The traditional gap between surgeons and internists was much wider 100 years ago than nowadays. At the beginning of the twentieth century, neither group was particularly open to the idea of scholarly exchange. In this respect, both early pioneers of laparoscopy, Georg Kelling (1866–1945) (Figure 1), a German surgeon of Dresden, and Hans Christian Jacobaeus (1879–1937) (Figure 2), an internist from Stockholm, Sweden, were interesting exceptions.
Figure 1.
“Georg Kelling (1866–1945)” Figure 1–9 in Highlights in the History of Laparoscopy.
Figure 2.

“Hans Christian Jacobaeus (1879–1937)” Figure 2–4 in Highlights.
Georg Kelling - Coelioscopy 1901
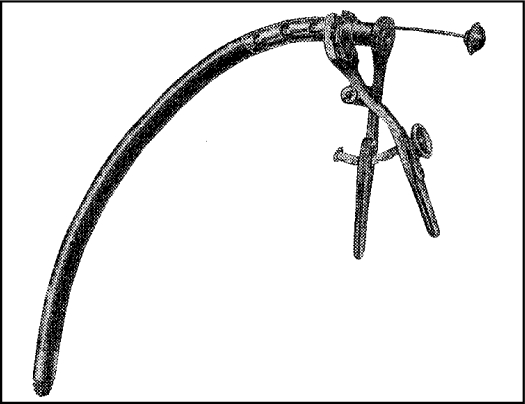
Although Kelling regarded himself as a surgeon, he devoted a great deal of energy to the development of “non-surgical” (or “minimally invasive”) methods of treatment. Since Kelling was convinced that determining stomach volume could have practical significance for healing diseases caused by hardening of the stomach walls, he conducted hundreds of experiments on cadavers and animals to measure the stomach capacity. In the 1890s, Kelling (against the skepticism of his colleagues), devised an esophagoscope by combining a ridged proximal part with a flexible distal part using the optical system designed by Nitze1 (Figures 3, 4).
Figure 3.
“Kelling esophagoscope before insertion”
Figure 4.
“Esophagoscope straightened after insertion”
Kelling spent the summer of 1898 in Breslau, at the Royal Surgical Clinic under the leadership of Mikulicz, a famous surgeon and the inventor of clinical esophagoscopy and gastroscopy. There, Kelling had many opportunities to refine his endoscopic technique and performed numerous examinations using his own “semi-flexible tube endoscopy” system. Kelling also worked with the Czech surgeon Vitezslav Chlumsky (1867–1943) in Breslau. They performed high-pressure gastrointestinal insufflations to examine the viability of gastroenterostomy, a procedure perfected by Mikulicz. These studies demonstrated that the enterostomy between stomach and small intestine could withstand increased intraluminal pressure.
At the turn of the century Kelling focused his attention on the problem of gastrointestinal bleeding into the abdominal cavity, which was fatal to many patients during that time. Gastrointestinal bleeding was particularly dangerous, and did not always manifest itself by hematemesis or melena. The only available method to establish a diagnosis and provide treatment was laparotomy. However, as the German surgeon observed, opening the abdomen might worsen the patient's condition. To halt blood loss, Kelling proposed a non-surgical treatment: high-pressure insufflation of air into the abdominal cavity, a technique he called Luffttamponade (air-tamponade)2 (Figure 5).
Figure 5.

“An apparatus for creating Lufttamponade” Figure 1–7 in Highlights.
In 1901, Kelling used both his own experiments with insufflation and the physiological experiments of other European scientists to calculate that a pressure of approximately 50 mm Hg could alleviate bleeding into the abdomen. Kelling carried out numerous experiments on live dogs, insufflating air up to the pressure of 100 mm Hg(!). Still, 2 of 20 dogs died as a result of his experiments. Since at that time the pathophysiology of pneumoperitoneum was still unknown, Kelling proclaimed the procedure to be perfectly harmless. “After an examination, a dog is as cheerful as it was before,” he wrote.2
Kelling wanted to observe the effects of his insufflation efforts. “I asked myself, how do the organs react to the introduction of air? To find out, I devised a method of using an endoscope on an unopened abdominal cavity (coelioscopy),” he stated.2 To visualize the effects of the high-pressure Lufttamponade on the abdominal organs, Kelling introduced a Nitze cystoscope directly through the abdominal wall. Given the force of the air pressure, it came as no surprise, Kelling observed, that the abdominal organs were colorless and smaller than normal.
