Abstract
Objective:
To evaluate the role of laparoscopic cholecystectomy in acute cholecystitis and establish the out-comes of this treatment modality at North Oakland Medical Centers.
Methods:
This was a retrospective analysis over a three-year period (January 1, 1994 to December 31, 1996), per-formed at a University-affiliated urban teaching hospital, North Oakland Medical Centers, Pontiac, Michigan. Five hundred and fifty-seven patients underwent surgical treatment for gallbladder disease; 88 patients had acute cholecystitis, and 469 patients had chronic cholecystitis. Acute cholecystitis patients underwent surgery within 72 hours of the onset of symptoms; the patient's selection for laparoscopic cholecystectomy or open cholecystectomy depended on severity of disease, comorbid factors and surgeon's preference.
The parameters of age, gender, operating (OR) time, length of stay, complications, conversion rates from laparoscopic cholecystectomy to open cholecystectomy, and cost were compared in patients who underwent laparoscopic cholecystectomy and/or open cholecystectomy.
Results:
Patients chosen to undergo laparoscopic cholecystectomy for acute cholecystitis tended to be younger females. Patients treated with laparoscopic cholecystectomy for acute cholecystitis had shorter OR times and LOS compared to patients treated with open cholecystectomy for acute cholecystitis. Conversion rates (CR) were 22% in acute cholecystitis and 5.5% in chronic cholecystitis during the study period; CR diminished considerably between the first and third year. Complications were also lower in patients who underwent laparoscopic cholecystectomy vs. open cholecystectomy.
Conclusions:
Laparoscopic cholecystectomy appears to be a reliable, safe, and cost-effective treatment modality for acute cholecystitis; however, the surgical approach should be cautionary because of the spectrum of potential technical hazards. CR is improving as surgeons gain experience.
Keywords: Acute cholecystitis, Chronic cholecystitis, Open cholecystectomy, Laparoscopic cholecystectomy
INTRODUCTION
Laparoscopic cholecystectomy has clearly become the choice over open cholecystectomy in the treatment of hepatobiliary disease since the introduction of laparoscopic cholecystectomy by Mouret in 1987. However, the role of laparoscopic cholecystectomy in acute cholecystitis remains undefined.
Surgeons remain concerned about the safety and efficacy of laparoscopic cholecystectomy in acute cholecystitis given the edema and the inflammation associated with acute cholecystitis. Several studies have been published describing varying results.1–5 This study evaluates a series of patients with acute cholecystitis and chronic cholecystitis who were treated with laparoscopic cholecystectomy or open cholecystectomy and assesses the outcomes of both techniques.
MATERIALS AND METHODS
We report a retrospective analysis of the charts of 557 patients treated for gallbladder disease at North Oakland Medical Centers from January 1, 1994 to December 31, 1996.
We defined acute cholecystitis by the acuity of clinical symptoms (24-72 hours), physical findings of right upper quadrant tenderness, guarding or rebound, laboratory data showing leukocytosis ≥12,000/ml, intraoperative gross morphologic findings of acute cholecystitis and histologic findings of neutrophil infiltration, edema, necrosis or microperforation.
We divided the patients based on their diagnosis and treatment modality into four groups: acute cholecystitis treated by laparoscopic cholecystectomy, acute cholecystitis treated by open cholecystectomy, chronic cholecystitis treated by laparoscopic cholecystectomy and chronic cholecystitis treated by open cholecystectomy.
These groups were compared on the basis of mean age, male/female ratio, operative time, length of hospital stay, hospital costs and conversion rates from laparoscopic cholecystectomy to open cholecystectomy when applicable.
For statistical comparative analysis among the groups, ANOVA was used for the age, length of stay, and OR time, Mann-Whitney for the gender ratio and Chi-square for the conversion rate.
RESULTS
Of the 557 patients reviewed, there were 133 males and 424 females; as expected, there were more female patients with gallbladder disease overall, but no statistical difference was delineated when the groups' ratios were tested by Mann-Whitney.
The overall age, expressed as mean ±SD, was 52 ±12 years, and no statistical difference was observed in age among the four groups by ANOVA.
Eighty-eight patients (15.8%) had acute cholecystitis; of these, 14.8% had acute calculous cholecystitis, 1% as acute acalculous cholecystitis.
