Abstract
Background and Objectives:
To compare laparoscopic appendectomy with traditional open appendectomy.
Methods:
Seventy-one patients requiring operative intervention for suspected acute appendicitis were prospectively compared. Thirty-seven patients underwent laparoscopic appendectomy, and 34 had open appendectomy through a right lower quadrant incision. Length of surgery, postoperative morbidity and length of postoperative stay (LOS) were recorded. Both groups were similar with regard to age, gender, height, weight, fever, leukocytosis, and incidence of normal vs. gangrenous or perforated appendix.
Results:
Mean LOS was significantly shorter for patients with acute suppurative appendicitis who underwent laparoscopic appendectomy (2.5 days vs. 4.0 days, p<0.01). Mean LOS was no different when patients classified as having gangrenous or perforated appendicitis were included in the analysis (3.7 days vs. 4.1 days, P=0.11). The laparoscopy group had significantly longer surgery times (72 min vs. 58 min, p<0.001). There was no significant difference in the incidence of postoperative morbidity.
Conclusions:
Laparoscopic appendectomy reduces LOS as compared with the traditional open technique in patients with acute suppurative appendicitis. The longer operative time for the laparoscopic approach in our study is likely related to the learning curve associated with the procedure and did not increase morbidity.
Keywords: Laparoscopy, Appendectomy
INTRODUCTION
Several reports have demonstrated that laparoscopic appendectomy is technically feasible in the management of acute appendicitis.1–10 Proponents of the procedure have claimed that it offers several advantages over the traditional open appendectomy through a right lower quadrant muscle splitting incision. However, the data concerning any superiority of the laparoscopic technique have not been entirely clear. To further evaluate this procedure, we prospectively compared patients undergoing laparoscopic versus traditional open appendectomy.
MATERIALS AND METHODS
We examined our experience with laparoscopic and open appendectomies for acute appendicitis during a 24-month interval. Surgical technique in each case was determined by individual surgeon preference and the availability of laparoscopy equipment. Patients who were not considered candidates for laparoscopic appendectomy were excluded from analysis and included pregnant women, patients with a palpable mass in the right lower quadrant (presumably representing a large phlegmon or abscess), and patients with diffuse peritonitis.
Thirty-seven patients underwent laparoscopic appendectomy, and 34 patients underwent traditional open appendectomy. The two patient groups were similar with regard to age, gender, height, weight, fever, and leukocytosis. The number of patients pathologically classified as having acute appendicitis versus gangrenous or perforated appendicitis were also similar.
Open appendectomies were performed through traditional transverse, right lower quadrant, muscle splitting incisions. The mesoappendix was serially ligated with 3-0 vicryl suture. The base of the appendix was doubly suture ligated with 0-chromic and then cauterized to prevent lymphocele. The right lower quadrant was irrigated with 500 cc of normal saline. The peritoneum and internal oblique fascia were closed with a running 0-vicryl suture as one layer separately from the external oblique fascia; scarpa's fascia was closed with a running 3-0 vicryl suture. The skin was closed with staples.
Laparoscopic appendectomy was approached by a three trocar technique with the addition of a fourth trocar when necessary. Usually, a 10 mm port was placed at the umbilicus for the camera, a 12 mm port was placed in the suprapubic area, and another 10 mm port was placed in the right upper quadrant. When needed, a 5 mm or 10 mm port was placed in the left lower quadrant. The mesoappendix was transected using clips, ligatures, or an EndoGIA stapling and cutting device (United States Surgical Corporation, Norwalk, CT). The appendiceal stump was controlled with ligatures or an EndoGIA staple line.11 The appendix was removed through the 12 mm port directly or after insertion into a bag. If the procedure could not be safely completed laparoscopically, the surgeon converted to an open procedure. These converted patients were included in the laparoscopy group for the subsequent analysis on an intent-to-treat basis.
Surgical residents participated in nearly all cases in the roles of both “surgeon” and “first assistant.” All attending surgeons and surgical residents had extensive prior experience with laparoscopic cholecystectomy.
Postoperative pain was controlled by varying parenteral and oral regimens at the discretion of the physician. Patients were discharged when they were afebrile for 24 hours and tolerating a regular diet.
