Abstract
Several works have separated the pressure waveform p in systemic arteries into reservoir p r and excess p exc components, p = p r + p exc, to improve pulse wave analysis, using windkessel models to calculate the reservoir pressure. However, the mechanics underlying this separation and the physical meaning of p r and p exc have not yet been established. They are studied here using the time-domain, inviscid and linear one-dimensional (1-D) equations of blood flow in elastic vessels. Solution of these equations in a distributed model of the 55 larger human arteries shows that p r calculated using a two-element windkessel model is space-independent and well approximated by the compliance-weighted space-average pressure of the arterial network. When arterial junctions are well-matched for the propagation of forward-travelling waves, p r calculated using a three-element windkessel model is space-dependent in systole and early diastole and is made of all the reflected waves originated at the terminal (peripheral) reflection sites, whereas p exc is the sum of the rest of the waves, which are obtained by propagating the left ventricular flow ejection without any peripheral reflection. In addition, new definitions of the reservoir and excess pressures from simultaneous pressure and flow measurements at an arbitrary location are proposed here. They provide valuable information for pulse wave analysis and overcome the limitations of the current two- and three-element windkessel models to calculate p r.
Keywords: Arterial haemodynamics, Pulse wave propagation, Pulse wave analysis, Reservoir-excess separation, Windkessel pressure, One-dimensional distributed model, Time-domain formulation, Conduit arteries, Well-matched bifurcations
Introduction
Several works (Wang et al. 2003; Davies et al. 2007, 2010; Aguado-Sierra et al. 2008; Tyberg et al. 2008, 2009; Parker 2009; Vermeersch et al. 2009) have suggested that the time-domain analysis of pulse wave propagation in systemic arteries is improved if the pressure waveform is separated into a reservoir pressure that varies in time, but is uniform (space-independent) throughout the arteries, and an excess pressure 1 that varies in time and space due to wave propagation; the so-called reservoir-excess separation. These works have shown that the pressure waveform in systole and early diastole is made up of the combination of reservoir and excess pressures, whereas the pressure decay in late diastole is well described by the reservoir pressure only. Davies et al. (2010) have recently shown that the reservoir pressure increases with aging and correlates well with factors that determine health risk.
Despite all these studies, the physical bases of the reservoir and excess pressures have not yet been established and the reservoir-excess separation has remained an ad hoc assumption. Moreover, two different algorithms have been proposed and used to calculate the reservoir pressure (Wang et al. 2003; Aguado-Sierra et al. 2008), but their assumptions and results have not been rigorously compared.
Other separations of the pulse waveform with better understood mechanics have been suggested. Simultaneous pressure and velocity measurements at an arbitrary arterial location and an estimation of the local pulse wave speed allow us to calculate the forward-travelling waveform propagated from proximal locations and the backward-travelling waveform propagated from distal locations (Westerhof et al. 1972; Parker and Jones 1990; Hughes and Parker 2009; Zhang and Li 2009). The pulse waveform simulated at an arbitrary location using the one-dimensional (1-D) formulation can also be separated into a peripheral waveform made of waves initially reflected at peripheral branches and a conduit waveform made of the remaining reflected and transmitted waves at the arterial junctions, aortic valve (when shut) and any other change in geometry and elasticity within the arterial segments (Alastruey et al. 2009). This separation showed that most of the pressure waveform consists of peripheral reflections, especially in diastole when the conduit pressure vanishes. The rest of reflected waves mainly contribute to the pressure waveform in systole and early diastole.
The purpose of this work is to theoretically and numerically study the mechanics underlying the reservoir-excess separation in systemic arteries, explore their implications for pulse wave analysis when the algorithms described in Wang et al. (2003) and Aguado-Sierra et al. (2008) are used to calculate the reservoir pressure, and find new definitions of the reservoir and excess pressures that provide valuable information for pulse wave analysis and overcome the limitations of the current algorithms. First, the algorithms used in Wang et al. (2003) and Aguado-Sierra et al. (2008) are described and compared, and their limitations are discussed ("Reservoir-Excess Separation"). These algorithms are then related to the 1-D equations of blood flow in elastic vessels ("The 1-D Formulation, From the 1-D Equations to the Windkessel Pressure, 3-Element Windkessel and 1-D Model Pressures, and Diastolic flow"), which are a reasonable approach to model pulse wave propagation in systemic arteries (Olufsen et al. 2000; Čanić and Kim 2003; Steele et al. 2003; Quarteroni and Formaggia 2004; Matthys et al. 2007). The new reservoir and excess pressures are defined in "New Reservoir and Excess Pressures". Pulse waveforms generated using the 1-D formulation in a single-vessel aortic model and a 55-segment arterial model ("Numerical Experiments") will be used to illustrate the results.
Methodology
Reservoir-Excess Separation
The reservoir-excess separation was introduced by Wang et al. (2003) using Frank’s windkessel pressure p w(t) as the reservoir pressure, which satisfies the mass conservation (Frank 1899)
 |
1 |
where t is the time, q
IN(t) the left ventricular flow ejection, C
T the net compliance of the whole arterial tree, R
T the net resistance of the peripheral systemic circulation, and P
out the pressure at which flow to the periphery ceases.  and P
out were assumed to be constant and estimated from in vivo pressure and flow waveforms measured at the ascending aorta, so that Eq. 1 could be solved for p
w,
and P
out were assumed to be constant and estimated from in vivo pressure and flow waveforms measured at the ascending aorta, so that Eq. 1 could be solved for p
w,
 |
2 |
with  the windkessel pressure at
the windkessel pressure at  . The excess pressure was defined as p − p
w, with p the measured pressure, and was found to be similar to
. The excess pressure was defined as p − p
w, with p the measured pressure, and was found to be similar to  in normal conditions (Wang et al. 2003), with Z
Ao the characteristic impedance of the ascending aorta (defined as the pressure-to-flow ratio of a forward-travelling wave (Milnor 1989)).
in normal conditions (Wang et al. 2003), with Z
Ao the characteristic impedance of the ascending aorta (defined as the pressure-to-flow ratio of a forward-travelling wave (Milnor 1989)).
If the flow is periodic with period T, Eq. 1 leads to
 |
3 |
where  is the mean over the time interval
is the mean over the time interval  , with
, with  .
.  is, therefore, the cardiac output.
is, therefore, the cardiac output.
To calculate p w we require q IN, which cannot always be measured in vivo. To overcome this limitation, Aguado-Sierra et al. (2008) proposed to calculate the reservoir pressure as the pressure p r satisfying the three-element windkessel equation
 |
4 |
where p is the measured pressure at an arbitrary location and λ is a resistance relating q
IN and the excess pressure  ; i.e.
; i.e.
 |
5 |
with the feet of the q
IN and p waves aligned in time to eliminate the delay between them. The constants  and
and  were determined using an iterative fitting algorithm, which means that λ, and hence p
r, were not defined explicitly.
were determined using an iterative fitting algorithm, which means that λ, and hence p
r, were not defined explicitly.
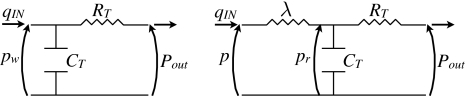
It is important to remark that if λ = Z Ao, then Eq. 4 corresponds to the three-element windkessel model (Westerhof et al. 1969, 1971). Moreover, Eqs. 1 and 4 and their analogous electrical circuits (Fig. 1) show that p w and p r are conceptually different.
Fig. 1.
Analogous electrical circuit diagrams governed by the (left) two-element windkessel Eq. 1 and (right) three-element windkessel Eq. 4
From Eq. 5 we have
 |
6 |
where  and
and  are the mean values of
are the mean values of  and p, respectively.
and p, respectively.
The 1-D Formulation
The nonlinear terms in the 1-D formulation will be neglected since it makes the analysis simpler and it is consistent with Eqs. 1 and 4 being linear. Moreover, the effect of nonlinearities is small for the physiological parameters used (Matthys et al. 2007).
Consider the arterial system to be a network of N elastic and homogeneous arterial segments (or edges) from 1 to N, in which pulse wave propagation is modelled using the linearised 1-D equations (Alastruey et al. 2009)
 |
7 |
where the superscript i indicates the number of the edge, x ∈ [0,l
i] is the axial coordinate along the vessel, l
i the edge length, p
i(x, t) the average internal pressure over the luminal cross section, q
i(x, t) the luminal flow rate,  the cross-sectional area of the lumen, and A
i
0 the area at
the cross-sectional area of the lumen, and A
i
0 the area at  assumed to be uniform within each edge. The constants
assumed to be uniform within each edge. The constants
 |
8 |
are the viscous resistance to flow, blood inertia and elastic wall compliance, respectively, per unit length of vessel, ρ is the constant mass density of blood, and μ the constant blood viscosity. The arterial wall is assumed to be thin, homogeneous, incompressible and elastic, and to deform axisymmetrically, each cross-section independent of the others. The constants h i and E i are the thickness and Young’s modulus of the wall, respectively.
