Abstract
Introduction
Both laparoscopic colectomy and application of enhanced recovery program (ERP) in open colectomy have been demonstrated to enable early recovery and to shorten hospital stay. This study evaluated the impact of ERP on results of laparoscopic colectomy and comparison was made with the outcomes of patients prior to the application of ERP.
Methods
An ERP was implemented in the authors’ center in December 2006. Short-term outcomes of consecutive 84 patients who underwent laparoscopic colonic cancer resection 23 months before (control group) and 96 patients who were operated within 13 months; after application of ERP (ERP group) were compared.
Results
Between the ERP and control groups, there was no statistical difference in patient characteristics, pathology, operating time, blood loss, conversion rate or complications. Compared to the control group, patients in the ERP group had earlier passage of flatus [2 (range: 1–5) versus 2 (range: 1–4) days after operation respectively; p = 0.03)] and a lower incidence of prolonged post-operative ileus (6% versus 0 respectively; p = 0.02). There was no difference in the hospital stay between the two groups [4 (range: 2–34) days in control group and 4 (range: 2–23) days in ERP group; p = 0.4)]. The re-admission rate was also similar (7% in control group and 5% in ERP group; p = 0.59).
Conclusions
In laparoscopic colectomy for cancer, application of ERP was associated with no increase in complication rate but significant improvement of gastrointestinal function. ERP further hastened patient recovery but resulted in no difference in hospital stay.
Keywords: Laparoscopic colectomy, Enhanced recovery program
Introduction
After the benefits of fast post-operative recovery and reduced morbidities without compromise in long-term oncologic outcomes were demonstrated by many studies [1–7], laparoscopic colectomy revolutionized colorectal surgery and gained wide acceptance to become the preferred approach for colon resection. On the other hand, the application of enhanced recovery program (ERP) in colorectal surgery has also been shown to accelerate post-operative recovery effectively and to reduce morbidities by many clinical studies and meta-analysis [8–15]. The concept of ERP advocated strongly on pre-operative optimization of patient information and organ function, means for reduction of surgical stress, adequate anesthesia and pain control, and modification of peri-operative care pathway [16–18]. Practice of ERP is not complicated but revolutionary and it soon becomes a new standard of peri-operative care in patients after major surgery.
The application of ERP in open colectomy has been reported to achieve a hospital stay of 2–5 days with no increase in complication or re-admission rate [8, 11, 19, 20]. This favorable result has generated the interest that ERP could also be an effective measure to optimize the short-term outcomes of laparoscopic colectomy further. ERP is very suitable for laparoscopic surgery as the patients have less wound pain and morbidity; hence, they can be ambulated and discharged early. ERP for laparoscopic colectomy had been reported to successfully reduce post-operative stay to 2–3 days in even high-risk patients [21] and make a 23-h stay be possible in selected patients [22]. However, literature review found only three reports that compared results of laparoscopic colectomy with conventional care and enhanced recovery care [23–25]. The purpose of this study was to evaluate the impact of ERP on outcomes of laparoscopic colectomy in a center which specializes in laparoscopic colorectal surgery.
Patients and methods
This study compared the short-term outcomes of patients who underwent laparoscopic resection for treatment of colonic cancer before and after the application of ERP in a university teaching hospital. Comparison was made between consecutive patients who underwent laparoscopic resection for colon cancer during the two periods. The control group included patients who had operation during January 2005 to November 2006. Within this period, patients in the unit were managed by conventional peri-operative care system. Patient management was directed mainly by order of surgeon in-charge during the ward round. There was no consensus on time to resume diet, management of drains and urinary catheter, measure of rehabilitation, criteria for discharge between surgeons. The ERP group included patients who were operated on from December 2006 to December 2007. From December 2006, an ERP was implemented in our unit for colectomy patients. The ERP for patients in the unit included the following elements:
Case manager
The case manager, who was a nurse specialist, took an active part in the peri-operative management of the patients. Before operation, the case manager interviewed the patients and their relatives to explain pre-operative preparation, expected recovery rate and also helped family members to prepare for the care of patient at home after discharge. The case manager had a telephone hotline to provide explanation and instruction to patients and their family members after discharge.
