Abstract
During the early 1980s, news of Semm's laparoscopic appendectomy was rippling through German medical circles. Erich Mühe, fascinated by Semm's technique and spurred by successes of the Erlangen endoscopists, came up with the idea of laparoscopic removal of gallstones. In 1984, Mühe had already worked out the details of an operative laparoscope, the “Galloscope,” and on September 12, 1985, he carried out the first laparoscopic cholecystectomy. Later, he modified his technique and operated through a trocar sleeve. Finally, he designed an “open laparoscope” with a circular light. By March 1987, Mühe had conducted 97 endoscopic gallbladder removals. He published information about his technique at the Congress of the German Surgical Society (April 1986) and at other surgical meetings in Germany. His concept, however, was ignored. In the middle of the 1980s, the surgical community was still not prepared for the era of “minimally invasive therapy.” Erich Mühe was a surgeon ahead of his time.
INTRODUCTION
In the 1960s, physicians of the Internal Clinic at the University of Erlangen, Germany, successfully performed endoscopic duodenoscopy, one of the earliest reports of that procedure. The first endoscopic retrograde cholangio-pancreaticography (ERCP) followed in 1970.1 In 1973, two Erlangen internists, Classen and Demling, performed an endoscopic papillotomy using their own device (Erlanger Papillotom). In Erlangen, 159 patients underwent this endoscopic procedure by the summer of 1976. By 1977, more than 1,500 papillotomies had been performed in ten West German centers, with an overall success rate of 93 percent. Complications occurred much less frequently than with transduodenal papillotomy, and the mortality rate dropped to 1.1 percent.2
Many surgeons were sharply critical of internists' entrance into classical fields of surgery. At the University of Erlangen, on the other hand, the surgeons had a different reaction. According to Erich Mühe (b. 1938), then an assistant in the Surgical Clinic, the Erlangen surgeons “respected the internists' pioneering work”3 on polypectomy in the upper and lower gastrointestinal tracts, loop biopsy, endoscopic tumor resection, and removal of foreign bodies. “We were very proud of ‘our’ internists,” he noted years after.3 In 1982, Mühe left Erlangen and became the Head of the Surgical Clinic in the Böblingen county hospital.
Laparoscopic Cholecystectomy
During this time, news of Semm's laparoscopic appendectomy was rippling through German medical circles. Although Semm's first report did not appear in the medical press until 1982, German surgeons were already aware of his path-breaking work.4 Mühe, spurred by successes of the Erlangen endoscopists and fascinated by Semm's technique, came up with the idea of laparoscopic cholecystectomy (LC). He recalls his underlying motivation:
I had the overwhelming feeling that we [general surgeons] had already lost traditional surgical fields like polypectomy, papillotomy, and now even endoscopic appendectomy was discussed. I was convinced that if we passed up this chance like endoscopic cholecystectomy, internists and gynecologists would again take away a piece of our competence.5 (Figure 1)
Figure 1.
Erich Mühe. (1986) Fig. 12-14 in Highlights.
In late September 1984, four packages of gynecological endoscopic instruments were delivered to the Böblingen hospital.6 Mühe realized that Semm's instruments were sufficient to remove a normal gallbladder, but he had concerns about the gallbladders containing numerous stones. Mühe gradually worked out the details of a new operative laparoscope, the “Galloscope.” It had side-view optics, instrumentation channel with valves, light conductor, and a duct for creating pneumoperitoneum.
The First LC on September 12, 1985
Almost five years to the date from Semm's first fully endoscopic appendectomy, Mühe adopted Semm's technique and employed his own “Galloscope.” He used a Veress needle to establish pneumoperitoneum and followed each step of the surgical laparoscopy established by Semm: pneumoperitoneum, trocars and insertion site for the “Galloscope.” Mühe then inserted a mandrin within a trocar sleeve and introduced his “Galloscope” through the umbilicus.7 The operation took two hours and went exceptionally well (Figure 2, 3).
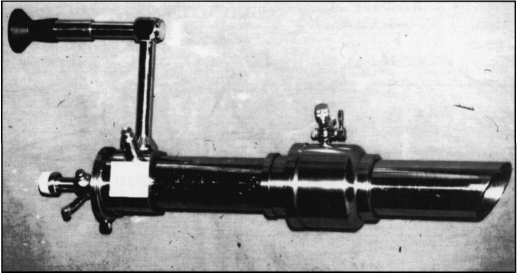
Figure 2.
The “Galloscope” of Mühe had side-view optics, an instrumentation channel with valves, light conductor, and duct for creating pneumoperitoneum. Fig. C-9 in Highlights.