The equations in 7 form a system of hyperbolic partial differential equations. The characteristic variables w i f and w i b of this system are
 |
9 |
where  is the characteristic impedance of the edge and
is the characteristic impedance of the edge and  its pulse wave speed. Changes in pressure and flow within any edge are propagated forward by w
i
f and backward by w
i
b along the characteristic lines
its pulse wave speed. Changes in pressure and flow within any edge are propagated forward by w
i
f and backward by w
i
b along the characteristic lines  , respectively, where
, respectively, where  represent lines in the (x, t) space. If viscous dissipation is neglected (i.e.
represent lines in the (x, t) space. If viscous dissipation is neglected (i.e.  ), w
i
f and
), w
i
f and  , are invariant along the characteristic lines and, hence, propagate changes in pressure and flow without wave dissipation.
, are invariant along the characteristic lines and, hence, propagate changes in pressure and flow without wave dissipation.
For convenience, the edges are indexed so that  refers to the ascending aorta and
refers to the ascending aorta and  to M (
to M ( ) refer to terminal edges. The inlet flow, q
1(0,t), is assumed to be given and equal to the flow waveform from the left ventricle q
IN. The distal ends of edges numbered from 2 to M are coupled to a matched RCR windkessel model relating
) refer to terminal edges. The inlet flow, q
1(0,t), is assumed to be given and equal to the flow waveform from the left ventricle q
IN. The distal ends of edges numbered from 2 to M are coupled to a matched RCR windkessel model relating  to
to  , through (Alastruey et al. 2008)
, through (Alastruey et al. 2008)
 |
10 |
where R j and C j are the constant peripheral resistance and compliance, respectively.
At the junctions (or nodes) of the network, conservation of mass and continuity of pressure are enforced. For each of the three edges  and c connected at a junction, the reflection coefficients
and c connected at a junction, the reflection coefficients  (
( ) are defined as the ratio of the change of pressure across the reflected wave to the change of pressure in the incident wave. They can be expressed as a function of the characteristic admittance of the edge
) are defined as the ratio of the change of pressure across the reflected wave to the change of pressure in the incident wave. They can be expressed as a function of the characteristic admittance of the edge  (Alastruey et al. 2009),
(Alastruey et al. 2009),
 |
11 |
Forward- and backward-travelling waveforms
We can calculate the forward ( ) and backward (
) and backward ( ) contributions to p and q at an arbitrary location in the network as
) contributions to p and q at an arbitrary location in the network as  and
and  (Parker and Jones 1990). They satisfy
(Parker and Jones 1990). They satisfy  and
and  . The former yields
. The former yields  when
when  in Eq. 9 (i.e. backward-travelling waves are absent) and the latter
in Eq. 9 (i.e. backward-travelling waves are absent) and the latter  when
when  (i.e. forward-travelling waves are absent) (
(i.e. forward-travelling waves are absent) ( ).
).
Conduit and Peripheral Pressures
In a linear 1-D model simulation, the conduit contribution to pressure p
con is obtained at any location in the network by enforcing terminal boundary conditions that completely absorb any incident wave; i.e. single resistances with  . The peripheral contribution to pressure p
per is then calculated for the linear case as
. The peripheral contribution to pressure p
per is then calculated for the linear case as  (Alastruey et al. 2009).
(Alastruey et al. 2009).
From the 1-D Equations to the Windkessel Pressure
Integrating the first two equations in (7) over the edge length l i yields
 |
12 |
where  , and
, and  and
and  are the space-averaged pressure and flow over an edge of length l
i. Assuming conservation of mass at the nodes of the network and combining the N equations of conservation of mass in 12 yield the following equation for the conservation of mass for the network,
are the space-averaged pressure and flow over an edge of length l
i. Assuming conservation of mass at the nodes of the network and combining the N equations of conservation of mass in 12 yield the following equation for the conservation of mass for the network,
 |
13 |
 |
14 |
where p
C(t) is the compliance-weighted space-average pressure of the network, C
c the total conduit compliance and  the total peripheral outflow driven by p
C.
the total peripheral outflow driven by p
C.
Hereafter,  , will be assumed since the resistance in large arteries is much smaller than peripheral resistances (Caro et al. 1978) [Chap. 12]. Taking
, will be assumed since the resistance in large arteries is much smaller than peripheral resistances (Caro et al. 1978) [Chap. 12]. Taking  , leads to
, leads to  , (i.e. changes in pressure and flow occur synchronously) and reduces the N equations of balance of momentum in (12) to
, (i.e. changes in pressure and flow occur synchronously) and reduces the N equations of balance of momentum in (12) to
 |
15 |
Furthermore,  , at any location of the i-th arterial segment, since 15 holds for any length l
i.
, at any location of the i-th arterial segment, since 15 holds for any length l
i.
Assuming continuity of pressure at the nodes of the network, we obtain  , where
, where  is the space-independent pressure to which the 1-D model pressures in 7 reduce when R
i
0D = 0 and
is the space-independent pressure to which the 1-D model pressures in 7 reduce when R
i
0D = 0 and  . Equation 13 then becomes
. Equation 13 then becomes
 |
16 |
 |
where  is the total outflow to the periphery driven by
is the total outflow to the periphery driven by  and C
p is the total peripheral compliance. The solution to Eq. 16 is
and C
p is the total peripheral compliance. The solution to Eq. 16 is
 |
17 |
where  is the pressure
is the pressure  at t = T
0 and
at t = T
0 and  is the total compliance. Finally, Eq. 16 reduces to Frank’s windkessel Eq. 1, with
is the total compliance. Finally, Eq. 16 reduces to Frank’s windkessel Eq. 1, with  , when
, when  ; i.e. we only have conduit compliance C
c.
; i.e. we only have conduit compliance C
c.
Next, the implications of time-averaging Eqs. 13, 14 and 16 will be explored.
Time-averaged behaviour. Integrating Eq. 13 over the interval  yields
yields
 |
18 |
If the flow is periodic with a period T, then Eqs. 10 and 18 lead to
 |
19 |
Integrating the balance of momentum in 12 over the interval  and assuming periodic flow with a period T yields
and assuming periodic flow with a period T yields  . Since Eq. 12 holds for any length l
i, we have
. Since Eq. 12 holds for any length l
i, we have  being evaluated at any location of the i-th arterial segment. Combining these results with continuity of pressure at the nodes of the network leads to
being evaluated at any location of the i-th arterial segment. Combining these results with continuity of pressure at the nodes of the network leads to  and i = 1, …, N. Equation 19, hence, reduces to
and i = 1, …, N. Equation 19, hence, reduces to
 |
20 |
i.e. the mean pressure at any location in the network is space-independent.
Combining Eqs. 14 and 20 yields
 |
21 |
and integrating Eq. 16 over the interval  yields
yields
 |
22 |
Thus,  .
.
3-Element Windkessel and 1-D Model Pressures
The calculation of the reservoir pressure using Eq. 4 is based on the assumptions of well-matched arterial junctions for the transmission of forward-travelling waves (i.e.  at the outlets of internal edges) and q
IN being proportional to p
exc except for a time shift to account for the propagation of q
IN to the measurement site of p (Aguado-Sierra et al. 2008). The latter is satisfied if the outlets of terminal edges are completely absorbent (i.e. they are single resistances with
at the outlets of internal edges) and q
IN being proportional to p
exc except for a time shift to account for the propagation of q
IN to the measurement site of p (Aguado-Sierra et al. 2008). The latter is satisfied if the outlets of terminal edges are completely absorbent (i.e. they are single resistances with  ), so that reflected waves are absent in the system (i.e.
), so that reflected waves are absent in the system (i.e.  ). Under these assumptions, the pressure
). Under these assumptions, the pressure  at the aortic root will maintain its shape throughout the network, leading to
at the aortic root will maintain its shape throughout the network, leading to  with q
IN and q
i time-aligned (so that the feet of both waves coincide), and
with q
IN and q
i time-aligned (so that the feet of both waves coincide), and  , if λ = Z
Ao (Eq. 5).
, if λ = Z
Ao (Eq. 5).
If p
i
exc is calculated using Eq. 5 with λ = Z
Ao in a network with reflective terminal boundary conditions (but still well-matched junctions for forward-travelling waves), then  and
and  (i = 1, …, N); i.e. p
i
exc is the part of p
i due to waves travelling from the aortic root to the periphery and p
ir is the part of p
i made of all the reflected waves originated at the terminal (peripheral) reflection sites.
