Abstract
Background and Objectives:
Morgagni hernias are unusual congenital diaphragmatic hernias that are generally asymptomatic and discovered incidentally. Surgical treatment is indicated once the diagnosis is made. These hernias have traditionally been repaired by the open abdominal or thoracic approaches. We report a case of Morgagni hernia repaired successfully via the laparoscopic approach.
Methods and Results:
The patient was noted to have a large anteromedial diaphragmatic hernia by chest radiograph and CT imaging. He underwent laparoscopy, during which the hernia was reduced and the defect repaired with mesh placement. We used intracorporeal suture placement to anchor the mesh. The patient recovered uneventfully after a short hospitalization.
Conclusions:
The laparoscopic approach for repair of Morgagni hernias offers diagnostic advantages as well as the potential for reduced morbidity when compared to laparotomy. We report intracorporeal knot-tying for fixation of the mesh to be a secure and satisfactory means to achieve the laparoscopic repair.
Keywords: Morgagni hernias, Laparoscopy
INTRODUCTION
Congenital diaphragmatic hernias (CDH) are rare congenital defects in which the abdominal contents herniate through a diaphragmatic defect into the chest cavity. There are four different types of CDH: 1) anterolateral hernia; 2) posterolateral or Bochdalek hernia; 3) pars sternalis; and 4) anteromedial or Morgagni hernia. The Morgagni hernia is one of the least common hernias, accounting for 3% of all diaphragmatic hernias.1 It often remains asymptomatic and is discovered incidentally on chest X-ray. Surgical treatment is indicated once the diagnosis has been made. Traditionally, the preferred operation is the abdominal approach where the contents can be reduced and the defect closed by direct suturing. Others have advocated the thoracic approach by open or thoracoscopic techniques.2 We report a case of successful laparoscopic repair of a Morgagni hernia with a placement of Marlex mesh. We applied advanced techniques of minimally invasive suturing to achieve satisfactory intracorporeal repair of this difficult hernia. Laparoscopic operations allow earlier return to physical activity and frequently result in reduced postoperative pain.
CASE REPORT
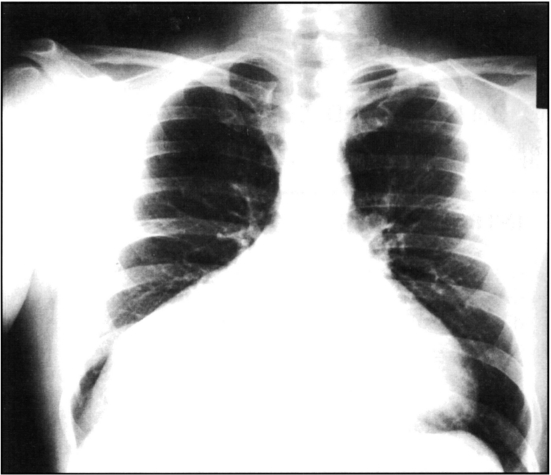
The patient is a 38-year-old Caucasian male with a 17-year history of schizophrenia, who was admitted to Harbor-UCLA Medical Center for an exacerbation of his schizophrenia. Chest radiograph revealed a right lower lung field mass with fluid collected in the right minor fissure (Figure 1). The patient denied shortness of breath, pleuritic chest pain, or gastrointestinal symptoms; however, he reported occasional non-productive cough and exercise intolerance for the past six months. He was unable to run farther than 300 yards without feeling tightness in his chest.
Figure 1.
Chest radiograph demonstrating an enlarged mediastinum and a right lower lung field mass.
