Abstract
Background:
Postcholecystectomy bilomas are relatively uncommon with a reported incidence of about 2.5%, and most often present with right upper quadrant pain and fever within seven days of the operation. There are a number of approaches to the treatment of this uncommon lesion.
Case Report:
The authors report a case of a cholecystectomy performed in a 35-year-old female which resulted in a biloma, presenting 11 days postoperatively with gastric outlet obstruction. The literature is reviewed to suggest the optimal management and treatment plans for this complication.
Results:
This patient was successfully managed with radiologic intervention for the treatment of a biloma and resulting gastric outlet obstruction after open cholecystectomy.
Conclusion:
Although uncommon, bilomas may present in an unusual manner such as with gastric outlet obstruction. As with early bilomas, they may be treated successfully with interventional radiologic techniques.
Keywords: Cholecystectomy, Biloma, Gastric outlet obstruction, Interventional radiology
INTRODUCTION
Cholecystectomy is one of the most common abdominal operations performed today. Bilomas are a rare complication following surgery for biliary disease (Table 1). Although it has been reported as occurring spontaneously with incarcerated choledocholithiasis, it is usually due to an iatrogenic injury following cholecystectomy.1 The incidence of post laparoscopic cholecystectomy biloma, in the two largest series, is about 2.5%.2,3 Most of the patients with biloma present within seven days after the operative procedure.2 The majority of minor bile leaks resolve spontaneously without creating further complications. To our knowledge, this is the first reported case of gastric outlet obstruction secondary to a post cholecystectomy biloma.
Table 1.
Summary of studies reporting bilomas after cholecystectomy.
CASE REPORT
A 35-year-old Hispanic female underwent a cholecystectomy that began using laparoscopic techniques, but was converted to open cholecystectomy due to bleeding from a small branch of the cystic artery which was easily controlled after laparotomy was performed. An intraoperative cholangiogram was obtained prior to conversion to an open procedure. Common bile duct, cystic duct and cystic artery were in normal anatomic location, and no anatomic abnormalities were identified. The patient was discharged four days after the operation. She returned one week later with complaints of nausea, vomiting, as well as right and left upper quadrant pain. There was no reported change in the color of her stools, urine or skin. Liver function tests showed elevated alkaline phosphatase, AST, ALT, with normal total and conjugated bilirubin. An abdominal ultra-sound study demonstrated large upper abdominal fluid collections bilaterally. Computed tomography (CT) of the abdomen and pelvis showed a large fluid filled structure along the dome of the liver, consistent with a subcapsular fluid collection (Figure 1). There was also marked dilatation of the stomach secondary to kinking of the duodenum by the displaced liver and subcapsular fluid mass. The patient was subsequently hospitalized and placed on naso-gastric suction. Further management included an upper gastrointestinal series that revealed extrinsic compression of the proximal duodenum, creating a partial gastric outlet obstruction (Figure 2). The patient subsequently underwent percutaneous pigtail catheter drainage placed under CT guidance, which spontaneously yielded 1.5 liters of bilious fluid. A hepatobiliary iminodiacetic acid (HIDA) scan obtained one day after the CT guided drainage concluded that there was a bile leak in the region of the gallbladder fossa (Figure 3). Endoscopic retrograde cholangiopancreatography (ERCP) showed that the second portion of the duodenum was normal, with a prominent minor ampulla, and a normal sized bile duct with no apparent leak. The patient had a sphincterotomy performed for decompression, and was subsequently discharged with catheter drainage. Ten days after discharge, the catheter became dislodged and the patient complained of recurrent pain. She was hospitalized and another ERCP was performed. It revealed a leak from a small branch of the right hepatic duct (Figure 4). A catheter drain was replaced and the patient discharged. This leak resolved spontaneously in ten days and the catheter was removed. She has remained asymptomatic and has a normal physical examination on follow-up.
