Abstract
South Africa is in the midst of one of the world’s most devastating HIV/AIDS epidemics and there is a well documented association between violence against women and HIV transmission. Interventions that target men and integrate HIV prevention with gender-based violence prevention may demonstrate synergistic effects. A quasi-experimental field intervention trial was conducted with two communities randomly assigned to receive either: (a) a five session integrated intervention designed to simultaneously reduce gender-based violence (GBV) and HIV risk behaviors (N=242) or (b) a single 3-hour alcohol and HIV risk reduction session (N=233). Men were followed for 1, 3, and 6-months post intervention with 90% retention. Results indicated that the GBV/HIV intervention reduced negative attitudes toward women in the short term and reduced violence against women in longer term. Men in the GBV/HIV intervention also increased their talking with sex partners about condoms and were more likely to have been tested for HIV at the follow-ups. There were few differences between conditions on any HIV transmission risk reduction behavioral outcomes. Further research is needed to examine the potential synergistic effects of alcohol use, gender violence, and HIV prevention interventions.
Introduction
South Africa has among the most devastating and fastest growing HIV/AIDS epidemics in the world, with as many as one in four South Africans living in urban townships and informal settlements infected with HIV (Shisana et al., 2005). In many areas of South Africa, as many as twice the number of women are living with HIV/AIDS as men (UNAIDS/WHO, 2006). One important factor that facilitates the AIDS gender gap is the power imbalance that characterizes heterosexual relationships. In South Africa, women’s risks for sexual assault are known to increase their risks for sexually transmitted infections (STI) including HIV/AIDS (Garcia-Moreno & Watts, 2000; Jewkes et al., 2001). HIV positive women in southern Africa, for example, experience more unwanted sexual contact and relationship violence than HIV negative women (Dunkle et al., 2004; Van der Straten et al., 1998). South African men, like men in most societies, possess greater control and power than women in their sexual relationships (Ajuwon et al., 2002). Although HIV prevention interventions targeting women have dominated AIDS research and public health practices, condom use and other safer sex behaviors, including female condom use, requires men to initiate or cooperate in preventive actions. Women who suggest using condoms with a resistant sex partner may experience adverse consequences, including raising partner suspicions about their sexual histories. Women who initiate condom use may find themselves vulnerable to rejection and potential loss of financial support from their male relationship partners. Men are therefore essential agents of change in reducing sexual risks for HIV/AIDS to themselves and their sex partners.
Unfortunately, men’s attitudes toward women impede HIV preventive actions. Research conducted in southern Africa consistently shows that men believe they are more powerful than women and that men are expected to control women in their relationships (Jewkes et al., 2001; Kalichman, Kaufman et al., 2005; Morrel, 2002). Adversarial attitudes toward women and social acceptance of violence against women directly influence HIV transmission risks. Men who have limited resources and lack opportunities for social advancement often resort to exerting control over women (Boonzaier, 2005; Jewkes & Abrahams, 2002). Power disparities enable men to maintain multiple concurrent partners and support their reluctance to use condoms (Carter et al., 2007).
Although few in number, there are community-based programs that target men for HIV risk reduction in South Africa. For example, Men as Partners in Reproductive Health (MAP) is a program disseminated throughout southern Africa with considerable community acceptance (Peacock & Levack, 2004). The MAP program engages small groups of men for five consecutive full day workshops that address gender-based violence, attitudes toward women, and HIV/STI risk reduction. Although widely implemented there are no published outcome evaluations of the MAP program. Another program that focuses on younger men, Stepping Stones has been tested in a randomized trial in South Africa. The outcomes of this study showed that Stepping Stones did not reduce HIV transmission, although there were significant gains in preventing herpes (HSV) transmission, increasing condom use, reductions in unprotected sex acts, and reductions in gender-based violence (Jewkes et al., 2008). Given the pattern of results, the lack of HIV prevention outcomes in this trial is perplexing, especially because the study was designed for sufficient statistical power to detect changes in HIV incidence. Addressing gender-based violence for HIV prevention is also a focus of structural interventions such as those that empower women with financial independence to reduce gender-based violence (Andersson et al., 2008; Jan et al., 2008; Pronyk et al., 2006). These interventions are grounded in the concept that reducing gender violence will synergize to reduce women’s HIV transmission risks. This rationale may also transfer to men, where increasing partner protective behaviors to reduce gender violence may synergize to reduce HIV transmission risks.
The current study tested an integrated intervention designed to simultaneously reduce gender-based violence and reduce HIV transmission risks among South African men. The intervention content was grounded in a unifying behavioral theory, developed specifically for South African men, and pilot tested for cultural appropriateness and community acceptance. The rationale for the intervention states that reductions in gender violence, reductions in numbers of partners, and increased condom use are all related as partner protective behaviors. We therefore expected that a single integrated intervention model would synergize to impact a cluster of behaviors. The initial pilot test of this concept did not include a control condition and did not include any follow-up assessments beyond a post-test (Simbayi et al., 2008). The initial pilot findings showed a high-degree of community acceptance for the intervention among men and demonstrated increases in AIDS knowledge, reductions in HIV risk supportive attitudes, and reductions in acceptance of violence against women. In this study, we hypothesized that an intensive integrated gender-based violence and HIV risk reduction intervention would demonstrate reductions in HIV risks as well as reductions in violence against women, relative to a brief alcohol/HIV risk-reduction intervention.