(i = 1, …, N); i.e. p
i
exc is the part of p
i due to waves travelling from the aortic root to the periphery and p
ir is the part of p
i made of all the reflected waves originated at the terminal (peripheral) reflection sites.
Diastolic Flow
In normal diastolic conditions q IN = 0, so that Eqs. 13 and 16 reduce to
 |
23 |
Alastruey et al. (2009) showed that  , converge to
, converge to  (Eq. 17) in diastole. According to the analysis in "From the 1-D Equations to the Windkessel Pressure", this implies that
(Eq. 17) in diastole. According to the analysis in "From the 1-D Equations to the Windkessel Pressure", this implies that  in diastole and, hence,
in diastole and, hence,  ; i.e. changes in pressure and flow occur synchronously. The convergence of
; i.e. changes in pressure and flow occur synchronously. The convergence of  , to
, to  leads to
leads to  and, hence,
and, hence,  , according to Eq. 23.
, according to Eq. 23.
This equation also shows that the contribution of each edge to the total diastolic outflow q
C increases with the edge compliance C
i
0D. Moreover, the conservation of mass in Eq. 7 with  , shows that the flow in each edge is linearly dependent on x,
, shows that the flow in each edge is linearly dependent on x,
 |
24 |
According to Eq. 17,  decays exponentially when
decays exponentially when  . In this case,
. In this case,
 |
25 |
where  is the windkessel pressure at the beginning of diastole, t = T
d.
is the windkessel pressure at the beginning of diastole, t = T
d.
New Reservoir and Excess Pressures
This work will explore the implications of defining the reservoir and excess pressures from simultaneous p and q measurements at an arbitrary location as
 |
26 |
A tilde is used to distinguish these new reservoir and excess pressures from the corresponding pressures calculated using the three-element windkessel model (p
r and p
exc). Note that  at the aortic root if λ = Z
Ao. Using
at the aortic root if λ = Z
Ao. Using  and
and  , and the relations
, and the relations  and
and  shown in "Forward- and Backward-Travelling Waveforms",
shown in "Forward- and Backward-Travelling Waveforms",  and
and  satisfy
satisfy
 |
27 |
at any location in the arterial network. Thus,  is made of waves coming from distal locations only and
is made of waves coming from distal locations only and  is the difference between proximal and distal contributions to p. In a well-matched network for forward-travelling waves with the outlets of terminal edges completely absorbent, p
b = 0 and, hence, p = p
f. Therefore,
is the difference between proximal and distal contributions to p. In a well-matched network for forward-travelling waves with the outlets of terminal edges completely absorbent, p
b = 0 and, hence, p = p
f. Therefore,  and
and  .
.
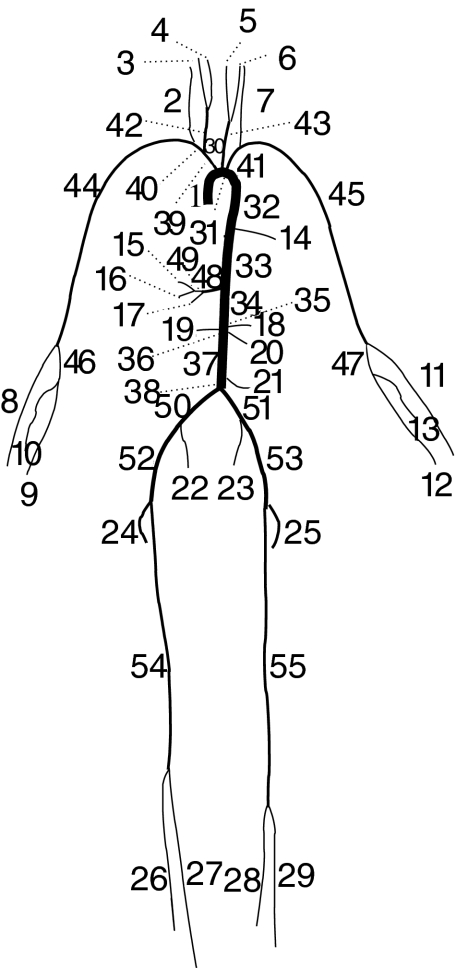
Numerical Experiments
The theoretical results described above will be illustrated using waveforms simulated in a single-vessel 1-D model of the human aorta coupled to a matched RCR windkessel model of the rest of the circulation (Alastruey et al. 2008). Two distributed models will also be used: a 55-artery 1-D model of the larger systemic arteries in the human, referred to as ‘normal 55-artery model’ (Fig. 2), and a version of this model with modified radii so that junctions are well-matched ( ) for forward-travelling waves, referred to as ‘well-matched 55-artery model’. Tables 1, 2 and 3 show the parameters of these models, which have the same total resistance R
T and compliance C
T, and outflow pressure P
out = 0. Figure 4b shows the flow rate q
IN prescribed at the aortic root of the three models; it is periodic until
) for forward-travelling waves, referred to as ‘well-matched 55-artery model’. Tables 1, 2 and 3 show the parameters of these models, which have the same total resistance R
T and compliance C
T, and outflow pressure P
out = 0. Figure 4b shows the flow rate q
IN prescribed at the aortic root of the three models; it is periodic until  s and zero afterward to study the relaxation of these models.
s and zero afterward to study the relaxation of these models.
Fig. 2.
Connectivity of the 55 larger systemic arteries in the human, as proposed in Stergiopulos et al. (1992). Their names and properties are shown in Tables 2 and 3
Table 1.
Parameters of the single-vessel model of the human aorta based on Caro et al. (1978) and Westerhof et al. (1969)
| Parameter | Value |
|---|---|
| Length l | 0.4 m |
| Cross-sectional area A 0 |

|
| Wall thickness h | 1.0 mm |
| Blood mass density ρ |

|
| Elastic Young’s modulus E | 0.4 MPa |
| Peripheral compliance C |

|
| Peripheral resistance R T |
|
The resulting pulse wave speed is 
Table 2.
Length, initial radius and wave speed of each arterial edge in the 55-artery network in Fig. 2
| Arterial edge | Length (cm) | Radius (mm) |
c ( ) ) |
 inlet inlet |
 outlet outlet |
|---|---|---|---|---|---|
| 1. Ascending aorta | 4.0 | 14.5 (14.7) | 4.0 (6.2) | – | 0.1 |
| 2. R. vertebral | 14.8 | 1.9 (2.4) | 8.3 (11.3) | −0.9 | – |
| 3. R. external carotid | 17.7 | 1.3 (3.8) | 9.6 (8.7) | −0.9 | – |
| 4. R. internal carotid | 17.7 | 1.3 (3.8) | 9.9 (9.0) | −0.9 | – |
| 5. L. internal carotid | 17.7 | 1.3 (3.4) | 9.9 (9.6) | −0.9 | – |
| 6. L. external carotid | 17.7 | 1.3 (3.4) | 9.6 (9.2) | −0.9 | – |
| 7. L. vertebral | 14.8 | 1.9 (2.0) | 8.3 (12.5) | −0.9 | – |
| 8. R. radial | 23.5 | 1.6 (3.7) | 8.8 (9.0) | −0.8 | – |
| 9. R. ulnar II | 17.1 | 1.9 (4.3) | 8.2 (8.5) | −0.2 | – |
| 10. R. interosseous | 7.9 | 0.9 (1.9) | 13.2 (14.1) | −0.9 | – |
| 11. L. radial | 23.5 | 1.6 (3.2) | 8.8 (9.5) | −0.8 | – |
| 12. L. ulnar II | 17.1 | 1.9 (3.8) | 8.2 (9.1) | −0.2 | – |
| 13. L. interosseous | 7.9 | 0.9 (1.7) | 13.2 (14.9) | −0.9 | – |
| 14. Intercostals | 8.0 | 1.8 (3.1) | 6.3 (7.3) | −1.0 | – |
| 15. Gastric | 7.1 | 1.8 (2.2) | 6.0 (8.3) | −0.6 | – |