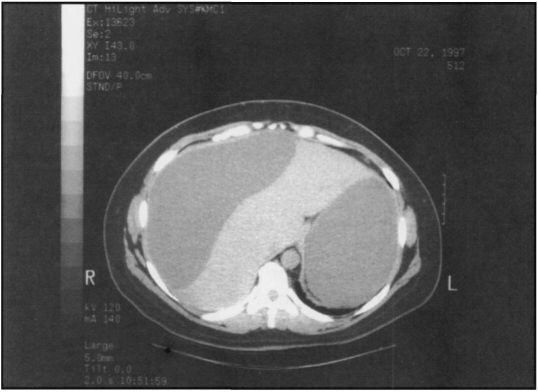
Figure 1.
Postoperative computed tomographic scan of the abdomen demonstrates a fluid collection on the right side of the liver. Note the dilatation of the stomach due to gastric outlet obstruction.
Figure 2.
Upper gastrointestinal series image reveals slow passage of contrast through the pylorus, consis-tent with a gastric outlet obstruction caused by inferior displacement of the liver secondary to a biloma.
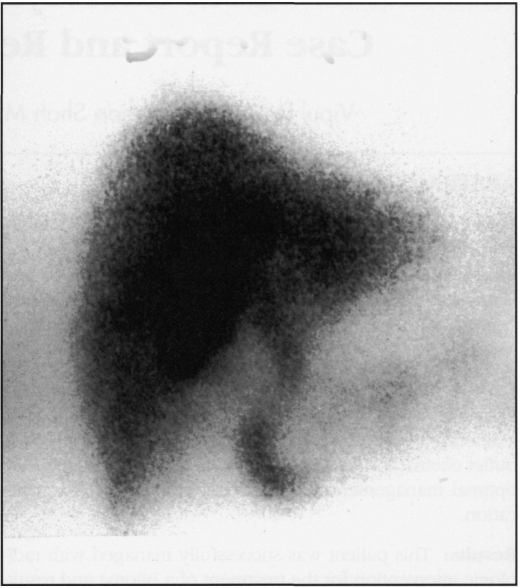
Figure 3.
Postoperative HIDA scan demonstrates a bile leak in the region of the gallbladder fossa.
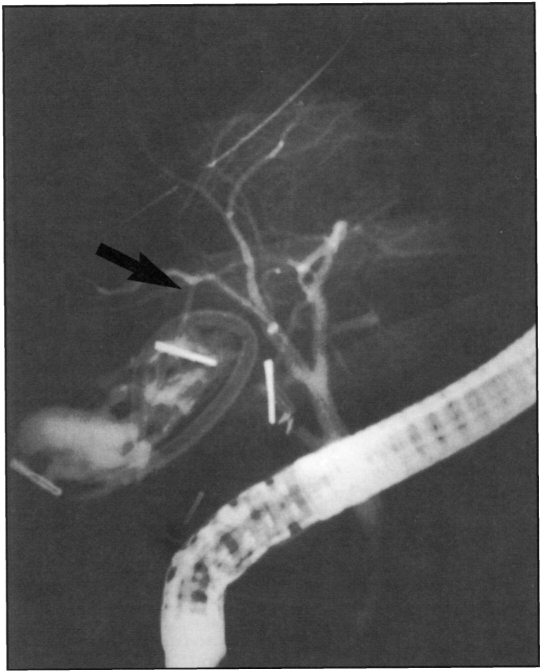
Figure 4.
ERCP shows a small leak from an accessory hepatic duct (arrow). During this procedure, a stent was placed in the common bile duct.
