Abstract
Background and Objectives:
To compare the use of patient-controlled analgesia to intermittent intramuscular injections of morphine following major gynecological laparoscopic procedures in order to assess differences in level of pain, sedation, episodes of nausea and/or vomiting, hospitalization time and patient satisfaction with their postoperative analgesia.
Methods:
Seventy-two patients undergoing major gynecological laparoscopic surgery were randomized to receive either postoperative analgesia via intermittent intramuscular injection of morphine (Group 1) or patient controlled analgesia (PCA - Group 2). All patients received anesthesia via a standardized protocol. Postoperative pain levels were recorded via a 10 cm visual analogue scale, and sedation scores were recorded on a standard PCA form. Episodes of nausea and vomiting were also recorded on the same form.
Results:
There were no statistically significant differences between intramuscular analgesia and PCA for any of the factors studied. Most significantly it was found that most patients ceased to require either form of parenteral analgesia within 24 hours of their procedure, regardless of the operating time.
Conclusion:
It is important for the surgeon to be aware of the effects of postoperative analgesia on his or her patients' level of satisfaction. We do not recommend the use of PCA analgesia following major laparoscopic gynecological surgery.
Keywords: PCA, Laparoscopy, Postoperative analgesia
INTRODUCTION
Regardless of the skill and expertise of the laparoscopic surgeon, few patients have any understanding of the operative procedure and judge their surgical experience largely on their level of postoperative pain and recovery time. Accordingly, it is of great importance to the surgical team that the method of postoperative analgesia utilized leads to greatest patient satisfaction.
The use of patient controlled analgesia (PCA) in the immediate postoperative period has been shown to provide constant levels of opioid analgesia to the patient with reduced sedation and a level of pain relief at least equivalent to that provided by standard intramuscular injections.1,2 In our institution, however, nursing staff have reported an observed association between the use of PCA and increased levels of nausea and vomiting and prolonged postoperative recovery and mobilization times. Among the reported advantages of laparoscopic surgery, the provision of surgical services with minimal levels of postoperative pain and speedier recovery are of great import.3 To ascertain the true effect of the type of analgesia administered on postlaparoscopy pain, sedation, episodes of nausea and vomiting and patient recovery time, a randomized prospective study was conducted.
METHODS
Calculation of power required to show a significant difference (p<0.05) between groups was performed prior to the commencement of the study. Seventy-two consecutive patients (36 in each group) undergoing major gynecological laparoscopic surgery by one of four surgeons at four local hospitals—Hurstville Community Hospital, St. George Private and Public Hospitals and Strathfield Private Hospital--were included in this study. All patients were preoperatively randomized to receive either intramuscular analgesia (Group 1) or PCA (Group 2) in the postoperative period and were counseled preoperatively by the anesthetist involved regarding the nature of analgesia to be used. As the study was designed to maximize postoperative patient comfort, no attempt was made to control for anti-emetic usage. Furthermore, OR nursing staff were not blinded to the type of analgesia used.
The study was approved by the ethics committees of each hospital involved. Contraindications to PCA included a history of opioid dependence or major postoperative complications; however, none of the patients were excluded for this, or any other reason. The method of analgesia was not altered in any case.
Oral temazepam was given to those patients requiring premedication; no patient received opioid premedication. Anesthesia commenced with a combination of Midazolam 2 mg, Droperidol 0.8 mg, Fentanyl 100 μg and Ondansetron 4 mg prior to entering the operating theatre. Following preoxygenation, propofol infusion was commenced and maintained at 8 mg/kg throughout the procedure and ventilation with O2/air, FiO2 0.40-0.45. Relaxation was achieved with Mivacurium 0.3 mg/kg/hr following an initial bolus. In addition to the initial dose of Fentanyl, all patients received at least 10 mg of morphine early in the procedure, with up to 5 mg in increments later in the procedure if required. They all received 5000 units Fragmin and 1g of a broad-spectrum cephalosporin intraoperatively.
All patients received 5 mL of local anesthetic injected into all skin wound sites and insertion of a rectal suppository of Indomethacin (100 mg) at the conclusion of the procedure. They each received up to 10 mg morphine intravenously in the recovery ward on awakening for control of immediate postoperative pain. Recorded observations were kept hourly for the first 12 hours and every two hours thereafter. Intramuscular injections of 7.5-10 mg morphine were administered to patients in Group 1, while the PCA regimen consisted of a 1.5 mg morphine bolus with a 5 minute lockout period. Doses of anti-emetic administered (chlorpromazine 12.5 mg or metoclopramide 10 mg imi) were also recorded as well as episodes of nausea and/or vomiting.