| 16. Splenic | 6.3 | 2.8 (3.4) | 5.3 (7.3) | 0.1 | – |
| 17. Hepatic | 6.6 | 2.2 (4.6) | 5.6 (6.1) | −0.6 | – |
| 18. Superior mesenteric | 5.9 | 4.4 (4.1) | 4.8 (7.6) | −0.6 | – |
| 19. R. renal | 3.2 | 2.6 (3.5) | 5.4 (7.2) | −0.8 | – |
| 20. L. renal | 3.2 | 2.6 (3.5) | 5.4 (7.2) | −0.9 | – |
| 21. Inferior mesenteric | 5.0 | 1.6 (2.5) | 6.2 (7.6) | −0.9 | – |
| 22. R. internal iliac | 5.0 | 2.0 (4.1) | 10.7 (11.6) | −0.8 | – |
| 23. L. internal iliac | 5.0 | 2.0 (4.1) | 10.7 (11.6) | −0.8 | – |
| 24. R. deep femoral | 12.6 | 2.2 (3.6) | 7.8 (9.5) | −0.5 | – |
| 25. L. deep femoral | 12.6 | 2.2 (3.6) | 7.8 (9.5) | −0.5 | – |
| 26. R. anterior tibial | 34.3 | 1.3 (2.0) | 13.1 (16.4) | −0.8 | – |
| 27. R. posterior tibial | 32.1 | 1.9 (3.8) | 11.5 (12.8) | −0.4 | – |
| 28. L. posterior tibial | 32.1 | 1.9 (3.8) | 11.5 (12.8) | −0.4 | – |
| 29. L. anterior tibial | 34.3 | 1.3 (2.0) | 13.1 (16.5) | −0.8 | – |
| 30. Aortic arch I | 2.0 | 11.2 (12.6) | 4.0 (5.8) | −0.3 | 0.0 |
| 31. Aortic arch II | 3.9 | 10.7 (11.9) | 3.9 (5.7) | −0.1 | 0.0 |
| 32. Thoracic aorta I | 5.2 | 10.0 (11.2) | 4.0 (5.8) | −0.1 | 0.4 |
| 33. Thoracic aorta II | 10.4 | 6.6 (10.7) | 4.6 (5.7) | −0.5 | −0.1 |
| 34. Abdominal aorta I | 5.3 | 6.1 (9.2) | 4.6 (5.8) | −0.2 | −0.2 |
| 35. Abdominal aorta II | 1.0 | 6.0 (8.4) | 4.4 (5.7) | −0.2 | −0.1 |
| 36. Abdominal aorta III | 1.0 | 5.9 (7.9) | 4.4 (5.9) | −0.1 | 0.0 |
| 37. Abdominal aorta IV | 10.6 | 5.6 (7.3) | 4.4 (5.9) | −0.1 | 0.0 |
| 38. Abdominal aorta V | 1.0 | 5.2 (6.8) | 4.2 (5.7) | −0.1 | 0.1 |
| 39. Brachiocephalic | 3.4 | 6.2 (7.0) | 4.3 (6.3) | −0.8 | 0.2 |
| 40. R. subclavian | 3.4 | 4.2 (5.4) | 4.8 (6.5) | −0.5 | 0.2 |
| 41. L. subclavian | 3.4 | 4.2 (4.7) | 4.8 (7.0) | −0.9 | 0.2 |
| 42. R. common carotid | 17.7 | 3.7 (4.7) | 4.9 (6.8) | −0.6 | 0.8 |
| 43. L. common carotid | 20.8 | 3.7 (4.2) | 4.9 (7.2) | −0.9 | 0.8 |
| 44. R. brachial | 42.2 | 3.2 (5.2) | 5.5 (6.7) | −0.4 | 0.4 |
| 45. L. brachial | 42.2 | 3.2 (4.6) | 5.5 (7.1) | −0.4 | 0.4 |
| 46. R. ulnar I | 6.7 | 2.2 (4.5) | 7.8 (8.3) | −0.6 | 0.1 |
| 47. L. ulnar I | 6.7 | 2.2 (4.0) | 7.8 (8.9) | −0.6 | 0.1 |
| 48. Celiac I | 1.0 | 3.9 (5.9) | 4.8 (6.1) | −0.7 | 0.4 |
| 49. Celiac II | 1.0 | 2.0 (4.0) | 6.8 (7.4) | −0.7 | −0.5 |
| 50. R. common iliac | 5.8 | 3.6 (5.1) | 4.9 (6.3) | −0.5 | 0.2 |
| 51. L. common iliac | 5.8 | 3.6 (5.1) | 4.9 (6.3) | −0.5 | 0.2 |
| 52. R. external iliac | 14.4 | 3.0 (4.8) | 7.2 (8.7) | −0.4 | 0.0 |
| 53. L. external iliac | 14.4 | 3.0 (4.8) | 7.2 (8.7) | −0.4 | 0.0 |
| 54. R. femoral | 44.3 | 2.2 (3.6) | 8.0 (9.7) | −0.5 | 0.2 |
| 55. L. femoral | 44.3 | 2.2 (3.6) | 8.0 (9.7) | −0.5 | 0.2 |
They are based on data in Stergiopulos et al. (1992). The last two columns show the reflection coefficients at the inlet and outlet of edges connected to junctions. The radii and wave speeds in brackets yield well-matched junctions for forward-travelling waves (with  at the outlets of internal edges)
at the outlets of internal edges)
Table 3.
Peripheral resistances and compliances at the terminal edges of the 55-artery network in Fig. 2
| Arterial edge |
 ( ( ) ) |
C
j ( ) ) |
|---|---|---|
| 2. R. vertebral | 0.60 | 0.93 (0.84) |
| 3. R. external carotid | 1.39 | 0.40 (0.36) |
| 4. R. internal carotid | 1.39 | 0.40 (0.36) |
| 5. L. internal carotid | 1.39 | 0.40 (0.36) |
| 6. L. external carotid | 1.39 | 0.40 (0.36) |
| 7. L. vertebral | 0.60 | 0.93 (0.84) |
| 8. R. radial | 0.53 | 1.06 (0.96) |
| 9. R. ulnar II | 0.53 | 1.06 (0.96) |
| 10. R. interosseous | 8.43 | 0.07 (0.06) |
| 11. L. radial | 0.53 | 1.06 (0.96) |
| 12. L. ulnar II | 0.53 | 1.06 (0.96) |
| 13. L. interosseous | 8.43 | 0.07 (0.06) |
| 14. Intercostals | 0.14 | 4.02 (3.64) |
| 15. Gastric | 0.54 | 1.03 (0.93) |
| 16. Splenic | 0.23 | 2.41 (2.18) |
| 17. Hepatic | 0.36 | 1.54 (1.39) |
| 18. Superior mesenteric | 0.09 | 6.00 (5.43) |
| 19. R. renal | 0.11 | 4.94 (4.47) |
| 20. L. renal | 0.11 | 4.94 (4.47) |
| 21. Inferior mesenteric | 0.69 | 0.81 (0.73) |
| 22. R. internal iliac | 0.79 | 0.70 (0.64) |
| 23. L. internal iliac | 0.79 | 0.70 (0.64) |
| 24. R. deep femoral | 0.48 | 1.17 (1.06) |
| 25. L. deep femoral | 0.48 | 1.17 (1.06) |
| 26. R. anterior tibial | 0.56 | 1.00 (0.90) |
| 27. R. posterior tibial | 0.48 | 1.17 (1.06) |
| 28. L. posterior tibial | 0.48 | 1.17 (1.06) |
| 29. L. anterior tibial | 0.56 | 1.00 (0.90) |
They yield  and
and  . In all these edges
. In all these edges  . The compliances in brackets correspond to the network with well-matched junctions for forward-travelling waves
. The compliances in brackets correspond to the network with well-matched junctions for forward-travelling waves
Fig. 4.
a New excess pressure  with time at
with time at  (inlet), l/4 (1/4), l/2 (mid) and 3l/4 (3/4) in the single-vessel aortic model. b Flow with time at the inlet (q
IN) and midpoint (mid), and outflows
(inlet), l/4 (1/4), l/2 (mid) and 3l/4 (3/4) in the single-vessel aortic model. b Flow with time at the inlet (q
IN) and midpoint (mid), and outflows  and q
C driven by
and q
C driven by  and p
C, respectively
and p
C, respectively
The equations in 7 were solved in each model using a discontinuous Galerkin scheme with a spectral/hp spatial discretisation, a second-order Adams-Bashforth time-integration scheme, a time step of  s, and zero pressures and flows as initial conditions (Alastruey 2006). Arterial edges were divided in non-overlaping elements with a 2 cm length (when physically possible) and a polynomial and quadrature order of 3. Elements or edges shorter than 2 cm were given a polynomial and quadrature order of 2.
s, and zero pressures and flows as initial conditions (Alastruey 2006). Arterial edges were divided in non-overlaping elements with a 2 cm length (when physically possible) and a polynomial and quadrature order of 3. Elements or edges shorter than 2 cm were given a polynomial and quadrature order of 2.
