Abstract
We measured the mediolateral (ML) and anteroposterior (AP) length, height and widths of the anterior, posterior and inferior section of the resected distal femurs using three dimensional computer tomographic measurements in 200 knees from 100 cadavers. We also calculated the aspect ratio (ML/AP) and compared the measured parameters with that of six conventionally used total knee femoral prostheses. We found that the average ML (70.2±5.5 mm) and AP (53.9±3.8 mm) dimensions from our study were lower than those reported from Western populations. The aspect ratio showed a progressive decline with an increasing antero-posterior dimension. All of the compared designs showed undersizing for the mediolateral dimension distally and for the widths of the resected medial and lateral posterior femoral condyles. But some of the compared designs showed oversizing for the height of the resected medial and lateral posterior femoral condyles. This study provides guidelines for designing a suitable femoral component for total knee prostheses that fit Asian populations.
Keywords: Distal femur anthropometry, Computed tomography, Aspect ratio, Femoral prosthesis
Introduction
Accurate sizing and proper placement of prosthetic components plays a major role in the success and long term survival of total knee arthroplasty (TKA)(Ranawat 1986; Goldberg et al., 1989). The femoral component sizing is an important determinant for achieving a well balanced flexion-extension gap in a TKA. Mediolateral sizing of the femoral component is necessary for proper patellofemoral tracking and uniform stress distribution over the resected distal femoral surface; this contributes to the long term stability of the prosthesis. Most of the total knee prostheses currently available have been developed using measurements from Caucasians. It is well known that Asian subpopulations are smaller with a shorter stature compared to their Caucasian counterparts (Vaidya et al., 2000; Urabe et al., 2003). Caucasian knees have been shown to be generally larger than Asian knees (Low FH et al., 2000). It follows that these discrepancies may give rise to implant size mismatch with the resected bony surface of Asian patients. Therefore, there is a need for the study of anthropometric measures of the resected distal femur in Asian subpopulations to design an accurate and proper-sized femoral component that can provide stability and longevity in these ethnic groups. There are few studies on anthropometric measurements of the distal femur in the Asian populations (Vaidya et al., 2000; Urabe et al., 2003; Ho et al., 2006). We believe that study of the morphometry of the resected distal femur, free of any deformities and osteoarthritic changes, would provide more accurate anthropometric data for the design of a suitable femoral component. We evaluated the anthropometric data from resected distal femurs that were obtained from a large number of Korean cadavers using 3-D computer tomography. These measurements were compared with the dimensions of commonly available total knee femoral component designs in Korea. Based on the anthropometric results of the resected distal femoral surface, we suggest the design parameters for the total knee femoral component that would be suitable for a majority of the Korean population.
Materials and Methods
We performed the study on 200 femurs obtained from 50 male and 50 female cadavers that were without any gross congenital anomaly or deformity. The average age at the time of death was 49 years (21~60 years) for the males and 54.3 years (38~60 years) for the females. The average height was 166 cm for the males and 156 cm for the females, and the femoral length was 44.3±2.3 cm for the males and 40.6±2.2 cm for the females. All of the measured parameters were analyzed by two of the authors independently.
