Abstract
Laparoscopic cholecystectomy (LC) using an electrosurgery energy source was successfully performed in 59 (95%) out of 62 selected patients. The procedures were performed by different surgical teams at Trakya University, Medical Fakulty, in the department of General Surgery and the Karl-Franzens-University School of Medicine, in the department of General Surgery. Cholangiography was routine at Karl Franzens University and selective at Trakya University. Laparoscopic intraoperative cholangiography (IOC) was performed in 48 (81.3%) patients, and open IOC was performed in 3 patients. Two patients had common duct stones; one of which was unsuspected preoperatively. These cases underwent endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic papillotomy (EP). One patient had a choledocal tumor, unsuspected preoperatively. Anatomical anomalies were not identified. Cholangiography could not be performed in one case in which there was no suspected pathology. ERCP was performed on one patient 30 days after being discharged because of acute cholangitis. In this case, residual stones were identified in the choledocus. Four patients underwent open cholecystectomy because of tumor, unidentified cystic duct or common bile duct pathology that could not be visualized on the cholangiogram. Our study suggests that cholangiography performed via the cystic duct before any structures are divided can prevent the most serious complication of laparoscopic cholecystectomy – common duct injury. We recommend that cholangiography be attempted on all patients undergoing LC.
Keywords: Laparoscopic cholecystectomy, Cholangiography, Tumor, Residual stone, ERCP
INTRODUCTION
Laparoscopic cholecystectomy (LC) is now the procedure of choice for the treatment of uncomplicated symptomatic gallstones.1,2 The advantages of minimal access technique go beyond that of a relatively painless postoperative period and small scar size.3 Intraoperative cholangiography (IOC) in the course of LC is not only valuable in detecting common bile duct stones, but also in delineating the anatomy of the biliary ducts, in facilitating dissection, avoiding injuries to the biliary tract and in identifying other abnormalities, such as fistulas, cysts and tumors of the biliary system.4 Cholangiography should be performed via the cystic duct before any structures are divided, as this can prevent the most serious complication of laparoscopic cholecystectomy – common duct injury. We feel that cholangiography should be attempted on all patients undergoing LC.5 This study was performed to evaluate the importance of intraoperative cholangiography during laparoscopic cholecystectomy.
MATERIALS AND METHODS
This study prospectively analyzes intraoperative cholangiographic findings in 62 consecutive patients who preoperatively were planned to have a LC and laparoscopic IOC. The procedures were performed by different surgical teams at Trakya University, Medical Fakulty, in the department of General Surgery in Turkey between January 11, 1997 and January 12, 1998 and at Karl-Franzens-University School of Medicine, in the department of General Surgery in Austria between January 10, 1996 and January 4, 1997. Cholangiography was routine at Karl Franzens University and selective at Trakya University. There were 46 females and 16 males, with a mean age of 44 years (range 10-79 years). Preoperative ultrasound examination of the gallbladder and common duct was performed in all patients. Two patients had undergone prior endoscopic sphincterotomy. Laparoscopic cholecystectomy was performed using a standard four-cannula technique. Laparoscopic cholecystectomy with cholangiography was carried out as previously described. Traction of the gallbladder fundus was applied in a cephalad direction with a grasper placed through the midclavicular port. The cystic duct was identified and dissected free. An endoscopic clip applier was then passed through the 10-mm epigastric port, and a single clip was placed across the proximal cystic duct to prevent spillage of gallbladder content. Endoscopic scissors were passed through the epigastric port, and the cystic duct was incised along one-half its circumference just distal to the previously placed titanium clip. A catheter was guided into the partially transected proximal cystic duct. Only in one case was the catheter inserted into the fundus of gallbladder (cholecystocholangiography). (The endoscopic grasper may be used in maneuvering the catheter. If difficulty is encountered in passing the catheter into the duct, a guidewire passed through the cholangiocatheter into the duct may facilitate this step.) The catheter was inserted 5 mm into the partially transected proximal cystic, and the catheter was secured in place in the cystic duct with a cholangioclamp (Storz, Inc.). A portable C-arm was positioned over the patient, and 5 to 15 mL of contrast (50% solution of imagopaque 300″) material was injected through the catheter to obtain visualization of the biliary ductal system. A photograph was taken of the cystic duct cholangiogram. After cholangiography, the biliary duct was flushed with saline. The catheter was removed; two clips were then placed on the common duct end of the cystic duct, and it was divided with scissors.