Methods
Participants
We recruited 475 African men living in two townships in Cape Town South Africa. We used methods of chain recruitment to reach men in their social networks. Active and passive word of mouth techniques were used and resulted in groups of men who were socially connected to each other within, but not between, communities. Participants were all African men of Xhosa cultural heritage. Men were on average 30.2 years old (SD = 9.5) and had a mean of 10.8 years (SD = 2.0) of education. The vast majority of men were unemployed (N = 422, 89%), and 27 (6%) men where married, with 234 (49%) having had children. More than half of the sample had been tested for HIV with 15 (6% of tested) disclosing that they had tested HIV positive.
Gender-based violence/HIV (GBV/HIV) prevention intervention
The five session gender violence and HIV risk reduction integrated intervention was grounded in Social Cognitive Theory (Bandura, 1997), with particular attention to enhancing behavior change self-efficacy and altering risk-related outcome expectancies. The intervention sessions have been described in detail elsewhere (Simbayi et al., 2008). In each component of the intervention, men examined the personal and community consequences of gender violence and HIV/AIDS, explored behavioral alternatives, observed models of behavior change, and participated in behavioral rehearsal skills building activities with facilitated feedback.
The intervention emphasized sexual transmission risk reduction and gender based violence reduction through skills building and personal goal setting. The intervention activities were also geared toward addressing gender roles, particularly exploring meanings of masculinity and reducing adversarial attitudes toward women. Participants identified high-risk sexual behaviors (triggers), leading to problem solving skills as applied to identifying and recognizing risk. These same concepts were applied to identifying and problem solving antecedents to violent reactions toward women. Condom use skills were trained through interactive group activities and sexual communication skills were rehearsed in response to sexual risk scenarios for skills training. Specifically, the intervention groups used scenes selected from popular South African films and television to form the context of role plays for risk reduction as used in previous HIV prevention interventions (e.g., Kalichman et al., 1998, 2001). Video scenes to establish contexts for role plays and problem solving were used for both HIV risk reduction and gender violence prevention components. Men portrayed in the gender violence and HIV risk scenarios provided a context for examining personal history of violent reactions to women and resistance to using condoms. Participants provided feedback to each other in behavioral rehearsal enactments and worked toward setting goals for both gender violence and HIV risk reduction.
The intervention also included a major segment on training men to become vocal advocates for risk reduction behavior changes with other men in their community. Participants learned communication skills for initiating conversations about HIV prevention and gender based violence (Friedman et al., 2006). We asked participants to select the person in their life they wanted to ‘teach’ and set a goal to talk with that person about gender violence and HIV/AIDS. Participants anticipated potential barriers that might hinder their sharing information and talking with friends about HIV/AIDS and violence against women. As a group, the men problem solved the barriers to talking with others about gender violence and HIV/AIDS, including selecting the best time and place, initiating conversations, and preparing for resistance or even rejection. The participants role-played talking with others about domestic violence and HIV/AIDS. The advocacy skills component of the intervention was modeled after previous interventions that used similar concepts (Kelly et al., 1997; Latkin et al., 2003).
Alcohol/HIV prevention intervention
The comparison intervention in this study was an alternative HIV prevention intervention that has been pilot tested in previous research (Kalichman et al., 2008). The intervention consisted of a single 3-hour interactive small group. The HIV/AIDS information/education component was similar to the GBV/HIV intervention. Alcohol use was integrated within the motivational component by adapting the World Health Organization’s (WHO) brief alcohol intervention model. Alcohol use in sexual contexts was specifically discussed in relation to risk situations. The final component of the workshop focused on behavioral self-management and sexual communication skills building exercises. This intervention did not address gender based violence and it did not include a peer advocacy component.
Group facilitator training and intervention quality assurance
The group facilitators for both conditions consisted of one man and one woman with prior experience conducting HIV/AIDS education programs. To protect against facilitator drift, the interventions were completely manualized and poster-size flipcharts were used to guide the groups through the session content. The facilitators attended weekly supervision meetings with the project manager to discuss their groups and adherence to the protocol.
Study design and procedures
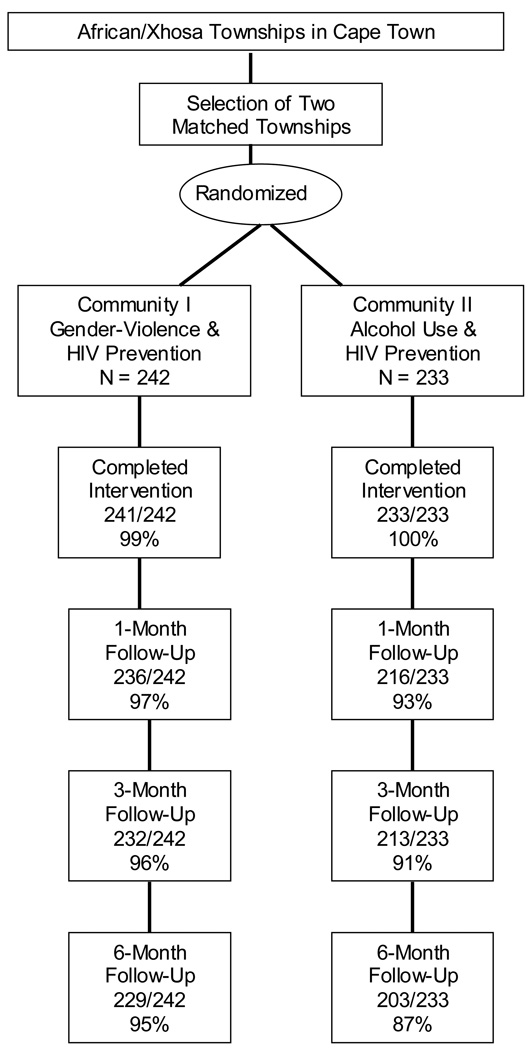
This study used a quasi-experimental design where two demographically similar communities were selected and randomly assigned to receive either the experimental integrated GBV/HIV intervention or the alcohol/HIV risk-reduction intervention. Random assignment occurred by blinded drawing the condition from a bin. This design was selected because of the likely contamination that would occur in a single community with chain referrals of men exposed to both interventions. However, resolving the potential contamination problem came at the cost of randomizing two communities while only being able to analyze outcomes at the individual level. This level of analysis problem limits the interpretation of the current findings. Figure 1 shows quasi-experimental design and the participant flow through the study.
