Abstract
Objective:
The aim of this study is to evaluate laparoscopy as another tool for management of cases of adhesive acute small bowel obstruction.
Methods:
Fourteen patients suffering from suspected adhesive small bowel obstruction were explored laparoscopically over a period of 24 months. The Veress needle was inserted either in a virgin part of the abdomen away from previous scars or under direct vision using an open technique. Careful inspection of the entire abdomen was done, and the small bowel was “run” in a retrograde fashion starting at the cecum. The point of obstruction was localized and adhesiolysis was performed, thus resolving the problem.
Results:
Laparoscopic exploration was able to determine the site and cause of obstruction precisely in all 14 cases, with resolution of the problem laparoscopically in 12 patients (85.7%). Two cases were converted to open surgery (14.3%). There were no mortalities and low morbidity (7.1%). The mean hospital stay was 3.7 days.
Conclusion:
Laparoscopic surgery can be an advantageous alternative to open surgery in acute small bowel obstruction, thus providing a new technique for its diagnosis and treatment with all the advantages of minimally invasive surgery.
Keywords: Acute small bowel obstruction, Adhesiolysis, Laparoscopy
INTRODUCTION
The goal of surgical management of bowel obstruction should focus on avoiding operative delay and reducing the morbidity associated with bowel strangulation.1 In many ways, the wisdom of the adage “never let the sun rise and set on a case of unrelieved intestinal obstruction” remains the safest guideline whenever any uncertainty exists.2
Although laparoscopic division of adhesions has long been practiced by gynecologists, the standard operative approach in acute small bowel obstruction has been laparotomy. Laparoscopy in such patients has been considered dangerous, with the possibility of damage to the dilated loops of the bowel by the insufflating needle or trocars.3 However, the recent expansion and acceptance of laparoscopic procedures has led to the re-evaluation of laparoscopic surgery as one more useful tool in the management of small bowel obstruction.4
PATIENTS AND METHODS
A total of 14 patients (five males and nine females) with ages ranging from 26 to 68 years (median age 53.5 years) were included in this study. All the patients presented with typical symptoms and signs of acute small bowel obstruction, and the diagnosis was confirmed by flat and upright films of the abdomen.
Initially, all patients were treated conservatively. They were maintained without oral intake, and nasogastric decompression was instituted. Peripheral or central intravenous lines were established for fluid and electrolyte replacement. Failure of expectant management to relieve symptoms or result in improvement in 24 hours, or the worsening of symptoms and signs, were indications to proceed with laparoscopic exploration.
All 14 patients in this study were explored by the laparoscope.
OPERATIVE TECHNIQUE
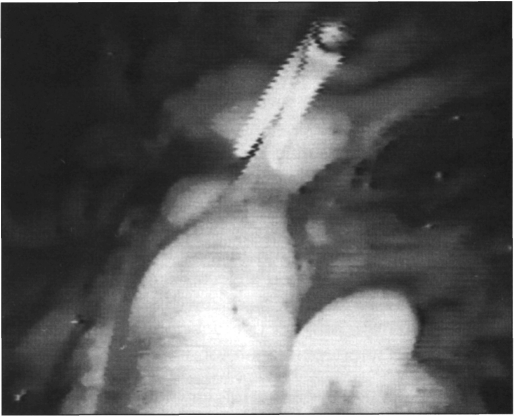
With the patient under general anesthesia, a Veress needle was inserted at the umbilicus in the previously un-operated patients (only 1 patient in this study), and the peritoneal cavity was insufflated with carbon dioxide to the level of 14 mm Hg of pressure. If the patient had previous surgery (13 patients), the umbilicus was avoided as a puncture site. We have modified a new procedure, where we now routinely use the open method for entering the abdominal cavity by performing a cut-down procedure for trocar insertion in the middle line in a virgin part of the abdomen away from any previous scars. However, in the presence of middle-line abdominal scars, our first port of entry was either in the middle line away from the scar (eg, the epigastrium in the case of subumbilical scars) or the right or left upper abdominal quadrants. A 10 mm trocar was then inserted into the peritoneal cavity under direct visualization, and the camera was introduced through this port. Direct visualization of the peritoneal cavity permitted the insertion of 2 additional 5 mm trocars in the right and left lower quadrants or as indicated for a specific point of obstruction, then lysis of adhesions in the subumbilical area was done sufficient enough to allow placement of another 10 mm trocar under visual control (Figure 1). The camera was then moved to this port.
Figure 1.
Lysis of adhesions in the periumbilical area to allow trocar placement.
A careful inspection of the entire abdominal cavity was performed, and the small bowel was “run” in a retrograde fashion starting at the cecum by grasping the bowel with two atraumatic graspers (endoscopie Babcock) and using a “hand to hand” technique (Figure 2). Placing the patient in the steep Trendelenburg position and tilting the patient to the far left for 30° allowed us to visualize the cecum properly and enhanced “running” of the small bowel even in the most distended patients. The point of transition between a proximal dilated loop of small intestine and a distal decompressed loop is considered to be the point of obstruction (Figure 3). Gentle manipulation of the bowel loops using the grasper was performed to identify the obstructing adhesive band, and a hooked electrocautery tip or diathermy scissors was used to divide it (Figure 4, 5). The affected bowel was observed for five minutes to confirm its viability.