Kelling continued his work on stomach insufflation, but did not return to coeliscopy and did not publish any work on Lufttamponade or endoscopy of an unopened abdominal cavity.3 It should be stressed that Kelling's “Coelioscopy” was created as an additional method to view the effects of Lufttamponade, not as an endoscopic method itself.
Hans Christian Jacobaeus - Laparothorascoscopy 1910
Unaware of Kelling's work, Hans Christian Jacobaeus (1879–1937), a Swedish internist, reported on his experience with laparothorascopic technique in humans in 1910.4 Unfortunately, there is little detailed information on his initial experiments with abdominal endoscopy. We know that before he began his work with “laparothorascopy,” he was aware of artificial pneumothorax, and pneumoperitoneum in the treatment of peritonitis tuberculosa.
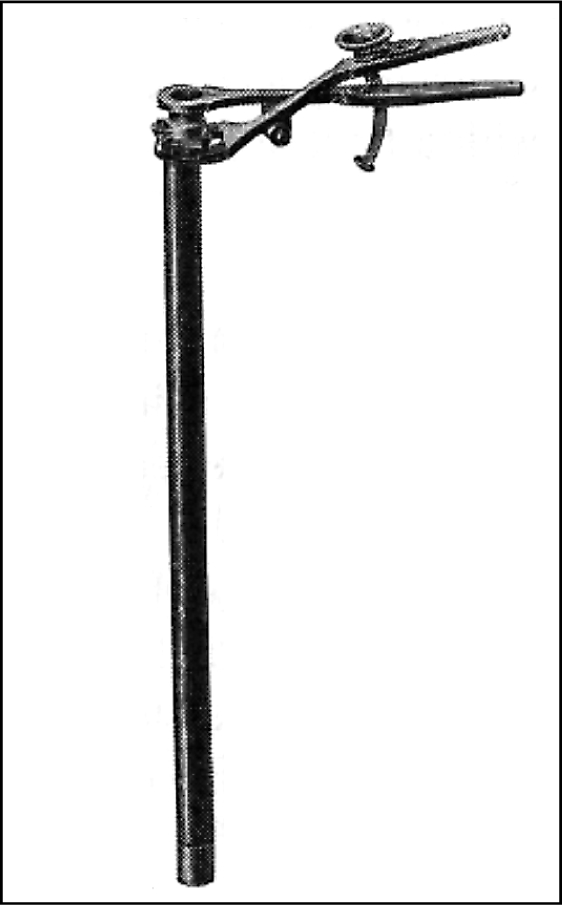
Jacobaeus entitled his first article on abdominal endoscopy “Concerning the Possibility of Applying Cystoscopy in the Examination of Serous Cavities.”4 The Stockholm internist evacuated ascites and created air-pneumoperitoneum using a trocar with a trap-valve (Figure 6). Jacobaeus' initial experience with this procedure was basically restricted to patients with ascites (17 patients); he examined only two patients without ascites by means of laparoscopy. He described his findings and outlined a range of applications. “It is highly significant,” he wrote, “that it will be possible to investigate the front and upper parts of the liver.” He felt that the stomach was difficult to reach by laparoscopic means; he had been unable, he noted, “to make any observations of value.”4
Figure 6.
“Jacobaeus' trocar” Figure 2-2 in Highlights.