-
2.
Peri-operative management
The patient was admitted 1 day before the operation for bowel preparation and preoperative management. Nasogastric tube and abdominal drain were not placed during the operation. Abdominal incisions were infiltrated with long acting local anesthetics before closure. Intravenous fluid was given at the discretion of anesthetist during operation but was restricted to 1.5 l/day in early post-operative period and was stopped as soon as the patient’s oral fluid intake became adequate. Unless there was contraindication, the medical and nursing care of patient after operation followed a standard clinical pathway, which aimed for accelerated recovery. Important points of the clinical pathway are summarized in Table 1. The pathway emphasized on (1) education of patient and family in pain and wound management; (2) routine chest physiotherapy and walking exercise; (3) early resumption of nutrition without the need to wait for presence bowel sound or passage of flatus. The criteria for discharge of patient included (1) absence of complication except for mild wound infection (2) full ambulation or availability of care person at home and (3) tolerance of diet.
-
3.
Exclusion criteria
Table 1.
Summary of clinical pathway for enhanced recovery program
| Day 1 | Assess for complication |
| Resume fluid ± solid diet | |
| Remove urinary catheter | |
| Chest physiotherapy | |
| Assisted ambulation | |
| Educate pain management and wound care | |
| Day 2 | Assess for complication |
| Progress to solid diet | |
| Ensure good pain control | |
| Walking exercise | |
| Discuss with patient and family about discharge plan | |
| Day 3 | Assess for complication |
| Plan to discharge | |
| Arrange community nursing service if indicated | |
| Educate patient/family on diet, wound care and pain management at home | |
| Day 4 | Full ambulation |
| Discharge from hospital |
Patients with mid and low rectal cancer, who required low anterior resection or abdominoperineal resection with total mesorectal excision, were excluded because of the need for stoma care. Patients who were not admitted to colorectal surgical ward because of administrative reason, who required synchronous second major procedure during the operation, who were anticipated to require intensive care unit (ICU) or high dependency unit (HDU) admission after the operation were also excluded from care with ERP.
All patients in both groups had colonic or recto-sigmoid junction cancer and underwent laparoscopic colectomy with a standardized medial-to-lateral approach. Detailed description of the operative procedure had been presented in the authors’ previous publication [26]. Patient controlled anesthesia (PCA) was used for both groups of patients. To allow for fair comparison between two groups, the same exclusion criteria in the ERP was applied to the control group, i.e. patients who met the exclusion criteria set for ERP during January 2005 to November 2006 were excluded from the control group. Data of patients’ demographics and pathology, operative details, complications and post-operative outcomes were collected prospectively. We defined high operative risk as patients who had an American Society of Anesthesiologist (ASA) score 3 or higher and advanced cancer stage as patients who had stage 3 or 4 cancer. Prolonged post-operative ileus was defined as absence of bowel movement and inability to tolerate diet for more than 5 days without evidence of intra-abdominal infection. Re-admission was defined as any unplanned admission into any hospital within 30 days after discharge. To ensure accurate report of re-admission rate, a retrospective review was made through an electronic clinical management system, which contained admission records of patients in all public hospitals in Hong Kong.
Statistical analysis was performed with Statistical Package for Social Sciences (SPSS 11.0, SPSS Inc., Chicago, IL, USA). Categorical variables were compared by Chi square test or Fisher’s exact test as appropriate. Patient’s age, operating time and blood loss were presented as mean with standard deviation and were compared by Student’s t test. Hospital stay and time for resumption of gastrointestinal function were presented as median with range and were compared by Mann Whitney U test. A p value <0.05 was regarded as statistically significant. All analyses between groups were based on principle of intention to treat.