Patients in both groups had pain scores recorded on a 10 cm visual analogue scale, and sedation scores recorded by nursing staff on standardized PCA forms (score of 0 as asleep and 4 fully alert). Finally, all patients recorded a score of 1 to 5 regarding their satisfaction with postoperative analgesia--1 being most satisfied.
Results were analyzed via the Winks (4.1c professional edition statistical package) using non-Parametric statistical analysis (ANOVA) for determination of variance between groups, and correlation analysis for determination of the relationship between morphine dose and inpatient stay.
RESULTS
There were no statistically significant differences between groups for demographic data (Table 1). All but eight patients in each group had undergone some form of surgery previously, while many patients had more than one previous surgical procedure (Table 2). Table 3 details the major surgical procedure undertaken, showing that many patients underwent more than one procedure at the same operation.
Table 1.
Demographic data.
| Group 1(intramuscular) n=36 | Group 2(PCA) n=36 | |
|---|---|---|
| Age (average) | 52 years | 49 years |
| Weight (average) | 72.0 kg | 71.4 kg |
| Stay (average) | 72 hours | 89 hours |
| ASA score (average) | 1.5 | 1.4 |
| No previous surgery | 8 | 8 |
Table 2.
Previous surgery.
| Type of operation | Group 1 (n=36) | Group 2 (n=36) |
|---|---|---|
| Abdominal Hysterectomy | 6 | 6 |
| Appendicectomy | 8 | 9 |
| Caesarean | 1 | 1 |
| Cholecystectomy | 4 | 4 |
| Colposuspension | 2 | 4 |
| Laparoscopy | 11 | 14 |
| Laparotomy | 4 | 2 |
| Vaginal Hysterectomy | 1 | 3 |
| Vaginal Repairs | 5 | 8 |
Table 3.
Current Surgery
| Type of operation | Group 1 | Group 2 |
|---|---|---|
| Laparoscopic Hysterectomy | 17 | 10 |
| Laparoscopic Colposuspension | 11 | 22 |
| Adhesiolysis | 10 | 9 |
| Laparoscopic pelvic floor repair | 9 | 14 |
| Ovarian cystectomy/endometriosis | 3 | 2 |
N.B. 20 patients in group 1 and 21 in group 2 had multiple procedures.
Sixteen patients in Group 1 had postoperative catheterization (9 suprapubic catheters, 7 urethral catheters) and four patients had an intra-abdominal drain. These were removed at an average of 34 hours. Twenty-five patients in Group 2 had postoperative catheterization (19 suprapubic, 6 urethral; average duration 31 hours) and only one drain which was removed the morning following surgery. Average operating time was 126 minutes in Group 1 and 113 minutes in Group 2. There were three cases complicated by severe adhesions in the first group and four in the second group. One patient in Group 2 also suffered a respiratory arrest in recovery; however, she remained able to use her PCA machine in the intensive care unit. None of these comparisons reached a statistically significant level of difference.
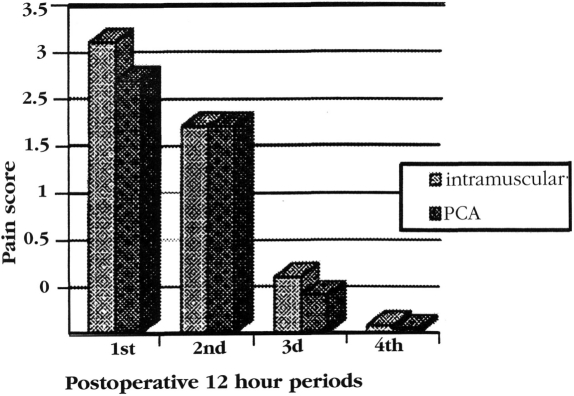
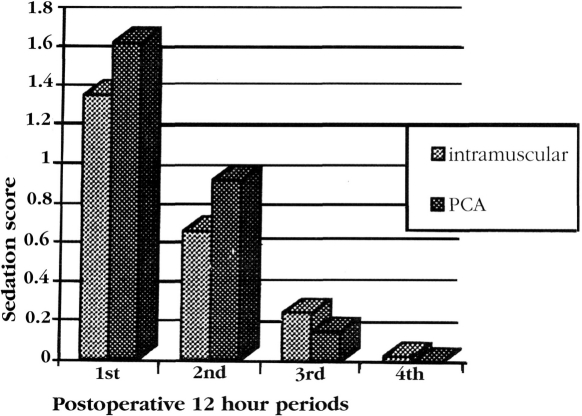
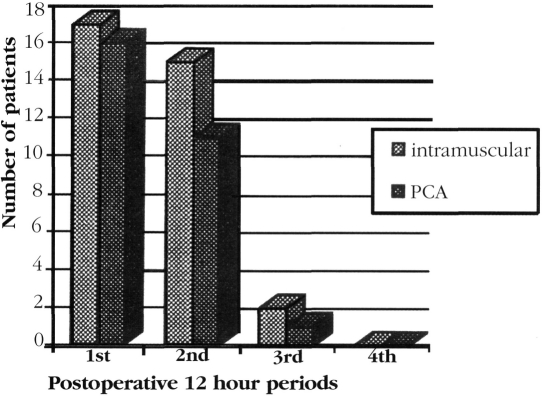
There were no statistically significant differences found in any postoperative period for either pain level or sedation (Figures 1 and 2). Similarly, there were no statistically significant differences in the number of patients suffering from nausea and/or vomiting (Figure 3). Average dose of morphine administered was 18.8 mg in Group 1 and 21.7 mg in Group 2. This difference was not significant.