Figure 1.
Participant flow through the quasi-experimental intervention study.
Following informed consent, participants completed baseline assessments and participated in the first group intervention session. Because both interventions were conducted in one week’s time, the two conditions maintained a yoked follow-up schedule, completing 1-month, 3-month and 6-month follow-up assessments in the same timeframe. For both conditions, interventions were delivered in small groups consisting of 8 to 12 men per group. A total of 25 group cycles were conducted. Table 1 shows the characteristics of men recruited in each of the two communities. The two communities differed only slightly in their age and their history of having hit a relationship partner; men in the experimental community were older and more likely to have hit or pushed a sex partner. Retention was also high in both communities, with 95% of men in the experimental community and 87% of men in the comparison community completing 6-month follow-ups (see Table 1).
Table 1.
Demographic and baseline behavioral characteristics of men in two intervention communities.
| GBV/HIV (N = 242) |
Alcohol/HIV (N = 233) |
|||||
|---|---|---|---|---|---|---|
| Variable | N | % | N | % | X2 | p |
| Exchanged sex | 31 | 13 | 30 | 13 | 0.1 | n.s. |
| Has used a condom | 210 | 90 | 207 | 30 | 0.1 | n.s. |
| Number of sex partners in past month | ||||||
| 0 | 23 | 10 | 29 | 12 | ||
| 1 | 101 | 42 | 92 | 40 | ||
| 2 | 67 | 28 | 63 | 27 | ||
| 3+ | 49 | 20 | 49 | 21 | 1.1 | n.s. |
| Diagnosed with an STI | 54 | 23 | 52 | 22 | 0.8 | n.s. |
| Tested for HIV | 116 | 57 | 117 | 51 | 1.7 | n.s. |
| Tested HIV positive | 8 | 6 | 7 | 5 | ||
| Has hit or pushed a sex partner | 135 | 56 | 109 | 47 | 4.2 | .05 |
| Detained for domestic violence | 42 | 18 | 49 | 21 | 0.8 | n.s. |
| Used threats to obtain sex | 38 | 16 | 39 | 17 | 0.8 | n.s. |
| Used force to obtain sex | 47 | 20 | 40 | 17 | 0.5 | n.s. |
| Completed follow-up assessments | ||||||
| 1-month | 236 | 97 | 216 | 93 | 5.5 | .05 |
| 3-month | 232 | 96 | 213 | 91 | 0.2 | n.s. |
| 6-months | 229 | 95 | 203 | 87 | 8.1 | .01 |
| M | SD | M | SD | t | p | |
| Age | 31.6 | 8.6 | 28.8 | 10.1 | 3.2 | .05 |
| Years of Education | 10.7 | 1.9 | 11.0 | 2.0 | 2.0 | n.s. |
Note: GBV/HIV is gender-based violence/HIV intervention; n.s. = not significant.
Participants were compensated 100 South African Rand ($12) for completing baseline assessments, with compensation increasing to 200 South African Rand ($24) at the 6-month follow-up. Issues of social justice for not exploiting participants were weighed against the potential for coercion in determining the proper participant incentives (Shisana et al., 2005). Participants were not paid for attending group sessions, although lunch was served at the groups in both conditions. All of the study procedures were approved by the University of Connecticut and the Human Sciences Research Council in Cape Town’s Institutional Review Boards.
Outcome measures
Measures were administered in English and Xhosa (an indigenous African language spoken in both communities) and included demographic and risk characteristics, theoretical correlates of behavior change (AIDS knowledge, AIDS stigma, risk reduction intentions, acceptance of violence against women), alcohol use, and primary outcomes (sexual risk, sexual protective, and gender-based violence behaviors). Measures were initially developed in English and translated/back translated to Xhosa. Participants where shown page by page how to complete the study measures by using a projected facsimile of the instruments and instructions, assuring that instructions for each measure were carefully described and that participants were given privacy with minimal demand characteristics when responding. Most (90%) participants in this study were able to read and self-administer the measures within approximately 45 minutes. The less than 10% of participants who required assistance were read the items and recorded their own responses to the surveys.
