 | 12 | 9.4 |
| 6-10 | 19 | 14.8 |
| 11-15 | 19 | 14.8 |
| > 15 | 78 | 60.9 |
Abbreviation: CON(c), certified oncology nurse in Canada.
General practitioner in oncology refers to a general practitioner/internist who provides oncology care in the primary care or cancer center setting.20
Total is > 100% because most providers worked in multiple clinics
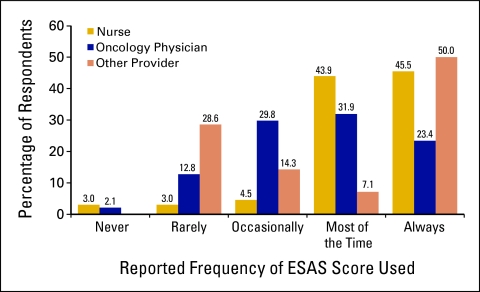
The majority of nurses (89%), physicians (55%), and other providers (57%) reported referring to the ESAS scores in clinic either “always” or “most of the time” (Fig 1). Differences were seen within the physician group, with general practitioners in oncology tending to use the ESAS more (100% used it “always” or “most of the time”) than medical and radiation oncologists (56%) and surgical oncologists (17%). Many of those who either “never” or “rarely” looked at ESAS scores reported finding it more efficient to talk to the patient and/or do their own assessment to determine symptom issues. Other common reasons provided for not using the ESAS at every visit were as follows: the scores were not given with the patient's chart (nurses, n = 10; physicians, n = 2); the clinic was too busy at that time (nurses, n = 3; physicians, n = 9); symptoms were not relevant to the patient visit (nurses, n = 3; physicians, n = 4), and other providers had already assessed the patient in clinic (nurses, n = 2; physicians, n = 3).
Figure 1.
Regularity with which providers look at patient's Edmonton Symptom Assessment System (ESAS) score when provided at the clinical visit (N = 128).
Table 2 presents providers' perceptions of the utility of the ESAS in their clinical practice. Although most of the nurses and allied health professions found the ESAS to enhance patient care (85% and 80%, respectively), help patients articulate their symptom issues (70% and 87%), and aid in following up with patients with past symptom issues (80% and 68%), only approximately half of the physicians agreed with these statements. Interestingly, the majority of providers (62% to 83%), across disciplines, indicated that patients often misinterpret the ESAS questions when completing the instrument. Radiation and surgical oncologists generally expressed that the ESAS was of the least value or benefit to them.
Table 2.
Providers' Perceived Utility of the ESAS
| Statement | Nurse |
Oncology Physician |
Other Provider |
|||
|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |
| ESAS enhances patient care | 55 | 84.6 | 24 | 51.1 | 12 | 80.0 |
| ESAS improves efficiency of the meeting with patient | 50 | 76.9 | 14 | 29.8 | 11 | 73.3 |
| ESAS enhances my assessment of patient's symptom severity | 50 | 76.9 | 25 | 53.2 | 11 | 73.3 |
| ESAS helps patients articulate their symptom issues | 45 | 70.3 | 21 | 44.7 | 13 | 86.7 |
| ESAS provides information on symptoms I don't routinely inquire about | 21 | 33.9 | 22 | 46.8 | 11 | 73.3 |
| Reviewing current scores is useful in clinical decision making | 44 | 67.7 | 21 | 44.7 | 10 | 66.7 |
| Reviewing trend of past scores is useful in clinical decision making | 50 | 78.1 | 19 | 42.2 | 9 | 69.2 |
| ESAS is useful during follow-up of a patient with past symptom issues | 51 | 79.7 | 21 | 44.7 | 10 | 66.7 |
| Patients often misinterpret the ESAS questions | 54 | 83.1 | 29 | 61.7 | 8 | 61.5 |
Almost half (45.3%) of the providers offered suggestions to improve the ESAS process. Among nursing responses, one third stated that patients need more initial instruction on how to properly complete the ESAS tool. Only physicians suggested using an ESAS tool that was disease-site specific. The most frequent suggestion was to ensure the availability of patients' past and present scores to providers in the clinic.