RESULTS
Laparoscopic cholangiography was performed in 48 out of 59 patients, and open transcystic cholangiography was performed in 3 patients. We attempted cholangiography in all patients but did not succeed in 11 (17.7%) patients.
Forty-seven cholangiographic studies were accomplished via the transcystic route, and one study was obtained via the gallbladder - a cholecysto-cystic duct IOC. Technically, visualization of the biliary tree was possible in all of these patients. Visualization could not be done adequately in only two cases. Of the 51 patients who had cholangiograms, 47 (92.1%) had normal operative cholangiograms, and 2 (10.2%) had common duct stones. One of the two was identified using operative cholangiography; other one was known preoperative (Figure 1). All these calculi were successfully treated with postoperative ERCP, EP and stone extraction. We had not done decompression of the biliary tree using the cystic duct catheters at the time of surgery. Two patients (10.2%) had no adequate visualized common biliary ductal system using operative cholangiography. We immediately converted to conventional surgery. One (1.9%) of the two patients had choledocus tumor (Figure 2); the other had occlusion of the common hepatic duct by clips (1.9%). The clip was removed immediately. No complications occurred in this group, but in one patient (1.6%) cholangiography could not be performed due to a cholangitis attack secondary to residual stones 30 days postoperatively (Figure 3). This case was successfully treated with ERCP, sphincterotomy, and stone extraction. The average time for the IOC was 11 minutes, with a range of 5-18 minutes.
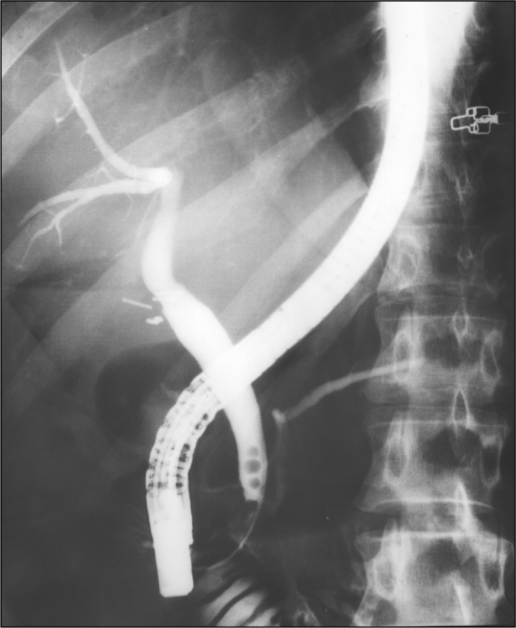
Figure 1.
ERCP demonstrating stones in the common bile duct. In this case, endoscopic removal of the common bile duct stones was done.
Figure 2.
There are a few stones in the distal common bile duct. This patient was referred to us with cholanjitis after laparoscopic cholecystectomy.
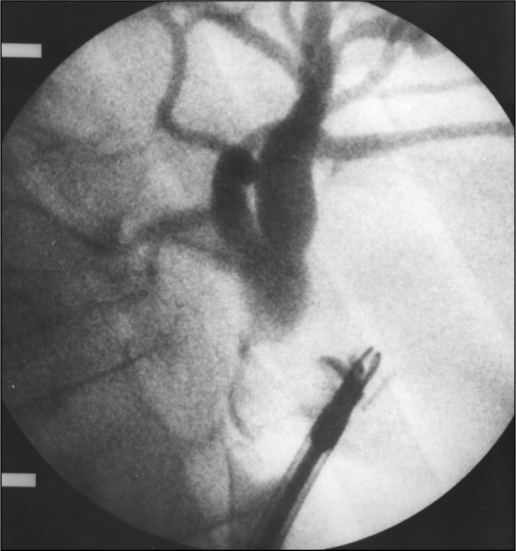
Figure 3.
Laparoscopic IOC shows multiple stones in the common bile duct. This patient underwent endoscopic papillotomy, ERCP, and endoscopic extraction of common bile duct stones.
