Abstract
Background and Objective:
Despite the numerous and often cited benefits of routine cholangiography during laparoscopic cholecystectomy, universal application of this technique has not been realized. Surgeons who advocate selective cholangiography cite the extra cost, the low yield of unanticipated findings, and the marked increase in the duration of the operation when cholangiography is added to laparoscopic cholecystectomy. We present our experience with preview cholangiography and compare it with the transcystic-duct approach.
Methods:
We attempted preview cholangiograms on 11 consecutive patients undergoing laparoscopic cholecystectomy. Successful cholangiography was determined by using established radiologic criteria.
Results:
Preview cholangiogram was successful in all 11 patients. No complications occurred. The average time required was 110 seconds. The mean operating time was 52 minutes. These times are far better than our best accomplishments using the cystic duct cannulation method for cholangiography (mean cholangiogram time, 22 minutes, and mean operative time, 75 minutes) following the first 100 cases.
Conclusions:
Preview cholangiography is a safe, relatively easy, quick method for outlining the anatomy of the extrahepatic biliary tree prior to dissection necessary to remove the gallbladder with laparoscopic techniques. The ease of this approach should result in more widespread use of cholangiography during laparoscopic cholecystectomy.
Keywords: Laparoscopic cholecystectomy, Cholangiogram, Preview cholangiography
INTRODUCTION
Laparoscopic cholecystectomy is now the procedure of choice for treating uncomplicated symptomatic gallstones.1,2 Even though laparoscopic cholecystectomy has been shown to be equivalent to open cholecystectomy with respect to morbidity and mortality, it offers the advantage of small scar size, shorter length of hospital stay, quicker recovery and return to full activity, and a relatively painless postoperative period. Mirizzi3 first popularized intraoperative cholangiography in 1932; however, its use has been controversial for years, and this controversy has continued into the laparoscopic era. Advocates 4–9 believe that routine cholangiography will not only help delineate biliary anatomy, detect common bile duct stones, facilitate dissection, and avoid injury to the biliary tract but also help identify other clinically silent diseases, such as cholangiocarcinoma, duodenal adenocarcinoma, and choledochal cyst. Those surgeons 10–12 who advocate selective use of intraoperative cholangiography cite the increased cost and the low yield. However, the time and the cost associated with intraoperative cholangiography are outweighed by the cost of managing bile duct injuries and working up retained stones postoperatively. Traditionally, intraoperative cholangiography has been performed by cannulating the cystic duct, which requires dissection and partial transection of the cystic duct and its cannulation, which can be tedious and time consuming. Daoud and McCallum13 reported a successful cystic duct cannulation rate of approximately 83%. In addition, the transcystic approach can also lead to ductotomy of other structures misidentified as the cystic duct.4–9 In preview cholangiography, the cholangiogram is obtained before any dissection is begun. It not only prevents erroneous ductotomies, but it is easier and quicker. In addition, it is more cost-effective because the operative time is shorter.
PATIENTS AND METHODS
Methods
We used the standard 4-cannula technique to perform laparoscopic cholecystectomy in all cases. A ratcheted grasper was passed through the midaxillary port. This was used to grasp the fundus of the gallbladder, which was then pushed in a cephalad direction to expose the gallbladder ampulla.
The traditional transcystic duct cannulation approach required dissection that began on the gallbladder and continued until the “cystic duct-gallblader junction” was identified. A single clip was then applied to the proximal “cystic duct.” Endoscopic scissors were then used to partially transect the “cystic duct” just distal to the previously placed clip. The cholangiocatheter was then introduced through a separate 8 Fr introducer sheath into the cystic duct, and then cholangiogram was performed.
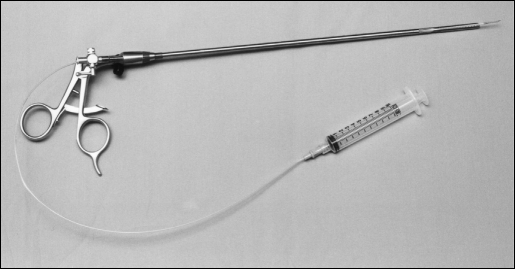
The specialized clamp used for the preview cholangiogram is a 5-mm grasper with a channel for the introduction of the cholangioneedlecatheter (Figure 1). Before any dissection is begun, this specialized clamp is passed through the midclavicular port and applied across the neck of the gallbladder. A disposable cholangiogram catheter with a 19-gauge needle is then introduced through the channel and advanced to puncture the gallbladder Hartman pouch. Biliary access is confirmed by aspiration of bile. Dye is injected, and the cholangiogram is performed. The clamp jaw can be opened and the gallbladder aspirated, or the grasper can be moved down to the puncture to prevent bile leakage and also to be used for traction on the gallbladder ampulla for the remainder of the operation. Figure 2 represents a typical cholangiogram obtained using the preview cholangiogram system.
