Patients with cancer often have complex needs that must be met within a short intervention window. The authors highlight opportunities for improved multidisciplinary care for patients with advanced cancer and their families.
Abstract
Purpose:
We sought to characterize the aggregate features and survival of patients who receive inpatient palliative care consultation, particularly focusing on patients with cancer, to identify opportunities to improve clinical outcomes.
Methods:
We reviewed prospectively collected data on patients seen by the Palliative Care Inpatient Consult Service at Mayo Clinic (Rochester, MN) from January 2003 to September 2008. Demographics, consultation characteristics, and survival were analyzed using Kaplan-Meier survival curves and Cox survival models.
Results:
Cancer was the most common primary diagnosis (47%) in the 1,794 patients seen over the 5-year period. A significant growth in the annual number of palliative care consultations has been observed (113 in 2003 v 414 in 2007), despite stable total hospital admissions. Frequently encountered reasons for consultation included clarification of care goals (29%), assistance with dismissal planning (19%), and pain control (17%). Although patients with cancer had the highest median survival after consultation in this cohort versus patients with other diagnoses, we observed a 5-year trend of decreasing survival from admission to death and from consultation to death. Median time from admission to death for patients with cancer was 36 days in 2003 and only 19 days in 2008 (P < .01). Median time from consultation to death decreased from 33 days in 2003 to only 11.5 days in 2008 (P < .01).
Conclusion:
Patients with cancer often have complex needs that must be met within a short window for intervention. We highlight opportunities for improved multidisciplinary care for patients with advanced cancer and their families, including opportunity for earlier palliative care involvement, even in the outpatient setting.
Introduction
Palliative care aims to optimize quality of life and alleviate suffering for patients and their families. It has become an essential part of the continuum of care for patients with severe and life-limiting illness, including those with cancer, and recent studies have demonstrated benefits in survival and quality of life with early palliative care.1 Hospital-based palliative care teams assist in the care of hospitalized patients by providing recommendations ranging from symptom management to spiritual support.2 Although palliative care is ideally provided throughout the course of a severe illness and alongside disease-modifying therapies, the majority of patients referred to inpatient palliative care services are moribund, with only hours to days left to live.3,4
Research demonstrates that high-quality palliative care occurs when health care professionals ensure desired physical comfort and emotional support, promote shared decision making, provide information and emotional support to family members, and coordinate care across settings.5 Yet, severely ill patients and their families report high rates of unrelieved suffering, including undertreated physical and psychological symptoms, inadequate communication, and insufficient emotional support, even in the very last days of patients' lives.6 Hospital-based palliative care consultation services have demonstrated improved physical and psychological symptom management, caregiver well-being, emotional and spiritual support, physician-patient communication, and markedly superior overall patient and family satisfaction.7 Previous studies have also found that inpatient palliative care teams frequently identify unrecognized symptoms and unmet needs3,8–10 and palliative care consultations are associated with a lower likelihood of dying in the intensive care unit,11 less use of intensive care units,12,13 and substantial decreases in health care costs.13–15 These factors were a major impetus for the development of our Palliative Care Consultation Service (PCCS) at Mayo Clinic (Rochester, MN).
As of 2005, 30% of US hospitals reported having a palliative care program,16 and this number is rapidly growing.15 Past studies have investigated inpatient palliative care consultation patterns and impact and reasons for consultation,3,4 including services designed for specialized populations.17 The goal of this study was to increase our understanding of referral patterns and patient- and provider-specific needs, with the goal of improving our practice. Herein, we report the results of our 5-year experience with palliative care consultations.
Methods
Data Collection and Analysis
After approval by the Mayo Clinic Institutional Review Board, we performed a retrospective analysis of all patients seen by the PCCS at Mayo Clinic between January 1, 2003, and September 15, 2008. Palliative care consultations were performed by an interdisciplinary team of palliative medicine physicians (attendings, fellows, and residents), allied health practitioners, nurses, and chaplains, with support from social workers and pharmacists. During the study period, the PCCS received administrative support from the Department of Oncology, although palliative medicine physicians came from several areas including general internal medicine, hospital medicine, medical oncology, psychiatry, and family medicine.