Results
Patient demographics and operation details
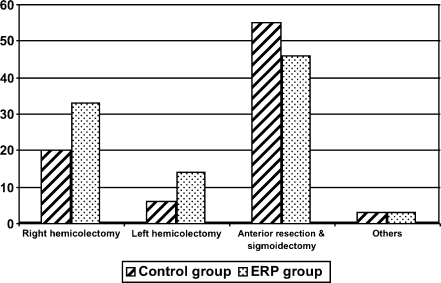
After exclusion, there were 96 patients in the ERP group and 84 patients in the control group. The number of patients excluded in each group and the reasons for exclusion were shown in Table 2. Eight patients in the ERP group and three patients in the control group were admitted to the HDU or ICU admission after the operation. As a result, the eight patients in the ERP group did not have post-operative care with ERP. Under the principle of intention to treat, patients who had unexpected HDU or ICU admissions were still included for analysis and comparison in both groups. The age of patients were similar in both groups (69.6 ± 13 versus 71.4 ± 10 in ERP and control groups respectively; p = 0.30). There were also no statistical difference in all other patient characteristics including gender, co-morbidities, ASA score, stage of cancer, and incidence of previous abdominal surgery (Table 3). The types of procedures performed were similar during the two periods (p = 0.09) and were summarized in Fig. 1. Between the ERP and control groups, there were no difference in operating time (171.1 ± 50 versus 160.5 ±41 min; p = 0.12), operative blood loss [100 (range: 50–150) versus 80 (range: 50–100) ml; p = 0.91] and open conversion rate (6.3% versus 8.3% respectively; p = 0.59).
Table 2.
Exclusion for enhanced recovery program and for comparison in control group
| Number of patients | ||
|---|---|---|
| ERP | Control | |
| Synchronous second major resection | 5 | 2 |
| Anticipated ICU/HDU admission | 8 | 2 |
| Not admitted to colorectal surgery ward | 9 | N.A. |
| Case manager not available | 3 | N.A. |
ERP enhanced recovery program, ICU intensive care unit, HDU high dependency unit, N.A. not applicable
Table 3.
Patient characteristics
| ERP (n = 96) | Control (n = 84) | p value | |
|---|---|---|---|
| Age | 72 (31–94) | 72 (46–92) | 0.30 |
| Sex (male/female) | 51/45 | 50/34 | 0.39 |
| Chronic pulmonary disease | 9 (9.4%) | 7 (8.3%) | 0.81 |
| Chronic heart disease | 17 (17.7%) | 15 (17.6%) | 0.98 |
| Previous stroke | 7 (7.3%) | 4 (4.8%) | 0.546 |
| Diabetes mellitus | 15 (15.6%) | 18 (21.4%) | 0.32 |
| High anesthetic risk | 13 (15.6%) | 16 (19%) | 0.2 |
| Previous abdominal surgery | 21 (21.9%) | 14 (16.7%) | 0.378 |
| Advanced cancer stage | 42 (43.8%) | 41 (48.8%) | 0.50 |
Fig. 1.
Types of laparoscopic colectomy in two groups of patients
Complications
There was no operative mortality in both groups of patients. Intra-operative complications occurred in four patients in the ERP group (two arrhythmia, bowel perforation, pre-sacral vein bleeding) and three patients in the control group (pre-sacral vein bleeding, iliac artery injury, bowel perforation). Post-operative complications occurred in 12.5% and 10.7% of patients in the ERP and control groups respectively (p = 0.71). Cardiopulmonary complications and wound infection accounted for majority of the complications in both groups. There was no difference in the incidence of any type of post-operative complications between the two groups and the details are listed in Table 4.
Table 4.
