Abstract
Background and Objectives:
Superior mesenteric artery (SMA) syndrome is a rare disorder, recognized as weight loss, nausea, vomiting, and post-prandial pain due to compression and partial obstruction of the third portion of the duodenum by the SMA. If conservative treatment fails, then laparotomy with duodenojejunostomy or lysis of the ligament of Treitz is indicated. Recently, laparoscopic division of the retroperitoneal attachments of the duodenum has been described. We report the first case of laparoscopic duodenojejunostomy as the definitive treatment of vascular compression of the duodenum.
Methods:
A very thin woman with a diagnosis of SMA syndrome was prepared for surgery after having failed medical therapy. The patient was placed in a supine position, and four laparoscopic ports were required to perform a 5 cm duodenojejunostomy.
Results:
The patient did well postoperatively. A gastrograffin study revealed no leak with patency of the duodenojejunal anastomosis. She was subsequently discharged home on a regular diet on postoperative day four.
Conclusion:
Laparoscopic duodenojejunostomy is a viable option to treat vascular compression of the duodenum. It provides definitive treatment while preserving the benefits of minimally invasive surgical techniques in the debilitated patient.
Keywords: SMA syndrome, Duodenal compression, Laparoscopy, Laparoscopic surgery, Duodenum, Duodenojejunostomy
INTRODUCTION
Vascular compression of the duodenum was first described by Rokitansky in 1842, with the first successful operative treatment, a duodenojejunostomy, performed by Stavely in 1908.1,2 The site of obstruction typically occurs in the third portion of the duodenum as the organ is held between the superior mesenteric artery and lumbar spine. Symptoms are typically chronic and intermittent and include nausea, vomiting, distention, and post-prandial epigastric pain, with resultant weight loss. The compression may occur in the setting of a narrowed aortomesenteric angle, abdominal compression by a cast or girdle, or it may be categorized as idiopathic.3–8 Some authors have suggested a genetic predisposition9 Patients are usually young, and women are affected more often than men. Surgical therapy is indicated when conservative management fails.
Historically, surgery has entailed laparotomy with duodenojejunostomy.10,11 Other technical approaches include lysis of the ligament of Treitz or gastro-jejunostomy which may be less effective; a duodenojejunostomy is required if these fail.
Recently, advances in laparoscopic skills have enabled surgeons to forego the need for laparotomy when performing operations of increasing complexity. In this report, we describe the first known case of laparoscopic duodenojejunostomy for superior mesenteric artery (SMA) syndrome.
CASE REPORT
The patient is a thin 24-year-old female with past medical history of total abdominal colectomy and ileorectal anastomosis five years earlier. She had previously done well; however, she began to complain of nausea, bilious vomiting and a recent 20 pound weight loss. An esophagogastroduodenoscopy was normal without evidence of gastric outlet obstruction. An upper gastrointestinal series with small bowel follow through demonstrated a partial obstruction of the third portion of the duodenum with marked dilatation proximally. With these clinical and radiologic findings, the diagnosis of SMA syndrome was made. The patient did not improve with conservative management and subsequently surgical consultation and operation was requested.