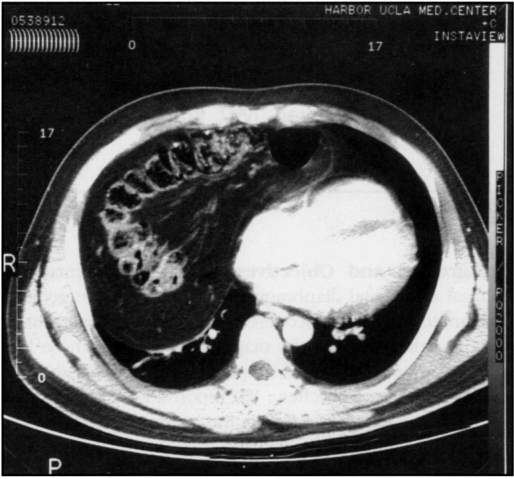
Physical examination was unremarkable except for increased dullness to percussion at the right lung base. CT scan of the chest showed the transverse colon entering the right chest via an anteromedial defect of the diaphragm (Figure 2). The patient was taken to the operating room for laparoscopy. The colon was reduced into the abdomen, the hernia sac excised, and the defect was repaired laparoscopically with a 5 × 6 cm Marlex mesh patch using 2-0 prolene suture (Figure 3). The patient subsequently did well and was discharged home three days postoperatively without complication. His chest x-ray following surgery was normal (Figure 4).
Figure 2.
CT scan of the chest showing the transverse colon entering the chest from the anteromedial region of the diaphragm.
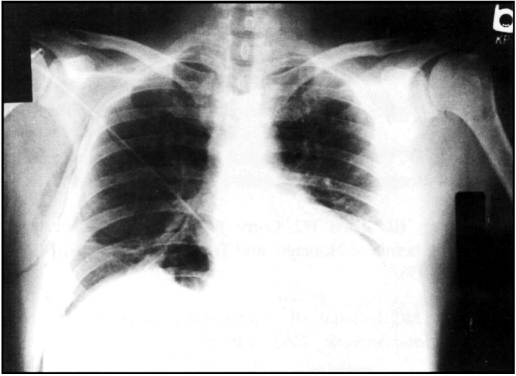
Figure 4.
Postoperative chest radiograph confirming repair of the hernia.
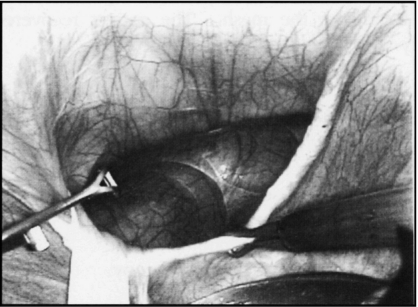
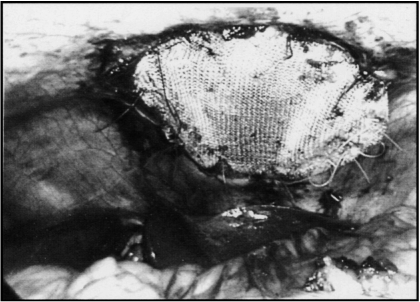
Figure 3.
3a. The operative appearance of the transverse colon within the diaphragmatic defect.
3b. The large hernia defect after the contents are reduced.
3c. The application of the mesh to cover the defect after the peritoneal sac has been removed with cautery.
3d. The finished repair using interrupted sutures circumferentially to affix the mesh.
DISCUSSION
Embryologically, the diaphragm is derived from four components:3 1) the anterior central tendon of the septum transversum, 2) dorsolateral portions of the pleuroperitoneal membranes, 3) dorsal crura from esophageal mesentery, and 4) lateral slips of costal muscle groups. The integrity of the diaphragm occurs after the fusion of the above four components with the posterolateral portion being the last part to be incorporated. Failure of the fusion of the par costalis and pars sternalis of the septum transversum leads to the development of a defect and the potential of an anteromedial (Morgagni) hernia. It has been reported to be associated with other congenital defects such as Down's syndrome, Turner's syndrome, Prader Willi syndrome, Tetralogy of Fallot, ventricular septal defect and omphalocele.4,5 Although no report has documented that the failure of fusion is the result of a genetic defect, Harris4 suggested it is an inherited defect based on concordance studies in twins.