DISCUSSION
Postoperative biloma usually presents in a delayed fashion (about seven days) with right upper quadrant pain (RUQ) and fever. The patient in this case presented with the novel finding of gastric outlet obstruction. CT scan or ultrasound usually establishes the diagnosis of a fluid collection; however, these tests are not specific. They are unable to differentiate between a seroma, lymphocele, hematoma or biloma.3 This differentiation is complicated by the fact that there is usually some fluid in the gallbladder fossa 3-5 days post cholecystectomy.4 The performance of an intraoperative cholangiogram can demonstrate aberrant anatomy, thus decreasing the likelihood of a biliary tract injury. Bilomas can occur intrahepatically, extrahepatically, or even in the retroperitoneum.5 Radionuclide scanning (HIDA) demonstrates continuity of the fluid collection with the biliary tree.3,6 There is also literature that supports the use of MRI in this distinction. The biloma is intense on T1 weighted images and hyperintense on T2 weighted images. Hematomas, the other major differential diagnosis, are hyperintense on both T1 and T2 images.7 ERCP can be used to delineate the source of the biliary leak. If the ERCP does not demonstrate the leak, it may be coming from an accessory biliary duct, or a duct of Luschka in the liver bed.8
The optimal treatment for postoperative biloma remains an area of some controversy. ERCP with stent placement,9 percutaneous drainage,10 and nasobiliary drainage have been used alone or in combination.11 All of these procedures have been found to be equally effective.12 Brady et al. recommend an algorithmic approach to the treatment of postoperative biloma starting with percutaneous drainage and ERCP to identify the source of the leak, and subsequent sphincterotomy and stent placement if the biloma does not resolve within ten days.11 Kozarek et al. successfully treated 25% of 14 patients with biloma by percutaneous drainage alone.2 These methods are effective, but not perfect, as the biloma may recur after the intervention, thus requiring a second interventional procedure.13 Sammak et al. suggest that bile leaks without associated abdominal collections should be first identified by ERCP followed by sphincterotomy and/or stent placement. These authors reserve surgery for cases of major bile duct injury when percutaneous drainage and endoscopic management fail initially.14
In the case presented, while a leak was observed on HIDA scan, ERCP did not initially identify the site of injury. Repeat ERCP showed a leak originating from an accessory bile duct. Percutaneous drainage evacuated the fluid collection accompanied by sphincterotomy which resulted in spontaneous resolution after several days. Postoperative biloma can be a diagnostic and therapeutic challenge. HIDA radionuclide scanning may be the most useful test to establish the diagnosis. ERCP is appropriate to identify the site of leak with percutaneous drainage used as an initial therapeutic maneuver. Major bile duct injuries which pre-sent as bilomas and are identified by ERCP may require early surgical intervention. If the biloma does not resolve, then sphincterotomy and stent placement may result in resolution of the leak. Surgical intervention may be necessary in patients who do not respond to this approach.
References:
- 1. Nakajima N, Taira T, Omine M, et al. A case of spontaneous biloma accompanied with incarcerated choledocholithiasis. Nippon Geka Gakkai Zasshi. 1993;94(4):412–415 [PubMed] [Google Scholar]
- 2. Kozarek R, Gannan R, Baerg R, Wagonfeld J, Ball T. Bile leak after laparoscopic cholecystectomy. Diagnostic and therapeutic application of endoscopic retrograde cholangiopancreatography. Arch Intern Med. 1992;152(5):1040–1043 [DOI] [PubMed] [Google Scholar]
- 3. Walker AT, Shapiro AW, Brooks DC, Braver JM, Tumeh SS. Bile duct disruption and biloma after laparoscopic cholecystectomy: imaging evaluation. Am J Roentgenol. 1992;158(4):785–789 [DOI] [PubMed] [Google Scholar]