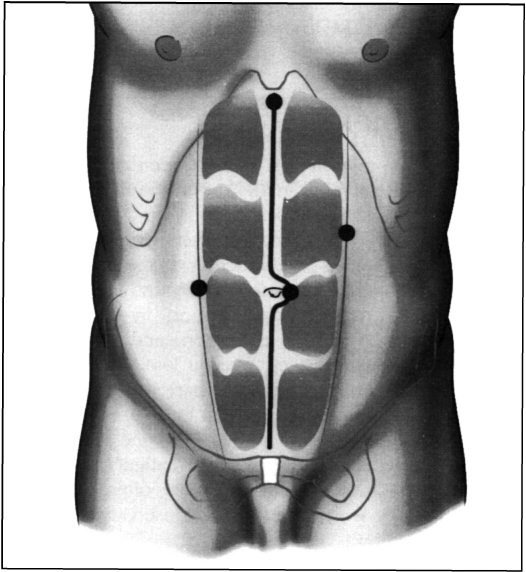
After thorough evaluation, the patient was taken to the operating room for a laparoscopic duodenojejunostomy. Due to the previous operation, an open Hasson technique12 was performed in the right paramedian position, lateral to the umbilicus. As the intra-abdominal adhesions were cleared, three additional trocars were placed, one each in the left lateral abdomen, xiphoid, and at the umbilicus (Figure 1). The proximal duodenum was notably dilated while the jejunum appeared to be normal. A Kocher maneuver was performed revealing no masses in the duodenum or head of the pancreas. The ligament of Treitz was identified, and a portion of the proximal jejunum, approximately 30 cm distal to the ligament of Treitz, was found to easily reach the duodenum. A silk suture was placed between the duodenum and jejunum, holding these two portions of the bowel in apposition. A duodenotomy was made in the lateral aspect of the second portion of the duodenum avoiding the ampulla. After performance of an anti-mesenteric jejunotomy, a 35 mm GIA (United States Surgical Corporation, Norwalk, CT) was introduced into both lumens and a duodenojejunostomy was created (Figure 2). A second load of the 35 mm GIA was used to extend the anastomosis in excess of 5 cm. The remaining duodenojejunotomy was then closed with a running 2-0 silk suture. The anastomosis was reinforced with interrupted 3-0 silk Lembert sutures and was noted to be airtight by insufflating the duodenum under a pool of saline. No drains or nasogastric tube were required, and the trocar sites were closed in the standard fashion.
Figure 1.
Trocar insertion sites for performance of a laparoscopic duodenojejunostomy. The right paramedian trocar was inserted first utilizing an open procedure, due to a previous midline incision.
Figure 2.
Creation of a laparoscopic duodenojejunostomy utilizing a 35 mm GIA stapler (United States Surgical Corporation, Norwalk, CT).
The patient did well postoperatively and was ambulating the morning after surgery. A gastrograffin study obtained on postoperative day 2 demonstrated free flow of contrast through the duodenojejunostomy (Figure 3). A diet was begun over the next 36 hours. She was discharged home on postoperative day 4 without complications, tolerating a regular diet.
Figure 3.
Upper gastrointestinal series demonstrating a patent duodenojejunostomy with flow of contrast past the stapled anastomosis.
DISCUSSION
SMA syndrome is a rare condition whose incidence ranges from 0.0024 to 0.34% for the general population, with a slightly higher incidence in chronic care facilities.13,14 Its actual incidence is largely unknown since its diagnosis is not frequently pursued in the chronically ill.
Non-operative treatment is recommended as initial therapy of the SMA syndrome.15 Patients typically assume the knee-chest position after eating, which widens the aortomesenteric angle, relieves their partial duodenal obstruction, and allows the passage of gastric contents through this area of duodenal narrowing. The use of total parenteral nutrition or aggressive nutritional support may increase the bulk of the retroperitoneal fat pad and provide relief by widening the aortomesenteric angle.16–18 This syndrome can be caused by body casts or girdles and removing these implements can aid by decreasing the extraluminal compressive forces inflicted upon the duodenum.18 If non-operative treatment fails, operation is indicated.19
Open surgical approaches have included amputation of the ligament of Treitz with repositioning of the duodenum, gastro-jejunostomy, and duodenojejunostomy.20,21 The most successful approach for treatment of the SMA syndrome has been the performance of a duodenojejunostomy, and some authors have suggested that other operative interventions are ineffective.11
Recently, laparoscopic techniques have been described. In a series by Massoud, 75% of patients were treated successfully by severing the ligament of Treitz.22 Our group opted to treat this syndrome laparoscopically by the same operation that we chose in open surgery, a duodenojejunostomy bypass. This is the first case report, to our knowledge, of performance of a laparoscopic duodenojejunostomy for treatment of SMA syndrome. Postoperative radiologic studies confirmed patency of the duodenojejunostomy, and there have been no further obstructive episodes.
CONCLUSION
In conclusion, SMA syndrome can be added to the growing list of disorders that can be successfully treated laparoscopically. Laparoscopic treatment via duodenojejunostomy is safe and effective and may offer patients the benefit of decreased pain, hospital stay, and postoperative disability.