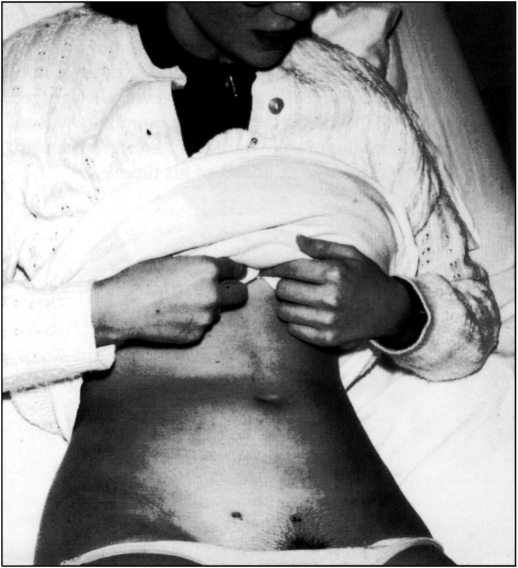
Figure 3.
Mühe followed each step of the surgical laparoscopy established by Semm; he first used lower abdominal access for the “Galloscope.” Later, Mühe introduced the laparoscope under the right costal arch. Fig. 12-7 in Highlights.
Like many laparoscopists, Mühe was astonished at his patients' rapid recoveries. “I couldn't believe it,” he recalled ten years later. “The patients had bowel movements almost immediately after the surgery and could eat supper the same evening. Over and over I asked myself what factors could be responsible.”8 Mühe came to the conclusion that “the approach was like magic.”9 That confirmed Semm's observations.
Mühe's Modifications: Gasless Technique, LC through Trocar Sleeve, and “Open Laparoscope”
Based on this insight, Mühe concluded that he could do away with pneumoperitoneum, created only to open the path from umbilicus to gallbladder. After several laparoscopic cholecystectomies, Mühe slightly changed his technique to introduce the laparoscope under the right costal arch. “I soon noticed that the costal margin served as a firm bone roof above the gallbladder,” noted Mühe, explaining his modification. “I strongly believed that the gasless laparoscopic cholecystectomy would find more acceptance.”10
Mühe's creative simplification led him to other modifications. He was intent on adapting the technique to a wide range of surgeons: “With or without the Galloscope, the magic approach would still be the same.”11 Mühe soon moved on to the next step and operated through the trocar sleeve, without the optical instrument. The “magic” endoscopic approach remained untouched.12
Since a surgeon had no light source inside the abdominal cavity without the Galloscope, Mühe affixed a procto-scope light cable to the proximal trocar end. He recalled, “I then asked myself if any simple ‘open laparoscope’ could replace the trocar. ... Of course it could. In fact, I intended to affix a proctoscope light cable to any ‘open tube’ available in our hospital workshop.”13 (Figure 4)
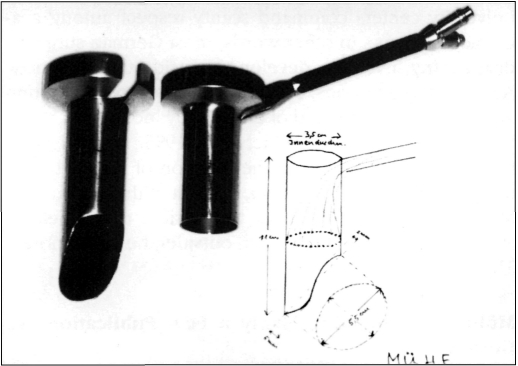
Figure 4.
“Open Laparoscope” according to Mühe (1986) was manufactured out of aluminum and vastly improved the light source by attaching a circular illumination to the distal end. Only once did Mühe present his “open tube with circular light,” at a CAES symposium held in October 1987. Fig. 12-10 in Highlights.
Mühe at the Congress of the German Surgical Society (GSS)
For a lecture on endoscopic cholecystectomy at the Congress of the German Surgical Society (GSS) in Munich, April 1986, Mühe prepared 42 slides.14 He took the first two from Semm's publications on an endoscopic resection of an ovarian cyst and a laparoscopic appendectomy. The next four showed the “Galloscope.” Mühe then presented 23 slides of his “open tube,” much to the amusement of his colleagues. In conclusion, he summarized the advantages of cholecystectomy without laparotomy in five main points:
1) Abdominal muscles are not cut,
2) Little postoperative pain,
3) Short immobilization,
4) Short postoperative hospitalization (4-5 days), and
5) Rapid return to the workplace.
The audience was skeptical of Mühe's claims.15 Most surgeons thought that operating through a small incision was dangerous. Mühe later had to deal with derogatory remarks such as “Mickey Mouse surgery” and “small brain—small incision.”