Demographic and risk history characteristics
Participants reported their age, race, years of formal education, whether they were employed and their marital status. Participants indicated whether they had ever given or received money or other material gain in exchange for sex and whether they had ever been diagnosed with a STI. Participants were asked if they had ever been tested for HIV and the results of their most recent HIV test. We also assessed whether participants had ever been detained by the police for domestic violence and whether they had ever used threats of force or actual force to obtain sex.
AIDS knowledge
An 11-item test was used to assess AIDS knowledge. Items were previously used in South Africa (Kalichman & Simbayi, 2005) and reflected information about HIV transmission, condom use, and AIDS-related knowledge and were responded to Yes, No, or Don’t Know. The AIDS knowledge test was scored for the number of correct responses, with Don’t Know responses scored incorrect, possible range of scores 0 to 11 expressed as the percent correct. The AIDS knowledge test demonstrated heterogeneous item content as is expected of knowledge tests, α = .58.
AIDS-related stigmas
Four AIDS-related stigma items were adapted from previous research and developed for use in South Africa (Kalichman et al., 2005). The AIDS stigma items reflected beliefs about negative qualities of people living with AIDS. These items were responded to on a 4-point scale, 1 = Agree, 4 = Disagree, higher mean responses represent stronger endorsement of stigmas, α = .71.
Risk reduction behavioral intentions
Theories of behavior change emphasize intentions to change behavior as important predictors of behavior change (Azjen & Fishbein, 1986). Participants responded to a 9-item measure assessing personal intentions to reduce sexual risk behaviors, such as "I will keep condoms nearby" and “I will try to have fewer sex partners” anchored on a 4-point response set ranging from 1 = I will not do, to 4 = I will do. Higher mean responses indicate stronger behavioral intentions, α = .75.
Sexual and substance use risk behaviors
Participants reported their number of male and female sex partners and the frequency of vaginal and anal intercourse occasions in the past 1-month and 3-month time frames. The two time frames were used to match the follow-up intervals of 1-month and 3, and 6-months without overlap. We asked participants to think back and estimate the number of male and female sex partners they had and the number of sexual occasions in which they practiced vaginal and anal intercourse. Numbers of partners and rates of sexual behaviors were recorded using open response formats. These measures were developed from instruments that have been shown reliable and valid (Schroder et al., 2003). We computed the percent of time that condoms were used by taking the ratio of condoms used/total intercourse. We also defined consistent condom use as 100% of intercourse occasions protected by condoms. Participants also reported whether they had talked with a sex partner about condoms in the past 1-month and 3-month periods.
Participants indicated whether they drank alcohol, defined as beer, wine, or other alcoholic beverages, before sex, representing frequencies of situational use of alcohol (Weinhardt & Carey, 2001). We used open response formats, indicating the number of occurrences in the previous 1-month and 3-months. Participants also reported if they had met sex partners at informal drinking establishments (i.e., shebeens) in the same time periods.
Domestic violence
At each assessment participants were asked whether they had lost their temper with a woman in the previous month and whether they had hit/pushed a sex partner in the previous month. To assess acceptance of violence against women, we administered a 7-item scale that was adapted from previous research (Simbayi et al, 2006). Example items include “A woman who talks disrespectfully to a man in public should expect trouble”, “There are times when a man should hit a woman because of things she has done”, and “A woman who teases a man sexually and doesn’t finish what she started deserves what she gets” (Glick et al., 2000). Items were responded to on a 4-point scale, 1 = Strongly disagree, 4 = Strongly agree, with higher mean scores representing greater acceptance of violence against women. The acceptance of violence against women items represented somewhat heterogeneous content, α = .65.
Data analyses
Variables that were significantly skewed, particularly rates of sexual behaviors, were transformed using the formula log10 (x+1) with non-transformed observed values presented in the tables (Schroder et al., 2003). To test for differential attrition across conditions, 2 attrition (lost vs. retained) × 2 condition/community contingency table chi-square tests were performed at each follow-up assessment point. Differences between community baseline characteristics were analyzed using t-tests and contingency table chi-square tests. Outcomes were examined using analyses of co-variance (ANCOVA) for continuous variables and logistic regressions for categorical variables. All outcome analyses controlled for participant age and baseline values. We used an intent-to-treat approach by including all participants who completed baseline assessments. Individual cell sizes vary due to missing values. Statistical significance was defined using the conventional value of p < .05.
Results
Initial analyses showed that the two communities were relatively homogeneous; with differences only indicated for participant age and history of domestic violence (see Table 1). We also tested for differences between conditions on retention at follow-up assessments. Although retention was high (> 90%) across the two conditions, there were differences observed at the 1-month and 6-month follow-ups; attrition was greater in the alcohol/HIV intervention community than the GBV/HIV intervention community (see Table 1).
Theoretical HIV risk behavior change constructs
Analyses indicated few differences between conditions in HIV risk reduction constructs. There were no differences at any follow-up point for AIDS knowledge and AIDS stigmatizing attitudes (see Table 2). For intentions to reduce HIV risk behaviors there were no differences at the 1-month and 3-month follow-ups. However, at the 6-month follow-up, the GBV/HIV prevention condition demonstrated greater intentions to reduce risk compared to the alcohol/HIV intervention.
Table 2.