References:
- 1. von Rokitansky CA.Handbook der Pathologischen Anatomic, 1st edition.: Vienna Wren, Braumuller, and Seidel; 1842 [Google Scholar]
- 2. Stavely AL. Acute and chronic gastromesenteric ileus with cure in a chronic case by duodenojejunostomy. Bull John Hopkins Hosp. 1908;19:252 [Google Scholar]
- 3. Mansberger AR, Jr., Hearn JB, Byers RM, Fleisig N, Buxton RW. Vascular compression of the duodenum. Emphasis on accurate diagnosis. Am J Surg. 1968;115:89–96 [DOI] [PubMed] [Google Scholar]
- 4. Lukes PJ, Rolny P, Nilson AE, Gamklou R, Darle N, Dotevall G. Diagnostic value of hypotonic duodenography in superior mesenteric artery syndrome. Acta Chir Scand. 1978;144:39–43 [PubMed] [Google Scholar]
- 5. Gustafsson L, Falk A, Lukes PJ, Gamklou R. Diagnosis and treatment of superior mesenteric artery syndrome. Br J Surg. 1984;71:499–501 [DOI] [PubMed] [Google Scholar]
- 6. Applegate GR, Cohen AJ. Dynamic CT in superior mesenteric artery syndrome. J Computer Assisted Tomography. 1988;12:976–980 [DOI] [PubMed] [Google Scholar]
- 7. Santer R, Young C, Rossi T, Biddlesberger MM. CT tomography in superior mesenteric artery syndrome. Pediatr Radiology. 1991;21:154–155 [DOI] [PubMed] [Google Scholar]
- 8. Ooi GC, Chan KL, Ko KF, Peh WC. Computed tomography of the superior mesenteric artery syndrome. Clin Imaging. 1997;21:210–212 [DOI] [PubMed] [Google Scholar]
- 9. Ortiz C, Cleveland RH, Blickman JG, Jaramillo D, Kim SH. Familial superior mesenteric artery syndrome. Pediatr Radiology. 1990;20:588–589 [DOI] [PubMed] [Google Scholar]
- 10. Kalouche I, Leturgie C, Tronc F, et al. The superior mesenteric artery syndrome: apropos of a case and review of the literature. Ann Chir. 1991;45:609. [PubMed] [Google Scholar]
- 11. Pool EH, Niles WL, Martin KA. Duodenal status: duodenojejunostomy. Ann Surg. 1933;98:587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gersin KS, Heniford BT, Arca MJ, Ponsky JL. Alternate site entry for laparoscopy in patients with previous abdominal surgery. Submitted for publication [DOI] [PubMed] [Google Scholar]
- 13. Lee CS, Mangla JC. Superior mesenteric artery compression syndrome. Am J Gastroenterol. 1978;70:141–150 [PubMed] [Google Scholar]
- 14. Goin LS, Wilk SP. Intermittent arteriomesenteric occlusion of the duodenum. Radiology. 1958;67:729. [DOI] [PubMed] [Google Scholar]
- 15. Wang YH, Takoda T. Superior mesenteric artery syndrome: a report of four cases. Gastroenterologia Japonica. 1984;19:479–485 [DOI] [PubMed] [Google Scholar]
- 16. Munns SW, Morrissy RT, Golladay ES, McKenzie CN. Hyperalimentation for superior mesenteric artery (cast) syndrome following correction of spinal deformity. J Bone and Joint Surg. American Volume 1984;66:1175–1177 [PubMed] [Google Scholar]
- 17. Milner EA, Cioffi WG, McManus WF, Pruitt BA., Jr Superior mesenteric artery syndrome in a burn patient. Nutrition in Clin Practice. 1993;8:264–266 [DOI] [PubMed] [Google Scholar]
- 18. Hutchinson DT, Bassett GS. Superior mesenteric artery syndrome in pediatric orthopedic patients. Clin Orthopaedics and Related Research. 1990;250:250–257 [PubMed] [Google Scholar]
- 19. Ylinen P, Kinnunen J, Hockerstedt K. Superior mesenteric artery syndrome. A follow up study of sixteen operated patients. J Clin Gastroenterol. 1989;11:386–391 [PubMed] [Google Scholar]
- 20. Weber H, Gumrich H, Klotz E. Arteriomesenteric duodenal compression. Chirurg. 1979;50:503–507 [PubMed] [Google Scholar]
- 21. Yang WL. Surgical treatment of superior mesenteric artery syndrome. Chinese J Surg. 1991;29:421–423 [PubMed] [Google Scholar]
- 22. Massoud WZ. Laparoscopic management of superior mesenteric artery syndrome. International Surg. 1995;80:322–327 [PubMed] [Google Scholar]