Figure 1.
The specialized grasper with the cholangioneedlecatheter used for preview cholangiography.
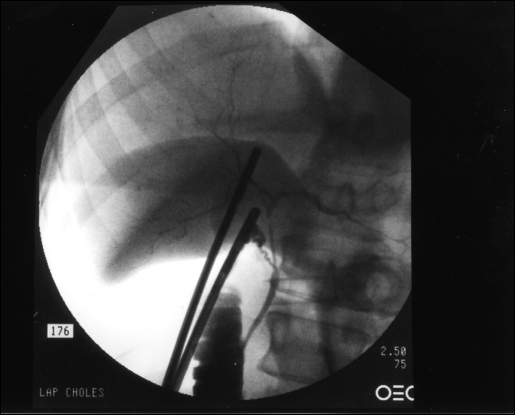
Figure 2.
A typical cholangiogram obtained using the preview cholangiogram system.
Patients
Of the 11 patients, 6 were males and 5 were females. The mean age of all the patients was 67 years (range, 34 to 80). Two patients were operated on for acute cholecystitis. In one patient, who had subacute cholecystitis, preview cholangiography revealed the presence of common bile duct stones, which were removed by laparoscopic common bile duct exploration. Six patients had chronic cholecystitis, and two of these patients were operated on with associated procedures (one had a laparoscopic sigmoid resection, and the other had a laparoscopic ventral hernia repair). One patient had biliary dyskenesia without stones. Her cholecystokinin (CCK) stimulated gallbladder ejection fraction was measured at 9%, and her symptoms consisted of postprandial right upper quadrant pain. One patient, an 80-year-old male, had a gangrenous gallbladder with pericholecystic abscess. He presented with diffuse abdominal pain. A computerized axial tomography (CAT) scan of the abdomen revealed a heterogeneous density within the gallbladder fossa with surrounding indurations suspicious for abscess involving the liver (Figure 3).
Figure 3.
A CAT scan demonstrating a heterogeneous density within the gallbladder fossa (liver abscess).
RESULTS
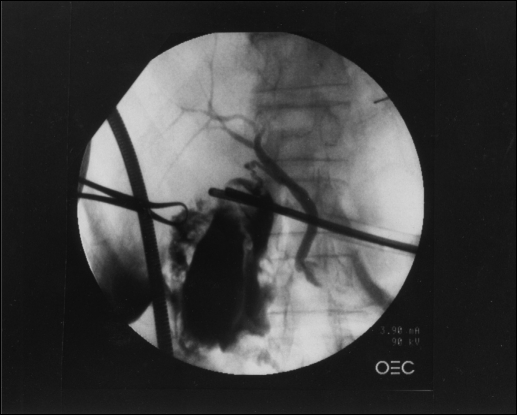
Preview cholangiograms were successfully performed in all 11 patients. No complications occurred. In one patient, preview cholangiography revealed the presence of unsuspected common bile duct stones. In another patient, reflux of contrast into the gallbladder occurred due to incomplete exclusion of the gallbladder by the application of the specialized clamp. However, preview cholangiography was successfully performed with clear visualization of the cystic duct and the remainder of the biliary tree including flow of contrast into the duodenum. In the patient with the gangrenous gallbladder, extravasation of contrast and reflux of the contrast into the gallbladder occurred (Figure 4). Even in this patient, clear visualization of the cystic duct and the reminder of the biliary tree was obtained. The average time elapsed during cholangiography was 110 seconds (range 91 to 142 seconds). The mean operating time was 52 minutes (range 48 to 66 minutes). These times, even this early in our experience using this technique, are far better than our best accomplishments using the cystic duct cannulation method for performing cholangiography. The mean cholangiogram time was 22 minutes (range 12 to 38 minutes), and the mean operative time was 75 minutes (range 68 to 92 minutes) following the first 100 cases.4
Figure 4.
Preview cholangiogram in the patient with gangrenous gallbladder demonstrating contrast extravasation and reflux into the gallbladder.
