Summary
Currently the medicolegal dissection rate for England and Wales is 22% (110,000 coronial autopsies for 500,000 deaths per annum), yet there is a general lack of evidence about the utility of and justification for such a high level of activity, which is between double and triple the rate in other jurisdictions. The government is currently consulting on how to reduce the numbers, and the Coroners and Justice Act 2009 is permissive of external examinations as an alternative to dissections. We describe the philosophy and practice of the Scottish system of postmortem external examinations, and the 20-year experience of a local initiative to maximize use of such external examinations. Currently our regional medicolegal dissection rate is 6%, which if applied to England and Wales would reduce the number of dissections from 110,000 to 30,000 per annum, with all of the social, resource and management implications. While the autopsy is an important tool in modern death investigation, an almost automatic recourse to it is inappropriate. In our view external examinations are not only cost-effective but also a necessary element in any death investigative system which wishes to strike an appropriate balance between intrusion by the state and the rights of the bereaved.
Introduction
A medicolegal dissection (autopsy) is an important tool in modern death investigation. However, it is also an intrusion by the state into what is otherwise the private matter of the death of a family member. The need for the state to seize the corpse and to dissect it for investigative purposes must be balanced against the rights of the family to privacy and freedom of religious practice.1,2 Quite apart from the issues of ethics and human rights, the overall cost of autopsies and other medical or scientific tests is rather more than half the total direct cost of the coroner service in England and Wales.2 Currently the medicolegal dissection rate for England and Wales is 22% (110,000 coronial autopsies for 500,000 deaths per annum), yet there is no evidence of a proportionate benefit to justify such high levels of activity. There is, indeed, a general lack of evidence about the utility of and justification for coroner autopsies on the scale on which they are practised.2 The high level of activity combined with workforce issues, with a national shortage of autopsy pathologists, may explain why pathologists ‘cut corners’ so that one-quarter of coronial autopsy reports are poor or unacceptable.3,4
Broadly, in England and Wales the autopsy rate is between double and triple the autopsy rate in other jurisdictions.2 It is almost twice that in Scotland where the option exists for an external examination of a body as an alternative to dissection.5,6 The new Coroners and Justice Act 2009 for England and Wales is permissive of external examinations and creates the opportunity for change. The Government's view is that there are too many coroner postmortems carried out and the question of when a postmortem examination is required is part of an ongoing consultation initiated in March 2010.7
One possible model for change exists in the forensic autopsy service provided by the University of Dundee to Tayside region in Scotland. From 1988 a program was initiated to maximize use of external examinations (called ‘view and grant’ examinations in Scotland), so that today the regional medicolegal dissection rate is 6%. In 2006, with the cooperation of NHS pathologists, the program was extended successfully to Fife and Central regions, and now serves a population of 1.1 million. If the philosophy and practice of the Scottish system and the Dundee initiative were replicated in England and Wales then it could reduce the number of medicolegal dissections from 110,000 to 30,000 per annum.
The setting
In Scotland there are no coroners and deaths are investigated by procurators fiscal – the state prosecution service – who receive reports of deaths through similar mechanisms as the English coroner. Not all deaths notified are investigated but those investigated are subject to police inquiry with a resulting comprehensive police report.5,8 The procurators fiscal authorize postmortem examinations which include, at the pathologists' discretion, the retention of tissue for histopathological examination in order to establish, confirm or refine diagnoses. Unlike the statutory position in England and Wales, this retained tissue for histopathology becomes part of the permanent clinical record.
If there is a reason to dissect a body to gain necessary information the fiscal will authorize this. When the family objects to a dissection, the fiscal can order an external examination instead. If there is no clear indication for a dissection then the fiscal can give the pathologist the discretion to perform either an external examination or dissection as the pathologist considers necessary to complete the death certificate (which cannot be completed by the fiscal). We have developed and encouraged this latter instruction over the years. Pathologists and fiscals discuss the options, so the fiscal's decision may change.
Given the discretion to perform either an external examination or dissection, the pathologist makes an initial choice prior to viewing the body. The rationale is that if the information contained in the police report and/or medical records is sufficient to establish the cause and manner of death then it is appropriate to perform an external examination. The purpose of this examination is to exclude any suspicious finding or anything which cannot be reconciled with the circumstances of death, history and the opinion on cause of death. The level of certainty applied to the diagnosis of cause and manner of death is that which would ordinarily be applied to a clinical diagnosis.