Four hundred and twenty-nine patients (84.2%) had chronic cholecystitis; of these, 68% were diagnosed as chronic calculous cholecystitis, 16.2% as chronic acalculous cholecystitis.
Sixty-seven of the 88 acute cholecystitis patients under-went primary laparoscopic cholecystectomy, while 21 patients were considered high risk enough to warrant primary open cholecystectomy. In the chronic cholecystitis group, 454 underwent laparoscopic cholecystectomy, while 15 underwent open cholecystectomy, primarily.
OR times were (in minutes) 134 in laparoscopic cholecystectomy and 157 in open cholecystectomy in the acute cholecystitis group and 112 in laparoscopic cholecystectomy and 149 in open Cholecystectomy in the chronic cholecystitis group. Laparoscopic cholecystectomy had a significantly shorter OR time compared to open Cholecystectomy in the chronic cholecystitis group (p<0.05 by ANOVA).
The length of stay was 2.81 days for laparoscopic cholecystectomy vs 9.29 days for open Cholecystectomy in the acute cholecystitis group and 2.34 days for laparoscopic Cholecystectomy vs 11.43 days for open Cholecystectomy in the chronic cholecystitis group. The length of stay was significantly shorter for laparoscopic cholecystectomy compared to open Cholecystectomy in both acute cholecystitis and chronic cholecystitis groups (p<0.04 by ANOVA).
Comparison of all the above-mentioned results in the four groups are demonstrated in Table 1.
Table 1.
Comparison of Open and Laparoscopic Cholecystectomy.
| Procedure | M/F Ratio | Age (years) | OR time (min) | LOS (days) | Conversion (%) |
|---|---|---|---|---|---|
| AC (LC) N=(67) | 29/38 | 46.39 ± 15.27 | 134 ± 38 | 2.81 ± 2.17 | 15 cases (22%) |
| AC (OC) N=(21) | 14/7 | 59.57 ± 14.66 | 157 ± 34 | 9.29 ± 6.55 | NA |
| CC (LC) N=(454) | 82/372 | 45.31 ± 17.78 | 112 ± 34 | 2.34 ± 3.23 | 25 cases (5.5%) |
| CC (OC) N=(15) | 8/7 | 61.33 ± 43.08 | 149 ± 74 | 11.43 ± 18.14 | NA |
Data are expressed above as Mean ± SD.
AC=Acute Cholecystitis
LC=Laparoscopic Cholecystectomy
OC=Open Cholecystectomy
CC=Chronic Cholecystitis
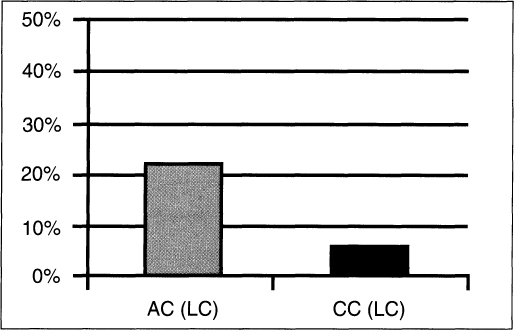
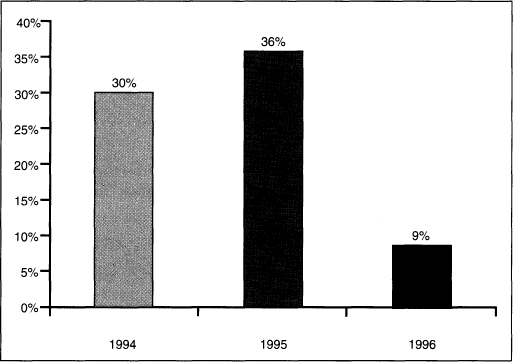
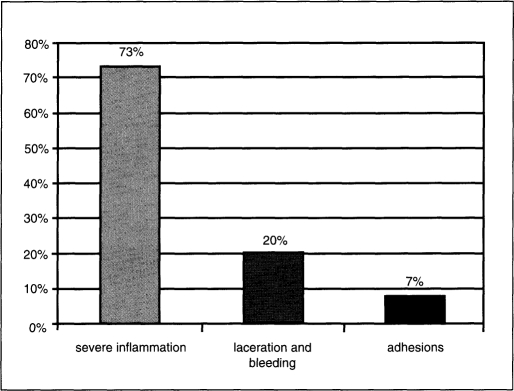
In the acute cholecystitis group, 15 patients (22%) required conversion, compared to 25 (5.5%) in the chronic cholecystitis group (Figure 1), and that was significantly higher in the acute cholecystitis group by Chi-square (p<0.05). Conversion rate for acute cholecystitis was noted to decrease from 30% in 1994 and 36% in 1995 to 9% in 1996 (Figure 2). The main reasons for conversion were the severity of inflammation in 11 cases (73.3%), laceration and bleeding of the gallbladder fossa/liver in 3 cases (20%) and, adhesions from previous surgeries preventing adequate exposure in 1 case (6.7%) (Figure 3)
Figure 1.