Patient information and consultation characteristics have been prospectively collected in a secure database since the inception of the PCCS in 2003. Patients seen in outpatient palliative care clinics, long-term care settings, their homes, or home or residential hospice were excluded. For our study, data with patient identifiers were reviewed by two palliative medicine physicians (A.H.K., K.M.S.) but de-identified information was available to all study authors and personnel.
Patient information collected consisted of demographics (including age, diagnosis, home zip code, and code status at time of consultation), hospitalization characteristics (including length of stay, time from discharge to death, and dismissal location), and consultation characteristics (including reason for consultation, time from consultation to death or discharge, and service requesting consultation). Demographic data were collected from a comprehensive, shared outpatient and inpatient electronic medical record. Consultative characteristics were reviewed from PCCS and primary inpatient team documentation. Date of death was obtained from our medical record, Medicare database, other public searchable databases, obituary search, and direct patient/family contact. Unless a confirmed date of death could be obtained, patients were assumed to be alive.
Statistical Analyses
The distribution of times from consultation to death and from admission to death was estimated using the Kaplan-Meier method. A Cox proportional hazards regression model was used to predict survival to hospital discharge in patients who lived less than 6 months (ie, hospice-eligible population) by adjusting for other potential risk factor such age, gender, month of the consultation, length of the stay, diagnosis code, consultation location, and known places of discharge.
Results
In our PCCS database, 1,794 patients had evaluable information during the inclusion time frame. The aggregated demographic and consultation characteristics are further described in Table 1. The median age of the patients at the time of palliative care consultation was 75.5 years (range, 0 to 104 years). More than one third were older than 80 years. Eighty percent of patients were subject to do not resuscitate/do not intubate orders at the time of consultation. A significant annual trend toward increased consultations was seen, despite no dramatic changes in available hospital beds or total inpatient admissions.
Table 1.
Patient Demographics and Characteristics of Palliative Care Consultations Completed (N = 1,794)
| Characteristic | No. | % |
|---|---|---|
| Year of consultation | ||
| 2003 | 113 | 6 |
| 2004 | 220 | 12 |
| 2005 | 283 | 18 |
| 2006 | 363 | 20 |
| 2007 | 414 | 23 |
| 2008 | 401 | 22 |
| Gender | ||
| Male | 933 | 52 |
| Female | 861 | 48 |
| Age at time of consultation, years | ||
| Median | 75.5 | |
| Range | 1 to 104 | |
| Birth-20 | 4 | <1 |
| 21-40 | 46 | 3 |
| 41-60 | 284 | 16 |
| 61-80 | 798 | 45 |
| 81+ | 661 | 37 |
| Resuscitation/code status | ||
| Full | 355 | 20 |
| DNR/DNI | 1,429 | 80 |
| Other | 10 | <1 |
| Primary diagnosis, reason for consultation | ||
| Cancer | 825 | 46 |
| Cardiac | 379 | 21 |
| Neurologic | 223 | 12 |
| Pulmonary | 167 | 9 |
| Renal | 91 | 5 |
| Vascular | 54 | 3 |
| Gastroenterology/hepatology | 46 | 3 |
| Not known | 5 | <1 |
| Service requesting consultation | ||
| Internal medicine | 556 | 31 |
| Cardiology/cardiac intensive care | 377 | 21 |
| Surgery | 269 | 15 |
| Medical intensive care | 161 | 9 |
| Hematology/oncology | 108 | 6 |
| Neurology | 90 | 5 |
Abbreviations: DNR, do not rescucitate; DNI, do not intubate.
Internal medicine–based hospital services (which in our analysis included gastroenterology and pulmonary services, but not hematology or oncology) were the leading requester of consultations (31%). Cardiology, including the coronary care unit, was second with 21%. Critical care units in the aggregate (medicine, noncardiac, excluding surgical and trauma) contributed to 9% of consultations. Primary hematology, oncology, and bone marrow transplantation services requested 6% of consultations.
The most common reason for consultation across services was a diagnosis of cancer, with cardiac, neurologic, and pulmonary diseases following (Table 1). Despite cancer being the overall leading diagnosis triggering consultation, most consultation requests came from nononcology services.