The external examination is thorough, includes the examination of clothing and a head-to-toe examination of the body to record all identifying features, old and recent injuries, postmortem changes, and recent medical intervention including resuscitation attempts. Minor incisions can be made to obtain samples for toxicology.
Analysis of practice
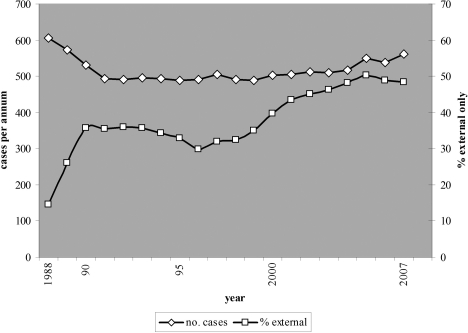
For the first 20 years of the Dundee initiative (1988–2007) the total number of postmortem examinations for Tayside (population 388,000) was 10,308, of which 38% (3875) were limited to external examinations. The first few years saw the rapid achievement of an external examination rate of 30%, which was associated with a fall in the number of cases referred by the fiscals for examination, and the years after 2000 saw a further steady increase in external examinations ( Figure 1).
Figure 1.
Annual caseload for Tayside and percentage of postmortem examinations which were external only, 1988–2007 (rolling 3-year averages)
A detailed analysis of practice for 2001–2007, utilizing a casework database, encompassed 3804 deaths in Tayside of whom 48% (1809) had external examinations (annual range 42–51%). The medicolegal dissection rate for Tayside (percentage of all deaths in the community subjected to medicolegal dissection) averaged 6.0% (annual range 5.5–6.8%).
Of 225 specific requests to perform an external examination, in only five cases was it necessary to dissect the body. The fiscal instructed a dissection or external examination, at the discretion of the pathologist, in 61% of cases (2334) and of these 66% (1528) were subject to external examination only. The fiscal instructed a dissection in 33% (1245) and the overwhelming majority of these were performed (96%; 1195), the remainder being converted to external examinations after discussion with the pathologist. Forty-nine dissections were curtailed after initial dissection disclosed a clear cause of death, e.g. ruptured aortic aneurysm. Use of the external examination was highest (72%) in those above 70 years.
External examinations were commonly used in a wide range of accidental and suicidal deaths (Table 1). Among natural deaths, cardiovascular deaths represented 48% of the caseload and were certified in 90% of cases as due to atherosclerosis, hypertension or a combination of the two. Among this group 32% had been dissected and no more precise a cause of death established. For the non-cardiovascular natural deaths, external examination rates were highest for the diagnoses of chronic bronchitis and emphysema, asthma and gastro-intestinal haemorrhage. Diagnoses associated with a low external examination rate were myocardial infarction, ruptured aortic aneurysm, peritonitis, pulmonary thrombo-embolism and pneumonia.
Table 1.
Tayside cases (2001–2007) by manner of death and selected cause of death with percentage of postmortem examinations which were external only
| Manner of death and selected causes | n | External examination (%) |
|---|---|---|
| All natural deaths | 2412 | 55 |
| Atheroma and/or hypertension | 1637 | 68 |
| Myocardial infarction | 68 | 7 |
| Ruptured aortic aneurysm | 33 | 12 |
| Chronic bronchitis and emphysema | 104 | 64 |
| Asthma | 26 | 46 |
| Gastro-intestinal tract haemorrhage | 26 | 42 |
| Peritonitis | 22 | 9 |
| Pulmonary thrombo-embolism | 59 | 7 |
| Pneumonia | 26 | 23 |
| All accidental deaths | 407 | 37 |
| RTA driver | 129 | 40 |
| RTA passenger | 56 | 32 |
| RTA pedestrian | 40 | 40 |
| Fall | 68 | 37 |
| Fire | 31 | 29 |
| Drowning | 22 | 50 |
| At work* | 19 | 16 |
| All suicides | 356 | 47 |
| Hanging | 135 | 80 |
| Poisoning | 102 | 30 |
| Carbon monoxide | 15 | 93 |
| Accident or suicide | 15 | 27 |
| Homicide | 42 | 5 |
| Substance abuse | 537 | 24 |
| Undetermined manner | 35 | 3 |
RTA = road traffic accident
Subject to mandatory public inquiries under the Fatal Accidents and Sudden Deaths Inquiry (Scotland) Act 1976
The initiative currently encompasses Tayside, Fife and Central regions (population 1.1 million) involving three Scottish police forces and nine procurator fiscal offices. From 2006 presumed unnatural deaths from Fife and Central regions were examined by forensic pathologists, with an average external examination rate of 22% (the data are not included above). All presumed natural deaths from the two regions were examined by NHS pathologists, reimbursed on a fee-per-item-of-service basis with the same fee for an external examination as a dissection, so that the decision to perform either was revenue-neutral for the pathologist. Over three years, 2006–2009, NHS pathologists performed 2140 postmortem examinations, 28% by external examination. The two regional groups of pathologists developed different practices, one with consecutive annual external examination rates of 28, 42 and 54%, and the other 20, 18 and 24%.