Graph depicting rates of conversion to open cholecystectomy (OC) between acute cholecystitis (AC) and chronic cholecystitis (CC).
Figure 2.
Graph depicting the conversion rates from laparoscopic Cholecystectomy (LC) to open Cholecystectomy (OC) over the three years of the study.
Figure 3.
Graph depicting the most common reasons of con-version from laparoscopic cholecystectomy (LC) to open cholecystectomy (OC).
The overall most frequent complications and comparison of complications of laparoscopic cholecystectomy/open cholecystectomy in acute cholecystitis patients including respiratory, gastrointestinal, urinary, cardiovascular, and iatrogenic complications are demonstrated in Table 2. The respiratory complications are the most frequently encountered. One patient with bile duct stricture due to thermal injury presented with obstructive jaundice and required stenting three months postoperatively, which was similar to other studies.6 The mortality rate was 0.7% and 1.8% for laparoscopic cholecystectomy and open cholecystectomy, respectively, and was comparable to other series.2
Table 2.
Complications
| Complications | Overall | LC/OC in AC |
|---|---|---|
| Respiratory (atelectasis, ARDS, pneumonia) | 27% | 2%/6% |
| GI (ileus, nausea or vomiting) | 17% | 3%/11% |
| latrogenic: Bleeding (intraoperative) | 11% | 6%/0% |
| Bleeding (postoperative) | 9% | 6%/0% |
| CBD injury (delayed stricture) | 1% | 1.1%/0% |
| Urinary (retention, infection) | 9% | 6%/15% |
| Wound Infection | 8% | 2%/6% |
| Cardiovascular (MI, CHF) | 4% | 1%/4% |
| Mortality | 1% | 0.7%/1.8% |
AC=Acute Cholecystitis
LC=Laparoscopic Cholecystectomy
OC=Open Cholecystectomy
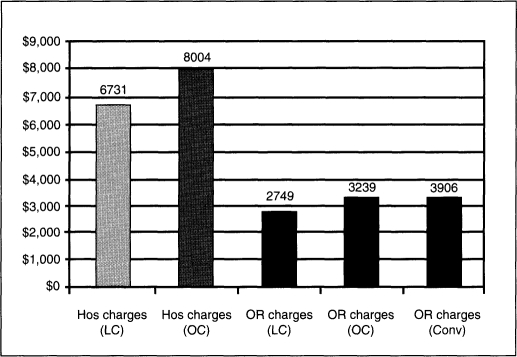
When we analyzed cases for hospital charges, a significant reduction was seen as follows: operating room (OR) charges were $2749 for laparoscopic cholecystectomy, $3239 for open cholecystectomy, and $3906 for laparoscopic cholecystectomy converted to open cholecystectomy. Hospital charges were $6731 for laparoscopic cholecystectomy and $8004 for open cholecystectomy (Figure 4). These figures are preset charges by the hospital.
Figure 4.
Graph comparing the hospital (Hos) and operating room (OR) charges between laparoscopic cholecystectomy (LC), open cholecystectomy (OC) and converted cases (Conv).
DISCUSSION AND CONCLUSIONS
Over the past decade, laparoscopic cholecystectomy has become the predominant procedure in the treatment of hepatobiliary disease. However, the role of laparoscopic cholecystectomy in acute cholecystitis remains unclear.
The fact remains that there have been wide variations in the definition of acute cholecystitis as published in various studies,1 as well as varying thresholds in surgeons' decisions preoperatively to perform open cholecystectomy primarily.