The anteromedial hernia was first described by Morgagni in 1760. Others have previously referred to it as a Larrey hernia. However, Larrey (1829) never described the hernia, rather he only developed the surgical approach to the pericardial cavity.6 Morgagni hernias occur primarily to the right of the sternum.7 However, 20% may occur on the left.7 Almost all Morgagni hernias have a well-developed peritoneal sac with communication into the thoracic cavity. The abdominal organs most commonly found in the sac in order of decreasing frequency are colon, omentum, stomach, liver, and small bowel.4
The Morgagni hernia can present in the new born period with respiratory distress, but it usually remains asymptomatic until later in life when it is noted incidentally on chest X-ray. If present, the symptoms are usually related to the contents of the hernia sac.7 When the sac contains bowel, the patient may present with abdominal pain or intestinal obstruction. If the size of the sac is large enough, the contents may compress the intra-thoracic structures and produce respiratory symptoms such as coughing, dyspnea and retrostenal pain.7
Although physical examination of the chest may reveal auscultatable bowel sounds or dullness to percussion, the diagnosis is invariably made by radiological means. Chest X--rays provide sufficient evidence for a diagnosis in most cases. Lateral films are essential because they show the lesion, haustration of colon, or other gas patterns in the anterior pericardiophrenic angle. Barium enema is a useful diagnostic test when the colon is herniated and the presentation is that of a large bowel obstruction. CT scan is the most helpful study to differentiate a Morgagni hernia from other mediastinal processes. Esophagography, bronchoscopy, lung scan and angiogram are of little value.7
Surgical repair is mandatory once the diagnosis is made since strangulation or incarceration of any contained viscera can occur. Repair has traditionally been performed either via a transthoracic or transabdominal approach.8 The abdominal approach is advantageous for patients with complex hernias because both the hernia and the trapped viscus can easily be addressed. Transthoracic operation is generally preferred when a definite preoperative diagnosis cannot be made in patients with an indeterminate anterior pericardial mass.9–17
Three previous case reports18–20 have advocated the use of laparoscopic techniques to repair the Morgagni hernia. Kuster18 described direct repair of a Morgagni hernia laparoscopically, using extracorporeally tied sutures through separate incisions. Rau19 used a stapled Marlex mesh patch to close a Morgagni hernia laparoscopically in a technique similar to transabdominal laparoscopic inguinal herniorraphy. Newman20 reported three cases of laparoscopic repair of Morgagni hernias, employing a Keith needle for suturing. His sutures were also tied extracorporeally via separate skin incisions. In contrast to the previously reported studies, we sutured the mesh in place intracorporeally without separate skin incisions. Visualization was enhanced with a 30° viewing scope. We laparoscopically reduced the hernia and estimated the extent of the defect. We excised the sac and covered the defect with a Marlex mesh patch. The hernia defect was too large for primary repair. The closure was facilitated with a laparoscopic suturing device (US Surgery Corp). To enhance security, the sutures were placed in an interrupted fashion (Figure 3).
CONCLUSION
The laparoscopic approach for repair of Morgagni hernias offers diagnostic advantages as well as the potential for reduced morbidity when compared to laparotomy or thoracotomy. Confirming the diagnosis of Morgagni hernia during the evaluation of an indeterminate mediastinal mass is made easily with the use of the laparoscope. Our report shows that excision of the sac and closure of the hernia defect with placement of a mesh sheet can be performed satisfactorily, intraabdominally without the need for separate skin incisions. The laparoscopic approach allows excellent access to the diaphragm utilizing minimal incisions. It also can result in reduced postoperative pain and an earlier return to physical activity.