Comparison of intervention communities on theoretical behavior change constructs.
| GBV/HIV | Alcohol/HIV | |||||
|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | F | p |
| AIDS knowledge (% correct) | ||||||
| Baseline | 84.5 | 16.2 | 87.8 | 12.7 | ||
| 1-month | 89.5 | 14.4 | 91.0 | 12.3 | 0.1 | n.s. |
| 3-month | 88.4 | 19.6 | 90.3 | 13.2 | 0.1 | n.s. |
| 6-month | 88.4 | 16.7 | 89.1 | 16.4 | 0.2 | n.s. |
| AIDS-related stigma | ||||||
| Baseline | 1.7 | 0.6 | 1.7 | 0.5 | ||
| 1-month | 1.6 | 0.6 | 1.5 | 0.5 | 0.4 | n.s. |
| 3-month | 1.6 | 0.6 | 1.6 | 0.5 | 0.8 | n.s. |
| 6-month | 1.6 | 0.5 | 1.6 | 0.6 | 0.5 | n.s. |
| HIV risk reduction intentions | ||||||
| Baseline | 3.4 | 0.5 | 3.5 | 0.5 | ||
| 1-month | 3.6 | 0.6 | 3.6 | 0.4 | 0.3 | n.s. |
| 3-month | 3.5 | 0.6 | 3.5 | 0.5 | 0.3 | n.s. |
| 6-month | 3.5 | 0.5 | 3.4 | 0.7 | 5.4 | .05 |
| Acceptance of violence against women | ||||||
| Baseline | 2.4 | 0.7 | 2.4 | 0.7 | ||
| 1-month | 2.2 | 0.7 | 2.4 | 0.7 | 5.3 | .05 |
| 3-month | 2.3 | 0.7 | 2.3 | 0.7 | 0.1 | n.s. |
| 6-month | 2.3 | 0.7 | 2.4 | 0.8 | 0.7 | n.s. |
Note: All analyses controlling for age and baseline scores.
Sexual risk and protective behavior change
Consistent with the measures of theoretical change constructs, we found limited evidence for enhanced HIV risk reduction in the GBV/HIV integrated intervention (see Table 3). Men in the GBV/HIV condition talked with their partners about condoms more than men in the alcohol/HIV comparison condition at the 1-month follow-up and were significantly more likely to have been tested for HIV at the 1-month and 3-month follow-ups (see Table 4). The alcohol/HIV condition reported less unprotected sex, fewer alcohol involved sexual encounters, and greater condom use that the GBV/HIV condition at the short-term follow-ups.
Table 3.
Comparison of intervention communities on continuous sexual risk behavior outcomes.
| GBV/HIV | Alcohol/HIV | |||||
|---|---|---|---|---|---|---|
| Variable | M | SD | M | SD | F | p |
| Unprotected intercourse | ||||||
| Baseline past 1-month | 3.1 | 7.2 | 2.0 | 4.2 | ||
| 1-month | 1.7 | 3.6 | 1.4 | 4.1 | 2.2 | n.s. |
| Baseline past 3-months | 7.2 | 18.1 | 4.6 | 12.6 | ||
| 3-month | 3.9 | 10.9 | 1.7 | 4.3 | 6.5 | .01 |
| 6-month | 2.5 | 7.2 | 3.1 | 10.3 | 0.5 | n.s. |
| Percent intercourse condom protected | ||||||
| Baseline past 1-month | 64.3 | 38.2 | 72.0 | 32.5 | ||
| 1-month | 69.9 | 34.3 | 76.1 | 32.9 | 1.1 | n.s. |
| Baseline past 3-months | 64.9 | 36.9 | 70.1 | 33.9 | ||
| 3-month | 72.3 | 32.7 | 73.7 | 33.6 | 0.1 | n.s. |
| 6-month | 74.1 | 31.8 | 72.5 | 34.9 | 0.3 | n.s. |
| Drank alcohol before sex | ||||||
| Baseline past 1-month | 3.3 | 5.1 | 2.5 | 3.9 | ||
| 1-month | 4.0 | 15.5 | 1.8 | 2.9 | 3.9 | .05 |
| Baseline past 3-months | 6.6 | 15.8 | 4.5 | 6.9 | ||
| 3-month | 3.6 | 8.8 | 2.6 | 5.1 | 1.5 | n.s. |
| 6-month | 3.4 | 8.6 | 3.6 | 11.8 | 0.4 | n.s. |
| Number of sex partners past 1-month | ||||||
| Baseline | 1.6 | 0.9 | 1.5 | 0.9 | ||
| 1-month | 1.5 | 0.9 | 1.4 | 0.9 | 1.7 | n.s. |
| 3-month | 1.5 | 0.9 | 1.4 | 0.9 | 1.5 | n.s. |
| 6-month | 1.6 | 0.9 | 1.4 | 0.9 | 4.9 | .05 |
| Sex partners met at informal drinking places | ||||||
| Baseline past 1-month | 0.7 | 1.5 | 0.8 | 1.7 | ||
| 1-month | 1.0 | 2.5 | 0.6 | 1.9 | 4.9 | .05 |
| Baseline past 3-months | 1.4 | 2.8 | 1.3 | 2.6 | ||
| 3-month | 1.5 | 3.5 | 1.2 | 2.9 | 1.3 | n.s. |
| 6-month | 1.3 | 3.7 | 1.5 | 7.4 | 0.3 | n.s. |
| Talked with partner about condoms | ||||||
| Baseline past 1-month | 4.2 | 6.8 | 3.5 | 4.9 | ||
| 1-month | 6.8 | 11.3 | 4.6 | 8.1 | 4.8 | .05 |
| Baseline past 3-months | 7.3 | 15.7 | 7.3 | 13.6 | ||
| 3-month | 7.3 | 13.7 | 7.2 | 13.4 | 1.1 | n.s. |
| 6-month | 9.5 | 17.3 | 8.7 | 18.3 | 1.1 | n.s. |
Note: All analyses controlling for age and baseline scores.