Post-operative complications
| ERP (n = 96) | Control (n = 84) | p value | |
|---|---|---|---|
| Cardiac | 4 (4.1%) | Nil | 0.12 |
| Pulmonary | 4 (4.1%) | 3 (3.6%) | 1.00 |
| Intra-abdominal collection | 1 (1%) | 1 (1.2%) | 1.00 |
| Anastomotic leakage | Nil | 2 (2.4%) | 0.22 |
| Deep vein thrombosis | 1 (1%) | Nil | 1.0 |
| Wound infection | 2 (2.1%) | 5 (6%) | 0.18 |
Recovery and re-admission
Recovery of gastrointestinal function in patients was assessed by the resumption of diet, passage of flatus and the incidence of prolonged ileus. In the ERP and control groups, the post-operative day of normal diet resumption diet was 1 (range: 1–3) versus 1 (range: 1–6) respectively (p = 0.96) and the post-operative day of passing flatus was 2 (range: 1–4) versus 2 (range: 1–5) respectively (p = 0.03). No patient in the ERP group and five (6%) patients in the control group had prolong ileus after operation (p = 0.02). The median hospital stay after operation, however, had no difference in both groups [4 (2–23) days in ERP group versus 4 (2–34) days in control group; p = 0.4)]. Five patients in the ERP group and six patients in the control group had re-admission and the re-admission rate were similar in both groups (5% and 7% respectively; p = 0.59). Wound infection was the commonest reason for re-admission and the reasons of re-admission were summarized in Table 5.
Table 5.
Reasons for re-admission of patients
| Enhanced recovery program group (n = 5) |
| 1. Abdominal pain |
| 2. Wound infection |
| 3. PR bleeding |
| 4. Abdominal distension |
| 5. Ureteric colic |
| Control group (n = 6) |
| 1. Fever |
| 2. Rectal bleeding |
| 3. Lower limb swelling |
| 4. Wound infection |
| 5. Groin abscess after catheter insertion |
| 6. Wound infection |
Factors affecting hospital stay of patients with laparoscopic colectomy were analyzed. While the median hospital stay for all patients in the study was 4 days, we arbitrarily defined hospital stay of 5 days or more as late discharge, which happened in 74 (40%) patients. Factors significantly associated with late discharge included age (p < 0.01), advanced cancer stage (p = 0.04), operative blood loss (p = 0.04), open conversion (p = 0.01), post-operation HDU/ICU admission (p < 0.01), prolong ileus (p < 0.01) and presence of complication (p < 0.01). Among these factors, multivariate analysis with logistic regression found that age (p < 0.01; 95% confidence interval, 1.03–1.12), advanced cancer stage (p = 0.01; 95% confidence interval, 0.17–0.82) and presence of complication (p = 0.01; 95% confidence interval, 0.05–0.52) were independent factors associated with late discharge.
Discussion
ERP has been proven to improve short-term outcomes after operation. In colorectal surgery, ERP was shown to have the benefits of early recovery of gastrointestinal function, reduced morbidities, reduced hospital stay and did not increase re-admission rate when applied for patients with open colectomy [9–12, 19]. Only a few studies have reported on implementation of ERP in laparoscopic colectomy and the authors believe that investigation into this subject is important. In laparoscopic colectomy, it is unclear that if ERP can hasten patient recovery further or actually add no further benefit to patients who already have prompt recovery. This information would be valuable in defining the role of ERP in current practice of colorectal surgery.
The present study investigated the impact of ERP on laparoscopic colectomy for colonic cancer. We included only cancer patients because they have a special need for nutritional and psychological care during peri-operative period when compared to patient with benign diseases and majority of our elective surgery is for colorectal cancer. An ERP was started in the authors’ center since December 2006 and 80% of patients were suitable for ERP during the study period. The main reason for excluding patients who were anticipated HDU or ICU admission after the operation and patients not admitted to the primary ward of colorectal surgery because of administrative consideration (Table 2). The implementation of ERP was successful with no increase in complication or re-admission rate when compared to the control group.
A remarkable improvement of gastrointestinal function after operation was observed in ERP group. While the post-operative day of tolerating diet was the same in both ERP and control groups, patients in the former group passed flatus significantly earlier [2 (range: 1–4) versus 2 (range: 1–5) respectively; p = 0.03)]. Passage of flatus is unlikely to be altered by any external factor and it should be a more objective parameter to herald resumption of gastrointestinal function when compared with time to toleration of diet after operation. The incidence of prolonged ileus in the FT surgery group was also significantly lower than the control group (0 versus 6% respectively; p = 0.02). Except for implementation of ERP, there was no other difference in peri-operative patient management of two groups of patients. All operations in the study were performed by same operative approach (medial-to-lateral mobilization) and the procedures were done mostly by fellows in colorectal surgery under supervision of the senior author. The operating time, blood loss and complication rate did not show any difference in both groups. Post-operative ileus is common after open abdominal surgery and the benefit of laparoscopic colectomy over open surgery is partly attributed by reduction of the duration of ileus. However, most studies on laparoscopic or ERP for colectomy in the past did not report post-operative ileus and its actual incidence in current practice was unclear. The reduction of prolonged ileus in the ERP group could be a result of enforced rehabilitation by effort of our nursing staff and physiotherapists in such a multi-modal care program. Through motility study using Indium scintigraphy, Basse et al. [27] demonstrated early normalization of gastrointestinal function when comprehensive ERP was applied to patients with colonic resection.