References:
- 1. Thomas V. Thomas. Subcostostemal diaphragmatic hernia. Thor Cardio Surg. 1972;63:279–283 [PubMed] [Google Scholar]
- 2. Akamine S, Kawahara K, Nakamura A, Takahashi T, Yamamoto S, Ayabe H, Tomita M. Successful utilization of a video-assisted thoracic approach to repair Morgagni's hernia: Report of a case. Surg Today. 1995;25:654–656 [DOI] [PubMed] [Google Scholar]
- 3. Butler MW, Stolan JHC, Altman RP. Contemporary management of congenital diaphragmatic hernia. World J Surg. 1993;17:350–355 [DOI] [PubMed] [Google Scholar]
- 4. Harris JG, Super TR, Kimura KK. Foramen of Morgagni hernia in identical twins: Is this an inheritable defect? J Fed Surg. 1993;28:177–178 [DOI] [PubMed] [Google Scholar]
- 5. Sinclair L, Klein LB. Congenital diaphragmatic hernia— Morgagni Type. J Emerg Med. 1993;11:163–165 [DOI] [PubMed] [Google Scholar]
- 6. Paris F, Tarazona V, Casillas M, Blaseo E, Canto A, Pastor J, Acosta A. Hernia of Morgagni. Thorax. 1973;28:631–636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wolloch Y, Grunebaum M, Glanz I, Dintsman M. Symptomatic retrostenal (Morgagni) hernia. Am J Surg. 1974;127:601–605 [DOI] [PubMed] [Google Scholar]
- 8. Saha PS, Mayo P, Graydon AL. Surgical treatment of anterior diaphragmatic hernia. Southern Med J. 1982;75:280–281 [DOI] [PubMed] [Google Scholar]
- 9. Chin EF, Duchesne ER. Parasternal defect. Thorax. 1955;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Comer TP, Clagett OT. Surgical treatment of hernia of the foramen of Morgagni. J Thor Cardio Surg. 1966;52:461–468 [PubMed] [Google Scholar]
- 11. Honore HL, Torfs PC, Curry JRC. Possible association between the hernia of Morgagni and Trisomy 21. Am J Med Gen. 1993;47:255–256 [DOI] [PubMed] [Google Scholar]
- 12. Moreno MC, Iovanne AB. Congenital diaphragmatic hernia: Part I. Neonatal Network. 1993;12:19–25 [PubMed] [Google Scholar]
- 13. Zaglul FH, Odita CJ. Multiple herniae: A defect in the celomic mesoderm? Am J Med Gen. 1995;57:537–535 [DOI] [PubMed] [Google Scholar]
- 14. Fotler R, Schirupl G, Sorantin E, Fritz K, Landler U. Delayed presentation of congenital diaphragmatic hernia. Pediatric Rad. 1992;22:187–191 [DOI] [PubMed] [Google Scholar]
- 15. Torfs PC, Curry FRC, Bateson FT, Honore HL. A population-based study of congenital diaphragmatic hernia. Tetralogy. 1992;46:555–565 [DOI] [PubMed] [Google Scholar]
- 16. Sekiguchi Y, Shimura S, Takishima T. Intrapleural omentum simulating pleural effusion. Chest. 1994;106:285–287 [DOI] [PubMed] [Google Scholar]
- 17. Smith J, Ghani A. Morgagni hernia: Incidental repair during laparoscopic cholecystectomy. Laparosc Surg. 1995;5:123–125 [DOI] [PubMed] [Google Scholar]
- 18. Kuster G, Kline L, Garzo G. Diaphragmatic hernia through the foramen of Morgagni: Laparoscopic repair case report. J Laparosc Surg. 1992;2:93–100 [DOI] [PubMed] [Google Scholar]
- 19. Rau H, Schardey H, Lange V. Laparoscopic repair of a Morgagni Hernia. Surg Endosc. 1994;8:1439–1442 [DOI] [PubMed] [Google Scholar]
- 20. Newman L, Eubank S, Briges W, Lucas G. Laparoscopic diagnosis and treatment of Morgagni Hernia. Surg Laparosc Endosc. 1995;5:27–31 [PubMed] [Google Scholar]