Measurements of patient characteristics and illness severity included age, gender, height, weight, fever, leukocytosis, and appendiceal findings by pathology. Total operating room time was measured from time of patient entrance into the room to time of exit. Surgery time was measured from skin incision to skin closure. Postoperative hospitalization was measured from date of surgery to date of discharge. Postoperative pain control was evaluated by counting the number of administered analgesic doses.
An unpaired Student's t-test was used to assess differences between the groups.
RESULTS
In the laparoscopy group, 31 patients had appendectomy completed laparoscopically; one had a normal appearing appendix left intact (there was a clear diagnosis of pelvic inflammatory disease), and five (14%) had conversion to open appendectomy (Table 1). In four of the conversions, extensive adhesions and phlegmon precluded safe laparoscopic dissection. These four patients all had a gangrenous or perforated appendix. A fifth conversion was due to dense adhesions from prior surgery and an inadvertent enterotomy. All patients in the open group had the appendix removed.
Table 1.
Results of laparoscopic versus open appendectomy.
| Laparoscopic | Open | p-value | |
|---|---|---|---|
| Total Patients | 37 | 34 | - |
| Converted to Open | 5 (13.5%) | N/A | - |
| Acute Suppurative Appendicitis | 24 (64.9%) | 23 (67.6%) | P > 0.05 |
| Surgery Time (min) | 72 | 53 | P < 0.001 |
| Total OR Time (min) | 119 | 85 | P < 0.001 |
| # Wounds Packed Open | 3 (8.1%) | 11 (32.4%) | - |
| Postop Narcotic Doses per Day | 1.9 | 2.0 | P > 0.05 |
| Postop Analgesic Doses per Day | 2.1 | 2.1 | P > 0.05 |
| Complications | 4 (10.8%) | 4 (11.8%) | P > 0.05 |
In the laparoscopy group, two conversion cases had the wounds packed open, and one laparoscopically completed case had the suprapubic wound packed open. In the open group, 11 wounds (32%) were packed open. Eight of these 11 wounds were closed on the third postoperative day; one was closed on the sixth postoperative day, and two patients were discharged with open wounds. Average postoperative hospitalization was 6.6 days for these 11 patients with open wounds.
In the laparoscopy group, both surgery time (72 vs. 53 minutes, p<.001) and total operating room time (119 vs. 85 minutes, p<.001) were longer than in the open group (Table 1). We did not observe any trend for decreasing surgical time with increasing experience in the laparoscopy group.
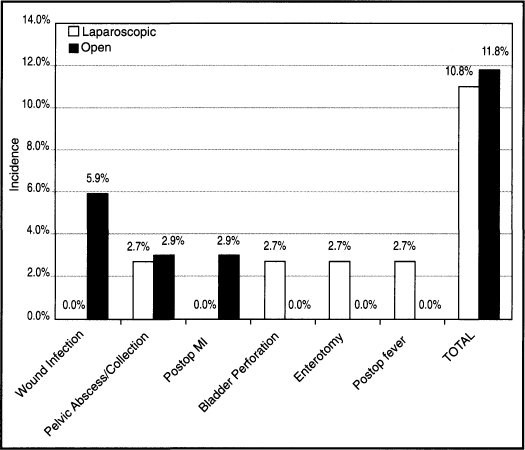
In the open group, four patients (12%) experienced postoperative morbidity (Figure 1). Two patients developed wound infections: one patient developed a pelvic abscess requiring transrectal drainage, and one had a postoperative myocardial infarction which resulted in the only death of this series. In the laparoscopy group, four patients (11%) suffered postoperative morbidity (Figure 1). One patient sustained a bladder perforation while inserting a suprapubic port under direct vision. This complication was not recognized until the postoperative period at which time the patient underwent laparotomy for primary bladder repair. Another patient suffered an enterotomy during laparoscopic dissection through extensive dense adhesions from prior surgery. The abdomen was opened to complete the procedure. A third patient was readmitted with fevers 4 days after discharge. An abdominal CT scan showed a 3 cm diameter pelvic fluid collection which was aspirated under radiologic guidance. The fluid contained few white blood cells, and cultures were negative. The fevers resolved with antibiotic therapy. A fourth patient who had been converted to an open procedure also was readmitted with fevers. No infectious source was identified but the fevers resolved with antibiotic therapy. No wound infections occurred in the laparoscopy group.