DISCUSSION
We have by previous experience and by this limited experience demonstrated that intraoperative cholangiography offers the advantage of visualization of the biliary anatomy, which we strongly believe will decrease the number and severity of bile duct injuries and will also lead to early detection of clinically silent diseases of the extrahepatic biliary tree that may be missed because of the limitations of the laparoscopic approach. The availability of preview cholangiography and the ease of its performance demonstrated even this early in our experience should eliminate the few remaining obstacles to making intraoperative cholangiography routine practice. Corbitt and Leonetti9 in their experience with 1060 consecutive laparoscopic intraoperative cholangiograms reported one case in which the cystic duct-common duct junction was misidentified and an incision was made at this junction leading to the need for T-tube placement. In our experience with 511 consecutive patients who underwent laparoscopic cholangiogram with the transcystic duct approach, we too, in two cases despite careful dissection, mistook the common hepatic duct as the cystic duct. This visual error led to the partial transection of the duct in both cases.4 Preview cholangiography should completely eliminate this potential problem.
CONCLUSION
Preview cholangiography is the answer and the future. It has many advantages over the traditional transcystic duct cholangiography. It is a safe, relatively easy, and exceptionally quick method for outlining the anatomy of the extrahepatic biliary tree. It is safe because cholangiography is performed prior to any dissection. It is quick; therefore, the total cost is significantly reduced because operative time is decreased. It can be performed even on gangrenous gallbladders. Because of the ease of preview cholangiography and its ability to outline the extrahepatic biliary anatomy, intraoperative preview cholangiography should be routinely performed.
References:
- 1. Wastell C. Laparoscopic cholecystectomy. Better for patients and health service. BMJ. 1991; 302: 303–304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. National Institutes of Health consensus development conference statement on gallstones and laparoscopic cholecystectomy. Am J Surg. 1993; 165;390–396 [DOI] [PubMed] [Google Scholar]
- 3. Mirizzi PL. Operative cholangiography. Surg Gynecol Obstet. 1937; 65: 702–710 [Google Scholar]
- 4. Romanelli JR, Edoga JK. 10 reasons for routine intraoperative cholangiography during laparoscopic cholecystectomy. Contemp Surg. 2000; 56: 281–286 [Google Scholar]
- 5. Polat FR, Abci I, Coskun I, Uranues S. The importance of intraoperative cholangiography during laparoscopic cholecystectomy. JSLS. 2000; 4(2): 103–107 [PMC free article] [PubMed] [Google Scholar]
- 6. Phillips EH, Berci G, Carroll B, Daykhovsky L, Sackier J, Partlow M. The importance of intraoperative cholangiography during laparoscopic cholecystectomy. Am Surg. 1990; 56(12): 792–795 [PubMed] [Google Scholar]
- 7. Stark ME, Loughry CW. Routine operative cholangiography with cholecystectomy. Surg Gynecol Obstet. 1980; 151: 657–658 [PubMed] [Google Scholar]
- 8. Doyle PJ, Ward-McQuaid JN, Smith AM. The value of routine properative cholangiography-a report of 4000 cholecystectomies. Br J Surg. 1982; 69: 617–619 [DOI] [PubMed] [Google Scholar]
- 9. Corbitt JD, Jr, Leonetti LA. One thousand and six consecutive laparoscopic intraoperative cholangiograms. JSLS. 1997; 1: 13–16 [PMC free article] [PubMed] [Google Scholar]
- 10. Gerber A, Malcom KA. The case against routine operative cholangiography. Am J Surg. 1982; 143: 734–736 [DOI] [PubMed] [Google Scholar]
- 11. Hauer-Jensen M, Karesen R, Nygaard K, et al. Consequences of routine peroperative cholangiography during cholecystectomy for gallstone disease: a prospective, randomized study. World J Surg. 1986; 10: 996–1002 [DOI] [PubMed] [Google Scholar]
- 12. Pernthaler H, Sandbichler P, Schmid T, Margreiter R. Operative cholangiography in elective cholecystectomy. Br J Surg. 1990; 77: 1343. [DOI] [PubMed] [Google Scholar]
- 13. Daoud M, McCallum MJ. An easy and effective method of cholangiography in laparoscopic cholecystectomy: laparascopic cholecystocholangiography. Aust NZ J Surg. 1999; 69(2): 138–140 [DOI] [PubMed] [Google Scholar]