Method for measurement
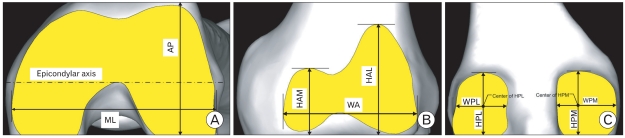
Fresh cadavers were placed supine in the scanner with both knees taped to the scanner platform in the extended position with the patella facing towards the ceiling. Tomograms of 1 mm axial thickness of high resolution were obtained from the hip joint to the ankle joint. A three-dimensional surface model of the knee joint was reconstructed on the computer using the Mimics program (Ver. 13.0, Materialise, Belgium); the bony cuts and measurements were performed using the same program. The osteophytes surrounding the distal femoral cut surface, if any, were excluded from the measurements. The mechanical axis of the femur was first drawn by connecting the center of the femoral head to the center of the femoral intercondylar notch as defined previously by Moreland et al. (Moreland et al., 1987). A distal femoral cut was made 10 mm proximal to the bottom of medial femoral condyle, perpendicular to the mechanical axis. An anterior cut was performed flush with the anterior cortical surface of the femur and parallel to the femoral clinical epicondylar axis with notch. A posterior condylar resection was also made parallel to the clinical epicondylar axis with a thickness of 10 mm from the posterior medial condyle. The AP dimension was defined as the perpendicular distance between the anterior cut surface and the end of posterior condyle. The mediolateral dimension (ML : MedioLateral length) was defined as the longest mediolateral measurement of the distal femoral cut surface drawn parallel to the anterior cut (Fig. 1A). We defined the largest length of the resected medial (HAM : Height of Anterior Medial condyle) and lateral anterior femoral condyles (HAL: Height of Anterior Lateral condyle) as the perpendicular distance from the distal cut surface to the most proximal point of the resected condyles (Fig. 1B). A HAM measurement was possible in only 119 knees (male-61, female-58); a definite proximal margin separating it from the proximal margin of the HAL could not be defined in the other cases. The largest width of the resected anterior condyle (WA : Width of Anterior condyle) was measured parallel to the distal cut. We measured the length of the resected posterior condyles as the perpendicular distance from the distal cut surface to the most proximal point of the resected posterior condyles (HPL : Height of Posterior Lateral condyle, HPM : Height of Posterior Medial condyle) and the width of the posterior condyles (WPL : Width of Posterior Lateral condyle, WPM : Width of Posterior Lateral condyle) at the midpoints of the lines HPL and HPM (Fig. 1C).
Fig. 1.
Schematic representation of the (A) resected distal femoral surface showing the mediolateral (ML) dimension, anteroposterior (AP) dimension and the clinical epicondylar axis. Anterior and posterior cuts were made parallel to the clinical epicondylar axis. (B) resected anterior femoral condyle surface showing the heights of the anterior medial (HAM) and lateral condyles (HAL), width of the anterior condyle (WA). (C) resected posterior femoral condyle surface showing the heights (HPM and HPL) and widths (WPM and WPL) of the posterior medial and lateral femoral condyles.
We calculated an aspect ratio (the medio-lateral dimension divided by the antero-posterior dimension×100) as described by Hitt et al.(Hittt et al., 2003). The mean values of the measurements were calculated and comparisons were made with similar values from six commonly used total knee femoral component designs: Scorpio, Duracon and Triathlon (Stryker Howmedica Osteonics, Allendale, NJ), PFC and LCS (Depuy-Johnson & Johnson, Warsaw, IN) and Nexgen (Zimmer, Warsaw, IN). We also attempted to analyze our findings in comparison with the previously published anthropometric studies on the distal femur in other population groups.
Statistical analysis
Statistical analysis was performed using the Student t-test, the Paired t-test and Pearson's correlation coefficient with SPSS for Windows (version 12.0, SPSS, Chicago, IL). Values for P<0.05 were accepted as significant. The Pearson correlation coefficient was represented as r.
Results
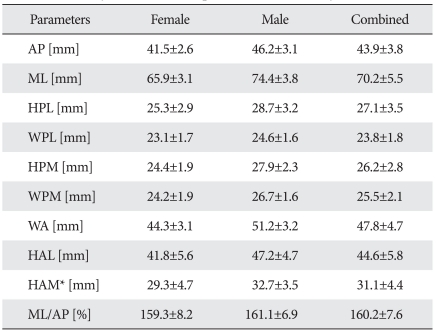
To define the suitable size for the total knee femoral component in the Korean population, we studied the anthropometry of the resected distal femur in 200 knees from 100 cadavers. The measurements are summarized in Table 1.
Table 1.
Summary of the measured parameters in our study
* HAM could be measured in only 119 knees (female 58, male 61).
