Abstract
Background:
Widespread adoption of minimal access techniques forced a generation of abdominal surgeons to re-learn many standard abdominal procedures. This threatened to reduce the pool of suitable “training” operations for surgical residents.
Methods:
Operator grade, duration of operation, acute/elective operation, conversion rate, complications, and postoperative stay were recorded prospectively on all laparoscopic cholecystectomies (LC) since 1992. This data was evaluated to determine how the introduction of LC affected residents' training.
Results:
The percentage of LCs performed by residents increased progressively to reach 58%. Operating time was longer for trainee surgeons, particularly for acute cases (145 ± 50 minutes vs 111 ± 54 minutes, p<0.05); however, conversion rate, incidence of complications, and postoperative stay were no different.
Conclusions:
LC can be performed by surgical trainees with similar complication rates and outcomes as those of qualified surgeons. Once institutional experience has accumulated, this procedure can be integrated into residency training.
Keywords: Laparoscopic cholecystectomy, Surgical training
INTRODUCTION
The provision of basic operative skills training in general surgery has traditionally relied heavily on the two most common abdominal procedures, appendicectomy and cholecystectomy. Performance of both of these operations under supervision gave surgical residents the opportunity to learn the principles of tissue handling and instrument technique, which they could subsequently apply to more complex procedures. One of the consequences of the widespread adoption of minimal access surgical techniques for these and other common abdominal operations was that a whole generation of trained surgeons was forced to re-evaluate and re-learn these procedures. This threatened to reduce the pool of suitable training operations for surgical residents.
The aim of this study was to compare the outcome of this procedure when performed by trainees compared with qualified surgeons and to evaluate the impact of the introduction of the laparoscopic method on the status of cholecystectomy as a training operation in a university clinic.
PATIENTS AND METHODS
Laparoscopic cholecystectomy was first introduced to this unit in 1992. The first 80 cases were performed by qualified surgeons only, mainly by a group of three surgeons who developed a special interest in laparoscopic and endoscopic surgery. From January 1995 onwards, surgical residents in their third or higher year of training were allowed to perform laparoscopic cholecystectomy under the supervision of a trained surgeon who acted as cameraman. Residents also attended an animal laboratory course and were encouraged to practice on a laparoscopic training rig. Between January 1992 and December 1996, a further 252 cases were performed, and these form the basis of this study. There were 57 male and 195 female patients with a mean age of 53 years (range 16-89 years). One hundred and ninety-nine procedures (79%) were elective operations for biliary colic or chronic cholecystitis, and the remaining 53 (21%) were performed following urgent admission with acute cholecystitis. Acute cholecystitis was defined by the presence of acute localized right upper quadrant pain with temperature greater than 37.5°C and leukocytosis. Confirmation of the diagnosis was by ultrasound with demonstration of gallstones, gallbladder wall thickening or edema, and peri-cholecystic fluid. For patients admitted with acute cholecystitis, operation was scheduled within 72 hours of hospitalization.
RESULTS
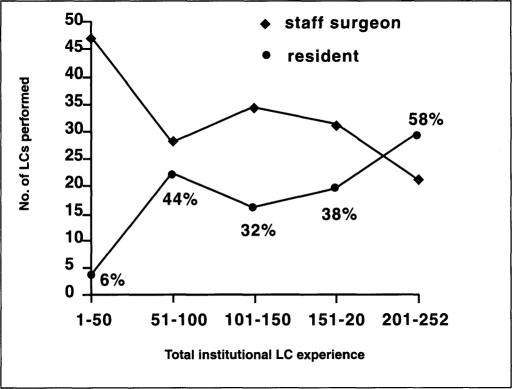
Over the complete two-year period covered by this study, trainee surgeons performed 37% of all elective laparoscopic cholecystectomies and 29% of all procedures done for acute cholecystitis (Table 1). However, the percentage of cases performed by residents increased progressively as the combined experience of all the surgeons in the unit expanded. During the first 50 cases “available” to residents, just 6% were operated on by trainees, whereas after a further 200 cases, residents operated on 58% of patients. The change in the percentage of patients operated on by residents compared to qualified surgeons over the study period is shown in Figure 1.
Table 1.
Effect of operator grade and presence or absence of acute cholecystitis on duration of operation (minutes).
| Surgeon | Resident | |||
|---|---|---|---|---|
| # of Cases | Operating Time (min ± SEM) | # of Cases | Operating Time (min ± SEM) | |
| Elective | 124 | 97 ± 42 | 74 | 119 ± 33a |
| Acute cholecystitis | 38 | 111 ± 54b | 15 | 145 ± 50c |
Statistical comparison of duration of operation was performed by chi-squared test. a vs c and b vs c both significantly different, p < 0.05.
Figure 1.
Percentage of laparoscopic cholecystectomies (LC) performed by residents. The x-axis shows the total institutional experience of laparoscopic cholecystectomy grouped into blocks of 50 cases.