Only three published reports [23–25] had compared outcomes of laparoscopic colectomy with and without ERP and they all reported reduction in hospital stay with the implementation of ERP. Ishiguro et al. [24] reported more patients discharged within 8 days after laparoscopic colectomy by the implementation of clinical pathway, Raue et al. [25] and Al Chalabi et al. [23] reported that ERP resulted in reducing hospital stay from about 8 to 5 days among their patients. In the present study, there was no difference in length of hospital stay between the ERP and control groups (medial hospital stay = 4 days in both groups), despite a better gastrointestinal function in the ERP group. Multivariate analysis found that hospital stay was influenced by patient factors including age, cancer stage and presence of complication in the present study. In the ERP of the present study, patients were targeted to be discharged on days 2–3 after operation and hence, pre-determined a hospital stay of about 4 days despite good recovery. As suggested by Maessen et al. [28] from the Enhanced Recovery After Surgery (ERAS) Group, the length of stay may be related to organization of care and not totally related to period of recovery. In view of the fact that patients managed with ERP in the study had better post-operative bowel function and no increase in complication or re-admission rate for patients, the structure of our ERP can be reviewed to target for earlier patient discharge on days 1– 2 after operation and improve the patient outcomes further. Most of previous studies in laparoscopic colectomy adopted traditional care pathway and reported hospital stay of 5 to 9 days [29], which was longer than what multi-modal rehabilitation program could achieve in open colectomy [30]. Two randomized control trials (RCT) [12, 19] had compared application of ERP in open and laparoscopic colectomy and they showed that the overall short-term outcomes of laparoscopic surgery with ERP were better or equal to open colectomy. However, a systematic review by Vlug et al. [31] in 2008 reported that due to the lack of data, no robust conclusion can be made on comparison of laparoscopic versus open surgery within application of ERP. The present study provided further evidence that the benefit of structured multi-modal rehabilitation program is also suitable for laparoscopic colectomy. Management of patients with enforced post-operative mobilization, pre-set time for resumption of nutrition and discharge according to pre-defined criteria was not associated with increase in patient morbidity, mortality or re-admission rate.
The ERP adopted in the present study is rather simple: it emphasized patient education, avoidance of tubes and drains, early resumption of nutrition and enforced rehabilitation through a structured post-operative care pathway. The design of this multi-disciplinary approach care system had made reference to the previous reports of successful experience in ERP [8, 12, 16, 18, 21] and taken into account of the feasibility of co-operation by the paramedics as well as the patient acceptance in the light of our local culture. The present study did not employ epidural anesthesia which was an important element in many multi-modal rehabilitation programs [11–13, 19]. Apart from better pain control and reduction of ileus, epidural anesthesia was shown to attenuate the endocrine-metabolic response through afferent neural blockade and to accelerate patient recovery through reduction of stress response [16]. Most of the evidence for benefit of epidural anesthesia is, however, from experience in open surgery [30, 32–34]. In the practice of minimally invasive surgery, there is evidence to suggest that epidural anesthesia may not be necessary [30]. Two randomized controlled trials [35, 36] had compared results of PCA versus epidural anesthesia for laparoscopic colectomy. Neudecker et al. [35] reported that epidural anesthesia did not improve post-operative ileus and Senagore et al. [36] reported that epidural anesthesia provided better pain control but no reduction in hospital stay. Hence, most recent studies on use of ERP for laparoscopic colectomy did not routinely use epidural anesthesia [23, 37]. The role of epidural anesthesia for laparoscopic abdominal surgery shall be an important area for further evaluation.