- 4. Moran J, Del Grosso E, Wills JS, Hagy JA, Baker R. Laparoscopic cholecystectomy: imaging of complications and normal postoperative CT appearance. Abdom Imaging. 1994;19(2):143–146 [DOI] [PubMed] [Google Scholar]
- 5. Colovic R, Perisic-Savic M. Retroperitoneal biloma secondary to operative common bile duct injury. HPB Surg. 1991;3(3):193–197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Morgenstern L, Berci G, Pasternak EH. Bile leakage after biliary tract surgery. A laparoscopic perspective. Surg Endosc. 1993;7(5):432–438 [DOI] [PubMed] [Google Scholar]
- 7. Shigemura T, Yamamoto F, Shilpakar SK, Kojima T, Yamamoto S, Pu Y. MRI differential diagnosis of intrahepatic biloma from subacute hematoma. Abdom Imaging. 1995;20(3):211–213 [DOI] [PubMed] [Google Scholar]
- 8. Cervantes J, Rojas GA, Ponte R. Intrahepatic subcapsular biloma. A rare complication of laparoscopic cholecystectomy. Surg Endosc. 1994;8(3):208–210 [DOI] [PubMed] [Google Scholar]
- 9. Manoukian AV, Schmalz MJ, Geenen JE, Hogan WJ, Venu RP, Johnson GK. Endoscopic treatment of problems encountered after laparoscopic cholecystectomy. Gastrointest Endosc. 1993;39(1):9–14 [DOI] [PubMed] [Google Scholar]
- 10. Nunez D, Jr, Becerra JL, Martin LC. Subhepatic collections complicating laparoscopic cholecystectomy: percutaneous management. Abdom Imaging. 1994;19(3):248–250 [DOI] [PubMed] [Google Scholar]
- 11. Brady PG, Pinkas H, Pencev D. Endoscopic retrograde cholangiopancreatography and laparoscopic cholecystectomy. DigDis. 1996;14(6):371–381 [DOI] [PubMed] [Google Scholar]
- 12. Foutch PG, Harlan JR, Hoefer M. Endoscopic therapy for patients with a post-operative biliary leak. Gastrointest Endosc. 1993;39(3):416–421 [DOI] [PubMed] [Google Scholar]
- 13. VanSonnenberg E, Casola G, Wittich GR, et al. The role of interventional radiology for complications of cholecystectomy. Surgery. 1990;107(6):632–638 [PubMed] [Google Scholar]
- 14. Sammak BM, Yousef BA, Gali MH, et al. Case report: radiological and endoscopic management of bile leak following laparoscopic cholecystectomy. J Gastroenterol Hepatol. 1997;12(1):34–38 [DOI] [PubMed] [Google Scholar]
- 15. Moss G. Raising the outcome standards for conventional open cholecystectomy. Am J Surg. 1996;172(4):383–385 [DOI] [PubMed] [Google Scholar]
- 16. Singh V, Kumar P, Rai HS, Singh K. Postcholecystectomy problems and the role of endoscopic retrograde cholangiopancreatography. Br J Clin Pract. 1996;50(4):183–186 [PubMed] [Google Scholar]
- 17. Lezoche E, Paganini AM, Carlei F, Feliciotti F, Lomanto D, Guerrieri M. Laparoscopic treatment of gallbladder and common bile duct stones: a prospective study. World J Surg. 1996;20(5):535–541 [DOI] [PubMed] [Google Scholar]
- 18. Baev S, Pozarliev T, Todorov GT. Laparoscopic cholecystectomy: 700 consecutive cases. Int Surg. 1995;80(4):296–298 [PubMed] [Google Scholar]
- 19. Bender JS, Zenilman ME. Immediate laparoscopic cholecystectomy as definitive therapy for acute cholecystectomy. Surg Endosc. 1995;9(10):1081–1084 [DOI] [PubMed] [Google Scholar]
- 20. Bezzi M, Silecchia G, Orsi F, et al. Complications after laparoscopic cholecystectomy. Coordinated radiologic, endoscopic, and surgical treatment. Surg Endosc. 1995;9(1):29–36 [DOI] [PubMed] [Google Scholar]
- 21. Tombazzi C, Lander B, Bacalao R, Marquez D, Lecuna V. Complications of laparoscopic cholecystectomy. GEN. 1994;48(4):245–249 [PubMed] [Google Scholar]
- 22. Traverse LW, Kozarek RA, Ball TJ, et al. Endoscopic retro-grade cholangiopancreatography after laparoscopic cholecystectomy. Am J Surg. 1993;165(5):581–586 [DOI] [PubMed] [Google Scholar]
- 23. Ghahremani GG, Crampton AR, Bernstein JR, Caprini JA. latrogenic biliary tract complications: radiologic features and clinical significance. Radiographics. 1991;11(3):441–456 [DOI] [PubMed] [Google Scholar]