It is interesting to note that in this study patients who were selected for open cholecystectomy primarily in both groups acute cholecystitis and chronic cholecystitis were similar, although the distinction was not statistically significant. We noted that the male to female ratio was higher in the open cholecystectomy group—-again not statistically significant. These results concur with previous series,7 which show that males tend to become symptomatic later in life and have associated with other comorbidities.
Shorter OR times in laparoscopic cholecystectomy versus open cholecystectomy in the acute cholecystitis and the chronic cholecystitis groups were noted; however, this was only statistically significant in the chronic cholecystitis group, but it did not reach statistical significance for the acute cholecystitis group.
The length of stay was significantly shorter for laparoscopic cholecystectomy when compared to open cholecystectomy in both the acute cholecystitis and the chronic cholecystitis groups. These numbers are in line with national and international standards for this procedures.7 Hospital costs were also lower for the laparoscopic cholecystectomy group vs the open cholecystectomy group, mainly because of the significantly shorter length of stay and the lower cost of OR charges for the laparoscopic cholecystectomy procedure. We believe that this reduction in length of stay, along with laparoscopic cholecystectomy as the procedure of choice for gallbladder disease, influences the economic component of treatment of this disease. This minimally invasive procedure is easier on the patients, and they recover faster.
The conversion rate of laparoscopic cholecystectomy to open cholecystectomy was higher for acute cholecystitis than that for the chronic cholecystitis group: “The most frequent reason for conversion was technical difficulty encountered because of the inflammatory process, similar to what has been described by other authors.”3
In our study, the rates of conversion markedly decreased over the three-year period. This probably correlates with increasing experience and confidence of the surgeons in this procedure, primarily. There appears to be reluctance on the part of laparoscopic surgeons, in general, to convert to open procedure.
Overall, published complications and mortality rates are lower for laparoscopic cholecystectomy than open cholecystectomy. However, iatrogenic injuries to the bile duct and the liver, as well as postoperative bleeding, were higher in the laparoscopic cholecystectomy group than the open cholecystectomy group, as was previously reported by our group and others,4,8 which reported similar results.
Laparoscopic cholecystectomy appears to be a reliable, safe and cost-effective procedure for acute cholecystitis with increasing experience. We believe that with a cautionary approach to acute cholecystitis, laparoscopic cholecystectomy will provide better outcomes in the management of this condition.
References:
- 1. Lujan JA, Parrilla P, Robles R, Marin P. Laparoscopic cholecystectomy vs open cholecystectomy in the treatment of acute cholecystitis — A prospective study. Arch Surg. 1998;133:173–175 [DOI] [PubMed] [Google Scholar]
- 2. Colonval P, Navez B, Cambier E, et al. Is laparoscopic cholecystectomy effective in acute cholecystitis? Ann Chir. 1997;51(7):689–696 [PubMed] [Google Scholar]
- 3. Schafer M, Krakenbuhl L, Farhadi J, Buckler MW. Cholecystitis-Laparoscopy or Laparotomy? Ther Umschau. 1998;55(2):110–115 [PubMed] [Google Scholar]
- 4. Kiviluoto T, Siren J, Luukkonen P, Kivilaasko E. Randomized trial of laparoscopic vs open cholecystectomy for acute and gangrenous cholecystitis. Lancet. 1998;351(9099):321–325 [DOI] [PubMed] [Google Scholar]
- 5. Turfah F, Nazzal M, Ali A, Silva Y. Laparoscopic cholecystectomy: analysis of the complications at a community hospital. Surg Laparosc Endose. 1994;4(4):264–267 [PubMed] [Google Scholar]
- 6. Targarona EM, Marco C, Balague C, et al. How, when, and why bile duct injury occurs. Surg Endose. 1998;12(4)322–326 [DOI] [PubMed] [Google Scholar]
- 7. Wherry DC, Marohn MR, Malanoski MP, Hetz SP, Rich NM. An external audit of laparoscopic cholecystectomy in the steady state performed in medical treatment facilities of the Department of Defense. Ann Surg. 1996;224(2):145–145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Chen AY, Daley J, Pappas TN, Henderson WG, Khuri SF. Growing use of laparoscopic cholecystectomy in the Veterans Affairs Surgical Risk Study. Ann Surg. 1998;227(1):12–24 [DOI] [PMC free article] [PubMed] [Google Scholar]