Major limitation of this study is that it compared patients in two different periods and was not a randomized controlled study. The better gastrointestinal function in the ERP group could theoretically be the results of better operative skill among surgeons and improvement in the surgical techniques. However, most of the laparoscopic colectomies in the two groups were done by different fellows in the unit. Moreover, there was no difference in operating time, blood loss or complication rate between the control and the ERP groups to suggest that the quality of operation was better in the ERP group. No result from randomized controlled trial to compare laparoscopic colectomy with and without ERP has been reported so far. The study protocol of a double blinded multi-center randomized controlled study for laparoscopic and open colectomy with or without fast track surgery in the Netherlands was reported [38]. The result of this study will provide stronger evidence on the value of ERP in laparoscopic colectomy.
Conclusions
In laparoscopic colectomy, application of ERP was associated with significant improvement in gastrointestinal function including earlier passage of flatus and reduction of prolonged ileus after operation but no difference in complication rate, hospital stay and re-admission rate. ERP could be an effective strategy to optimize the outcomes of laparoscopic colectomy and further investigation is warranted.
Acknowledgments
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Clinical Outcomes of Surgical Therapy (COST) Study Group A comparison of laparoscopically assisted and open colectomy for colon cancer. N Engl J Med. 2004;350(20):2050–2059. doi: 10.1056/NEJMoa032651. [DOI] [PubMed] [Google Scholar]
- 2.Guillou PJ, Quirke P, Thorpe H, et al. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365(9472):1718–1726. doi: 10.1016/S0140-6736(05)66545-2. [DOI] [PubMed] [Google Scholar]
- 3.Hewett PJ, Allardyce RA, Bagshaw PF, et al. Short-term outcomes of the Australasian randomized clinical study comparing laparoscopic and conventional open surgical treatments for colon cancer: the ALCCaS trial. Ann Surg. 2008;248(5):728–738. doi: 10.1097/SLA.0b013e31818b7595. [DOI] [PubMed] [Google Scholar]
- 4.Jayne DG, Guillou PJ, Thorpe H, et al. Randomized trial of laparoscopic-assisted resection of colorectal carcinoma: 3-year results of the UK MRC CLASICC Trial Group. J Clin Oncol. 2007;25(21):3061–3068. doi: 10.1200/JCO.2006.09.7758. [DOI] [PubMed] [Google Scholar]
- 5.Law WL, Lee YM, Choi HK, Seto CL, Ho JW. Impact of laparoscopic resection for colorectal cancer on operative outcomes and survival. Ann Surg. 2007;245(1):1–7. doi: 10.1097/01.sla.0000218170.41992.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Poon JT, Law WL, Wong IW, et al. Impact of laparoscopic colorectal resection on surgical site infection. Ann Surg. 2009;249(1):77–81. doi: 10.1097/SLA.0b013e31819279e3. [DOI] [PubMed] [Google Scholar]
- 7.Veldkamp R, Kuhry E, Hop WC, et al. Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6(7):477–484. doi: 10.1016/S1470-2045(05)70221-7. [DOI] [PubMed] [Google Scholar]
- 8.Basse L, Hjort JD, Billesbolle P, Werner M, Kehlet H. A clinical pathway to accelerate recovery after colonic resection. Ann Surg. 2000;232(1):51–57. doi: 10.1097/00000658-200007000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bradshaw BG, Liu SS, Thirlby RC. Standardized perioperative care protocols and reduced length of stay after colon surgery. J Am Coll Surg. 1998;186(5):501–506. doi: 10.1016/S1072-7515(98)00078-7. [DOI] [PubMed] [Google Scholar]