Results
Single-Vessel Aorta
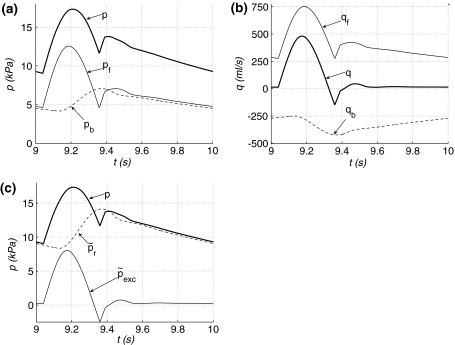
Blood pressure p at any location in the single-vessel aortic model and the reservoir p
r, compliance-weighted space-average p
C and windkessel  pressures, calculated using Eqs. 5 (with λ = Z
Ao), 14 and 17 (with
pressures, calculated using Eqs. 5 (with λ = Z
Ao), 14 and 17 (with  and
and  to satisfy the initial conditions of the 1-D model), respectively, tend to the same shape with the increasing time in diastole. Figure 3a,b show these pressures (p and p
r in the midpoint) once the flow has become periodic. Figure 3a also shows the excess pressure p
exc in the midpoint, which is proportional to q
IN. The difference between
to satisfy the initial conditions of the 1-D model), respectively, tend to the same shape with the increasing time in diastole. Figure 3a,b show these pressures (p and p
r in the midpoint) once the flow has become periodic. Figure 3a also shows the excess pressure p
exc in the midpoint, which is proportional to q
IN. The difference between  and p
C is smaller than 2 kPa in systole and becomes smaller with time in diastole (Fig. 3b). From 9 to 10 s, the mean values of
and p
C is smaller than 2 kPa in systole and becomes smaller with time in diastole (Fig. 3b). From 9 to 10 s, the mean values of  and p at any location, p
C and
and p at any location, p
C and  are 12.5 kPa; the same value as predicted by Eqs. 6, 20, 21 and 22.
are 12.5 kPa; the same value as predicted by Eqs. 6, 20, 21 and 22.
Fig. 3.
a Pressure p and reservoir p
r and excess p
exc pressures calculated using the three-element windkessel model with λ = Z
Ao in the midpoint of the single-vessel aortic model, and windkessel pressure  with time. b
with time. b
 and compliance-weighted space-average pressure p
C. c Reservoir pressure p
r calculated using the three-element windkessel model with λ = Z
Ao at x = 0 (inlet), l/4 (1/4), l/2 (mid) and 3l/4 (3/4). d New reservoir pressure
and compliance-weighted space-average pressure p
C. c Reservoir pressure p
r calculated using the three-element windkessel model with λ = Z
Ao at x = 0 (inlet), l/4 (1/4), l/2 (mid) and 3l/4 (3/4). d New reservoir pressure  at the same locations as in (c)
at the same locations as in (c)
Figure 3c shows that p
r calculated with λ = Z
Ao changes in space in systole and early diastole. At any location, p
r is identical to p
per and p
exc is identical to p
con. On the other hand,  is space-independent except for the time alignment (Fig. 3d), and
is space-independent except for the time alignment (Fig. 3d), and  is proportional to the flow at any location (Fig. 4a). At the inlet,
is proportional to the flow at any location (Fig. 4a). At the inlet,  and
and  .
.
Figure 4b shows the blood flow q in the midpoint of the vessel and the convergence of the outflows q
C and  (calculated using Eqs. 13 and 16) to the same shape in late diastole. From 9 to 10 s, the mean values of q at any location, q
C and
(calculated using Eqs. 13 and 16) to the same shape in late diastole. From 9 to 10 s, the mean values of q at any location, q
C and  are equal to
are equal to  ml s−1. During approximately the last half of diastole the flow satisfies
ml s−1. During approximately the last half of diastole the flow satisfies  (Eq. 24); i.e. q increases linearly from zero at the inlet to the exponential shape dictated by
(Eq. 24); i.e. q increases linearly from zero at the inlet to the exponential shape dictated by  at the outlet.
at the outlet.
The forward and backward parts of p and q are space-independent except for the time alignment. Figure 5a, b show  and q
b in the midpoint: in most of the cardiac cycle p
f is greater than p
b and q
f is greater than −q
b; in most of diastole p
f and p
b have a similar shape, as do q
f and −q
b. At the inlet,
and q
b in the midpoint: in most of the cardiac cycle p
f is greater than p
b and q
f is greater than −q
b; in most of diastole p
f and p
b have a similar shape, as do q
f and −q
b. At the inlet,  and
and  when q
IN = 0.
when q
IN = 0.
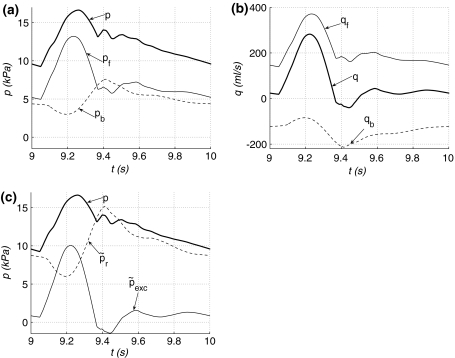
Fig. 5.
Forward (p
f and q
f) and backward (p
b and q
b) contributions to a pressure p and b flow q, and c new reservoir  and excess
and excess  pressures with time in the midpoint of the single-vessel aortic model
pressures with time in the midpoint of the single-vessel aortic model
Figure 5c shows  and
and  in the midpoint;
in the midpoint;  is the major component of p, especially in diastole, and
is the major component of p, especially in diastole, and  significantly determines the pressure shape in systole and early diastole. During approximately the last half of diastole
significantly determines the pressure shape in systole and early diastole. During approximately the last half of diastole  , in agreement with Eqs. 24 and 26. Thus,
, in agreement with Eqs. 24 and 26. Thus,  at the inlet so that
at the inlet so that  captures all the diastolic decay. As we approach the outlet
captures all the diastolic decay. As we approach the outlet  increases and
increases and  decreases.
decreases.
55-Artery Network
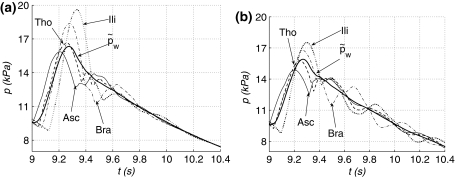
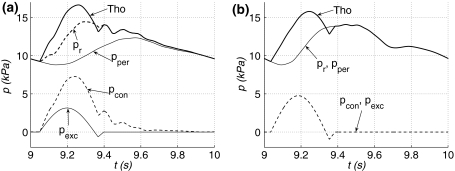
In diastole, pressures everywhere in the normal and well-matched 55-artery models eventually converge to  calculated using Eq. 17 with
calculated using Eq. 17 with  and
and  . Figure 6 shows this convergence at four locations in both models once the flow is periodic, including their decay up to t = 10.4 s due to q
IN = 0. The diastolic pressure decay is also well captured by p
per and p
r (with λ = Z
Ao) (Fig. 7). Moreover,
. Figure 6 shows this convergence at four locations in both models once the flow is periodic, including their decay up to t = 10.4 s due to q
IN = 0. The diastolic pressure decay is also well captured by p
per and p
r (with λ = Z
Ao) (Fig. 7). Moreover,  and
and  everywhere in the well-matched model (Fig. 7b). In the normal model, p
per and p
r, and p
con and p
exc differ in systole and early diastole (Fig. 7a). Figure 8a compares
everywhere in the well-matched model (Fig. 7b). In the normal model, p
per and p
r, and p
con and p
exc differ in systole and early diastole (Fig. 7a). Figure 8a compares  at several locations in the well-matched model, showing their space dependency. Both p
per and p
r are also space-dependent in the normal model.
at several locations in the well-matched model, showing their space dependency. Both p
per and p
r are also space-dependent in the normal model.
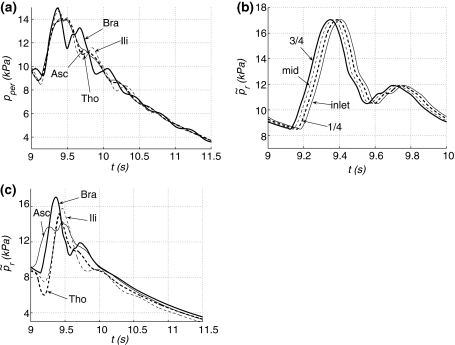
Fig. 6.
Pressure with time at the root of the ascending aorta (Edge 1, Asc) and the midpoint of the thoracic aorta II (Edge 33, Tho), left brachial (Edge 45, Bra) and right external iliac (Edge 52, Ili) arteries of the a normal and b well-matched 55-artery models. Pressures  in thick solid lines. After
in thick solid lines. After  s,
s,  to show the relaxation of both models
to show the relaxation of both models
Fig. 7.