Figure 2.
“Hand to hand” technique of bowel exploration using non-traumatic laparoscopic clamps.
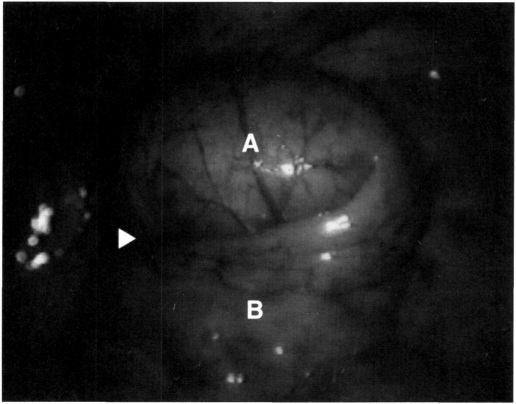
Figure 3.
Portion of bowel suspected to harbor an adhesive band (arrow) showing distended bowel (A) proximal to this point and decompressed bowel (B) distal to this point.
Figure 4.
Lysis of adhesions using diathermy scissors.
Figure 5.
Lysis of adhesions using diathermy scissors.
RESULTS
Table 1 shows the ages, operative findings and procedures, complications and duration of hospital stay for the 14 patients studied in this series.
Table 1.
Ages, operative findings and procedures, complications and duration of hospital stay for the 14 patients studied in this series.
| No. of Patients | Age of patients | Operative findings | procedure | Complications | Hospital stay |
|---|---|---|---|---|---|
| 1 | 68 y | Jejunal adhesions of unknown etiology | Laparoscopic lysis of adhesions | Atelectasis | 12 days |
| 10 | 26-61 y | Single and multiple adhesions with small bowel obstruction | Laparoscopic lysis of adhesions | None | 48 hrs to 9 days |
| 1 | 33 y | Adhesions at appendectomy scar with small incisional hernia | Laparoscopic lysis of adhesions with repair of the defect | None | 5 days |
| 2 | 39-46 y | Dense multiple adhesions with matting of the small bowel | Conversion to open Procedure for lysis of adhesions | Wound sepsis in 1 case | 2 weeks |
In 12 cases, the obstruction was secondary to adhesions in patients with past history of abdominal surgery. One patient had obstruction from jejunal adhesions of unknown etiology, with no history of previous surgery. In the remaining case, the etiology of obstruction was adhesions together with a small incisional hernia at an old appendectomy incision (Figure 6).
Figure 6.
Incisional hernia in an old appendectomy site with adhesions.
In all the cases, we were able to determine the point of obstruction with the laparoscope; and the diagnosis was confirmed, clearly demonstrating the exact location of the problem.
In 12 patients, the procedure of laparoscopic exploration with adhesiolysis was successful (85.7%). No bowel resections were needed, as no necrotic bowel was present due to our early surgical intervention. However, two patients (14.3%) were converted to an open procedure because of massive adhesions and inability to relieve the obstruction in a safe and timely manner. There has been low morbidity related to this procedure with no mortality. One patient developed atelectasis after laparoscopic exploration (7.1%) that necessitated prolonged hospitalization (12 days). Another one developed postoperative wound sepsis after open laparotomy.
The average operative time for the entire laparoscopic procedure was 1 hour 15 minutes (30-120 minutes). The average postoperative hospital stay was 3.7 days with a range from 2 to 14 days, and return to normal activity was within 7 to 18 days (average of 12.6 days) postoperatively.
DISCUSSION
The standard surgical approach to acute small bowel obstruction has been laparotomy. This is often undertaken in an ill patient with fluid and electrolyte imbalance. To determine the site of obstruction, a large incision is usually required, and there may be significant manipulations of the bowel. However, in the case of a band of adhesion, the obstruction is usually relieved speedily with relative ease.
Postoperatively, these patients suffer from the pain of laparotomy, and they usually have a significant ileus complicating existing fluid and electrolyte, and nutritional disturbances. There is also a high incidence of cardiorespiratory complications. In addition, there is the risk of more adhesions being caused by the laparotomy designed to release them.3
The recent advances in video equipment, together with the acceptance of laparoscopic surgery by surgeons and the public in general, led us to evaluate laparoscopy as an alternative to the conventional management of small bowel obstruction.
Although laparoscopy is a new technique to many physicians, it has been used for more than 60 years in gynecology,5 and lysis of adhesions has been performed by gynecologists for years.6
In the past, bowel dilatation and adhesions have been seen as relative exclusion criteria for laparoscopy because of the risk of visceral perforation at insufflation or with the introduction of the first port. Using the open technique that we have applied for trocar insertion usually allows a safe entry into the peritoneum in the face of mechanical bowel obstruction with dilated loops of intestine. So, we did not consider massive intestinal dilatation an absolute contraindication to laparoscopic evaluation, although visualization was obviously more difficult in those patients and particular care was exercised during insufflation and initial trocar placement.