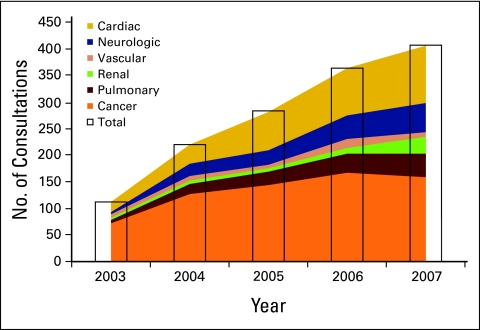
Trends in diseases seen during palliative care consultation are presented in Figure 1. Whereas cancer diagnosis accounted for 64% of consultation requests in 2003, it contributed to only 38% in 2008. Over the 5-year period, we observed steady growth of diagnoses such as pulmonary (eg, pulmonary hypertension, interstitial lung disease, chronic obstructive pulmonary disease), neurologic (eg, stroke, traumatic brain injury, amyotrophic lateral sclerosis), and renal (eg, end-stage renal failure, transplant rejection). The most commonly cited reasons for consultation include aiding in establishing goals of care (approximately one fourth of patients); addressing pain (approximately one fifth of patients); and, to a lesser degree, working with the care team on appropriate dismissal planning or relief of dyspnea. A wide variety of other symptom-control issues were also addressed. The mean number of documented interventions per patient was 6.1, indicating that patients rarely had only one or two issues to be addressed. The combination of goals of care and at least one symptom-control issue was the most common grouping of interventions performed during the PCCS visit.
Figure 1.
Distribution of primary diagnosis of palliative care consultations received.
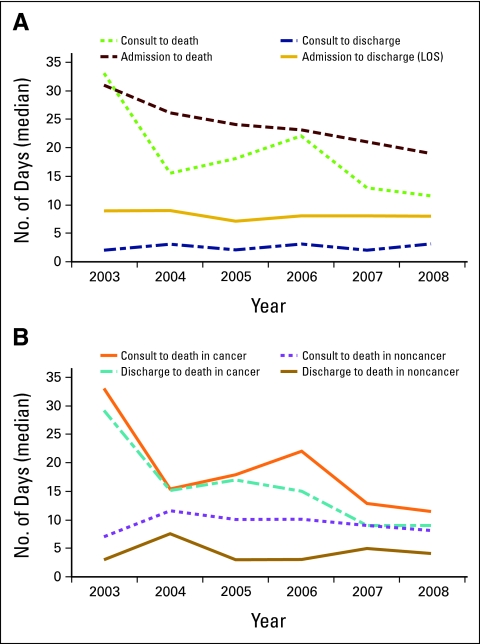
Analysis of outcomes at key time points in a patient's care is shown in Figure 2A. Whereas the median time from hospital admission to death was 36 days in 2003, this number decreased to only 19 days in 2008 (P < .01). Likewise, time from palliative care consultation to death also decreased from 33 days to 11.5 days over the 5-year span (P < .01). Despite the apparent increasing morbidity of the patients who were admitted during our study period, both time from hospital admission to discharge (ie, length of stay) and time from palliative care consultation to discharge (ie, the intervention window for PCCS) remained stable at 8 and 2.5 days, respectively (P = NS).
Figure 2.
Time to patient-specific outcomes regarding relationship between time of admission, consultation, discharge and death. (A) relates to patients with all diagnoses, whereas (B) breaks down cancer versus noncancer diagnoses.
We performed a side-by-side comparison of metrics we considered important to determine the window for PCCS intervention. Figure 2B shows a comparison of time from palliative care consultation to death and time from hospital discharge to death in patients with cancer and patients with noncancer diagnoses. This analysis shows that the initial time advantage, both after consultation (ie, time for consultative intervention) and discharge (ie, time for hospice intervention) seen in cancer patients is decreasing.
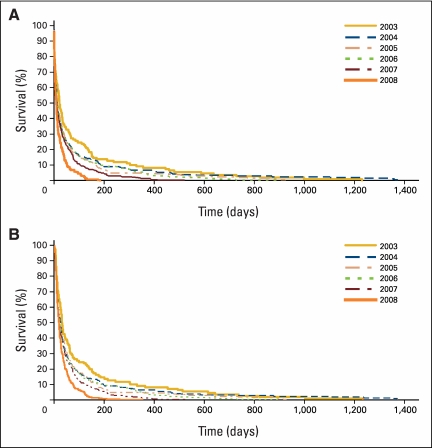
Kaplan-Meier curves of time from palliative care consult to death and time from hospital admission to death are presented in Appendix Figures A1A and A1B (online version only), respectively. A Cox model of predicting survival to hospital discharge in patients who lived less than 6 months (ie, hospice-eligible population) was made using variables from the original database plus known places of discharge. This model shows time from admission to discharge, time from consultation to discharge, and dismissal location as prognostic factors for survival to discharge.