DISCUSSION
Common bile duct stones are found in approximately 8% to 12% of all patients who undergo cholecystectomy for symptomatic gallstone disease. Intraoperative cholangiography continues to be an effective way of identifying common bile duct stones at the time of surgery.6 Recently, considerable discussion has focused on the role of IOC in the performance of LC.7–9 Initial recommendations included routine IOC so as to identify ductular anatomy and hopefully reduce the incidence of common bile duct injury. With greater experience, many authors have begun to recommend selective cholangiography for LC. When the anatomical structures are not clearly distinguishable during LC, IOC is mandated in order to avoid serious injury to vital structures. Surgeons performing LC should be well versed with the technique of IOC so that it can be utilized when appropriate.6
Technical success, defined as the ability to obtain a cholangiogram of sufficient quality to allow interpretation, appears to be over 90% in most hands. Although follow-up was not complete in most studies, the percentage of patients experiencing the clinical syndrome of retained stones was less than 1% in the selective approach. These studies incorporated preoperative ERCP in those individuals with a high risk for common bile duct stones (IO). Laparoscopic IOC (whether used selectively or routinely) is safer than ERCP and more cost effective (IO). Two of our patients underwent ERCP and EP preoperatively. But in one case, enough stones could not be removed in the common bile duct, which was detected by laparoscopic IOC (Figure 4).
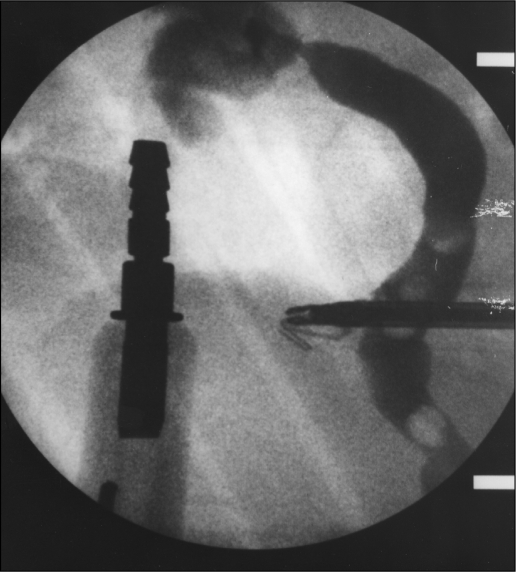
Figure 4.
This laparoscopic IOC shows incomplete obstruction at the common bile duct. In this case had malign tumor in proximal common hepatic duct on biopsy.
In a recent consensus article from the National Institute of Health (NIH), preoperative ERCP or transhepatic cholangiography was recommended for all patients with clinical suspicion of common duct stones prior to LC. According to the NIH, this strategy would allow “laparoscopic cholecystectomy to be performed without the need for (intraoperative) common duct evaluation and with detailed knowledge of the biliary anatomy.” This recommendation seems to have been founded on the perception that laparoscopic IOC is difficult to perform, relatively inaccurate and costly when compared to preoperative cholangiography.10–14
Intraoperative cholangiography in the course of laparoscopic cholecystectomy is not only valuable in detecting common bile duct stones, but also in delineating the anatomy of the biliary ducts, facilitating dissection, avoiding injuries to the biliary tract and identifying other abnormalities, such as fistulas, cysts and tumors of the biliary system.4 All of our patients who had cholelithiasis or gallbladder polyp had no preoperative findings to suggest ductal pathology, with the exception of one who had common duct stones preoperatively and who underwent ERCP and EP. Two of our 62 patients had common duct stones at surgery. In one case, cholangiography could not be performed and there was no suspected pathology. Thirty days after being discharged, ERCP was performed because of cholangitis and common duct stones. Ultrasound examination showed normalized common ducts, with the exception of one who had common duct stones preoperatively, and liver function tests were normal or revealed minimal elevation, not suggestive of ductal pathology.
Two cases had inadequate visualization of the common biliary ductal system using operative cholangiography. We immediately converted to conventional surgery. One of the two patients had a choledochus tumor; the other patient had occlusion of the common hepatic duct by clips. The clip was removed immediately.
Berci suggests that 10% of patients harbor biliary ductal anomalies of surgical importance that can be identified using cholangiography.15 We had no biliary ductal anomalies. Proponents of routine cholangiography contend that the extent of common duct injury can be minimized with technically adequate cholangiograms.7
These enthusiasts also emphasize the importance of immediate recognition of biliary tract injuries as a way to decrease overall morbidity and mortality.16
The routine use of IOC ensures experience with the technique, optimizing results and interpretation to a much greater extent than when IOC is employed occasionally, as dictated by the selective policy.17
Footnotes
This scientific paper was presented at the 8th International Meeting of Laparoendoscopic Surgeons, SLS Annual Meeting, Endo Expo '99, December 4-7, 1999 in New York City, USA.