Discussion
This study is one of the first to examine multidisciplinary provider perspectives on the use and utility of the ESAS tool in a regional cancer center. This research illuminates some of the challenges of enhancing patient-centered, multidisciplinary care in a large cancer center through the implementation of standardized symptom assessment in the clinic setting.
Overcoming physician resistance to consistent use of the ESAS appears to be a major challenge in achieving multidisciplinary symptom assessment and management. Most providers reported using the ESAS in clinical visits to some extent; however, only a quarter of physicians reported using the ESAS “always,” compared with nearly half of nurses and other providers. Moreover, physicians consistently were less likely to agree on the usefulness of the ESAS on multiple dimensions of patient benefit compared with the other providers. Variable adoption of the ESAS by physicians may limit its potential to improve symptom control and interdisciplinary communication. Physicians play a key role in referring patients to other supportive care services, such as pain and symptom management clinics or psychological evaluations for depression.21–23 Without a formalized initial assessment, supportive care needs of patients with cancer may remain unmet.
Physicians stated that a main reason for not using the ESAS was their preference to assess symptoms on their own. Yet there is evidence that patients are often not asked about their symptoms and that symptom burden is under-recognized by physicians.3,4 As well, nonstandardized assessments pose challenges for the nonphysician providers in the team with regard to interpreting information and providing appropriate treatment. Another major reason for not looking at ESAS scores for physicians was working in a busy clinic. This is often the nature of clinical practice and was precisely the impetus behind mandating and standardizing symptom assessment across the province.24 The responses provided by specialized physicians may be indicative of a focus on their medical role in patient care, with less emphasis on multidimensional supportive care. Our results suggest that radiation oncologists and surgeons find it more efficient to center on treatment-related symptomatology rather than more comprehensive assessment. Encouraging physician adoption of the symptom assessment process might require providing tools that are useful in essential tasks and flow easily into physicians' practice patterns. Examples include longitudinal trend reporting, capture of symptoms of treatment-related toxicity,8 and matched education tools that are triggered by patient distress thresholds.25
High use of the ESAS among oncology nurses is not surprising given that their defined role includes in-depth assessment of patient needs, as well as facilitating continuity of care and decision making.26 Nurses play a key role in effective multidisciplinary care. They share information from their assessments with other providers on the clinical team, which results in patient interventions, referrals, and/or supportive counseling. This partially explains why a physician may not always look at the ESAS if a nurse has already used it for assessment in her scope of practice.
Despite some physician resistance to use of the ESAS, our results indicate that the tool likely improves symptom assessment and interdisciplinary communication and care. The vast majority of nurses and other providers, and nearly half of physicians, agree on the utility of the ESAS to improve various dimensions of patient care. These results emerge despite the fact that all three provider types also agree that patients often misinterpret the ESAS questions; this perception implies that these health professionals are indeed inquiring about ESAS symptoms, evidence that the tool successfully fulfills its role in symptom assessment. The ESAS is intended to lead to a discussion among the providers reviewing the scores and with the patient, not as an absolute measure of symptom severity. Quality patient-centered care requires patient input, which the ESAS facilitates. Moreover, nurses and physicians reported that one reason they did not use the ESAS at every clinic visit is because it was already examined by another provider, indicating that interdisciplinary communication is occurring in the clinic. Also, that the single most reported suggestion to improve ESAS was to provide the histogram of past symptom scores to providers supports the positive impact that this system has had on the care process.
The study is limited by not including patient perspectives on whether the ESAS helps manage symptom issues and by providing perspectives from only a single regional cancer center. Second, nonrespondents might have different perspectives, possibly more negative, the exclusion of which could have led to an overestimate of ESAS use. Finally, the limited use by physicians found in our study may be due to the nature of the ESAS tool itself, as it does not provide all pertinent symptom information required by physicians (eg, toxicity-related symptoms).
Our study may provide insights into the enhancement of multidisciplinary care in other facilities with standardized, patient-reported outcome systems. Our results show that members of the multidisciplinary team other than physicians are more able to undertake supportive care responsibilities; if this is true, an efficient and responsive system needs to take advantage of this finding. To encourage consistent use, a symptom assessment system needs to be complementary to the perceived roles of all team members, including physicians. The information provided must efficiently highlight outcomes of interest and streamline care provision, without overburdening patients with excessive questions.