Figure 1.
Incidence of various postoperative complications and total complications in the laparoscopic and open appendectomy groups.
Analgesic and narcotic doses/postoperative hospital day were nearly identical in the laparoscopy and open groups, 2.1 vs. 2.2 analgesic doses/postoperative hospital day and 1.9 vs. 2.0 narcotic doses/postoperative hospital day, respectively (Table 1).
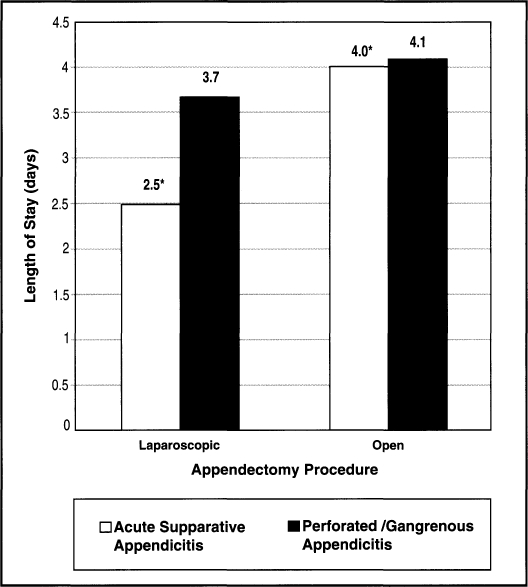
Twenty-four patients in the laparoscopy group and 23 patients in the open group were classified as having acute suppurative appendicitis (non-gangrenous, non-perforated). Mean LOS for the laparoscopy vs. the open group was 2.5 days versus 4.0 days (p<.01). Overall LOS, with analysis including patients in both groups classified as having gangrenous or perforated appendicitis, was not statistically significantly different between groups (3.7 days vs. 4.1 days, P=0.11)
DISCUSSION
In the past few years, advances in laparoscopic technology have altered the surgical approach to various abdominal problems with cholecystectomy being the most prominent example. A major benefit of laparoscopy apparently derives from the reduced abdominal wall trauma as compared to traditional open procedures. However, the abdominal wall injury may not be a significant factor for every type of abdominal incision and pathologic process. Traditional open appendectomy through a muscle splitting incision generally produces a relatively small degree of abdominal wall trauma. Patients typically return to normal activities quicker than with other types of abdominal incisions. A more limiting factor in the postoperative course of acute appendicitis may be sequelae of the inflammatory/infectious process itself. Patients require time for resolution of inflammatory changes and return of bowel function.
Our experience appears to offer a reasonable preliminary comparison between these two technical approaches. Although patients were not truly randomized, the various patient characteristics and measurements of disease severity were equally distributed between the two groups. In Attwood's series,10 patients were randomized between laparoscopic and open approaches but the report contained little information about the patients and the severity of illness.
The longer total operating room and surgery times in the laparoscopic group were not surprising. Setting up laparoscopy equipment generally took longer than setting up traditional surgical equipment. To some degree, the frequent introduction of residents to this approach contributed to procedure length. While we observed no decrease in surgery time with increasing numbers of procedures, we still feel that our experience with this procedure is not yet enough to conquer the learning curve. As our collective experience with this approach expands, we fully expect to improve our statistics in this area.
The complication rates in our two groups were similar to those previously reported for open appendectomy.12,13 No wound infections occurred in any of the laparoscopy trocar sites. Two of the complications in the laparoscopy group were technical in nature. The patient who experienced the bladder perforation had somewhat unusual anatomy. The patient with the enterotomy had extensive lower abdominal adhesions from prior surgery.
The laparoscopic technique did reduce the number of wounds that were packed open. Although packed wounds in open appendectomies reduce the incidence of wound infection, they also constitute an additional element of post-operative care and patient concern. The issue of packed wounds was not addressed in Attwood's10 randomized study.
The patients requiring conversion from laparoscopic to open appendectomy were included in the laparoscopy group on an intent-to-treat basis. With further experience, we may see a drop in the number of conversion cases but it is unlikely that these will be completely eliminated.