Discussion
In our study, we observed dramatic and consistent growth in palliative care consultation volume. We noted that our patient population is elderly, has an increasingly diverse array of life-limiting diseases, and is mostly referred by nononcology internal medicine services. Cancer is overall the most common diagnosis for consultation, although annual trends show an increase in other life-limiting diseases. The mean number of issues addressed during consultation was more than six and most often included establishing goals of care, addressing pain, and aiding in dismissal planning. We observed a steady decline in time from hospital admission to death and palliative care consultation to death, despite a steady hospital length of stay and time from PCCS consultation to discharge.
Compared with previous studies that report on palliative care experience at academic comprehensive cancer centers,18–20 we note a progressive trend of later involvement by PCCS with patients with cancer. For example, Cheng et al21 reported, in a mixed population of inpatient and outpatient consultations, a median time of 1.9 months between palliative care referral and death. Our data suggest that this delay is worsening, which not only shortens the possibility for building rapport and providing meaningful relief of symptoms, but also provides less opportunity for cost saving.15 This progressive delay may reflect a hardening of a biased belief that palliative care and end-of-life care are synonymous, a misunderstanding that is still observed in surveys of health care providers regarding attitudes22 and practice patterns.23 Moreover, the role of palliative care professionals may still be perceived as involving end-of-life care only. Fewer than half of polled oncologists feel adequately trained to perform palliative care tasks, although they report feeling comfortable addressing common symptoms found in advanced cancer.24 Late referral to consultative palliative care is not unique; hospice enrollment has also been progressively delayed, leading to lower satisfaction and more unmet needs.25
Although cancer remains the key consultative diagnosis, a minority of referrals actually came from hematologists or oncologists. Although palliative care–related issues may be perceived to be within the purview of hematology/oncology practice, studies have demonstrated that patients with cancer often have undertreated pain26,27 and potentially multiple additional symptoms beyond the reason for consultation.19 Recent data suggest that early palliative care involvement in caring for patients with advanced cancer provided improved quality of life and survival compared with traditional care provided by oncologists alone.1 Furthermore, clearly documented wishes regarding goals of care in patients with advanced cancer are completed only approximately 25% of the time,28 and only 31% of dying cancer patients reported having direct discussions about death with their oncologist.29 Data further suggest that difficult but honest discussion regarding outcomes in advanced cancer is not associated with taking hope away from patients or families.30
The dramatic gap between cancer diagnosis referrals from nononcology versus oncology providers remains hypothesis generating. The majority of our institution's interactions (including patient care and relationship building) between palliative care providers and all referring specialties, including hematology and oncology, occur in the inpatient setting. This had been due to the relative infancy of our outpatient palliative care program during the study period. Others have reported significant increases in palliative care consultations and oncologist satisfaction with services after integrating these services into an outpatient oncology practice.31 Those authors concluded that proximity and frequent clinical interactions ultimately built familiarity, trust, and an appreciation of the value of palliative care. Most hematologists/oncologists at our institution do not regularly attend on the inpatient oncology hospital services or inpatient consult services; hence, the opportunity to influence those individual providers remained limited.
In addition, a unique aspect of our hospital practice is the presence of multiple and separate inpatient hematology and oncology services (ie, solid tumor services [two]; lymphoma, leukemia, and bone marrow transplant services [one each]). Patients are admitted to these services only if they have active relationships with an outpatient hematologist or oncologist at our institution. Because we are a tertiary care center, many patients admitted with advanced cancer may have yet to be diagnosed and/or treated at our institution, and thus are often admitted to a nononcology hospital service. The observation that these patients are more likely to receive a palliative care consultation may reflect the lack of an established relationship with an oncologist, who traditionally may be coordinating palliative care efforts elsewhere on the patients' behalf. Interestingly, among inpatients who receive both inpatient medical oncology and palliative care consultation, the suggestion for palliative care consultation often comes from the consulting oncologist in a collegial fashion. Last, a significant portion of our consultation requests were placed by those who perform inpatient care regularly (eg, house staff, hospitalists) and who palliative care providers see and interact with often. Moreover, previous educational efforts were primarily aimed at these inpatient providers, suggesting success of the efforts to increase palliative care consultations at our institution.