A Weak Response to Mühe's Lectures
Mühe did not achieve his hope for a breakthrough at the GSS congress. Only a handful of surgeons contacted him in the following months (among them, F. Hutterer of Cologne,16 H. Troidl of Cologne,17 and G. Wilkenau of Aachen18). In October 1986, Mühe gave a lecture at the annual meeting of the Lower Rhine-Westphalian Surgical Society held in Cologne.19 In the fall of 1987, he presented endoscopic cholecystectomy at a Symposium of CAES (Surgical Study Group on Endoscopy and Ultrasound) in Mainz.20 The response to Mühe's lectures was disappointingly weak.21 That same fall, Mühe was dealt another blow when the GSS failed to publish his lecture in its 1986 Proceedings. Only an abstract appeared, even though Mühe's talk had been one of the main features of the congress.22
By March 1987, Mühe had performed 97 endoscopic cholecystectomies.23
Reasons for the Rejection of Mühe's LC
1) “Big Surgeon—Big Incision”
Seen from today's perspective, it is difficult to understand why the German surgical world closed its eyes to Mühe's achievement. Perhaps one of the reasons is that abdominal surgery at that time was one of the few areas still largely untouched by the concept of “minimally invasive therapy.” The introduction of ever more sophisticated drugs, the impressive results of intensive care medicine, and advances in anesthesia together had led to the development of “major surgery.”24
Many leading abdominal surgeons had focused their attention on organ transplantation and cancer treatment. Abdominal operations were radical and extensive. The battle for higher five-year survival rates was in full swing, and countless new surgical techniques were published every year. “General surgical thinking was oriented to the concept that big problems required big incisions, and that incisions healed side to side, not end to end,” observed Michael S. Kavic of McKees Rocks, Pennsylvania.25 The idea that large problems require large incisions so deeply dominated surgical thinking in the 1980s that there was little room to appreciate the advances of “key-hole” techniques. Surgeons had little interest in modifying operations with low mortality rates, such as appendectomy and cholecystectomy.
2) Non-Surgical Treatment of Biliary Stones
In this context, it is important to emphasize another aspect of gallstone treatment, the non-surgical therapy of biliary calculi. Experiments and clinical alternatives for non-surgical treatment of biliary stones proliferated into the mid-1980s: clinical results with chenodeoxycholic acid (CDCA) (1972), ursodeoxycholic acid (UDCA) (1975), endoscopic papillotomy (1973), and, finally, mechanical lithotripsy of bile and common duct stones (1982).26 Expectations were high. Many believed that the era of effective chemical dissolution or lithotripsy was only a question of time.27 In light of such promising alternatives, little attention was paid to the development of surgical gallbladder removal.
3) The German Healthcare System
Perhaps more puzzling for the reader, especially in North America, is that German healthcare professionals were unmoved by the economic benefits of endoscopic cholecystectomies, such as rapid return to work. But the German healthcare system was not designed to accommodate such considerations; at that time, hospitals based their charges on the length of stay rather than the individual details of a patient's hospitalization!28 In short, the longer a patient was hospitalized, the more money the hospital received from the insurance company. Consequently, hospitals tended to keep surgical patients longer to cover operating costs.
Why were private surgeons in Germany not interested in laparoscopic cholecystectomy? Here, even greater differences exist between Germany and the United States. Private surgeons in Germany generally do not operate in hospitals. They refer patients who require surgery to the hospital, where residents or professors carry out the operation—nor do they have much say as to the preparation for the operation, type of surgery, or postoperative treatment.
4) The German University System
The traditional structure of German medicine is of course a reflection of the centralized decision-making process in European politics and education. As noted by a European social scientist, “The centralization of academic decision-making that is characteristic of European countries, it is argued, contrasts so sharply with the decentralization of academic decision-making in the U.S. that comparisons are not useful.”29 In this system, non-university centers command scanty respect among academic surgeons. In other words, most German surgeons distrust any invention developed outside the university. And, among surgeons, Mühe was not a recognized university expert in the field of endoscopy, not even a member of any endoscopic society. In 1995, Michael Jung, former senior physician in the Division of Endoscopy at the University of Heidelberg, gave a pithy account of Mühe's struggle: “Mühe was an outsider to the field of surgical endoscopy. And as an outsider, he was ignored. That's it.”30
Mühe's Shortcomings Only a Few Publications in German
During the 18 months of his clinical activity with the “Galloscope” and “open laparoscope,” Mühe held only three lectures, and demonstrated the method on an individual basis. This period stands in sharp contrast to his previous average of 30 publications a year. In recent statements, Mühe agrees that he was too intent on the German audience and underestimated the North American potential; in fact, he was a surgeon with deep German roots. Of his 342 publications between 1965 and 1983, only 7 percent appeared in English.31 In contrast to Semm, Mühe did not recognize the potential audience in North America for innovations.