The laparoscopy group showed a tendency to earlier post-operative discharge but the difference was not statistically significant. Typical postoperative hospitalization in previous reports on laparoscopic appendectomy is somewhat difficult to assess. Scott-Conner8 reported a mean postoperative stay of 2.4 days for patients treated by laparoscopic appendectomy but excluded patients converted to an open procedure from the calculation. McAnena5 reported an average postoperative stay of 4.8 days for 36 open patients and 2.2 days for 27 laparoscopic patients. The difference was reported as significant but two conversion cases appear to have been excluded from the laparoscopy group statistics. Attwood's10 randomized study showed significantly earlier discharge (2.5 vs. 3.8 days, p<0.01) for laparoscopic appendectomy cases. Nowzaradan4 only stated that laparoscopic appendectomy was associated with “a shorter hospital stay.” Saye3 did not provide statistics about hospitalization. The 625 patients of Pier2 were “generally dis-charged a week after the operation.”
Two major factors may have lengthened the average post-operative stay of our laparoscopy group to 3.7 days. First, our statistics included the five patients who were converted to an open procedure. Second, our population contained more patients with advanced appendicitis. Our 35% incidence of gangrenous or perforated appendicitis in the laparoscopy group is greater than the 11% reported by McAnena5 and the 6% reported by Scott-Conner.8 The report by Attwood10 did not mention the incidence of advanced appendicitis. Our population also had relatively few negative appendices with only 14%. We feel that delayed patient presentation in our population may be the primary explanation. Interestingly, when we excluded the gangrenous and perforated appendicitis patients, the difference in postoperative hospitalization between the two groups (2.5 vs. 4.0 days) became statistically significant (Figure 2). For this subgroup, the 2.5 day postoperative hospitalization for the laparoscopy group was comparable to the 2.4 day, 2.2 day, and 2.5 day values reported by Scott-Conner, McAnena, and Attwood. The postoperative hospitalization for the open appendectomy patients in this subgroup was similar to the 3.8 days reported by Attwood. Although this sort of statistical manipulation carries limited power in a small series, the results suggest a possible relationship between disease severity, operative approach, and postoperative course. For early appendicitis with minimal peritonitis, the amount of abdominal wall trauma may play a significant role in postoperative recovery. Thus, the laparoscopic approach may result in a shorter hospitalization than the open approach. However, for advanced appendicitis, the intraperitoneal inflammation may be a more important determinant of postoperative course than the amount of abdominal wall injury from the operative approach.
Figure 2.
Postoperative length of stay in the laparoscopic versus open appendectomy groups for both acute suppurative (non-perforated, non-gangrenous) appendicitis and perforated and/or gangrenous appendicitis. The length of stay was significantly shorter for the laparoscopic appendectomy group as compared to the open appendectomy group when the appendix was not perforated or gangrenous (*P < 0.01); however, in the presence of a perforated or gangrenous appendix, there was no significant difference (P = 0.11).
An important issue not addressed in other reports concerns the criteria for patient discharge from the hospital. The clinical decision to send a patient home on a certain day rather than one day earlier or one day later can bias results which may be looking at only a one day difference between groups. Attwood10 randomized the operative approach but provided no information about discharge criteria. It would be difficult to blind a surgeon with regard to operative approach so that an unbiased decision could be made regarding hospital discharge.
We would advise surgeons to always remove the appendix when laparoscopically approaching patients with a preoperative diagnosis of acute appendicitis. This helps avoid future diagnostic dilemmas and prevents missing an early acute appendicitis with minimally visible inflammatory changes. In addition, the laparoscopic approach does not allow for appreciation of palpable abnormalities. One of our patients with a visibly normal appendix showed distinct microscopic acute appendicitis by pathology.
We attempted to use laparoscopy as a technical approach to the appendix in patients with suspected appendicitis by traditional clinical criteria. We realize that most appendectomies are diagnostic procedures initially since there is no other confirmatory test prior to operative intervention. Laparoscopy may have utility as a diagnostic tool in a broader group of patients with lower abdominal pain but we are uncertain about the indications for use.