Figure 1.
Postoperative pain
Figure 2.
Postoperative sedation score.
Figure 3.
Reported episodes of Nausea and/or Vomiting.
Comparison of sedation scores between those patients administered chlorpromazine and those administered metoclopramide showed no significant difference. Mean time to discharge was 72 hours in Group 1 and 89 hours in Group 2. This difference did not reach the level of statistical significance and can be accounted for by the slightly higher number of patients having laparoscopic colposuspension in Group 2. These patients are often hospitalized for a slightly longer duration until the return of normal bladder function. Furthermore, no correlation was found to exist between morphine dose administered and duration of inpatient stay (p=0.9).
Twenty five patients reported a high level of satisfaction with their pain/sedation control in Group 1 (eight reported a satisfaction rating of 2/5, one of 3/5 and two of 4/5). In Group 2, 28 patients reported a satisfaction rating of 1/5 (two a rating of 2/5, two of 3/5 and four a rating of 4/5). These differences were not statistically significant.
DISCUSSION
The form of postoperative analgesia used after gynecological laparoscopic surgery is often a decision made entirely by the anesthesia staff. Yet, postoperative pain and time to recovery are important factors in an individual patient's assessment of his or her surgical experience. It is, therefore, most important that laparoscopic surgeons are aware of the method of analgesia used for their patients and the effects of that method. The advantages of PCA versus standard intermittent intramuscular analgesia for the control of postoperative pain have previously been reported in the medical literature.4 The theory supporting this technique is the provision of a more constant level of analgesia compared with documented fluctuations in opioid concentration in the blood after intramuscular administration. These studies hold the view that PCA provides at least as effective pain control with reduced sedation.1,2,5,6 Furthermore, it has been shown that interindividual analgesic requirement is highly variable and that PCA allows patients to control their own analgesia, with reduced chance of overdosageand, it is postulated, reduced resultant recovery time, including faster return to mobility and bowel motility.2
However, conflicting results exist. Snell et al. could not demonstrate a statistically significant advantage of PCA over intermittent intramuscular injections of morphine in 73 patients following major abdominal surgery, in terms of postoperative pain, amount of analgesia used, patient satisfaction or hospital stay.7 In our institution there existed a belief amongst health workers involved in the postoperative management of laparoscopic gynecological surgery patients that those receiving analgesia via a PCA machine suffer more nausea and vomiting with slower recovery time compared with patients receiving intermittent intramuscular injections, on the same postoperative ward. One of the major advantages of laparoscopic surgery to the patient is the more rapid recovery time and speedier discharge from the hospital. Among the reasons for this is reduced postoperative pain from the procedures themselves, a combination of reduced wound pain and minimal tissue handling. Accordingly, it is postulated that postoperative analgesia requirements following laparoscopic surgery, no matter how extensive the procedure, are reduced--thus obviating the need for PCA.
Our results support this contention. There was no significant difference in the postoperative pain level recorded between the group of patients receiving intermittent analgesia and those using a PCA machine. This occurred despite lengthy average surgical time with 20 patients in Group 1 and 21 patients in Group 2 having more than one procedure at the same operation. In fact, few patients required use of the PCA machine, or indeed further intramuscular opioid, after the initial 24 hours following their procedure, with one patient in the PCA group and seven in the intermittent intramuscular analgesia group not using parenteral analgesia at all. This may be explained by the accessibility of the PCA machine to the patient as well as a possible reticence to undergo further intramuscular injections. A potential bias, in terms of higher pain scores for the intramuscular group, was, however, not detected statistically.
Similarly, sedation levels were similar between groups for each period studied. As few patients required their PCA longer than 24-36 hours, it is unlikely that it had any impact on duration of inpatient stay--although this was clinically, if not statistically, slightly lengthened in Group 2. Certainly there was no correlation detected between the amount of morphine used per patient and the duration of inpatient stay. We do, however, acknowledge that the anesthetic protocol used, namely the use of preoperative ondansetron, intraoperative Fentanyl and morphine, postoperative nonsteroidal anti-inflammatory agents and wound infiltration with local anesthetic, may reduce the levels of postoperative nausea and vomiting. The regimen was utilized in all cases and, therefore, could be expected to affect both groups equally. We also acknowledge that not blinding nursing staff to the form of analgesia used may have altered nursing response time and, therefore, biased patient satisfaction.