On the basis of these data, opportunities have been identified for improved palliative care delivery to patients with cancer. Targeted education to both inpatient and outpatient hematology and bone marrow transplantation physicians/nursing staffs has led to increased palliative care consultations and use. We have expanded our outpatient palliative care clinic through improved appointment availability and have built relationships with hematology and oncology administrators and physicians through research collaboration and mutual conferences. We also recently began a twice-weekly outpatient cancer pain clinic staffed by palliative medicine physicians, which has improved detection and treatment of pain and nonpain symptoms and improved quality of life.32 Specific efforts have been made to educate patients, providers, and staff about what palliative care truly means; how palliative care can be consistent with life-prolonging therapies such as radiation or chemotherapy; and how improvement in symptoms, quality of life, and satisfaction can result from a parallel, as opposed to sequential, relationship. This includes educating providers about the cancer-specific expertise that is available, including that one third of our palliative medicine physicians are also clinical oncologists, and that others are regularly involved with care of patients with cancer from rehabilitation and psychiatric perspectives. Efforts to truly integrate palliative care along with tumor-specific therapy have been suggested33 and are part of the multidisciplinary model that strives to provide the best possible patient care.
There are limitations to this study. This is a single-center experience, in a suburban/rural setting, at a tertiary care/referral medical center, which may limit the ability to extrapolate our findings. Because patients referred to tertiary care centers have more advanced disease, opportunities for providing palliative care services (which are determined by the referring hospital team who request the consultation) may be more plentiful than in settings with lower levels of morbidity. In addition, lack of quantitative patient or family feedback on patient-physician satisfaction regarding PCCS consultation is a noted limitation to our study, and this is a subject worthy of further study.
It is important to note that a shorter intervention period does not necessarily mean a less significant intervention. Certainly, high-yield, limited palliative care consultations in distress situations may produce relief of suffering that meets patients' and families' short-term goals. Nevertheless, earlier palliative care consultations have been associated with improved overall patient and family satisfaction and outcomes.1,7 This notwithstanding, an optimal time for involvement of palliative care has yet to be defined.
Summary
Within our academic medical center, palliative care consultative services increased dramatically over the 5-year study period. The primary diagnosis for consultation continues to diversify, with increased numbers of nononcology patients being seen. The reasons for consultation primarily include conversations involving goal-setting and recommendations for symptom control measures. We demonstrate that despite a stable length of stay, time for palliative care intervention before discharge and before death continues to shorten. The demonstrated discrepancy between the number of consultation requests for patients with cancer from nononcology versus oncology hospital services may be explained by the familiarity between oncologists and the palliative care service and the presence of an established, treating oncologist for patients from oncology hospital services. We believe that continued increase in palliative care services, better demonstration of the benefit of palliative care consultation, and strengthening relationships between treatment groups will continue to improve our world-class comprehensive cancer care. We conclude that cancer patients benefit most from earlier palliative care involvement that extends longitudinally, is performed by a multidisciplinary team, and is parallel to the care by the oncologist.
Acknowledgment
This research was presented at the 45th Annual Meeting of the American Society of Clinical Oncology, May 29-June 2, 2009, Orlando, FL.
Figure A1.
Survival curves from (A) time of palliative care consultation to death by year of consultation and (B) time of hospital admission to death by year of consultation.