Also, placing the patient in the steep Trendelenburg position and tilting the patient to the far left for 30° allowed us to visualize the cecum properly and enhanced “running” of the small bowel even in the most distended patients. However, we strongly recommend appropriate selection of cases, and we advise that patients chosen for laparoscopic exploration for small bowel obstruction should show no evidence of inflammatory bowel disease or intraabdominal malignancy. Also, the obstruction should be of relatively short duration, and the cause of obstruction should be a band of adhesion and not the dense fibrinous adhesions seen in patients with numerous previous laparotomies.
At the present level of technology in laparoscopic surgery, this technique should not be recommended if suspicion of a simple adhesive band as the etiology of the obstruction is not present, since management of small bowel obstruction secondary to other etiologies may not be technically feasible.7
Also, what is of great concern is the proper handling of the dilated, and often fragile, loops of intestine. We believe that the use of non-traumatic bowel clamps pre-vents this complication, and they are strongly recommended, as smaller sharp dissectors and graspers will result in injury and tearing of the bowel.
The selection of patients for a laparoscopic approach to intestinal obstruction should also depend on the skill and experience of the surgeon as well as the presenting circumstances and past history of the patient. Thus, we recommend that a surgeon just gaining experience in laparoscopic techniques should obviously not tackle such patients.
We agree with Jentschura,8 that patients with elevated white blood count, temperature elevation, massively dilated bowel and exquisite abdominal tenderness could very well be evaluated laparoscopically, but then converted rapidly to an open procedure if necrotic bowel is suspected or severe adhesions are present.
In our study, laparoscopy was used to explore 14 patients suffering from acute adhesive small bowel obstruction, and it was successful to confirm the diagnosis and to manage this obstruction in 12 cases (85.7%), thus sparing these patients from laparotomy. There was low morbidity (7.1%), no mortality, short hospital stay (3.7 days) and rapid return to normal activities. However, we did not hesitate to resolve the acute obstruction with a classic open technique when the laparoscopic approach was found difficult or hazardous, because we believe that surgeons should not allow the excitement for a new surgical technique to cloud their clinical or surgical judgment.
CONCLUSION
The relatively new field of endoscopie surgery shows much promise and allows alternative treatment options. With increasing numbers of surgeons gaining experience with this technique, new approaches to old conditions are being reported. We believe that laparoscopic surgery in small bowel obstruction has the advantage of precisely localizing the problem and providing a means of rapid treatment of the disease process with minimal morbidity and mortality and, at the same time, overcoming all the drawbacks of the classic open technique. However, we strongly recommend that there should be proper patient selection and a skilled laparoscopic surgeon available.
Contributor Information
Ahmed Awad El Dahha, Assistant Professor of Surgery, Faculty of Medicine, Minia University, EGYPT..
Ashraf M. Shawkat, Assistant Professor of Surgery, Faculty of Medicine, Minia University, EGYPT..
Ashraf Aly Mohammad Bakr, Assistant Professor of Surgery, Faculty of Medicine, Cairo University, EGYPT..
References:
- 1. Mucha P. Small bowel obstruction. Surg Clin North Am. 1983;67:597–620 [DOI] [PubMed] [Google Scholar]
- 2. Fabri PJ, Rosemurgy A. Reoperation for small bowel obstruction. Surg Clin North Am. 1991;71:131–146 [DOI] [PubMed] [Google Scholar]
- 3. Adams S, Wilson T, Brown AR. Laparoscopic management of acute small bowel obstruction. Aust NZJ Surg. 1993;63:39–41 [DOI] [PubMed] [Google Scholar]
- 4. Franklin ME, Dorman JP, Pharand D. Laparoscopic surgery in acute small bowel obstruction. Surg Laparosc Endose. 1994;4:289–296 [PubMed] [Google Scholar]
- 5. Semm K. Current concepts in female sterilization. Clin Obstet Gynecol. 1974;17:141–142 [DOI] [PubMed] [Google Scholar]
- 6. Semm K. Atlas of Gynecologic Laparoscopy and Hysteroscopy. Philadelphia: W B Saunders; 1977:7–14 [Google Scholar]
- 7. Bastug DF, Trammell SW, Boland JP, Mantz EP, Tiley EH., III Laparoscopic adhesiolysis for small bowel obstruction. Surg Laparosc Endose. 1991;1(4):259–262 [PubMed] [Google Scholar]
- 8. Jentschura D, Wissenbach R, Manegold BC. Laparoscopic treatment of postoperative intraperitoneal adhesions. Abstract from the Society of American Gastrointestinal Endoscopie Surgeons. 1991 Scientific Session, Monterey, CA [Google Scholar]