- 10.Delaney CP, Fazio VW, Senagore AJ, et al. ‘Fast track’ postoperative management protocol for patients with high co-morbidity undergoing complex abdominal and pelvic colorectal surgery. Br J Surg. 2001;88(11):1533–1538. doi: 10.1046/j.0007-1323.2001.01905.x. [DOI] [PubMed] [Google Scholar]
- 11.Khoo CK, Vickery CJ, Forsyth N, Vinall NS, Eyre-Brook IA. A prospective randomized controlled trial of multimodal perioperative management protocol in patients undergoing elective colorectal resection for cancer. Ann Surg. 2007;245(6):867–872. doi: 10.1097/01.sla.0000259219.08209.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.King PM, Blazeby JM, Ewings P, et al. Randomized clinical trial comparing laparoscopic and open surgery for colorectal cancer within an enhanced recovery programme. Br J Surg. 2006;93(3):300–308. doi: 10.1002/bjs.5216. [DOI] [PubMed] [Google Scholar]
- 13.Nygren J, Soop M, Thorell A, Hausel J, Ljungqvist O. An enhanced-recovery protocol improves outcome after colorectal resection already during the first year: a single-center experience in 168 consecutive patients. Dis Colon Rectum. 2009;52(5):978–985. doi: 10.1007/DCR.0b013e31819f1416. [DOI] [PubMed] [Google Scholar]
- 14.Walter CJ, Collin J, Dumville JC, Drew PJ, Monson JR. Enhanced recovery in colorectal resections: a systematic review and meta-analysis. Colorectal Dis. 2009;11(4):344–353. doi: 10.1111/j.1463-1318.2009.01789.x. [DOI] [PubMed] [Google Scholar]
- 15.Wind J, Polle SW, Fung Kon Jin PH, et al. Systematic review of enhanced recovery programmes in colonic surgery. Br J Surg. 2006;93(7):800–809. doi: 10.1002/bjs.5384. [DOI] [PubMed] [Google Scholar]
- 16.Kehlet H, Wilmore DW. Multimodal strategies to improve surgical outcome. Am J Surg. 2002;183(6):630–641. doi: 10.1016/S0002-9610(02)00866-8. [DOI] [PubMed] [Google Scholar]
- 17.Kehlet H, Wilmore DW. Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. 2008;248(2):189–198. doi: 10.1097/SLA.0b013e31817f2c1a. [DOI] [PubMed] [Google Scholar]
- 18.Wilmore DW, Kehlet H. Management of patients in fast track surgery. BMJ. 2001;322(7284):473–476. doi: 10.1136/bmj.322.7284.473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Basse L, Jakobsen DH, Bardram L, et al. Functional recovery after open versus laparoscopic colonic resection: a randomized, blinded study. Ann Surg. 2005;241(3):416–423. doi: 10.1097/01.sla.0000154149.85506.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kehlet H, Mogensen T. Hospital stay of 2 days after open sigmoidectomy with a multimodal rehabilitation programme. Br J Surg. 1999;86(2):227–230. doi: 10.1046/j.1365-2168.1999.01023.x. [DOI] [PubMed] [Google Scholar]
- 21.Bardram L, Funch-Jensen P, Jensen P, Crawford ME, Kehlet H. Recovery after laparoscopic colonic surgery with epidural analgesia, and early oral nutrition and mobilisation. Lancet. 1995;345(8952):763–764. doi: 10.1016/S0140-6736(95)90643-6. [DOI] [PubMed] [Google Scholar]
- 22.Levy BF, Scott MJ, Fawcett WJ, Rockall TA. 23-hour-stay laparoscopic colectomy. Dis Colon Rectum. 2009;52(7):1239–1243. doi: 10.1007/DCR.0b013e3181a0b32d. [DOI] [PubMed] [Google Scholar]
- 23.Al Chalabi CH, Kavanagh DO, Hassan L et al (2010) The benefit of an enhanced recovery programme following elective laparoscopic sigmoid colectomy. Int J Colorectal Dis [DOI] [PubMed]
- 24.Ishiguro S, Yamamoto S, Fujita S, et al. Effect of a clinical pathway after laparoscopic surgery for colorectal cancer. Hepatogastroenterology. 2008;55(85):1315–1319. [PubMed] [Google Scholar]