Pressure (Tho) with time in the midpoint of the thoracic aorta II (Edge 33) and reservoir p r (with λ = Z Ao), peripheral p per, excess p exc and conduit p con pressures at the same location in the a normal and b well-matched 55-artery models
Fig. 8.
a Peripheral pressure p
per with time at the root of the ascending aorta (Edge 1, Asc), and the midpoint of the thoracic aorta II (Edge 33, Tho), left brachial (Edge 45, Bra) and right external iliac (Edge 52, Ili) arteries of the well-matched 55-artery model. b New reservoir pressure  with time at
with time at  (inlet), l/4 (1/4), l/2 (mid) and 3l/4 (3/4) in the left brachial artery of the normal 55-artery model. c
(inlet), l/4 (1/4), l/2 (mid) and 3l/4 (3/4) in the left brachial artery of the normal 55-artery model. c
 with time at Asc, Tho, Bra and Ili of the normal 55-artery model. After
with time at Asc, Tho, Bra and Ili of the normal 55-artery model. After  s,
s,  in panels (a) and (c)
in panels (a) and (c)
In both networks,  is equal to p
r (λ = Z
Ao) at the inlet of the ascending aorta and space-independent, except for the time alignment, within any edge. Figure 8b shows this in the left brachial artery of the normal model. Comparison of
is equal to p
r (λ = Z
Ao) at the inlet of the ascending aorta and space-independent, except for the time alignment, within any edge. Figure 8b shows this in the left brachial artery of the normal model. Comparison of  within several edges shows its convergence to the decay given by
within several edges shows its convergence to the decay given by  , except for the time alignment (Fig. 8c).
, except for the time alignment (Fig. 8c).
In systole, the difference between  and p
C is less than 0.8 kPa in the normal model (Fig. 9a) and 0.35 kPa in the well-matched model (Fig. 9b). This difference decreases with time in diastole. Once the flow has become periodic, the mean values (over a cardiac cycle) of
and p
C is less than 0.8 kPa in the normal model (Fig. 9a) and 0.35 kPa in the well-matched model (Fig. 9b). This difference decreases with time in diastole. Once the flow has become periodic, the mean values (over a cardiac cycle) of  and p at any location, p
C and
and p at any location, p
C and  are 12.5 kPa; the same value as predicted by Eqs. 6, 20, 21 and 22. In both models, the outflows q
C and
are 12.5 kPa; the same value as predicted by Eqs. 6, 20, 21 and 22. In both models, the outflows q
C and  tend to the same shape with the increasing time in diastole (Fig. 9c,d).
tend to the same shape with the increasing time in diastole (Fig. 9c,d).
Fig. 9.
a, b Windkessel  and compliance-weighted space-average p
C pressures, and c, d outflows
and compliance-weighted space-average p
C pressures, and c, d outflows  and q
C driven by
and q
C driven by  and p
C, respectively, with time in the normal (a, c) and well-matched (b, d) 55-artery models
and p
C, respectively, with time in the normal (a, c) and well-matched (b, d) 55-artery models
Within any edge in both networks,  and q
b are space-independent except for the time alignment. Figure 10a, b show them in the midpoint of the thoracic aorta of the normal model. In diastole p
f is similar to p
b in shape, and so is q
f to −q
b. They differ more in systole, with p
f and q
f being dominant. Figure 10c shows
and q
b are space-independent except for the time alignment. Figure 10a, b show them in the midpoint of the thoracic aorta of the normal model. In diastole p
f is similar to p
b in shape, and so is q
f to −q
b. They differ more in systole, with p
f and q
f being dominant. Figure 10c shows  and
and  at the same location;
at the same location;  is the major component of the diastolic decay and
is the major component of the diastolic decay and  is greater in systole than in diastole. This result is observed at any location in both models. At the aortic root and in diastole,
is greater in systole than in diastole. This result is observed at any location in both models. At the aortic root and in diastole,  and
and  produces all the pressure decay.
produces all the pressure decay.
Fig. 10.
Forward (p
f and q
f) and backward (p
b and q
b) contributions to a pressure p and b flow q, and c new reservoir  and excess
and excess  pressures with time in the midpoint of the thoracic aorta II (Edge 33) of the normal 55-artery model
pressures with time in the midpoint of the thoracic aorta II (Edge 33) of the normal 55-artery model
Figure 11 compares the diastolic decays of  in all the models studied using a semi-logarithmic plot. They are all approximately exponential with a time constant that differs from
in all the models studied using a semi-logarithmic plot. They are all approximately exponential with a time constant that differs from  s by less than 5 %. If peripheral compliances are zero (i.e.
s by less than 5 %. If peripheral compliances are zero (i.e.  ) in the normal 55-artery model and
) in the normal 55-artery model and  , are increased so that C
c is equal to the original C
T, then the time constant is 1.6 s. This is in agreement with Eq. 25. In all cases,
, are increased so that C
c is equal to the original C
T, then the time constant is 1.6 s. This is in agreement with Eq. 25. In all cases,  approaches the asymptote P
out = 0 with time.
approaches the asymptote P
out = 0 with time.
Fig. 11.
Diastolic  on a logarithm scale with time in the single-vessel aorta (1art) and the normal (55art) and well-matched (55art wm) 55-artery models. After
on a logarithm scale with time in the single-vessel aorta (1art) and the normal (55art) and well-matched (55art wm) 55-artery models. After  s,
s,  to show the relaxation of the models
to show the relaxation of the models
Discussion and Concluding Remarks
This work has provided a theoretical and numerical description of the mechanics underlying the reservoir and excess pressures calculated using the two- and three-element windkessel models, and has proposed a new definition of them that provides valuable information for pulse wave analysis and overcomes the limitations of the current algorithms. Indeed, the two-element windkessel model requires a measurement of the left ventricular flow ejection q IN, which cannot always be measured in vivo, to calculate the reservoir pressure. The three-element windkessel model does not require q IN, but the reservoir pressure that provides is not defined explicitly.
We start by discussing the theoretical results obtained when the two-element windkessel model is used (e.g. Wang et al. 2003; Tyberg et al. 2008, 2009; Davies et al. 2010). In a network with inviscid flow and terminal outflows modelled using single resistances (i.e. all the compliance of the vessel walls is located within the 1-D model network and all the flow resistance is at the periphery of the network), the reservoir pressure p
w calculated using Frank’s windkessel Eq. 1 is the space-independent pressure to which blood pressure p at any location tends with the increasing time in diastole. This result is in agreement with in vivo canine pressures, measured every 2 cm from the aortic root to the femoral artery, being approximately uniform during the last two-thirds of diastole (Wang et al. 2003). If we numerically allow for some peripheral compliance, then p at any location tends to the space-independent  (Fig. 6), which like p
w depends on global properties (left ventricular flow ejection, total compliance and resistance and outflow pressure) (Eq. 17), dictates the total flow to the periphery (Eq. 16) and is equal to p
w when terminal outflows are modelled using single resistances.
(Fig. 6), which like p
w depends on global properties (left ventricular flow ejection, total compliance and resistance and outflow pressure) (Eq. 17), dictates the total flow to the periphery (Eq. 16) and is equal to p
w when terminal outflows are modelled using single resistances.
Since  was derived assuming blood inertia to be zero, the results in the previous paragraph suggest that there is a progressive loss of blood inertia in diastole, which is recovered by the time of the next left ventricular ejection. Thus, a clear distinction exists between the systolic and diastolic mechanics underlying blood flow in systemic arteries. In systole, the changes in blood pressure and flow produced by the contraction of the left ventricle propagate in the form of waves (called pulse waves) through the systemic arteries. These waves are reflected at the arterial junctions, peripheral branches, aortic valve (when shut), and any other change in arterial geometry and elasticity, and produce space-dependent pressures and flows. With the increasing time, the number of reflected waves increases exponentially, but the amplitude of the pressure and flow changes associated with these waves tends to decrease exponentially (Alastruey et al., 2009). In diastole, waves progressively lose inertia and the flow is dominated by the global relaxation of the compliant vessels.
was derived assuming blood inertia to be zero, the results in the previous paragraph suggest that there is a progressive loss of blood inertia in diastole, which is recovered by the time of the next left ventricular ejection. Thus, a clear distinction exists between the systolic and diastolic mechanics underlying blood flow in systemic arteries. In systole, the changes in blood pressure and flow produced by the contraction of the left ventricle propagate in the form of waves (called pulse waves) through the systemic arteries. These waves are reflected at the arterial junctions, peripheral branches, aortic valve (when shut), and any other change in arterial geometry and elasticity, and produce space-dependent pressures and flows. With the increasing time, the number of reflected waves increases exponentially, but the amplitude of the pressure and flow changes associated with these waves tends to decrease exponentially (Alastruey et al., 2009). In diastole, waves progressively lose inertia and the flow is dominated by the global relaxation of the compliant vessels.