Opportunities and sensitivities
External examinations have long been an established part of the Scottish death investigative system. Currently, Edinburgh and Aberdeen have external examination rates of around 15–20%, but Glasgow has very few (personal communication with public mortuary staff, 2010). The Dundee initiative achieved an external examination rate of 30% within 2 years. After 2000 the rate increased, facilitated by changes in attitude both generally and among fiscals following the organ retention scandals.9,10 The Shipman scandal11 did not undermine confidence in the system because fiscals were aware that it is based upon a thorough police investigation5 and a detailed focused external examination which can include toxicology.
In England and Wales the coronial service has a medicolegal dissection rate (medicolegal dissections/all deaths in country) of around 22%.12 If the Tayside dissection rate of 6% were applied to England and Wales the current 110,000 dissections per annum would fall to 30,000 with all of the social, resource and management implications.
Just as the option to perform an autopsy is a necessary element in modern scientific death investigation, so too the option to perform an external examination is a necessary element in the death investigative system of any society which aspires to respect human rights. Our data show that a significant minority of the bereaved spontaneously object to dissection and that if there is no legal imperative for dissection then it is possible in almost all cases to comply with their request and still meet the needs of death certification. Weconcur with the view expressed in the Luce report that ‘In cases where the family object to an autopsy it should not be proceeded with unless there is positive indication of the need to investigate a possible crime or lack of medical or other care, or a public health risk that requires the cause of the individual death to be established, in order to prevent similar fatalities’.2 In Queensland, Australia the introduction of mechanisms whereby the views of the bereaved are actively sought and any decision to dissect the body must be justified and documented by the legal authorities is a welcome innovation,13 and is linked to the introduction of an external examination procedure. Section 14(2) of the new Coroners and Justice Act 200914 is permissive of external examinations, so that the procedure could be introduced in England and Wales.
There will always be differences of professional judgement in some deaths as to whether a dissection is required or not. We have found that the patient education of legal colleagues on the medical issues can lead to changes in practice over time even among the seriously risk-averse. Among pathologists it is important to separate revenue concerns which arise in a fee-per-item-of-service system, as exists in England and Wales, from professional standards concerns, since the former may be articulated through the latter. Extension of our initiative was achieved after eliminating such revenue concerns, and it is noteworthy that our own service in Tayside is block-grant funded and provided by salaried staff.
Added value
The decision on whether or not to dissect a body should be based upon the added value which the procedure is likely to offer for the legal investigation as a whole. Every dissection produces more data, but the question is whether these data provide information which adds value with regard to the specific goals of the investigation, rather than collateral information.15,16 Any medical investigation ordered by the coroner, whether autopsy or other test, should be to clarify a defined uncertainty or range of uncertainties about the death and should be at the lowest level of invasiveness likely to resolve the uncertainty. Referrals for autopsy or other technical investigations should never be routine or automatic. This may apply equally after traumatic deaths.2
In many unnatural deaths both the cause and manner of death are apparent following a police investigation, e.g. suicidal hanging,17–19 so dissection may be unnecessary. In road traffic fatalities in which police investigation of the circumstances establishes the causation and death is due to multiple injuries, there seems little point in dissecting the body to document the detail of the injuries, all the more so if the death is still certified as being due to ‘multiple injuries’. On the other hand dissection is necessary in some road traffic fatalities because of, for example, a possible natural death at the wheel, or criminal proceedings.