Table 4.
Comparison of intervention communities on categorical sexual risk and gender violence behavior outcomes.
| GBV/HIV | Alcohol/HIV | |||||
|---|---|---|---|---|---|---|
| Variable | N | % | N | % | OR | 95%CI |
| 100% condom use | ||||||
| Baseline | 79 | 38 | 85 | 46 | ||
| 1-month | 84 | 43 | 101 | 56 | 1.7* | 1.1–2.7 |
| 3-month | 88 | 43 | 86 | 50 | 1.3 | 0.8–2.0 |
| 6-month | 91 | 51 | 80 | 51 | 1.1 | 0.7–1.8 |
| Tested for HIV in past month among men not tested at baseline |
||||||
| 1-month | 40 | 18 | 17 | 8 | 0.4** | 0.2–0.8 |
| 3-month | 48 | 21 | 28 | 13 | 0.5* | 0.3–0.9 |
| 6-month | 47 | 21 | 30 | 15 | 0.7 | 0.4–1.1 |
| Did not lose temper with a woman among men who had at baseline |
||||||
| 1-month | 53 | 23 | 27 | 13 | 0.5** | 0.3–0.7 |
| 3-month | 43 | 18 | 32 | 15 | 0.7 | 0.4–1.2 |
| 6-month | 52 | 23 | 29 | 14 | 0.5** | 0.3–0.8 |
| Hit a sex partner in the past month | ||||||
| 1-month | 54 | 23 | 40 | 19 | 1.3 | 0.8–2.0 |
| 3-month | 84 | 36 | 62 | 29 | 1.2 | 0.8–1.9 |
| 6-month | 72 | 31 | 124 | 61 | 0.3** | 0.2–0.4 |
Note: All analyses controlling for age and baseline values,
p < .05,
p < .01
Domestic violence attitudes and behaviors
Men in the GBV/HIV integrated intervention condition indicated significantly less acceptance of violence against women at the 1-month follow-up assessment, with the difference no longer significant at the subsequent assessments (see Table 2). In addition, men in the GBV/HIV intervention were significantly less likely to have lost their temper with a woman 1-month and 6-months following the intervention (see Table 4). Men in the GBV/HIV intervention were also significantly less likely to have hit/push a sex partner at the 6-month assessment.
Discussion
The current study successfully recruited and engaged a large sample of South African men into two community-based prevention interventions. Confirming previous research, the men in our study demonstrated high-risk for HIV infection, with one in five having been diagnosed with an STI and nearly half reporting two or more sex partners in the previous month. The sample also indicated high-rates of relationship violence, with more than half of men reporting a history of physically assaulting a sex partner and one in five having been detained for domestic violence. Men in the current study therefore reaffirm the urgent need for interventions to prevent both HIV/AIDS and gender-based violence in South Africa.
The results of our quasi-experimental trial partially supported the hypothesized effects of an integrated gender-based violence and HIV/AIDS prevention intervention. We observed reductions in negative attitudes toward women and reductions in the propensity to act violently against women among participants in the GBV/HIV intervention. Men in the GBV/HIV intervention also increased their talking with sex partners about condoms and were more likely to get tested for HIV over the follow-up period, both behaviors that are conceptually consistent with partner protective actions. The GBV/HIV intervention did not, however, demonstrate evidence for efficacy in reducing unprotected sex acts, reducing numbers of sex partners or increasing condom use. The pattern of risk behavior changes observed actually suggests that the alcohol/HIV prevention intervention offered greater potential for sexual risk reduction than that realized in the GBV/HIV prevention intervention. These results are therefore intriguing and suggest that future research may examine more complex integrated models, such as a tripartite intervention approach that integrates alcohol reduction, gender violence prevention, and HIV risk reduction for South African men.
The current study is limited by its use of a two-community quasi-experimental design. Although the two communities in our study were rather homogeneous, the study design did not randomize participants to conditions. Relying on two communities randomized to two conditions yields an inherently weak study design, particularly in terms of examining individual level behavior change. The baseline differences between communities in history of gender violence may have resulted from the chain recruitment procedures and represents another limitation of the study. Our participants were primarily unemployed and were therefore able to attend lengthy workshops, suggesting another limitation of our sample’s generalizability. The GBV/HIV intervention also did not include intersession intervals, reducing men’s opportunities for practicing new skills during the course of the intervention. The two interventions in this study differed in multiple and important ways. The difference in intervention duration, for example, may account for the differential attrition in follow-up assessments as well as potential influences on behavioral response reporting. Our measures were also limited to a relatively few constructs, especially those regarding gender-based violence. Our findings may therefore be explained by constructs that were not assessed in our study. In addition, some of our measures were limited by ceiling effects, most notably AIDS knowledge, reducing our sensitivity for detecting change. The study was also limited by relying entirely on self-reported behaviors, most of which are socially sanctioned. Because reports of sexual risks and domestic violence behaviors may be sensitive to social desirability influences, the rates of risk and violent behaviors observed in this study should be considered lower-bound estimates. The high-degree of variability in our measures, as evidenced by the large standard deviations for variables, also cautions against drawing definitive conclusions from our findings. Our study is also limited by intervening with men from only one of the many cultural groups in South Africa. Future attempts to reduce HIV transmission and gender-based violence risks with men should examine multiple cultural groups.