Despite such limitations, Jacobaeus was enthusiastic about the method. He published articles in Germany, France, and Sweden, and delivered a lecture at an international conference in London. An important milestone in the development of laparothorascopy was Jacobaeu's trip to Hamburg in January, 1912, where he presented this technique to Ludolph Brauer at Eppendorfer Hospital. Brauer was an influential figure in the medical world, both a university professor and editor of a German medical journal. At that time, Brauer was preparing for the Second International Congress of Tuberculosis, and was keenly interested in the use of artificial pneumothorax for treatment of tuberculosis.5 Due to Brauer's influence, Jacobaeus' remarkable work on laparothorascopy (170 pages!) was published only several months later.
In a 1912 monograph, Jacobaeus gave an exact description of the patients' conditions and the 97 laparoscopies performed between 1910 and 1912 in Stockholm's community hospital.6 Jacobaeus also described the therapeutic application of laparoscopy, namely allowing air to remain in the abdominal cavity. “According to older surgeons,” he wrote, “the entry of air into the peritoneum should exert a favorable influence on the healing.” In all cases but one, Jacobaeus observed a rapid improvement in the patients and concluded, “One could, in any event, exclude an injurious effect of the air entry.” With typical reserve, he refrained from deciding whether patients actually benefitted from the procedure; his material was too limited.
In 1912, Jacobaeus differentiated between patients with and without ascites. He viewed laparoscopy on patients with ascites as simple and uncomplicated. It is remarkable that most of the patients selected suffered from acute ascites. The amount of ascites was less than three liters in only four cases; usually patients had 8 to 10 liters, and in one case 23 liters. The operation was more difficult in those without ascites, as Jacobaeus explained, “due to the risk of injuring the intestinal tract.” According to his report, Jacobaeus had conducted only eight studies (out of 97 total patients) on patients without ascites. He advocated a cautious approach; should injury to the intestine occur in even a small percentage of cases, Jacobaeus recommended “rejecting the entire procedure.” For patients without ascites, he undertook laparoscopy on only rare occasions and with great circumspection.
Interestingly, Jacobaeus also addressed the issue of what he termed “Probelaparotomie oder Laparoskopie” (Exploratory laparotomy or laparoscopy).6 He discussed this question with “several colleagues including surgeons, and heard very different opinions on it.” As Jacobaeus noted, “The result of our discussions was that one must always individualize... What plays the largest role at this time is which method one is accustomed to. Naturally a surgeon always performs an exploratory laparotomy while an internist with some experience in laparoscopy will prefer the latter operation.”
Final Remarks:
Kelling saw little future in abdominal endoscopy. On the other hand, Jacobaeus was an energetic proponent of laparoscopy and did much to popularize this technique. For many reasons, however, laparoscopy did not make much headway into mainstream medical practice before the First World War.7
References:
- 1. Kelling G. Mittelung zur Benutzung des Oesophagoscops. Allgemeine Medicinsche Central-Zeitung. 1896; 65: 73 [Google Scholar]
- 2. Kelling G. Die Tamponade der Bauchhöhle mit Luft zur Stillung lebensgefährlicher Intestinalblutungen. Münch Med Wochenschr. 1901; 48: 1480–1483; 1535–1538 [Google Scholar]
- 3. Kelling G. Untersuchungen über die Spannungszustände der Bauchwand, der Magen-und der Darmwand. Zeitschr Biol. 1903; 44: 161–258 [Google Scholar]
- 4. Jacobaeus HC. Ueber die Möglichkeit die Zystokopie bei Untersuchung seröser Höhlungen anzuwenden. Münch Med Wochenschr. 1910; 57: 2090–2092 [Google Scholar]
- 5. Brauer L. Über Laparo- und Thorakoskopie von H.C. Jacobaeus, Privatdozent Stockholm. Geleitwort. Beitr Klin Tuberk. 1912; 25: I–II [Google Scholar]
- 6. Jacobaeus HC. Über Laparo- und Thorakoskopie. Beitr Klin Tuberk. 1912; 25: 185–354 [Google Scholar]
- 7. Litynski GS. Highlights in the History of Laparoscopy. Frankfurt/Main, Germany: Barbara Bernert Verlag, 1996 [Google Scholar]