Patient reticence to utilizing analgesic agents has been documented8 and depends largely on attitudes to opioids and preoperative expectation of pain. Indeed, it has been shown that increased patient education can result in greater use of these agents in the postoperative period and subsequent reduced levels of pain. While pain levels in the current study may have been influenced by patient attitudes (despite preoperative anesthetic counseling), it is assumed this would have impacted equally on both groups.
As a historical comparison to studies of analgesia following gynecological abdominal surgery, the laparoscopic approach compares favorably. In comparison to a similar study of open gynecological surgery,2 average total morphine doses in the laparoscopic group of patients in either arm (21.9 mg in Group 1, 18.5 mg in Group 2) were considerably less than comparable figures for the open surgery groups receiving either PCA or intermittent intramuscular analgesia (109.8 mg and 117.0 mg respectively).
It is of interest to note that, despite anecdotal reports to the contrary, episodes of nausea and/or vomiting were slightly greater in the first 24-hour period in the group of patients using intermittent intramuscular analgesia-although, again, this difference was not statistically significant. While the type of anti-emetic was not controlled and, therefore, a potential source of bias, no significant difference was found between sedation scores for those patients administered chlorpromazine and those given metoclopramide in either group.
CONCLUSION
We have found that the levels of analgesia, sedation and episodes of nausea and vomiting provided by patient controlled analgesia following major laparoscopic gynecological surgery is not significantly different to that provided by intermittent intramuscular administration of opioid, nor does it have any significant difference on time to discharge. While PCA analgesia may give patients greater control over their own pain, we have found that laparoscopic gynecological surgery is not associated with high levels of postoperative discomfort, and most patients are able to avoid parenteral analgesia after the first 24 hours following their surgery. These results suggest that a study comparing parenteral with oral postoperative analgesia following major laparoscopic surgery is timely and indeed is currently being addressed at this institution.
Acknowledgments:
The authors would like to thank Dr. M. Henderson, Dr. R. Ng, Dr. N. Robson and Dr. A. Schimmelfeder for their agreement to use the standard anesthetic protocol for all patients. We would also like to gratefully acknowledge the contribution of Sr. V. Irving, Sr. M. Gane and Sr. C. Clarke for their help in data collection and the nursing staff of the postoperative wards of Hurstville Community Hospital, St. George Private and Public Hospitals and Strathfield Private Hospital.
References:
- 1. Colwell CW, Morris BA. Patient-controlled analgesia compared with intramuscular injection of analgesics for the management of pain after an orthopaedic procedure. J Bone Joint Surg. 1995;77-A:726–733 [DOI] [PubMed] [Google Scholar]
- 2. Wasylak TJ, Abbot FV, English MJM, Jeans M. Reduction of postoperative morbidity following patient-controlled morphine. Can J Anaesth. 1990;37:726–731 [DOI] [PubMed] [Google Scholar]
- 3. Rosen DMB, Cario GM. Return to work following laparoscopic hysterectomy. doi: 10.1016/s1074-3804(96)80280-5. In press. [DOI] [PubMed] [Google Scholar]
- 4. Ferrante FM, Orav JE, Rocco AG, Gallo J. A statistical model for pain in patient-controlled analgesia and conventional intramuscular opioid regimens. Anesth Analg. 1988;67:457–461 [PubMed] [Google Scholar]
- 5. Albert JM, Talbott TM. Patient-controlled analgesia vs. conventional intramuscular analgesia following colon surgery. Dis Colon Rectum. 1988;31:83–86 [DOI] [PubMed] [Google Scholar]
- 6. Dahl JB, Daugaard JJ, Larsen HV, Mouridsen P, Nielsen TH, Kristoffersen E. Patient-controlled analgesia: a controlled trial. Acta Anaesthesiol Scand. 1987;31:744–747 [DOI] [PubMed] [Google Scholar]
- 7. Snell CC, Fothergill-Bourbonnais F, Durocher-Hendriks S. Patient controlled analgesia and intramuscular injections: a comparison of patient pain experiences and postoperative outcomes. J Adv Nurs. 1997;25:681–690 [DOI] [PubMed] [Google Scholar]
- 8. Wilder-Smith CH, Schuler L. Postoperative analgesia: pain by choice? The influence of patient information and patient education. Pain. 1992;50:257–262 [DOI] [PubMed] [Google Scholar]