AP and ML dimensions
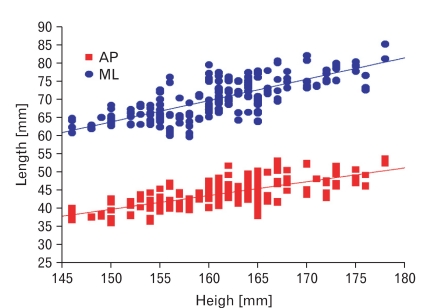
To define the gross size of the resected distal femur, we measured the antero-posterior (AP) and medio-lateral (ML) dimensions. We found that the average antero-posterior (AP) and medio-lateral (ML) dimensions for the Korean population were 53.9±3.8 mm and 70.2±5.5 mm, respectively. The AP and ML dimensions of the male distal femur were on average 11% greater than those of females. A positive correlation was observed between the AP and ML dimensions of the distal femur and population height. (r=0.7, P<0.01) (Fig. 2). These results show that comparatively smaller sized femoral components are needed for the females who make up the larger percentage of TKA patients in the Korean population.
Fig. 2.
Anteroposterior (AP) and mediolateral (ML) dimensions of the resected distal femoral compared to the height of the study population. Both AP and ML dimensions showed a positive correlation to the height of the population (r=0.7).
Dimensions of the condyles
To anticipate the anterior and posterior extent of the medial and lateral condyles of the femoral component, we measured the maximal height and width of the resected medial and lateral condyles anteriorly and posteriorly at well defined points. We found that the maximal height of the lateral femoral anterior condyle was longer than the medial femoral anterior condyle by 13.5±1.4 mm in concordance with the "piano sign" described in TKA. Posteriorly, we found that the medial condyle (25.5±2.1 mm) was wider than the lateral condyle (23.8±1.8 mm), this was statistically significant (P<0.05). We found no statistically significant difference (P>0.05) between the heights of the medial (26.2±2.8) and lateral (27.1±3.5) posterior femoral condyles although the height of the lateral posterior condyle was greater than the medial posterior femoral condyle. These findings show the need for a more proximal extension of the lateral anterior femoral condyle compared to the medial anterior femoral condyle.
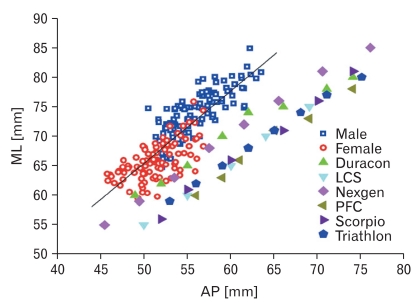
Comparison of ML and AP dimensions with the femoral component
To identify the ideal size of the femoral component needed in the Korean population, we compared the ML and AP dimensions of the distal femur with comparative values from six conventional femoral prostheses (Fig. 3). We found that all of the six femoral prostheses were undersized in the mediolateral dimension, for our population data, compared to the anteroposterior dimensions. A greater difference was noted in the dimensions of the femurs from males. Our measurements show that there is a need for some conventional prostheses with a smaller AP dimension than the conventional AP dimensions in our population.
Fig. 3.
The resected distal femoral mediolateral (ML) and anteroposterior (AP) dimensions in 100 knees of females and males each compared with that of the six conventional femoral designs of total knee arthroplasty. The lines represent the average values for the female and male population. All the femoral designs showed mediolateral undersizing for matching AP dimensions and no availability of smaller AP dimensions suited for our population.
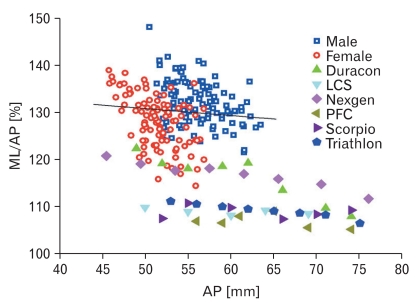
Comparison of the aspect ratio and AP dimension with that of the femoral component
To anticipate the shape of the distal femoral component, that is suitable for the Korean population, we calculated the aspect ratio and compared it with the AP dimension of the resected distal femur (Fig. 4). The aspect ratio of the resected distal femur, for our population, depicted a progressive decline with an increasing AP dimension, regardless of gender. By contrast, all six femoral prostheses showed a relatively constant and lowered aspect ratio as compared to the Korean population data.
Fig. 4.
The distal femoral aspect ratio (ML/AP in %) and the anteroposterior dimension (AP) in 100 knees of females and males each compared with that of six conventional femoral designs. The line represents the average values for the female and male population. The population data shows a progressive decline in the aspect ratio with increasing size of the knee, whereas all of the femoral designs show a relatively constant aspect ratio.