Summary
The implementation of standardized ESAS symptom assessment in Ontario's regional cancer centers represents a unique opportunity to illuminate the challenges of managing cancer symptoms by a multidisciplinary team. Physicians appear more focused on their specialized scope of practice rather than on their role as a member of a larger multidisciplinary team. Nonetheless, standardizing symptom assessment appears to help improve interdisciplinary communication and patient care. Future research is needed to determine which universal symptom assessment system efficiently meets the needs of all providers in the multidisciplinary team.
Acknowledgment
This research was supported by a grant from the Juravinski Cancer Centre Foundation. We wish to acknowledge the Juravinski Cancer Centre and the Credit Valley Hospital, Peel Regional Cancer Program for their participation in the survey, and John Medeiros, Marie Hoy, Susan King, Sheldon Fine, and Robert Sauls for their assistance in refining the survey instrument and survey procedure.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Daryl Bainbridge, Hsien Seow, Jonathan Sussman, Greg Pond, Lorraine Martelli-Reid, William Evans
Financial support: Hsien Seow
Administrative support: Hsien Seow
Provision of study materials or patients: Daryl Bainbridge, Carole Herbert
Collection and assembly of data: Daryl Bainbridge, Lorraine Martelli-Reid, Carole Herbert
Data analysis and interpretation: Daryl Bainbridge, Hsien Seow, Jonathan Sussman, Greg Pond, Lorraine Martelli-Reid, William Evans
Manuscript writing: Daryl Bainbridge, Hsien Seow, Jonathan Sussman, Greg Pond, Lorraine Martelli-Reid, William Evans
Final approval of manuscript: Daryl Bainbridge, Hsien Seow, Jonathan Sussman, Greg Pond, Lorraine Martelli-Reid, Carole Herbert, William Evans
References
- 1.Kirkova J, Davis MP, Walsh D, et al. Cancer symptom assessment instruments: A systematic review. J Clin Oncol. 2006;24:1459–1473. doi: 10.1200/JCO.2005.02.8332. [DOI] [PubMed] [Google Scholar]
- 2.Naughton M, Homsi J. Symptom assessment in cancer patients. Curr Oncol Rep. 2002;4:256–263. doi: 10.1007/s11912-002-0024-0. [DOI] [PubMed] [Google Scholar]
- 3.Grossman SA. Undertreatment of cancer pain: Barriers and remedies. Support Care Cancer. 1993;1:74–78. doi: 10.1007/BF00366899. [DOI] [PubMed] [Google Scholar]
- 4.Portenoy RK. Cancer-related fatigue: An immense problem. Oncologist. 2000;5:350–352. doi: 10.1634/theoncologist.5-5-350. [DOI] [PubMed] [Google Scholar]
- 5.Carr D, Goudas L, Lawrence D, et al. Rockville, MD: Agency for Healthcare Research and Quality; 2002. Management of cancer symptoms: Pain, depression, and fatigue. Evidence Report/Technology Assessment No: 61: AHRQ Publication No. 02–E032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mock V, Atkinson A, Barsevick A, et al. NCCN Practice guidelines for cancer-related fatigue. Oncology. 2000;14:151–161. [PubMed] [Google Scholar]
- 7.Zabora J, BrintzenhofeSzoc K, Curbow B, et al. The prevalence of psychological distress by cancer site. Psycho-oncolgy. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 8.Basch E, Artz D, Dulko D, et al. Patient online self-reporting of toxicity symptoms during chemotherapy. J Clin Oncol. 2005;23:3552–3561. doi: 10.1200/JCO.2005.04.275. [DOI] [PubMed] [Google Scholar]
- 9.Basch E, Iasonos A, McDonough T, et al. Patient versus clinician symptom reporting using the National Cancer Institute Common Terminology Criteria for Adverse Events: Results of a questionnaire-based study. Lancet Oncol. 2006;7:903–909. doi: 10.1016/S1470-2045(06)70910-X. [DOI] [PubMed] [Google Scholar]