The numerical results show a transient exponential building-up in the diastolic pressure waveform p from the initial zero pressure. Separation of p into peripheral p per and conduit p con contributions suggests that this building-up is due to p per and, hence, generated by waves originated as reflections at the peripheral outflows (Alastruey et al., 2009). Indeed, a simulation started at zero pressure in a network with completely absorbent peripheral outflows produces a periodic pressure p = p con without a physiological diastolic decay from the first heartbeat. Therefore, peripheral resistances must be greater than peripheral characteristic impedances in order for arteries to store sufficient blood volume and potential energy in systole and generate sufficient pressure and kinetic energy for the perfusion of the periphery in diastole.
The numerical results in this work also suggest that  in systole and early diastole is well approximated by the compliance-weighted space-average pressure of the arterial network p
C defined in 14. In diastole
in systole and early diastole is well approximated by the compliance-weighted space-average pressure of the arterial network p
C defined in 14. In diastole  and p
C (and the flows
and p
C (and the flows  and q
C that they drive) gradually converge to the same shape (Figs. 3b, 4b, 9), which is consistent with the gradual convergence of p to
and q
C that they drive) gradually converge to the same shape (Figs. 3b, 4b, 9), which is consistent with the gradual convergence of p to  . Therefore, p
C provides an approximate physical interpretation of
. Therefore, p
C provides an approximate physical interpretation of  (and hence p
w), and shows that the more compliant arteries are, the larger their contribution is to the total peripheral outflow in diastole.
(and hence p
w), and shows that the more compliant arteries are, the larger their contribution is to the total peripheral outflow in diastole.
The mechanics underlying the reservoir pressure p
r calculated using the three-element windkessel model (e.g. Aguado-Sierra et al. (2008); Davies et al. (2007); Parker (2009); Vermeersch et al. (2009)) have been studied taking λ = Z
Ao. Under this assumption, this work has shown that p
r is not space-independent in systole and early diastole (Figs. 3c, 8a). Moreover, the mean p
r is smaller than the mean p
w when the flow is periodic; the mean p
w being equal to the mean blood pressure for inviscid flow. Aguado-Sierra et al. (2008) assumed well-matched junctions for forward-travelling waves, which seems to be a reasonable approximation in normal humans and animals (Milnor, 1989; Papageorgiou and Jones, 1987). Under this assumption, this work has shown that p
r is equal to the pressure p
per generated by the reflected waves originated at the terminal reflection sites, and p
exc is the pressure p
con obtained by propagating the left ventricular flow ejection without any peripheral reflection (Fig. 7b). The larger the reflection coefficients for forward-travelling waves at junctions are, the less valid these descriptions of p
r and p
exc become (Fig. 7a). Indeed, if junctions are not well-matched for forward-travelling waves, p
r calculated at the ascending aorta with λ = Z
Ao differs from p
per in systole and early diastole, and only converges to p
per later in diastole. A similar relation, therefore, exists between  and
and  .
.
The new reservoir  and excess
and excess  pressures (Eq. 26) proposed here overcome the limitations of the two- and three-element windkessel models, since
pressures (Eq. 26) proposed here overcome the limitations of the two- and three-element windkessel models, since  and
and  are independent of q
IN and well defined at any location in the arterial network. Moreover, if local compliances are constant within each arterial edge,
are independent of q
IN and well defined at any location in the arterial network. Moreover, if local compliances are constant within each arterial edge,  is space-independent within each edge (except for the time alignment) unlike p
r, and
is space-independent within each edge (except for the time alignment) unlike p
r, and  is always proportional to the local flow unlike p
exc. Calculation of
is always proportional to the local flow unlike p
exc. Calculation of  requires simultaneous pressure and velocity q/A
0 measures and an estimation of the local pulse wave speed c, which can be obtained using the methods in Davies et al. (2006) and Khir et al. (2001).
requires simultaneous pressure and velocity q/A
0 measures and an estimation of the local pulse wave speed c, which can be obtained using the methods in Davies et al. (2006) and Khir et al. (2001).
In the models studied here,  is the major contribution to the diastolic pressure decay, while
is the major contribution to the diastolic pressure decay, while  plays a more significant role in shaping the pressure waveform in systole and early diastole (Figs. 5c, 10c). At the aortic root
plays a more significant role in shaping the pressure waveform in systole and early diastole (Figs. 5c, 10c). At the aortic root  produces all the diastolic pressure decay, since
produces all the diastolic pressure decay, since  in diastole due to q = 0. Note that
in diastole due to q = 0. Note that  is made up of contributions to pressure from distal locations (Eq. 27) and, hence, plays a similar role to p
per. However, p
per accounts only for distal contributions that originate at peripheral reflection sites, whereas
is made up of contributions to pressure from distal locations (Eq. 27) and, hence, plays a similar role to p
per. However, p
per accounts only for distal contributions that originate at peripheral reflection sites, whereas  includes contributions from reflections at any other change in distal arterial geometry or elasticity; e.g. at all the arterial junctions.
includes contributions from reflections at any other change in distal arterial geometry or elasticity; e.g. at all the arterial junctions.
The separation of p into  and
and  is closely related to the separation of p into forward p
f and backward p
b waves described in Westerhof et al. (1972), Parker and Jones (1990), and Hughes and Parker (2009), as shown by Eq. 27. In diastole, p
f and p
b are approximately equal and relatively large, leading to self-cancelling forward q
f and backward q
b flow waves (Figs. 5a, b, 10a, b). This diastolic pattern was considered to be a necessary result of the wave separation analysis, but its origin was difficult to explain physically, since the heart is not ejecting blood into the aorta in diastole (Parker 2009).
is closely related to the separation of p into forward p
f and backward p
b waves described in Westerhof et al. (1972), Parker and Jones (1990), and Hughes and Parker (2009), as shown by Eq. 27. In diastole, p
f and p
b are approximately equal and relatively large, leading to self-cancelling forward q
f and backward q
b flow waves (Figs. 5a, b, 10a, b). This diastolic pattern was considered to be a necessary result of the wave separation analysis, but its origin was difficult to explain physically, since the heart is not ejecting blood into the aorta in diastole (Parker 2009).
Pulse wave analysis using  and
and  provides a more physically plausible description of p
f and p
b and their relation to q. At any time,
provides a more physically plausible description of p
f and p
b and their relation to q. At any time,  is proportional to q and, hence, determines the magnitude and direction of q (Eq. 27). The increase in systolic p
f at the aortic root generated by the left ventricular flow ejection is propagated to distal locations increasing
is proportional to q and, hence, determines the magnitude and direction of q (Eq. 27). The increase in systolic p
f at the aortic root generated by the left ventricular flow ejection is propagated to distal locations increasing  . In diastole, a relatively smaller
. In diastole, a relatively smaller  indicates a better balance between proximal and distal contributions to p. In normal diastolic conditions, q
IN = 0 and hence p
b is totally reflected at the closed aortic valve, so that
indicates a better balance between proximal and distal contributions to p. In normal diastolic conditions, q
IN = 0 and hence p
b is totally reflected at the closed aortic valve, so that  . Thus
. Thus  is a better approximation to the diastolic pressure decay than p
b is. On the other hand, p
f is partially reflected at the peripheral reflection sites. This pattern of wave reflections of p
f at the peripheral reflection sites and p
b at the closed aortic valve leads to a positive
is a better approximation to the diastolic pressure decay than p
b is. On the other hand, p
f is partially reflected at the peripheral reflection sites. This pattern of wave reflections of p
f at the peripheral reflection sites and p
b at the closed aortic valve leads to a positive  in most of diastole, so that q is mostly directed toward the periphery. The progressive loss of diastolic blood inertia in the 1-D balance of momentum that leads to the convergence of p to
in most of diastole, so that q is mostly directed toward the periphery. The progressive loss of diastolic blood inertia in the 1-D balance of momentum that leads to the convergence of p to  also yields uniform p
f and p
b in diastole, and hence
also yields uniform p
f and p
b in diastole, and hence  , except for the time alignment (Fig. 8c). The summation of p
f and p
b in diastole produces a space-independent p and their difference leads to non-zero q in diastole.
, except for the time alignment (Fig. 8c). The summation of p
f and p
b in diastole produces a space-independent p and their difference leads to non-zero q in diastole.
The numerical results presented here have shown that the time constant that characterises the diastolic pressure decay can be reasonably estimated using an exponential fitting to diastolic pressure at an arbitrary arterial location (Fig. 11). It is important to emphasise that the longer the diastolic time (e.g. when a heartbeat is missed) the better the accuracy of the fitting. However, the assumption of constant total compliance becomes less valid for a larger change in pressure, since in vivo arterial compliance is pressure dependent (Roy 1880–1882; Frank 1899).
Experimental and clinical investigations will be required to assess the validity of the results presented here and test the relevance of the new definition of reservoir and excess pressures. According to this work, they should improve our understanding of the relationship between the pattern of pulse waveforms and the physical properties of the cardiovascular system.