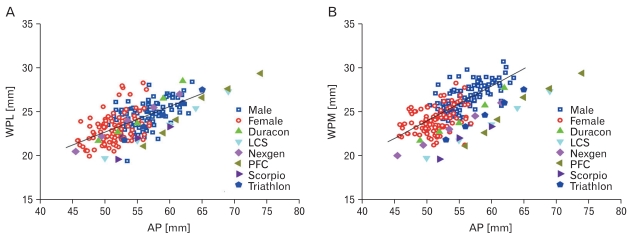
Comparison of the widths of the posterior medial and lateral condyles with that of the femoral component
To assess the coverage of the resected distal femur posteriorly, we compared the widths of the resected medial and lateral posterior femoral condyle with that of the femoral component. We assessed the widths of the posterior medial and lateral femoral condyles in relation to increasing AP dimensions of the resected distal femur and prostheses (Fig. 5). We found that for matching AP dimensions, of the resected distal femur and the prostheses, the widths of the posterior medial femoral condyles of our population tended to be greater than the widths of the medial posterior femoral condyles of all six prostheses. But the widths of the posterior lateral condyle of two prostheses tended to be greater than the widths of the lateral posterior femoral condyles of our population. Especially the large size AP dimensions showed the severe oversize problems.
Fig. 5.
Comparison of the width of the resected posterior femoral medial condyle (A) and posterior femoral lateral condyle (B) with that of femoral designs for matching AP dimensions. The line represents the average values for the female and male population. All designs show undercoverage for both condyles.
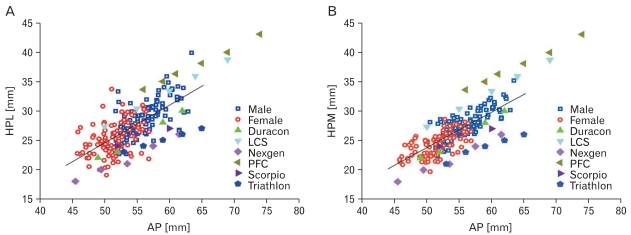
Comparison of the height of the posterior medial and lateral condyles with that of the femoral component
To assess the coverage of the resected distal femur posteriorly, we compared the heights of the resected medial and lateral posterior femoral condyle with that of the femoral component (Fig. 6). With comparable AP dimensions of the resected distal femur and prostheses, the height of the medial and lateral posterior femoral condyles were smaller than the compared femoral designs in two groups of prostheses. This observation indicates the need for decreasing the heights of the medial and lateral posterior femoral condyles of our femoral components compared to the some conventional AP dimensions (LCS, PFC).
Fig. 6.
Comparison of the height of the resected posterior femoral medial condyle (A) and posterior femoral lateral condyle (B) with that of the femoral designs for matching AP dimensions. The line represents the average values for the female and male population. The PFC femoral design closely matches our population data with larger AP dimensions.
Discussion
In total knee arthroplasty, a precise match between the resected bony surface and the prosthetic components can reduce the complications and maximize the survival rate of the prosthesis (Hitt et al., 2003). Morphometry of the resected bony surfaces of the knee joint shows variation in comparisons between Caucasian and Asian populations (Low et al., 2000). Therefore, it is essential to determine the anthropometric measurements of the distal femur, at the resection level, to design a suitable total knee femoral component that fits a given population.
Medial or lateral overhang could result in soft tissue irritation and interfere with the ligament balancing. This results in limitation of the range of joint movement, incomplete correction of the deformities and induces pain in the postoperative period. Undersizing in the mediolateral plane may lead to placement of the implant on the weaker cancellous bone, which could be a source of increased bleeding into the knee joint in the immediate postoperative period and reduce the effectiveness of the implant over the long term. Mediolateral size mismatch could affect patellar tracking especially during the flexion of the knee joint. Anteroposterior sizing of the femoral component is essential as it is an important factor in maintaining the flexion-extension gap balance and optimal tension for the quadriceps (Vaidya et al., 2000). The AP dimension has been a widely used parameter for implant sizing as it is strongly associated with normal gait motion and accurate balancing of the ligaments in flexion and extension (Dorr & Boiardo, 1986). Thus, we compared all other dimensions with reference to the AP dimensions.