Erich Mühe: A Surgeon Ahead of His Time
For Mühe, the technique of laparoscopic cholecystectomy was a logical step in the evolution of surgery, a further application of already-available technology. Today, Mühe's approach seems pragmatic and simple. In the heyday of “big surgeon—big incision” and pharmaceutical gallstone treatment, few people thought it would be necessary to alter gallbladder surgery. Mühe was an exception. While numerous surgeons were aware of the potential in gynecological laparoscopic surgery, only Mühe took the decisive step.
Perhaps the significance of Mühe's work is found in the fact that he could prepare the way for the introduction of laparoscopy into surgical practice. One wonders whether any individual would have been in a position to over-come the opposition in the German medical and social system of that time. It is not the first (nor the last) time in the history of medicine that the medical world has overlooked the work of a pioneering member (Figure 5).
Figure 5.
Mühe had to watch from the sidelines as others received credit for the laparoscopic “revolution.” First, on April 21, 1992, Mühe received official honors for pioneering work in endoscopic surgery. From right to left: Wittmoser, Mühe, Buess, Pier, and Götz at a opening ceremony of the 1992 Congress of the German Surgical Society. Fig. C-11 in Highlights.
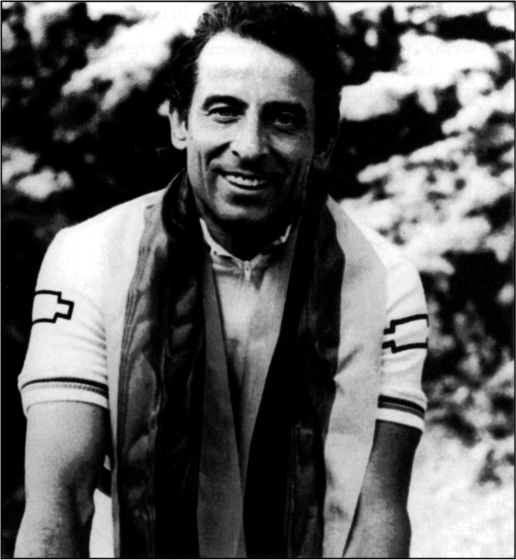
Laurence Olivier once listed three things necessary to a successful career: talent, luck, and stamina. He then said of luck: “Though this must vary, it must be good enough to believe in the truth of it yourself. You must see that it has provided you with the right opportunities at the right times.”32 Erich Mühe was graced by neither time nor place. He was a surgeon ahead of his time (Figure 6).
Figure 6.
“Biking gives me an intensive sense of life.” Erich Mühe is the 1985 German and the 1987 World Champion in a bike race for physicians. Fig. 12-17 in Highlights.
References:
- 1. Lux Endoscopic papillotomy. The development of a method. Endoscopy. 1978;10:206–208 [DOI] [PubMed] [Google Scholar]
- 2. Ibid.
- 3. Mühe E. Interview by GS Litynski, tape recording, December 4, 1995. In [33] [Google Scholar]
- 4. Semm K. Advances in pelviscopic surgery. In John M. Leventhal, ed. Current Problems in Obstetrics and Gynecology, Vol. V, Nr. 10. Chicago-London: Year Book Medical Publishers; 1982. The first publication on laparoscopic appendectomy appeared a year later: Semm K. Die endoskopische appendektomie. Gynäkol Prax. 1983;7:131–140 [Google Scholar]
- 5. Mühe E. Interview by GS Litynski. In [33] [Google Scholar]
- 6. WISAP (Gesellschaft für wissenschaftlichen Apparatebau mbH) Lieferschein [Shipping List], September 28, 1984. Transcript in hands of GS Litynski [Google Scholar]
- 7. Mühe E. Interview by GS Litynski. In [33] [Google Scholar]
- 8. Ibid.
- 9. Ibid.
- 10. Ibid.
- 11. Ibid.
- 12. Ibid.
- 13. Ibid.
- 14. Mühe E. Die erste Cholecystektomie durch das Laparaskop. 103. Kongress der Deutschen Gesellschaft für Chirurgie, München, 23.-26 April 1986. Manuscript not published. Transcript in hands of GS Litynski. “At the 1986 German Congress of Surgeons in Munich, I myself heard a paper by a Dr. Mühe where he presented the first cholecystectomy through a laparoscope. I do not know Dr. Mühe personally.” Garaguly G. Letter to Ch. Klaiber, January 20, 1994. Transcript in hand of GS Litynski [Google Scholar]
- 15. “I still recall very clearly your report at the Congress of Surgeons… You took a completely new path, for which … you were laughed at a bit.” Grill W. Letter to E. Mühe, February 19, 1993. Transcript in hand of GS Litynski.