When it is unclear whether the manner of death is natural or unnatural then a dissection is indicated, since this distinction is a primary purpose of the legal investigation. Where the manner of death is clearly natural, and there is a history of chronic illness but the immediate cause of death is not precisely known, the death does not usually warrant further legal investigation. Whether or not to dissect the body to more precisely establish the natural cause of death is a focus of debate. In England and Wales, the overwhelming majority of bodies dissected have died of natural causes, yet there is no evidence of a proportionate benefit to justify a policy of high autopsy rates in natural deaths.2
However, some diagnoses of natural disease are commonly missed if a dissection is not performed. Our own data (Table 1) confirm previous studies demonstrating that pulmonary thrombo-embolism, ruptured abdominal aortic aneurysm, peritonitis and pneumonia are all underestimated without dissection.15,17–19 Similarly determination of death from the more precise ‘myocardial infarction’ rather than the broader ‘ischaemic heart disease’ more commonly follows dissection,15 and often histopathology. It is axiomatic that certification of natural deaths without dissection and histopathology is less precise and less accurate.17–19 Whether or not we are prepared to accept this random error and imprecision in the certification of some natural deaths referred for investigation is a system-critical policy decision.20 Any debate needs to be grounded in a consensus on the purpose of the medicolegal investigative service.21 In Scotland the procurator fiscal has no responsibility for the accuracy of death certification generally but in England and Wales it has been suggested that the coroner has or should have such a responsibility.22
It is questionable whether the very large numbers of dissections of natural deaths under the auspices of the coroner significantly improve national mortality statistics since cause of death is a judgemental variable, even after dissection, and it would be unrealistic to expect derived mortality data (which gives a single cause of death) to be valid with respect to factual accuracy, completeness and comparability.10,15,23–26 Also the overwhelming majority of all deaths are certified without any autopsy, coronial or otherwise. The Office for National Statistics has stated that there is only a ‘weak’ relationship between the quality of mortality data and the autopsy rate (cited in 2). One negative effect of the high autopsy rate in natural deaths is the weakening of the investigation of unnatural deaths by the drain on available resources, a situation which is both unsustainable and undesirable.2
There is a moral issue also: whether it is acceptable to operate a death investigative system which enforces the dissection of citizens who have died from natural causes principally for the declared purpose of improving the overall accuracy of national mortality statistics. Legal advice to the Luce inquiry was that ‘a simple bureaucratic desire to gather general statistics on the incidence of one natural disease rather than another would not, in our view, be sufficient to override religious or other objections based on the rights contained in Articles 8 and 9 of the Convention’ – the European Convention on Human Rights.2
All of these issues arise against the backdrop of the near extinction of the hospital (consent) autopsy as a means of medical audit and of improving accuracy of death certification.10,20,27 There is an inference that the medical profession as a whole has performed its cost-benefit analysis for consent autopsies and found them wanting. Hospital autopsies require engaging with the bereaved and obtaining consent28 and also consume NHS resources while by contrast medicolegal dissections are enforced and generate income for NHS mortuaries and individual pathologists.1 Today there is a paradox of too few hospital dissections and too many medicolegal dissections.21 We have found that collaborating with the NHS so that dissections of natural deaths in medicolegal cases are available to train young pathologists and to maintain the dissection skills of hospital pathologists mitigates some effects of the decline in hospital consent autopsies without compromising our commitment to making external examinations maximally available.