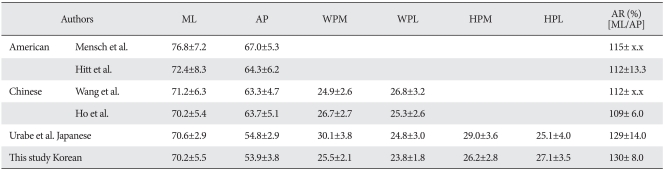
We performed anterior and the posterior cuts parallel to the clinical epicondylar axis to allow for a flexion-extension gap balance maintenance. A thickness of 10 mm in the distal and the posterior cut simulated the optimal cutting thickness performed for the majority of the total knee cases. The gross size of the distal femur (ML and AP), in females, was found to be smaller than that in males by 11%; this finding is consistent with reports by Mensch & Amstutz (Mensch & Amstutz, 1975). Both the AP and ML lengths were found to be smaller than in Western populations but similar to the Japanese population (Table 2). We found a positive correlation between the height of the population and ML and AP dimensions of the distal femur similar to the findings reported in the Caucasian population by Mensch et al. (Mensch & Amstutz, 1975).
Table 2.
Summary of the morphometry of the distal femur (in mm) by different authors
ML: mediolateral diameter, AP: anteroposterior dimension, WPM: medial posterior condyle width, WPL: lateral posterior condyle width, HPM: medial posterior condylar height, HPL: lateral posterior condylar height, AR (%): aspect ratio.
We found that all six femoral designs were undersized mediolaterally for comparable anteroposterior dimensions with the population data. This is a very commonly encountered peroperative finding in Korean patients undergoing TKA where we have observed mediolateral undercoverage for femoral components with matching anteroposterior dimensions. We therefore suggest that femoral prostheses be designed with several ML lengths for a given AP dimension.
The term 'aspect ratio' defines the relationship of the medio-lateral dimension to the antero-posterior dimension; this acts as a guide to predict the shape of the anticipated prostheses. An aspect ratio of 100% indicates that the ML dimension equals the AP dimension, and predicts a circular shape for a suitable femoral component. Therefore, it follows that an aspect ratio over 100% indicates that the shape of the anticipated femoral component becomes medio-laterally oval. The average aspect ratio of our population group (130%) was similar to that of the Japanese population (129%) but higher compared to the Chinese (109~112%) or American population (112~115%) (Table 2). We compared the aspect ratio to the AP dimension of our population data with that of the total knee femoral component designs. All of the six total knee femoral component designs compared showed a relatively constant aspect ratio whereas the population data showed a declining aspect ratio with increasing AP dimension of the distal femur. A constant aspect ratio of the femoral component indicates a constant shape for the prosthesis. A progressive fall in the aspect ratio of the population indicates the need for changing the shapes of the femoral component with an increase in the AP dimension. We propose an alteration in the ML and AP dimensions of the available prostheses so that their aspect ratio matches the morphologic data for the Korean population.
Urabe et al. found that the width of the medial posterior femoral condyle was greater than the lateral posterior femoral condyle width by an average of 5.5 mm in the Japanese population (Urabe et al., 2003). We found a comparatively smaller but statistically significant difference (1.7 mm) in the widths of the medial and lateral posterior femoral condyle in our population. The height of the medial posterior femoral condyle was larger than the lateral posterior femoral condyle height by an average of 4 mm in the Japanese population. By contrast, we found that the height of the lateral posterior femoral condyle was greater than the medial posterior femoral condyle in our population though the difference was small (0.9 mm) and statistically not significant. This finding, different from the Japanese population, is significant for preoperative assessment in our population. If the height of the resected posterior lateral condyle is significantly smaller then the height of the resected posterior medial condyle in our population, this suggests that either there is excessive external rotation in the posterior cut or there are severe osteophytes at the posterior medial femoral condyle that need to be osteotomized. Based on these observations, we suggest that it would be better to have similar heights, of the lateral posterior femoral condyles, for femoral prosthesis designs in our population.