- 25.Raue W, Haase O, Junghans T, et al. ‘Fast-track’ multimodal rehabilitation program improves outcome after laparoscopic sigmoidectomy: a controlled prospective evaluation. Surg Endosc. 2004;18(10):1463–1468. doi: 10.1007/s00464-003-9238-y. [DOI] [PubMed] [Google Scholar]
- 26.Poon JT, Law WL, Fan JK, Lo OS. Impact of the standardized medial-to-lateral approach on outcome of laparoscopic colorectal resection. World J Surg. 2009;33(10):2177–2182. doi: 10.1007/s00268-009-0173-5. [DOI] [PubMed] [Google Scholar]
- 27.Basse L, Madsen JL, Kehlet H. Normal gastrointestinal transit after colonic resection using epidural analgesia, enforced oral nutrition and laxative. Br J Surg. 2001;88(11):1498–1500. doi: 10.1046/j.0007-1323.2001.01916.x. [DOI] [PubMed] [Google Scholar]
- 28.Maessen JM, Dejong CH, Kessels AG, von Meyenfeldt MF. Length of stay: an inappropriate readout of the success of enhanced recovery programs. World J Surg. 2008;32(6):971–975. doi: 10.1007/s00268-007-9404-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Abraham NS, Young JM, Solomon MJ. Meta-analysis of short-term outcomes after laparoscopic resection for colorectal cancer. Br J Surg. 2004;91(9):1111–1124. doi: 10.1002/bjs.4640. [DOI] [PubMed] [Google Scholar]
- 30.Kehlet H, Kennedy RH. Laparoscopic colonic surgery—mission accomplished or work in progress? Colorectal Dis. 2006;8(6):514–517. doi: 10.1111/j.1463-1318.2006.00955.x. [DOI] [PubMed] [Google Scholar]
- 31.Vlug MS, Wind J, Van der Zaag E, et al. Systematic review of laparoscopic vs open colonic surgery within an enhanced recovery programme. Colorectal Dis. 2009;11(4):335–343. doi: 10.1111/j.1463-1318.2008.01679.x. [DOI] [PubMed] [Google Scholar]
- 32.Fotiadis RJ, Badvie S, Weston MD, len-Mersh TG. Epidural analgesia in gastrointestinal surgery. Br J Surg. 2004;91(7):828–841. doi: 10.1002/bjs.4607. [DOI] [PubMed] [Google Scholar]
- 33.Grass JA. The role of epidural anesthesia and analgesia in postoperative outcome. Anesthesiol Clin North Am. 2000;18(2):407–428. doi: 10.1016/S0889-8537(05)70170-X. [DOI] [PubMed] [Google Scholar]
- 34.Moraca RJ, Sheldon DG, Thirlby RC. The role of epidural anesthesia and analgesia in surgical practice. Ann Surg. 2003;238(5):663–673. doi: 10.1097/01.sla.0000094300.36689.ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Neudecker J, Schwenk W, Junghans T, et al. Randomized controlled trial to examine the influence of thoracic epidural analgesia on postoperative ileus after laparoscopic sigmoid resection. Br J Surg. 1999;86(10):1292–1295. doi: 10.1046/j.1365-2168.1999.01242.x. [DOI] [PubMed] [Google Scholar]
- 36.Senagore AJ, Delaney CP, Mekhail N, Dugan A, Fazio VW. Randomized clinical trial comparing epidural anaesthesia and patient-controlled analgesia after laparoscopic segmental colectomy. Br J Surg. 2003;90(10):1195–1199. doi: 10.1002/bjs.4223. [DOI] [PubMed] [Google Scholar]
- 37.Patel GN, Rammos CK, Patel JV, Estes NC. Further reduction of hospital stay for laparoscopic colon resection by modifications of the fast-track care plan. Am J Surg. 2010;199(3):391–394. doi: 10.1016/j.amjsurg.2009.09.009. [DOI] [PubMed] [Google Scholar]
- 38.Wind J, Hofland J, Preckel B, et al. Perioperative strategy in colonic surgery; LAparoscopy and/or FAst track multimodal management versus standard care (LAFA trial) BMC Surg. 2006;6:16. doi: 10.1186/1471-2482-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]