Footnotes
DECLARATIONS —
Competing interests None declared
Funding None
Ethical approval Not applicable
Guarantor DP
Contributorship DP established the autopsy initiative, designed the casework database, planned the review, resolved data discrepancies and wrote the paper; HP and MJ planned the review and abstracted data; all three authors analysed data and reviewed the literature
Acknowledgements
None
References
- 1.Pounder D. The coroner service. A relic in need of reform. BMJ 1999;318:1502–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Secretary of State Death Certification and Investigation in England, Wales and Northern Ireland. The Report of a Fundamental Review 2003. London: HSMO; 2003. See http://www.kcl.ac.uk/depsta/law/research/coroners/review_june03.pdf [Google Scholar]
- 3.National Confidential Enquiry into Patient Outcome and Death. The Coroner's Autopsy: Do we deserve better? London: NCEPOD; 2006. See http://www.ncepod.org.uk/2006Report/Downloads/ncepod_2006_report.pdf [Google Scholar]
- 4.Furness P. The Coroner's Autopsy: Do we deserve better? London: NCEPOD; 2006. See http://www.ncepod.org.uk/2006Report/Downloads/PeterFurness.pdf [Google Scholar]
- 5.Davison AM, McFarlane JH, Clark JC. Differences in forensic pathology practice between Scotland and England. Med Sci Law 1998;28:283–8 [DOI] [PubMed] [Google Scholar]
- 6.Pounder DJ. Law and forensic medicine in Scotland. Am J For Med Path 1993;14:340–9 [DOI] [PubMed] [Google Scholar]
- 7.Ministry of Justice Reform of the Coroner System Next Stage. Preparing for implementation. London: Ministry of Justice; 2010. See http://www.justice.gov.uk/consultations/docs/coroner-reform.pdf [Google Scholar]
- 8.Sampson H, Johnson A, Carter N, Rutty G. Information before coronial necropsy: how much should be available? J Clin Pathol 1999;52:856–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hall D, Lilleyman JS. Reflecting on Redfern: what can we learn from the Alder Hey story? Arch Dis Child 2001;84:455–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Burton JL, Underwood JCE. Necropsy practice after the ‘organ retention scandal’: requests, performance and tissue retention. J Clin Pathol 2003;56:537–41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pounder DJ. The case of Dr Shipman. Am J For Med Path 2003;24:219–26 [DOI] [PubMed] [Google Scholar]
- 12.The Shipman Inquiry Third report – Death Certification and the Investigation of Deaths by Coroners. London: The Shipman Inquiry; 2003. See http://www.the-shipman-inquiry.org.uk/thirdreport.asp [Google Scholar]
- 13.Coroners Act 2003; Queensland. See http://www.legislation.qld.gov.au/LEGISLTN/ACTS/2003/03AC013.pdf
- 14.Coroners Justice Act 2009. See http://www.opsi.gov.uk/acts/acts2009/pdf/ukpga_20090025_en.pdf .
- 15.O'Sullivan JP. The coroner's necropsy in sudden death: an under-used source of epidemiological information. J Clin Pathol 1996;49:737–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carpenter B, Barnes M, Naylor C, Adkins G, White B. Issues surrounding a reduction in the use of internal autopsy in the coronial system. JLM 2006;14:199–208 [PubMed] [Google Scholar]
- 17.Biggs MJP, Brown LJR, Rutty GN. Can cause of death be predicted from the pre-necropsy information provided in coroners' cases? J Clin Pathol 2008;61:124–6 [DOI] [PubMed] [Google Scholar]
- 18.Rutty GN, Duerden RM, Carter N, Clark JC. Are coroners' necropsies necessary? A prospective study examining whether a ‘view and grant’ system of death certification could be introduced into England and Wales. J Clin Pathol 2001;54:279–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nashelsky MB, Lawrence CH. Accuracy of cause of death determination without forensic autopsy examination. Am J For Med Path 2003;24:313–19 [DOI] [PubMed] [Google Scholar]
- 20.Robinson IA, Marley NJE. Factors predicting cases with unexpected clinical findings at necropsy. J Clin Pathol 1996;49:909–12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Berry C, Lynch S. A misdirected step in the right direction. Med Sci Law 2007;47:93–5 [DOI] [PubMed] [Google Scholar]
- 22.Cooper H, Leigh MAMS, Lucas S, Martin I. The Coroner's autopsy. The final say in establishing cause of death? Med Leg J 2007;75:114–19 [DOI] [PubMed] [Google Scholar]
- 23.Lawler W. The negative coroner's necropsy: A personal approach and consideration of difficulties. J Clin Pathol 1990;43:977–80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Roulson J, Benbow EW, Hasleton PS. Discrepancies between clinical and autopsy diagnosis and the value of post mortem histology; a meta-analysis and review. Histopathology 2005;47:551–9 [DOI] [PubMed] [Google Scholar]
- 25.Death certification and epidemiological research. BMJ 1978;2:1063–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ison TG. Statistical significance and the distraction of ‘scientific proof’. Can Bar Review 2008;87:119–59 [Google Scholar]
- 27.Twisselmann B. Death of the teaching autopsy. Summary of responses. BMJ 2004;328:167 [Google Scholar]
- 28.McDermott MB. Obtaining consent for autopsy. BMJ 2003;327:804–6 [DOI] [PMC free article] [PubMed] [Google Scholar]