According to our evaluation, a femoral component with a size variation between 60~80 mm in the mediolateral length and 45~65 mm in the anteroposterior length would be suitable for the majority of the Korean population. The aspect ratio of the implants must be re-designed to match the morphologic data so that there is no medio-lateral undersizing for given AP dimensions of the population. For better coverage of the resected posterior femoral condyles in some conventional prostheses, smaller widths and heights of the posterior medial and lateral femoral condyles and smaller widths of the posterior lateral femoral condyle for the conventional anteroposterior dimensions are advised.
A major limitation of our study is the lack of comparisons with similar aged patients evaluated during surgery. Moreover, there is always a possibility of additional variations in dimensions in the cut surface produced during actual surgery, according to the stage of the disease, compared to the cut surface produced by computed tomography under constant conditions in relatively normal bone. However, our study emphasis is on providing anthropometric data of the distal femur based on the commonly performed cut and inclination.
Our results obtained from the three-dimensional surface model constructed by CT images. The computational model study could get more clear and exact data easily than dry bone measurement study. Because of the geometrical operations and the mathematical relations could be used for measuring. Moreover the computational model had less measurement error caused by shrinkage than the dry bones.
In conclusion, our study provides anthropometric data on the resected distal femur for TKA in the Korean population. The dimensional relationships of the distal femur with conventional total knee femoral components, shown in this study, may be used as a guideline for improving the design of future total knee prostheses for the Korean population. Similar anthropometric studies are advised in other population groups for achieving the goal of improved outcomes for total knee arthroplasty.
Acknowledgements
This work was supported by National Research Foundation of Korea Grant funded by the Korean Government (314-2007-1-E00002).
References
- 1.Dorr LD, Boiardo RA. Technical considerations in total knee arthroplasty. Clin Orthop Relat Res. 1986;205:5–11. [PubMed] [Google Scholar]
- 2.Goldberg VM, Figgie HE, 3rd, Figgie MP. Technical considerations in total knee surgery. Management of patella problems. Orthop Clin North Am. 1989;20:189–199. [PubMed] [Google Scholar]
- 3.Hitt K, Shurman JR, 2nd, Greene K, et al. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003;85-A(Suppl 4):115–122. [PubMed] [Google Scholar]
- 4.Ho WP, Cheng CK, Liau JJ. Morphometrical measurements of resected surface of femurs in Chinese knees: correlation to the sizing of current femoral implants. Knee. 2006;13:12–14. doi: 10.1016/j.knee.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 5.Low FH, Khoo LP, Chua CK, Lo NN. Kinematic analysis of total knee prosthesis designed for Asian population. Crit Rev Biomed Eng. 2000;28:33–40. doi: 10.1615/critrevbiomedeng.v28.i12.70. [DOI] [PubMed] [Google Scholar]
- 6.Mensch JS, Amstutz HC. Knee morphology as a guide to knee replacement. Clin Orthop Relat Res. 1975;112:231–241. [PubMed] [Google Scholar]
- 7.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69:745–749. [PubMed] [Google Scholar]
- 8.Ranawat CS. The patellofemoral joint in total condylar knee arthroplasty. Pros and cons based on five- to ten-year follow-up observations. Clin Orthop Relat Res. 1986;205:93–99. [PubMed] [Google Scholar]
- 9.Urabe K, Miura H, Kuwano T, et al. Comparison between the shape of resected femoral sections and femoral prostheses used in total knee arthroplasty in Japanese patients: simulation using three-dimensional computed tomography. J Knee Surg. 2003;16:27–33. [PubMed] [Google Scholar]
- 10.Vaidya SV, Ranawat CS, Aroojis A, Laud NS. Anthropometric measurements to design total knee prostheses for the Indian population. J Arthroplasty. 2000;15:79–85. doi: 10.1016/s0883-5403(00)91285-3. [DOI] [PubMed] [Google Scholar]
- 11.Wang SW, Feng CH, Lu HS. A study of Chinese knee joint geometry for prosthesis design. Chin Med J (Engl) 1992;105:227–233. [PubMed] [Google Scholar]