Contributor Information
Fatin R. Polat, Assistant Doctor, Department of General Surgery, Trakya University Hospital, Edirne, Turkey..
Ilker Abci, Assistant Doctor, Department of General Surgery, Trakya University Hospital, Edirne, Turkey..
Irfan Coskun, Professor of Surgery, Department of General Surgery, Trakya University Hospital, Edirne, Turkey..
Selman Uranues, Professor of Surgery, Department of Surgical Research, Karl Franzens University School of Medicine, Graz, Austria..
References:
- 1. Macintyre IMC, Wilson RG. Laparoscopic cholecystectomy. Br J Surg. 1993;80:552–559 [DOI] [PubMed] [Google Scholar]
- 2. Perissat J. Laparoscopic cholecystectomy. The European experience. Am J Surg. 1993;165:444–449 [DOI] [PubMed] [Google Scholar]
- 3. Roumen RM, van Meurs PA, Kuypers HH, Kraak WA, Sauerwein RW. Serum interleukin-6 and C reactive protein responses in patients after laparoscopic or conventional cholecystectomy. Eur J Surg. 1992;158:541–544 [PubMed] [Google Scholar]
- 4. Kuster GG, Gilroy S, Graefen M. Intraoperative cholangiography for laparoscopic cholecystectomy. Surg Gynecol Obstet. 1993;176(5):411–417 [PubMed] [Google Scholar]
- 5. Phillips EH, Berci G, Carroll B, Daykhovsky L, Sackier J, PazPartlow M. The importance of intraoperative cholangiography during laparoscopic cholecystectomy. Am Surg. 1990;56(12):792–795 [PubMed] [Google Scholar]
- 6. Lipsett PA, Karan JA, Yeo CJ, Tompkins RK, Cushierrei A, Rosin DR. Gallbladder and bile duct. In: Zinner Michael J., ed. Abdominal Operations. 10th ed. London: Prentice Hall International, Inc. 1997:1701–1898 [Google Scholar]
- 7. Sackier JM, Berci G, Phillips E, Carroll B, Shapiro S, Pazpartlow M. The role of cholangiography in laparoscopic cholecystectomy. Arch Surg. 1991;126:1021. [DOI] [PubMed] [Google Scholar]
- 8. Soper NJ, Dunnegan DL. Routine versus selective intraoperative cholangiography during laparoscopic cholecystectomy. World J Surg. 1992;16:1133. [DOI] [PubMed] [Google Scholar]
- 9. Traverso LW, Hauptmann EM, Lynge DC. Routine intraoperative cholangiography and its contribution to the selective cholangiographer. Am J Surg. 1994;167:464. [DOI] [PubMed] [Google Scholar]
- 10. Christopher R, Bryan H, Lewis B. Laparoscopic cholecystectomy, cholangiography and management of choledocholithiasis. In: Pappas N., ed. Atlas of Laparoscopic Surgery. London: Electronic Press Ltd; 1996:CD [Google Scholar]
- 11. Carrol BJ, Phillips EH, Rosenthal R, Gleischman S, Bray JF. One hundred consecutive laparoscopic cholangiograms. Surg Endosc. 1996;10:319–323 [DOI] [PubMed] [Google Scholar]
- 12. Johnson AS, Ferrara JJ, Steinbers SM, Gassen GM, Hollier LH, Flint LM. The role of endoscopic retrograde cholangiography: sphincterotomy versus common bile duct exploration. Am Surg. 1993;59:78–84 [PubMed] [Google Scholar]
- 13. Lillemoe K, Yeo CH, Talamini M, et al. Selective cholangiography. Ann Surg. 1992;215(6):669–676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. NIH Consensus Conference Gallstones and Laparoscopic Cholecystectomy. JAMA. 1993;269(8):1018–1024 [PubMed] [Google Scholar]
- 15. Berci G. Biliary ductal anatomy and anomalies. Surg Clin North Am. 1992;72:1069–1075 [DOI] [PubMed] [Google Scholar]
- 16. McSherry GH. Cholecystectomy: the golden standard. Am J Surg. 1989;158:174–178 [DOI] [PubMed] [Google Scholar]
- 17. Cuschieri A, Berci G. Laparoscopic biliary surgery. In: Cuschieri A, ed. Laparoscopic Surgery. 2nd ed. London, Edinburg, Boston, Melbourne, Paris, Berlin, Vienna, Oxford: Blackwell Scientific Publication; 1995:69–131 [Google Scholar]