Acknowledgments
The author would like to acknowledge Emeritus Professor Kim Parker (Imperial College London) for his helpful comments on the paper. This work was funded by a British Heart Foundation Intermediate Basic Science Research Fellowship (FS/09/030/27812).
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
The excess pressure was called wave pressure in some papers (e.g. Tyberg et al. (2009)).
References
- Aguado-Sierra J, Alastruey J, Wang J-J, Hadjiloizou N, Davies J, Parker K. Separation of the reservoir and wave pressure and velocity from measurements at an arbitrary location in arteries. Proc Inst Mech Eng Part H J Eng Med. 2008;222:403–16. doi: 10.1243/09544119JEIM315. [DOI] [PubMed] [Google Scholar]
- Alastruey J. Numerical modelling of pulse wave propagation in the cardiovascular system: development, validation and clinical applications. Ph.D. thesis, Imperial College London, University of London, UK 2006.
- Alastruey J, Parker K, Peiró J, Sherwin S. Lumped parameter outflow models for 1-D blood flow simulations: effect on pulse waves and parameter estimation. Commun Comput Phys. 2008;4:317–36. [Google Scholar]
- Alastruey J, Parker K, Peiró J, Sherwin S. Analysing the pattern of pulse waves in arterial networks: a time-domain study. J Eng Math. 2009;64:331–51. doi: 10.1007/s10665-009-9275-1. [DOI] [Google Scholar]
- Caro C, Pedley T, Schroter R, Seed W. The mechanics of the circulation. Oxford: Oxford University Press; 1978. [Google Scholar]
- Davies J, Whinnett Z, Francis D, Willson K, Foale R, Malik I, Hughes A, Parker K, Mayet J. Use of simultaneous pressure and velocity measurements to estimate arterial wave speed at a single site in humans. Am J Physiol Heart Circ Physiol. 2006;290:H878–85. doi: 10.1152/ajpheart.00751.2005. [DOI] [PubMed] [Google Scholar]
- Davies J, Hadjiloizou N, Leibovich D, Malaweera A, Alastruey J, Whinnett Z, Manisty C, Francis D, Aguado-Sierra J, Foale R, Malik I, Parker K, Mayet J, Hughes A. Importance of the aortic reservoir in determining the shape of the arterial pressure waveform—The forgotten lessons of Frank. Artery Res. 2007;1:40–5. doi: 10.1016/j.artres.2007.08.001. [DOI] [Google Scholar]
- Davies J, Baksi J, Francis D, Hadjiloizou N, Whinnett Z, Manisty C, Aguado-Sierra J, Foale R, Malik I, Tyberg J, Parker K, Mayet J, Hughes A. The arterial reservoir pressure increases with aging and is the major determinant of the aortic augmentation index. Am J Physiol Heart Circ Physiol. 2010;298:H580–6. doi: 10.1152/ajpheart.00875.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frank O. Die Grundform des arteriellen Pulses. Erste AbhandlungMathematische Analyse Z Biol. 1899;37:483–526. (Translated by Sagawa K, Lie RK, Schaefer J. J Mol Cell Cardiol. 1990;22:253–77) . [DOI] [PubMed]
- Hughes A, Parker K. Forward and backward waves in the arterial system: impedance or wave intensity analysis? Med Bio Eng Comput. 2009;47:207–10. doi: 10.1007/s11517-009-0444-1. [DOI] [PubMed] [Google Scholar]
- Khir A, O’Brien A, Gibbs J, Parker K. Determination of wave speed and wave separation in the arteries. J Biomech. 2001;34:1145–55. doi: 10.1016/S0021-9290(01)00076-8. [DOI] [PubMed] [Google Scholar]
- Matthys K, Alastruey J, Peiró J, Khir A, Segers P, Verdonck P, Parker K, Sherwin S. Pulse wave propagation in a model human arterial network: assessment of 1-D numerical simulations against in vitro measurements. J Biomech. 2007;40:3476–86. doi: 10.1016/j.jbiomech.2007.05.027. [DOI] [PubMed] [Google Scholar]
- Milnor W. Hemodynamics. Baltimore: Williams and Wilkins; 1989. [Google Scholar]
- Olufsen M, Peskin C, Kim W, Pedersen E, Nadim A, Larsen J. Numerical simulation and experimental validation of blood flow in arteries with structured-tree outflow conditions. Annals Biomed Eng. 2000;28:1281–99. doi: 10.1114/1.1326031. [DOI] [PubMed] [Google Scholar]
- Papageorgiou G, Jones N. Arterial system configuration and wave reflection. J Biomed Eng. 1987;9:299–301. doi: 10.1016/0141-5425(87)90076-8. [DOI] [PubMed] [Google Scholar]
- Parker K, Jones C. Forward and backward running waves in the arteries: analysis using the method of characteristics. J Biomech Eng. 1990;112:322–6. doi: 10.1115/1.2891191. [DOI] [PubMed] [Google Scholar]
- Parker K. An introduction to wave intensity analysis. Med Bio Eng Comput. 2009;47:175–88. doi: 10.1007/s11517-009-0439-y. [DOI] [PubMed] [Google Scholar]
- Quarteroni A, Formaggia L. Mathematical modelling and numerical simulation of the cardiovascular system. In Ayache N, editors. Modelling of living systems. Amsterdam: Elsevier; 2004.
- Roy C. The elastic properties of the arterial wall. J Physiol (Lond) 1880;3:125–59. doi: 10.1113/jphysiol.1881.sp000088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steele B, Wan J, Ku J, Hughes T, Taylor C. In vivo validation of a one-dimensional finite-element method for predicting blood flow in cardiovascular bypass grafts. IEEE Trans Biomed Eng. 2003;50:649–56. doi: 10.1109/TBME.2003.812201. [DOI] [PubMed] [Google Scholar]
- Stergiopulos N, Young D, Rogge T. Computer simulation of arterial flow with applications to arterial and aortic stenoses. J Biomech. 1992;25:1477–88. doi: 10.1016/0021-9290(92)90060-E. [DOI] [PubMed] [Google Scholar]
- Tyberg J, Shrive N, Bouwmeester J, Parker K, Wang J-J. The reservoir—wave paradigm: potential implications for hypertension. Curr Hypertens Rep. 2008;4:203–12. doi: 10.2174/157340208785132572. [DOI] [Google Scholar]
- Tyberg J, Davies J, Wang Z, Whitelaw W, Flewitt J, Shrive N, Francis D, Hughes A, Parker K, Wang J-J. Wave intensity analysis and the development of the reservoir—wave approach. Med Biol Eng Comput. 2009;47:221–32. doi: 10.1007/s11517-008-0430-z. [DOI] [PubMed] [Google Scholar]
- Čanić S, Kim E. Mathematical analysis of the quasilinear effects in a hyperbolic model of blood flow through compliant axi-symmetric vessels. Math Meth Appl Sci. 2003;26:1161–86. doi: 10.1002/mma.407. [DOI] [Google Scholar]
- Vermeersch SJ, Rietzschel E, Buyzere MD, Bortel LV, Gillebert T, Verdonck P, Segers P. The reservoir pressure concept: the 3-element windkessel model revisited? Application to the Asklepios population study. J Eng Math. 2009;64:417–428. doi: 10.1007/s10665-009-9286-y. [DOI] [Google Scholar]
- Wang J-J, O’Brien A, Shrive N, Parker K, Tyberg J. Time-domain representation of ventricular-arterial coupling as a windkessel and wave system. Am J Physiol Heart Circ Physiol. 2003;284:H1358–68. doi: 10.1152/ajpheart.00175.2002. [DOI] [PubMed] [Google Scholar]
- Westerhof N, Bosman F, de Vries C, Noordergraaf A. Analog studies of the human systemic arterial tree. J Biomech. 1969;2:121–43. doi: 10.1016/0021-9290(69)90024-4. [DOI] [PubMed] [Google Scholar]
- Westerhof N, Elzinga G, Sipkema P. An artificial arterial system for pumping hearts. J Appl. Physiol. 1971;31:776–781. doi: 10.1152/jappl.1971.31.5.776. [DOI] [PubMed] [Google Scholar]
- Westerhof N, Sipkema P, Bos GVD, Elzinga G. Forward and backward waves in the arterial system. Cardiov Res. 1972;6:648–56. doi: 10.1093/cvr/6.6.648. [DOI] [PubMed] [Google Scholar]
- Zhang H, Li JK-J. A novel wave reflection model of the human arterial system. Cardiovasc Eng. 2009;9:39–48. doi: 10.1007/s10558-009-9074-3. [DOI] [PubMed] [Google Scholar]