Proponents have claimed that the laparoscopic approach allows patients to resume work or their normal lifestyle earlier than the traditional open approach but the data has not been clear. In Scott-Conner's report,8 all patients had returned to “normal activities” by their first postoperative visit one to two weeks after surgery. Attwood's randomized study10 attempted to gather more detailed information by contacting patients after their postoperative clinic visit and asking about duration of pain and return to “employment, sport, and full fitness.” The laparoscopic appendectomy patients appeared to have experienced a quicker recovery. However, Attwood's series also contained mostly younger patients in the laparoscopy group with a mean age of 20.8 years (range 12 to 39) in the laparoscopy group. In addition, we do not know how many of his patients had advanced appendicitis. We suspect that patients with simple appendicitis recover more quickly than patients with complicated appendicitis. In our series, we observed that laparoscopic appendectomy patients typically returned to normal activities within one to two weeks but we could not gather sufficient data for presentation. A patient's return to work or “normal” activity can be influenced by factors beyond the illness or surgical technique. The type of work, the desire to work, the employment status, and the availability of vacation time can significantly influence a patient's “progress.” We also observed many motivated open appendectomy patients who returned to work in one to two weeks after surgery.
CONCLUSIONS
Laparoscopic appendectomy reduces LOS as compared with the traditional open technique in patients with acute suppurative appendicitis. Mean LOS is not statistically different between groups when analysis includes patients with perforated or gangrenous appendicitis. The greater severity of illness in these patients likely outweighs those advantages of the laparoscopic approach which led to a decreased LOS in patients with uncomplicated appendicitis. Operative time for laparoscopic appendectomy was longer than for open appendectomy and is likely related to the learning curve associated with the procedure. Use of post-operative analgesia and incidence of postoperative morbidity were not statistically significantly different between groups.
We agree with other authors recommending further investigation of the laparoscopic approach in the management of right lower quadrant pain. A randomized trial should be done to more clearly define the role of laparoscopy as a “diagnostic” and “therapeutic” modality in these patients.
References:
- 1. Semm K. Endoscopic appendectomy. Endoscopy. 1983;15:59–64 [DOI] [PubMed] [Google Scholar]
- 2. Peir A, Gotz F, Bacher C. Laparoscopic appendectomy in 625 cases: from innovation to routine. Surg Laparosc Endosc. 1991;1:8–13 [PubMed] [Google Scholar]
- 3. Saye WB, Rives DA, Cochran EB. Laparoscopic appendectomy: three years' experience. Surg Laparosc Endosc. 1991;1:109–115 [PubMed] [Google Scholar]
- 4. Nowzardan Y, Westmoreland J, McCarver CT, Harris RJ. Laparoscopic appendectomy for acute appendicitis: indications and current use. J Laparoendosc Surg. 1991;1:247–257 [DOI] [PubMed] [Google Scholar]
- 5. McAnena OJ, Austin O, Hederman WP, et al. Laparoscopic versus open appendectomy. Lancet. 1991;338:693. [DOI] [PubMed] [Google Scholar]
- 6. Reddick EJ, Saye WB. Laparoscopic appendectomy. In Zucker KA, Bailey RW, Reddick EJ. eds. Surgical Laparoscopy. St Louis: Quality Medical Publishing, Inc.; 1991:227–239 [Google Scholar]
- 7. Loh A, Taylor RS. Laparoscopic appendectomy. Br J Surg. 1992;79:289–290 [DOI] [PubMed] [Google Scholar]
- 8. Scott-Conner CEH, Hall TJ, Anglin BL, Muakkassa FF. Laparoscopic appendectomy: initial experience in a teaching pro-gram. Ann Surg. 1992;215:660–670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Geis WP, Miller CE, Kokoszka JS, et al. Laparoscopic appendectomy for acute appendicitis: rationale and technical aspects. Contemporary Surg. 1992;40:14–19 [Google Scholar]
- 10. Attwood SEA, Hill ADK, Murphy PG, Thornton J, Stephens RB. A prospective randomized trial of laparoscopic versus open appendectomy. Surgery. 1992;112:497–501 [PubMed] [Google Scholar]
- 11. Olsen DO. Laparoscopic appendectomy using a linear stapling device. Surgical Rounds. 1991;14:873–883 [Google Scholar]
- 12. Lewis FR, Holcroft JW, Boey J, Dunphy JE. Appendicitis: a critical review of diagnosis and treatment in 1,000 cases. Arch Surg. 1975;110:677–684 [DOI] [PubMed] [Google Scholar]
- 13. Berry J, Malt RA. Appendicitis near its centenary. Ann Surg. 1984;200:567–575 [DOI] [PMC free article] [PubMed] [Google Scholar]