With these limitations considered, we believe that our current study findings offer new information for HIV prevention efforts in South Africa. HIV/AIDS and gender-based violence remain in great need of immediate effective interventions in South Africa. We are intrigued by the potential effects of both the GBV/HIV and alcohol/HIV intervention outcomes. Alcohol is a known risk correlate to both HIV/AIDS and gender-based violence in South Africa (Abrahams et al., 2004; Phorano et al., 2005). Interventions that directly address alcohol in relation to sexual risks have demonstrated short-term efficacy in previous intervention trials in South Africa (Kalichman et al., 2007; Kalichman, Vermaak et al., 2008). An intervention model that addresses alcohol use in relation to both gender-based violence and HIV/AIDS behavioral risks may prove most promising.
Acknowledgments
National Institute of Mental Health Grant R01-MH MH071160 supported this research.
References
- Abrahams N, Jewkes R, Hoffman M, Laubsher R. Sexual violence against intimate partners in Cape Town: Prevalence and risk factors reported by men. Bulletin of the World Health Organization. 2004;82:330–337. [PMC free article] [PubMed] [Google Scholar]
- Ajuwon AJ, McFarland W, Hudes ES, Adedapo S, Okikiolu T, Lurie P. HIV risk-related behavior, sexual coercion, and implications for prevention strategies among female apprentice tailors, Ibadan, Nigeria. AIDS and Behavior. 2002;6:229–235. [Google Scholar]
- Ajzen I, Madden T. Prediction of goal-directed behaviour: Attitudes, intentions, and perceived behavioral control. Journal of Experimental Social Psychology. 1986;22:453–474. [Google Scholar]
- Andersson N, Cockcroft A, Shea B. Gender-based violence and HIV: Relevance for HIV prevention in hyperendemic countries of southern Africa. AIDS. 2008;22 Suppl 4:S73–S86. doi: 10.1097/01.aids.0000341778.73038.86. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: Freeman; 1997. [Google Scholar]
- Boonzaier F. Women abuse in South Africa: A brief contextual analysis. Feminism & Psychology. 2005;15:99–103. [Google Scholar]
- Carter M, Kraft JM, Koppenhaver T, Galavotti C, Roels T, Kilmax P, et al. “A bull is not meant to remain the Kraal”: Concurrent sexual relationships in Botswana. AIDS and Behavior. 2007;11:822–830. doi: 10.1007/s10461-006-9203-6. [DOI] [PubMed] [Google Scholar]
- Dunkle K, Jewkes R, Brown H, Gray G, McIntyre J, Harlow S. Gender-based violence, relationship power and risk for prevalent HIV infection among women attending antenatal clinics in Soweto, South Africa. Lancet. 2004;363:1415–1421. doi: 10.1016/S0140-6736(04)16098-4. [DOI] [PubMed] [Google Scholar]
- Friedman S, Bolyard M, Mateau-Gelabert P, Goltzman P, Pawlowicz M, Zunino S, et al. Some data-driven reflections on priorities in AIDS network research. AIDS and Behavior. 2006;11:641–651. doi: 10.1007/s10461-006-9166-7. [DOI] [PubMed] [Google Scholar]
- Garcia-Moreno C, Watts C. Violence against women: Its importance for HIV/AIDS. AIDS. 2000;14 suppl 3:S253–S265. [PubMed] [Google Scholar]
- Glick P, Fiske ST, Mladinic A, Saiz JL, Abrams D, Masser B, et al. Beyond prejudice as simple anitpathy: Hostile and benevolent sexism across cultures. Journal of Personality and Social Psychology. 2000;79:763–775. doi: 10.1037//0022-3514.79.5.763. [DOI] [PubMed] [Google Scholar]
- Jan S, Pronyk P, Kim J. Accounting for institutional change in health economics evaluation: A program to tackle HIV/AIDS and gender violence in Southern Africa. Social Science and Medicine. 2008;66:922–932. doi: 10.1016/j.socscimed.2007.11.010. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Abrahams N. The epidemiology of rape and sexual coercion in South Africa: An overview. Social Science and Medicine. 2002;55:1231–1244. doi: 10.1016/s0277-9536(01)00242-8. [DOI] [PubMed] [Google Scholar]
- Jewkes R, Nduna M, Levin J, Jama N, Dunkle K, Puren A, et al. Impact of stepping stones on incidence of HIV and HSV-2 and sexual behaviour in rural South Africa: cluster randomised controlled trial. British Medical Journal. 2001;337:a506. doi: 10.1136/bmj.a506. doi: 10.1136/bmj.a506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Penn-Kekana L, Levin J, Ratsaka M, Schrieber M. Prevalence of emotional, physical, and sexual abuse of women in three South African provinces. South African Medical Journal. 2001;9:315–317. [PubMed] [Google Scholar]