The duration of the procedure (skin-to-skin time) was affected by the grade of the operator (Table 1). Residents required more time (119 ± 33 minutes) compared to qualified surgeons (97 ± 42 minutes) for elective cases, although this did not reach statistical significance.
However, when the operation was performed for acute cholecystitis, the duration of the operation was significantly longer for residents (145 ± 50 minutes) than trained surgeons (111 ± 54 minutes, p<0.05, chi-squared test).
Conversion rate and complications according to operator grade are shown in Table 2. The rate of conversion to open cholecystectomy was not significantly different between trainee and qualified surgeons [resident: 2 cases (2%); surgeon: 11 cases: (6%)]. There was only one bile duct injury in a patient operated on by a staff surgeon, which was recognized at the time of injury and converted to laparotomy for primary repair. Bile leak due to cystic duct stump insufficiency was seen in four patients, two of whom had been operated on by resi-dents. All four cases were managed successfully by endoscopic stent insertion. Other complications included subhepatic abscess and port-site bleeding, which occurred in one patient each, respectively, and minor wound infections in three patients.
Table 2.
Effect of operator grade on conversion rate and complications. Percentages are given in brackets.
| Surgeon | Resident | |
|---|---|---|
| Conversion rate | 11 (6) | 2 (2) |
| CBD injury | 1 (0.5) | 0 (0) |
| Cystic duct leak | 2 (1) | 2 (2) |
| Subhepatic abscess | 1 (0.5) | 0 (0) |
| Small bowel injury | 0 (0) | 1 (1) |
| Port site bleeding | 0 (0) | 1 (1) |
Mean postoperative stay is shown in Table 3. Postoperative stay was not influenced by the grade of operator or by the presence of acute cholecystitis.
Table 3.
Effect of operator grade on postoperative length of stay in days (range).
| Surgeon | Resident | |||
|---|---|---|---|---|
| # of Cases | Length of Stay | # of Cases | Length of Stay | |
| Elective | 124 | 5 (1-34) | 74 | 6 (1-18) |
| Acute cholecystitis | 38 | 6 (1-18) | 15 | 8 (2-37) |
No significant differences.
DISCUSSION
The widespread adoption of minimal access techniques raised concerns about the possibly detrimental effects this might have on operative experience of surgical residents.1,2 Certainly, most residents in training viewed the period during which their mentors re-learned many standard abdominal procedures with a degree of dissatisfaction, since they were deprived of access to many cases that they would previously have performed themselves, especially appendicectomies, inguinal herniorraphies, and cholecystectomies. These three common general surgical procedures had traditionally provided ample opportunity for residents to acquire basic surgical operative skills training at a relatively early stage in their careers.
In this study, the introduction of laparoscopic cholecystectomy was associated with a serious hiatus in exposure of residents to biliary surgical procedures as primary operator. However, once the learning phase had been passed, cholecystectomy became readily reintegrated into the resident training schedule with no increase in complication rate or hospital stay. The average length of stay documented in this study, in common with European experience in general, is longer than that reported from North American centers. Economic considerations will continue to force a decrease in postoperative hospital stay, although the period under review in this study was too short to detect any change in length of stay.
Because of the major socio-political changes in this region associated with German reunification, it is difficult to obtain a valid comparison of resident training experience in this clinic prior to the introduction of laparoscopic techniques, but the proportion of cases currently performed by residents is in line with the numbers reported from other centers. These other studies have also shown a similar dip in residents' exposure to biliary surgery during the development phase of laparoscopic surgical services, which recovers once institutional expertise with the procedure increases.3,4 One important trend that has emerged is that laparoscopic cholecystectomy tends to be performed by residents at a more senior level, whereas, previously, residents were introduced to open cholecystectomy at a more junior grade.1 It has been suggested that residents need a higher level of skill and should be more advanced in their training before being allowed to perform cholecystectomy laparoscopically.5 In addition, many centers advocate the use of training rigs and animal models as a means of acquiring laparoscopic skills before operating on patients.6,7 The trainees in this clinic are encouraged to practice laparoscopic dissection techniques using a training rig and attend an animal laboratory laparoscopic training course. Interestingly, our residents regarded the training gained in the animal laboratory as being of limited benefit compared to the value of proctored operative experience. Although laparoscopic skills can be measurably improved by bench training, the need for animal laboratory training is less clear-cut now that sufficient experience has accumulated throughout the surgical community 5,8–10 Although undoubtedly of great value in the early stages of dissemination of these operative skills and in the evaluation of new techniques, routine animal workshop training may be a luxury that many centers feel is no longer affordable or necessary. These teaching modalities can certainly never replace the absolute requirement for supervision of the trainee by an experienced laparoscopic surgeon during the learning curve phase. The exact number of procedures that should be performed under supervision has been the subject of some debate. Davidoff and colleagues reported that the risk of bile duct injury was highest during the first 13 cases.11 Analysis of the Southern Surgeons' Club series in the South-Eastern United States showed that 90% of bile duct injuries occurred within the first 30 cases of the operating surgeon.12 The European Association of Endoscopic Surgery has recommended that surgeons who have not graduated from a residency program that provides structured experience in laparoscopic surgery should attend an approved EAES laparoscopic cholecystectomy course and perform 3-5 preceptor-assisted cases, as well as providing documentation of their subsequent ten cases before being granted privileges in laparoscopic cholecystectomy.13
The accompanying decrease in the number of open cholecystectomies also has important implications for residency training. As with other centers, we have found that the number of open cholecystectomies has dwindled dramatically. These cases tend to be technically difficult and, therefore, usually are performed by a senior resident or staff surgeon.1 Although some reports contend that residents still receive adequate exposure to open biliary procedures in the era of laparoscopic cholecystectomy, we would suggest that it is becoming increasingly difficult to achieve this aim.14
Organizers of residency programs must continue to monitor these changing trends to ensure that the needs of their trainees are met in the future. Appendicectomy, whether open or laparoscopic, will remain an important “starter” operation, allowing junior residents to develop laparoscopic skills at an early stage.15 As a higher percentage of laparoscopic cholecystectomies are performed by residents, and junior residents learn laparoscopic technique from appendicectomy, some of the more straightforward cases should “filter down” to the more junior residents. With the exception of numbers of open biliary cases, the situation is likely to continue to improve rather than worsen for surgical residents.