- 10.Velikova G, Booth L, Smith AB, et al. Measuring quality of life in routine oncology practice improves communication and patient well-being: A randomized controlled trial. J Clin Oncol. 2004;22:714–724. doi: 10.1200/JCO.2004.06.078. [DOI] [PubMed] [Google Scholar]
- 11.Dudgeon DJ, Knott C, Chapman C, et al. Development, implementation, and process evaluation of a regional palliative care quality improvement project. J Pain Symptom Manage. 2009;38:483–495. doi: 10.1016/j.jpainsymman.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bruera E, Kuehn N, Miller MJ, et al. The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. J Palliat Care. 1991;7:6–9. [PubMed] [Google Scholar]
- 13.Chang VT, Hwang SS, Feuerman M. Validation of the Edmonton Symptom Assessment Scale. Cancer. 2000;88:2164–2171. doi: 10.1002/(sici)1097-0142(20000501)88:9<2164::aid-cncr24>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 14.Moro C, Brunelli C, Miccinesi G, et al. Edmonton Symptom Assessment Scale: Italian validation in two palliative care settings. Support Care Cancer. 2006;14:30–37. doi: 10.1007/s00520-005-0834-3. [DOI] [PubMed] [Google Scholar]
- 15.Nekolaichuk C, Watanabe S, Beaumont C. The Edmonton Symptom Assessment System: A 15-year retrospective review of validation studies (1991-2006) Palliat Med. 2008;22:111–122. doi: 10.1177/0269216307087659. [DOI] [PubMed] [Google Scholar]
- 16.Nelson JE, Meier DE, Oei EJ, et al. Self-reported symptom experience of critically ill cancer patients receiving intensive care. Crit Care Med. 2001;29:277–282. doi: 10.1097/00003246-200102000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Rees E, Hardy J, Ling J, et al. The use of the Edmonton Symptom Assessment Scale (ESAS) within a palliative care unit in the UK. Palliat Med. 1998;12:75–82. doi: 10.1191/026921698674135173. [DOI] [PubMed] [Google Scholar]
- 18.Richardson LA, Jones GW. A review of the reliability and validity of the Edmonton Symptom Assessment System. Curr Oncol. 2009;16:55. doi: 10.3747/co.v16i1.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baba K, Fransson P, Lindh J. Use of a modified ESAS in cancer patients: A pilot study of patient and staff experiences. Int J Palliat Nurs. 2007;13:610–616. doi: 10.12968/ijpn.2007.13.12.27890. [DOI] [PubMed] [Google Scholar]
- 20.Canadian Association of General Practitioners in Oncology. http://www.cos.ca/cagpo/web/welcome.html.
- 21.Brazil K, Sussman J, Bainbridge D, et al. Who is responsible? The role of family physicians in the provision of supportive cancer care. J Oncol Pract. 2010;6:19–24. doi: 10.1200/JOP.091060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bulsara C, Ward AM, Joske D. Patient perceptions of the GP role in cancer management. Aust Fam Physician. 2005;34:299–300. [PubMed] [Google Scholar]
- 23.Gray RE, Goel V, Fitch MI, et al. Supportive care provided by physicians and nurses to women with breast cancer: Results from a population-based survey. Support Care Cancer. 2002;10:647–652. doi: 10.1007/s00520-002-0370-3. [DOI] [PubMed] [Google Scholar]
- 24.Cancer Care Ontario: Symptom Assessment. http://csqi.cancercare.on.ca/cms/One.aspx?portalId=40955&pageId=41113.
- 25.Chumbler NR, Kobb R, Harris L, et al. Healthcare utilization among veterans undergoing chemotherapy: The impact of a cancer care coordination/home-telehealth program. J Ambul Care Manage. 2007;30:308–317. doi: 10.1097/01.JAC.0000290399.43543.2e. [DOI] [PubMed] [Google Scholar]
- 26.Canadian Association of Nurses in Oncology (CANO) Roles in Oncology Nursing. http://www.cano-acio.ca/roles.