- Kalichman SC, Cherry C, Brown-Sperling F. Effectiveness of a video-based motivational skills-building HIV risk reduction intervention for inner-city African-American men. Journal of Consulting and Clinical Psychology. 1999;67:959–966. doi: 10.1037//0022-006x.67.6.959. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Kaufman M, Simbayi LC, Jooste S. Gender attitudes, sexual violence, and HIV/AIDS risks among men and women in Cape Town, South Africa. Journal of Sex Research. 2005;42:299–305. doi: 10.1080/00224490509552285. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Rompa D, Cage M, DiFonzo K, Simpson D, Austin J, et al. Effectiveness of an intervention to reduce HIV transmission risks in HIV positive persons. American Journal of Preventive Medicine. 2001;21:84–92. doi: 10.1016/s0749-3797(01)00324-5. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Kaufman M, Cain D, Jooste S. Alcohol and HIV/AIDS risk behaviors in Southern Africa: Systematic review of empirical findings. Prevention Science. 2007;8:141–151. doi: 10.1007/s11121-006-0061-2. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, et al. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town South Africa. Journal of Acquired Immune Deficiency Syndromes. 2007;44:594–600. doi: 10.1097/QAI.0b013e3180415e07. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi L, Jooste S, Toefy Y, Cain D, Cherry C, et al. Development of a brief scale to measure AIDS-related stigmas in South Africa. AIDS & Behavior. 2005;9:135–143. doi: 10.1007/s10461-005-3895-x. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Smith G, Mthebu J, Jooste S, et al. Community-based HIV and alcohol risk reduction intervention for men and women in Cape Town, South Africa. Annals of Behavioral Medicine. 2008;36:270–279. doi: 10.1007/s12160-008-9067-2. [DOI] [PubMed] [Google Scholar]
- Kelly JA, McAullife W, Sikkema KJ, Murphy D, Solmai A, Mulry G, et al. Reduction in risk behavior among adults with severe mental illness who learned to advocate for HIV prevention. Psychiatric Services. 1997;48:1283–1288. doi: 10.1176/ps.48.10.1283. [DOI] [PubMed] [Google Scholar]
- Latkin C, Sherman S, Knowlton A. HIV prevention among drug users: Outcomes of a network-oriented peer outreach intervention. Health Psychology. 2003;22:332–339. doi: 10.1037/0278-6133.22.4.332. [DOI] [PubMed] [Google Scholar]
- Morrell R. Changing men in South Africa. Durban, South Africa: University of Natal Press; 2002. [Google Scholar]
- Peacock D, Levack A. The Men as Partners program in South Africa: Reaching men to end gender-based violence and promote sexual and reproductive health. International Journal of Men’s Health. 2004;3:173–188. [Google Scholar]
- Phorano OD, Nthomang K, Ntseane D. Alcohol abuse, gender-based violence and HIV/AIDS in Botswana: Establishing the link based on empirical evidence. Sahara: Journal of Social Aspects of HIV/AIDS. 2005;2:188–202. doi: 10.1080/17290376.2005.9724842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pronyk PM, Hargreaves JR, Kim JC, Morison LA, Phetla G, Watts C, et al. Effect of a structural intervention for the prevention of intimate-partner violence and HIV in rural South Africa: a cluster randomised trial. Lancet. 2006;368(9551):1973–1983. doi: 10.1016/S0140-6736(06)69744-4. [DOI] [PubMed] [Google Scholar]
- Schroder K, Carey M, Vanable P. Methodological challenges in research on sexual risk behaviors: II Accuracy of self-reports. Annals of Behavioral Medicine. 2003;26:104–123. doi: 10.1207/s15324796abm2602_03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shisana O, Rehle T, Simbayi L, Parker W, Bhana A, Zuma K, Connoly C, Jooste S, Pillay V. South African National HIV Prevalence, Incidence, Behaviour And Communication Survey. Cape Town: Human Sciences Research Council Press; 2005. 2005. [Google Scholar]
- Simbayi LC, Kalichman SC. Risk behaviors and risk fatcors for sexually transmitted infection among Youth in an African Township in Cape Town, South Africa. AIDS & Behavior. 2005;9:53–62. doi: 10.1007/s10461-005-1681-4. [DOI] [PubMed] [Google Scholar]
- Simbayi LC, Kalichman SC, Jooste S, Mathiti V, Cain D, Cherry C. HIV/AIDS risks among South African men receiving sexually transmitted infection clinic services who report sexually assaulting women. American Journal of Health Behavior. 2006;30:158–166. doi: 10.5555/ajhb.2006.30.2.158. [DOI] [PubMed] [Google Scholar]
- Simbayi LC, Cloete A, Strebel A, Henda N, Kalichman SC, Cherry C, Kalichman M, Crawford M, Cain D, Shefer T, Thabalala M. HIV/AIDS risk reduction and domestic violence intervention for South African men: theoretical foundations, development, and test of concept. International Journal of Men’s Health. 2008;7:254–272. [Google Scholar]
- UNAIDS/WHO. AIDS epidemic update, 2006. Joint United Nations Programme on HIV/AIDS, 2006. 2006
- Van der Straten A, King R, Grinstead O. Interpersonal violence and HIV infection in women in steady relationships in Kigali, Rwanda. AIDS & Behavior. 1998;2:61–73. [Google Scholar]
- Weinhardt L, Carey MP. Does alcohol lead to sexual risk behavior? Annual Review of Sex Research. 2001;12:125–157. [PMC free article] [PubMed] [Google Scholar]