Footnotes
Presented at the Joint Euro-Asian Congress of Endoscopic Surgery, Istanbul, June 1997. The abstract was published in 1997, Volume 11, Surgical Endoscopy. Mr. Geoghegan was supported in part by a Travel Grant from the Royal College of Surgeons in Ireland.
References:
- 1. Schauer PR, Page CP, Stewart RM, Schwesinger WH, Sirinek K. The effect of laparoscopic cholecystectomy on resident training. Am J Surg. 1994;l68:566–570 [DOI] [PubMed] [Google Scholar]
- 2. Shaper NJ, Harrison M, Bates T. Impact of laparoscopic cholecystectomy on surgical training. Ann R Coll Surg Engl. 1996;78:39–42 [PMC free article] [PubMed] [Google Scholar]
- 3. Schol FP, Go PM, Gouma DJ, Koostra G. Laparoscopic cholecystectomy in a surgical residency training programme. Eur J Surg. 1996;l62:193–197 [PubMed] [Google Scholar]
- 4. Sefr R, Ochmann J. Our experience with early integration of laparoscopic cholecystectomy in surgical residency training. Surg Endosc. 1995;9:902–904 [DOI] [PubMed] [Google Scholar]
- 5. Hodgson WJ, Byrne DW, Savino JA, Liberis G. Laparoscopic cholecystectomy. The early experience of surgical attendings compared with residents trained by apprenticeships. Surg Endosc. 1994;8:1058–1062 [DOI] [PubMed] [Google Scholar]
- 6. Cushieri A. The dust has settled - let's sweep it clean. J R Coll Surg. 1992;37:213–214 [PubMed] [Google Scholar]
- 7. Wolfe BM, Szabo Z, Moran ME, Chan P, Hunter JG. Training for minimally invasive surgery. Need for surgical skills. Surg Endosc. 1993;7:93–95 [DOI] [PubMed] [Google Scholar]
- 8. Friedman RL, Pace BW. Resident training in laparoscopic cholecystectomy. Surg Endosc. 1996;10:26–28 [DOI] [PubMed] [Google Scholar]
- 9. Hawasli A, Featherstone R, Lloyd L, Vorhees M. Laparoscopic training in residency program. J Laparoendosc Surg. 1996;6:171–174 [DOI] [PubMed] [Google Scholar]
- 10. Melvin WS, Johnson JA, Ellison EC. Laparoscopic skills enhancement. Am J Surg. 1996;172:377–379 [DOI] [PubMed] [Google Scholar]
- 11. Davidoff A, Pappas TN, Murray EA, et al. Mechanisms of major biliary injury during laparoscopic cholecystectomy. Ann Surg. 1992;215:196–202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Moore MJ, Bennett CL. The learning curve for laparoscopic cholecystectomy. The Southern Surgeons Club. Am J Surg. 1995;170:55–59 [DOI] [PubMed] [Google Scholar]
- 13. EAES guidelines. Training and assessment of competence. Surg Endosc. 1994;8:721–722 [PubMed] [Google Scholar]
- 14. Deziel DJ, Millikan KW, Staen ED, Doolas A, Economou SG. The impact of laparoscopic cholecystectomy on the operative experience of surgical residents. Surg Endosc. 1993;7:17–21 [DOI] [PubMed] [Google Scholar]
- 15. Botha AJ, Elton C, Moore EE, Sauven P. Laparoscopic appendicectomy: a trainee's perspective. Ann R Coll Surg Engl. 1995;77:259–262 [PMC free article] [PubMed] [Google Scholar]