Authors' Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
Author Contributions
Conception and design: Arif H. Kamal, Keith M. Swetz, Timothy J. Moynihan, Jeff A. Sloan, Judith S. Kaur
Administrative support: Keith M. Swetz
Collection and assembly of data: Arif H. Kamal, Keith M. Swetz, Elise C. Carey, Suzanne R. Ruegg
Data analysis and interpretation: Arif H. Kamal, Keith M. Swetz, Elise C. Carey, Andrea L. Cheville, Heshan Liu, Suzanne R. Ruegg, Timothy J. Moynihan, Jeff A. Sloan, Judith S. Kaur
Manuscript writing: Arif H. Kamal, Keith M. Swetz, Elise C. Carey, Andrea L. Cheville, Timothy J. Moynihan, Jeff A. Sloan, Judith S. Kaur
Final approval of manuscript: Arif H. Kamal, Keith M. Swetz, Elise C. Carey, Andrea L. Cheville, Heshan Liu, Suzanne R. Ruegg, Timothy J. Moynihan, Jeff A. Sloan, Judith S. Kaur
References
- 1.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 2.Weissman DE. Consultation in palliative medicine. Arch Intern Med. 1997;157:733–737. [PubMed] [Google Scholar]
- 3.Manfredi PL, Morrison RS, Morris J, et al. Palliative care consultations: How do they impact the care of hospitalized patients? J Pain Symptom Manage. 2000;20:166–173. doi: 10.1016/s0885-3924(00)00163-9. [DOI] [PubMed] [Google Scholar]
- 4.von Gunten CF, Camden B, Neely KJ, et al. Prospective evaluation of referrals to a hospice/palliative medicine consultation service. J Palliat Med. 1998;1:45–53. doi: 10.1089/jpm.1998.1.45. [DOI] [PubMed] [Google Scholar]
- 5.Teno JM, Clarridge B, Casey V, et al. Validation of Toolkit After-Death Bereaved Family Member Interview. J Pain Symptom Manage. 2001;22:752–758. doi: 10.1016/s0885-3924(01)00331-1. [DOI] [PubMed] [Google Scholar]
- 6.Teno JM, Clarridge BR, Casey V, et al. Family perspectives on end-of-life care at the last place of care. JAMA. 2004;291:88–93. doi: 10.1001/jama.291.1.88. [DOI] [PubMed] [Google Scholar]
- 7.Casarett D, Pickard A, Bailey FA, et al. Do palliative consultations improve patient outcomes? J Am Geriatr Soc. 2008;56:593–599. doi: 10.1111/j.1532-5415.2007.01610.x. [DOI] [PubMed] [Google Scholar]
- 8.Bailey FA, Burgio KL, Woodby LL, et al. Improving processes of hospital care during the last hours of life. Arch Intern Med. 2005;165:1722–1727. doi: 10.1001/archinte.165.15.1722. [DOI] [PubMed] [Google Scholar]
- 9.Bascom PB. A hospital-based comfort care team: Consultation for seriously ill and dying patients. Am J Hosp Palliat Care. 1997;14:57–60. doi: 10.1177/104990919701400202. [DOI] [PubMed] [Google Scholar]
- 10.Abrahm JL, Callahan J, Rossetti K, et al. The impact of a hospice consultation team on the care of veterans with advanced cancer. J Pain Symptom Manage. 1996;12:23–31. doi: 10.1016/0885-3924(96)00045-0. [DOI] [PubMed] [Google Scholar]
- 11.Elsayem A, Smith ML, Parmley L, et al. Impact of a palliative care service on in-hospital mortality in a comprehensive cancer center. J Palliat Med. 2006;9:894–902. doi: 10.1089/jpm.2006.9.894. [DOI] [PubMed] [Google Scholar]
- 12.Norton SA, Hogan LA, Holloway RG, et al. Proactive palliative care in the medical intensive care unit: Effects on length of stay for selected high-risk patients. Crit Care Med. 2007;35:1530–1535. doi: 10.1097/01.CCM.0000266533.06543.0C. [DOI] [PubMed] [Google Scholar]
- 13.Penrod JD, Deb P, Luhrs C, et al. Cost and utilization outcomes of patients receiving hospital-based palliative care consultation. J Palliat Med. 2006;9:855–860. doi: 10.1089/jpm.2006.9.855. [DOI] [PubMed] [Google Scholar]
- 14.Smith TJ, Coyne P, Cassel B, et al. A high-volume specialist palliative care unit and team may reduce in-hospital end-of-life care costs. J Palliat Med. 2003;6:699–705. doi: 10.1089/109662103322515202. [DOI] [PubMed] [Google Scholar]
- 15.Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with US hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783–1790. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 16.American Hospital Association. AHA Hospital Statistics. Chicago, IL: American Hospital Association; 2007. [Google Scholar]