- 16. As Hutterer's superior, Heinz Pichlmaier, of Cologne, wrote later to Mühe, Hutterer “gave a very positive report” on endoscopic cholecystectomy. Pichlmaier H. Letter to E. Mühe, November 24, 1986. Transcript in hand of GS Litynski.
- 17. Troidl H. Interview by GS Litynski, tape recording, October 11, 1995. In [33] [Google Scholar]
- 18. Winkeltau G. Letter to E. Mühe, May 21, 1986. Transcript in hand of GS Litynski. [Google Scholar]
- 19. Mühe E. Cholezystektomie ohne Laparotomie. 153. Tagung der Vereinigung Niederrheinisch-Westfällischer Chirurgen, Köln, October 9–11, 1986. Manuscript not published. Transcript in hand of GS Litynski [Google Scholar]
- 20. Mühe E. Endoskopische Cholezystektomie. 14. Symposium der Chirurgischen Arbeitsgemeinschaft Endoskopie und Sonografie, Mainz, October 9–11, 1987. Manuscript not published. Transcript in hand of GS Litynski [Google Scholar]
- 21. Mühe E. Interview by GS Litynski. [Google Scholar]
- 22. Mühe E. Die erste Cholecystektomie durch das Laparaskop. Langenbecks Arch Chir. 1986;369;804 “My paper on LC was one of the main lectures and consequently several hundred surgeons were in the hall, including most German university professors and numerous non-university heads of surgical clinics.” (Mühe E., Interview by GS Litynski) [Google Scholar]
- 23. Mühe E. Long-term follow-up after laparoscopic cholecystectomy. Endoscopy. 1992;24:754–758 [DOI] [PubMed] [Google Scholar]
- 24. Troidl H. Surgical endoscopy and sonography. Surgery at the crossroads. Surg Endosc. 1990;4:41–46 [DOI] [PubMed] [Google Scholar]
- 25. Kavic MS. Letter to GS Litynski, October 17, 1995. [Google Scholar]
- 26. Danziger R, Hofmann A, Schoenfield L. Dissolution of cholesterol gallstones by chenodeoxycholic acid. N Engl J Med. 1972;286:1-8. Classen M. Endoscopic papillotomy—new indications, short- and long-term results. Clin Gastroenterol. 1986;15:333–358 Demling L, Seuberth K, Riemann J. A mechanical lithotripter. Endoscopy. 1980;14:100-101 [DOI] [PubMed] [Google Scholar]
- 27. In 1986, W. Leuschner of Frankfurt/Main, Germany, an authority in the treatment of biliary calculi, commented on the development of this field: “There is no prospect of an end to this development. At present, ultrasound and electrohydraulic probes are under construction that can be placed near the stone under endoscopic guidance and then break it up. Lithotripsy by extracorporeal Shockwaves ... is about to be introduced into routine practice.” Leuschner W. Endosc Thr of Billiary Calculi Clin Gastroenterol. 1986;15:333–353 [PubMed] [Google Scholar]
- 28.Semm K. According to Semm, this system was one of the reasons for the slow acceptance of laparoscopic surgery in Germany. He noted, “I frequently received calls from the administrative director of the University Clinic. He would claim: 'We spent a lot of money on expensive endoscopic equipment and the patients leave the hospital only a day or two after surgery. Are you going to ruin us?'”. Interview by GS Litynski, tape recording, February 28, 1994. In [33]
- 29. El-Khawas E. The need for trans-Atlantic cooperation and exchange of concepts. In Teichler U, Wasser H. eds. German and American Universities. Mutual Influences—Past and Present. Kassel, Germany: Wissenschaftliches Zentrum fur Berufs—und Hochschulforschung der Gesamthochschule Kassel; 1992:57–66 [Google Scholar]
- 30. Jung M. Interview by GS Litynski, tape recording, March 29, 1996. [Google Scholar]
- 31. Mühe E. Curriculum Vitae. Transcript in hand of GS Litynski. [Google Scholar]
- 32. Olivier L.Confession of an Actor. London, England: Simon and Schuster; 1982 [Google Scholar]
- 33. Litynski GS.Highlights in the History of Laparoscopy. Frankfurt/Main, Germany: B. Bernert Verlag; 1996 [Google Scholar]