- 17.Selwyn PA, Rivard M, Kappell D, et al. Palliative care for AIDS at a large urban teaching hospital: Program description and preliminary outcomes. J Palliat Med. 2003;6:461–474. doi: 10.1089/109662103322144844. [DOI] [PubMed] [Google Scholar]
- 18.Osta BE, Palmer JL, Paraskevopoulos T, et al. Interval between first palliative care consult and death in patients diagnosed with advanced cancer at a comprehensive cancer center. J Palliat Med. 2008;11:51–57. doi: 10.1089/jpm.2007.0103. [DOI] [PubMed] [Google Scholar]
- 19.Braiteh F, El Osta B, Palmer JL, et al. Characteristics, findings, and outcomes of palliative care inpatient consultations at a comprehensive cancer center. J Palliat Med. 2007;10:948–955. doi: 10.1089/jpm.2006.0257. [DOI] [PubMed] [Google Scholar]
- 20.Delgado-Guay MO, Parsons HA, Li Z, Palmer LJ, Bruera E. Symptom distress, interventions, and outcomes of intensive care unit cancer patients referred to a palliative care consult team. Cancer. 2009;115:437–445. doi: 10.1002/cncr.24017. [DOI] [PubMed] [Google Scholar]
- 21.Cheng WW, Willey J, Palmer JL, et al. Interval between palliative care referral and death among patients treated at a comprehensive cancer center. J Palliat Med. 2005;8:1025–1032. doi: 10.1089/jpm.2005.8.1025. [DOI] [PubMed] [Google Scholar]
- 22.Mahon MM, McAuley WJ. Oncology nurses' personal understandings about palliative care. Oncol Nurs Forum. 37:E141–E150. doi: 10.1188/10.ONF.E141-E150. [DOI] [PubMed] [Google Scholar]
- 23.Ward AM, Agar M, Koczwara B. Collaborating or co-existing: A survey of attitudes of medical oncologists toward specialist palliative care. Palliat Med. 2009;23:698–707. doi: 10.1177/0269216309107004. [DOI] [PubMed] [Google Scholar]
- 24.Cherny NI, Catane R. Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer: Report on a survey by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care. Cancer. 2003;98:2502–2510. doi: 10.1002/cncr.11815. [DOI] [PubMed] [Google Scholar]
- 25.Teno JM, Shu JE, Casarett D, et al. Timing of referral to hospice and quality of care: Length of stay and bereaved family members' perceptions of the timing of hospice referral. J Pain Symptom Manage. 2007;34:120–125. doi: 10.1016/j.jpainsymman.2007.04.014. [DOI] [PubMed] [Google Scholar]
- 26.van den Beuken-van Everdingen M, de Rijke J, Kessels A, et al. Prevalence of pain in patients with cancer: A systematic review of the past 40 years. Ann Oncol. 2007;18:1437–1449. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- 27.Deandrea S, Montanari M, Moja L, et al. Prevalence of undertreatment in cancer pain. A review of published literature Ann Oncol. 2008;19:1985–1991. doi: 10.1093/annonc/mdn419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kish S, Martin C, Price K. Advance directives in critically ill cancer patients. Crit Care Nurs Clin North Am. 2000;12:373–383. [PubMed] [Google Scholar]
- 29.Wright A, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA. 2008;300:1665–1673. doi: 10.1001/jama.300.14.1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith TJ, Dow LA, Virago E, et al. Giving honest information to patients with advanced cancer maintains hope. Oncology (Williston Park) 2010;24:521–525. [PubMed] [Google Scholar]
- 31.Muir JC, Daly F, Davis MS, et al. Integrating palliative care into the outpatient, private practice oncology setting. J Pain Symptom Manage. 40:126–135. doi: 10.1016/j.jpainsymman.2009.12.017. [DOI] [PubMed] [Google Scholar]
- 32.Swetz K, Mauck W, Pingree M, et al. Palliative medicine intervention in patients referred to an anesthesia-based cancer pain clinic. J Support Oncol. 2009;7:200. [Google Scholar]
- 33.Sanft T, Von Roenn H. Palliative care across the continuum of cancer care. J Natl Compr Cancer Net. 2009;7:481–487. doi: 10.6004/jnccn.2009.0033. [DOI] [PubMed] [Google Scholar]